Abstract
Background
Multidrug resistance (MDR) in the family Enterobacteriaceae is a perniciously increasing threat to global health security. The discovery of new antimicrobials having the reversing drug resistance potential may contribute to augment and revive the antibiotic arsenal in hand. This study aimed to explore the anti-Enterobacteriaceae capability of bioactive polyphenols from Punica granatum (P. granatum) and their co-action with antibiotics against clinical isolates of Enterobacteriaceae predominantly prevalent in South Asian countries.
Methods
The Kandhari P. granatum (Pakistani origin) extracts were tested for anti-Enterobacteriaceae activity by agar well diffusion assay against MDR Salmonella enterica serovar Typhi, serovar Typhimurium and Escherichia coli. Predominant compounds of active extract were determined by mass spectrometry and screened for bioactivity by agar well diffusion and minimum inhibitory concentration (MIC) assay. The active punicalagin was further evaluated at sub-inhibitory concentrations (SICs) for coactivity with nine conventional antimicrobials using a disc diffusion assay followed by time-kill experiments that proceeded with SICs of punicalagin and antimicrobials.
Results
Among all P. granatum crude extracts, pomegranate peel methanol extract showed the largest inhibition zones of 25, 22 and 19 mm, and the MICs as 3.9, 7.8 and 7.8 mg/mL for S. typhi, S. typhimurium and E. coli, respectively. Punicalagin and ellagic acid were determined as predominant compounds by mass spectrometry. In plate assay, punicalagin (10 mg/mL) was active with hazy inhibition zones of 17, 14, and 13 mm against S. typhi, S. typhimurium and E. coli, respectively. However, in broth dilution assay punicalagin showed no MIC up to 10 mg/mL. The SICs 30 μg, 100 μg, and 500 μg of punicalagin combined with antimicrobials i.e., aminoglycoside, β-lactam, and fluoroquinolone act in synergy against MDR strains with % increase in inhibition zone values varying from 3.4 ± 2.7% to 73.8 ± 8.4%. In time-kill curves, a significant decrease in cell density was observed with the SICs of antimicrobials/punicalagin (0.03–60 μg/mL/30, 100, 500 μg/mL of punicalagin) combinations.
Conclusions
The P. granatum peel methanol extract exhibited antimicrobial activity against MDR Enterobacteriaceae pathogens. Punicalagin, the bacteriostatic flavonoid act as a concentration-dependent sensitizing agent for antimicrobials against Enterobacteriaceae. Our findings for the therapeutic punicalagin-antimicrobial combination prompt further evaluation of punicalagin as a potent activator for drugs, which otherwise remain less or inactive against MDR strains.
Similar content being viewed by others
Background
South Asian countries including Pakistan are considered a hot zone for the fast-growing emergence of both multi-drug resistant (MDR) and extensively drug-resistant bacterial strains of the Enterobacteriaceae family [1, 2]. Resistance to last-resort antibiotics like carbapenem [3, 4], fluoroquinolones [5], and cephalosporin [6] have knocked down all health-related assurances by increasing the risk of morbidity and mortality rates associated with Enterobacteriaceae infections, making this an issue of significant global concern. For the upcoming two decades, a budget of approximately 100 trillion United States Dollars and millions of lives per year are considered at risk due to the emergence of “antibiotic resistance superbugs” with even worse consequences in low-middle income countries. More than 4.95 million mortalities are associated with increasing drug resistance against broad-spectrum antibiotics [7]. Several epidemiological reports all over the world proved the prevalence of multi-drug resistant extended-spectrum beta-lactamase-producing isolates belonging to Enterobacteriaceae from healthcare facilities as well as in community-acquired infections [8,9,10].
In the last decade, Escherichia coli (E. coli) has emerged as a microbe acquiring antibiotic resistance at an alarming rate with urinary tract infections being the most reported clinical infections in Pakistan and about 28 studies have described its high resistance against first-line antibiotics [11]. World Health Organization (WHO) has reported that E. coli resistance to third-generation cephalosporins and fluoroquinolones would lead to the end of the antibiotic era [12].
Salmonella enterica subspecies enterica serovar Typhi (S. typhi) causes the deadly systemic infection called typhoid fever also referred to as “enteric fever” when combined with paratyphoid fever caused by Paratyphi A, B and C [13]. Rapidly reducing susceptibility to fluoroquinolone in South Asian countries has been reported [14], which makes third-generation cephalosporins and azithromycin the drugs of choice. Although cephalosporin resistance has not been reported as extensively as fluoroquinolone resistance, S. typhi is acquiring resistance due to the production of extended-spectrum beta-lactamases, especially in Asian countries including Pakistan [15]. Every year 11.9 million to 27.1 million people, mostly children and elderly, suffer from enteric fever globally and mortality ranges from 129,000 to 223,000 [16].
Salmonella enterica serovar Typhimurium (S. typhimurium), a zoonotic serovar, is becoming a global threat due to its high antibiotic resistance rate in the last decade. Gastroenteritis is the major infection caused by non-typhoidal Salmonella in humans with 80.3 million foodborne illnesses per year [17]. A study reported that 35.2% of isolates of S. typhimurium were carrying the beta-lactam (carbapenems and cephalosporins) resistance gene (blaTEM-1) in Pakistan [1].
Overall, in the Enterobacteriaceae, cephalosporin resistance is due to the production of enzymes called beta-lactamases such as extended-spectrum beta-lactamase, AmpC beta-lactamases [18] and quinolone resistance is due to gene mutation in quinolone resistance-associated genes [19]. This resistance can be correlated with the irrational use of antibiotics in food animals for their better growth and infection prevention, which makes a linkage of antibiotic resistance between food and its consumers i.e., animals and humans [20]. This rapid emergence of antibiotic resistance warrants re-screening of natural products as a faster approach to identify new “antimicrobial magic bullets”, which can act alone or contribute synergistic effects with the inactive or lesser active existing antibiotics to augment their potencies and reverse their drug resistance. In this manner, exploration of phytochemicals may contribute to identify novel antibiotic potentiators to augment the potencies of drugs against which the resistance has already emerged and/or the first-line antibiotics, which will likely face resistance in near future [21,22,23,24].
Punica granatum is famous due to its medicinal potential [25], which is rich in metabolites having anticancer, antimicrobial and antidiabetic potential [26]. Both the edible fruit and non-edible (peels, seeds, flowers, leaves and bark) parts of this plant have metabolites with substantial antimicrobial properties [27]. The major fraction of the fruit consists of the peel, which is mostly discarded as waste without any commercial utilization. The interesting fact is that peel extract has the highest amount of bioactive phenolic compounds such as ellagitannins, tannins [28] and anthocyanin [29, 30], including ellagic acid as well as punicalagin (2,3-hexahydroxydiphenoylgallagyl-D-glucose) [31]. Recently, pomegranate extracts were evaluated against beta-lactamase-producing drug resistance Gram-positive and Gram-negative bacteria using agar diffusion and minimum inhibitory concentration assays [27, 32].
In the current study, we compared the anti-Enterobacteriaceae activity of different solvent extracts of edible and non-edible parts of Kandhari pomegranate of Pakistan. Because of the remarkable antibacterial activity of P. granatum peel methanol extract, it was further investigated by mass spectrometric analysis that revealed punicalagin as a major constituent of pomegranate extract. Punicalagin was further explored for its bioactivity and as an antimicrobial adjuvant/potentiator efficacy in conjunction with the representatives of different classes of antimicrobials against the MDR Enterobacteriaceae.
Methods
Pomegranate peel powder
P. granatum peels (50 kg), obtained as a co-product during pomegranate juice extraction, were supplied by a local juice shop located in Jinnah Market (Faisalabad). The collected peels were then rinsed with distilled water. The peels were air-dried under ambient conditions and maintained at − 20 °C in vacuum-sealed packages. A grinder mill and sieves were used to obtain a powder particle size of less than 0.417 mm.
Pomegranate whole fruit juice, pomegranate fresh seed juice and pomegranate dried seed powder
P. granatum fruits were freshly procured from a local market and divided into two portions. From the one portion pomegranate whole fruit juice was obtained by pressure extraction of the whole fruit (15 units of fruit that weighed 8 kg). After chopping with a grinder, pomegranate pieces were ground and juice was sieved. From the other portion, the edible seeds were separated from the peels and the total weight of the arils was divided into two equal parts. Pomegranate fresh seed juice was obtained by pressure extraction of the fresh arils. While the other portion was dried under shade to get pomegranate dried seed powder. A grinder mill and sieves were used to obtain a powder particle size of less than 0.417 mm. Liquid samples were dried by a rotary evaporator. All the prepared samples were stored at − 20 °C in vacuum-sealed packages until analysis (2 months as a maximum).
Preparation of extracts
An amount of 200 g of each of the samples of pomegranate was separately blended (using a blender for 2 minutes) with solvents having an increasing polarity: 100% ethyl acetate, 80% methanol, 100% methanol, 70% ethanol, 100% ethanol, 100% water and boiling in 100% water. Dilutions for the varying concentrations were accomplished using distilled water. The samples were incubated at 37 °C for 2–8 h in a shaking incubator (Witeg Wisd shaking incubator WIS20, Germany) at 200 rpm. After this, the sample extracts were filtered with Whatman No. 1 filter paper in a Buchner funnel to remove peel particles and concentrated under reduced pressure at 40 °C in a rotary Evaporator (Heidolph, Schwabach Germany) to remove almost 90% of the solvent. It was further dried in a desiccator under a vacuum to achieve constant weight [33]. The extraction process was repeated three times to extract the maximum components from each sample. Dried extracts were dissolved in 100 and 30% liquid chromatography-mass spectrometry grade (LC-MS) methanol for MS analysis and antimicrobial assay, respectively.
Yield of extract
The yields of all extracts (extractable components) expressed on a dry weight basis were calculated from the following equation and reported as percent yield.
where W1 is the weight of the extract residue obtained after concentration and drying, whereas, W2 is the weight of the peel or pulp taken [33].
Bacterial strains
A total of 3 Gram-negative MDR clinical isolates including S. typhi, S. typhimurium and E. coli were used to screen for the antimicrobial activity of all the prepared extracts of pomegranate. All isolates used in this study were clinical, and isolated from hospitalized patients (Allied Hospital, Faisalabad, Pakistan). S. typhi and S. Typimurium were from typhoid-suspected patients and E. coli was from UTIs suspected patients, originally collected and stored by NIBGE bacterial stock culture department. All the clinical isolates were identified by staining characters and morphology; colony characters and pigmentation and reaction in triple sugar iron agar media. For molecular confirmation of the isolates, genus-specific PCR was performed using previously reported protocols [34] for Salmonella and E. coli [35]. Genomic DNA extraction was done by the chloroform-isoamyl alcohol method [36]. A highly specific stm gene fragment was selected for the identification of serovar Typhimurium [37], fliC for serovar Typhi and uidA gene for E. coli [35]. A list of the primers used in the identifications of isolates is given in Table S1. The final products were confirmed with 1.5% agarose gel electrophoresis.
Determination of the antimicrobial resistance profile of the Enterobacteriaceae strains
Antimicrobial susceptibility studies were carried out on the bacterial isolates using commercially available antimicrobial discs (Oxoid) by the Kirby Bauer disc diffusion technique. Lauria-Bartani (LB) broth (Himedia, Mumbai, India) containing 0.5 McFarland (MF) turbidity (0.14–0.17 OD600) of bacterial culture was swabbed on Mueller Hinton agar plates. Antimicrobial discs were placed on prepared plates about 20 mm apart, inhibition zone diameter was measured after 16–18 h incubation at 37 °C, and the results were interpreted as per Clinical and Laboratory Standard Institute guidelines [38]. Antimicrobial discs from seven major antimicrobial groups were included for phenotypic susceptibility testing as given in Table 1.
Mass spectrometric analysis of the crude extracts
The detailed investigation of crude extracts was completed using a mass Spectrometer (LTQ XL Linear Ion Trap, Thermo Fisher Scientific, Waltham, MA, United States), furnished with an Electrospray Ionization probe. Approximately 5 mg of the extract was dissolved in 5 mL methanol (LC-MS grade), which was further diluted 10 times with methanol. The sample after passing through the polytetrafluoroethylene filter membrane (0.45 μm) was injected into the mass spectrometer using a direct syringe pump with a flow rate of 10 μL min−1. The sample was analyzed on positive and negative ionization modes within the range of m/z 50–2000. The capillary and source voltages were tuned at 35 kV and 4.2 kV, respectively, for positive ion mode and -30 kV and − 4.5 kV, respectively, for negative ion mode. Capillary temperature (280 °C), nitrogen flow rate (25 L.min−1), and auxiliary gas flow rate (5 L min−1) were set at positive and negative ion modes for full scan and MS2. The ion peaks were further fragmented using Collision-Induced Dissociation. The MS and MS2 data were obtained and processed using Xcalibur software. The chemical structures of parent and daughter ion peaks were drawn using ChemDraw Ultra 12.0 software. The identification of compounds was confirmed by their fingerprinting fragments with reference standards and literature values. The Mass Spectrometry analysis was performed as described by Mphahlele et al. [39] and pure reference standards (Sigma-Aldrich, Germany) were used to confirm the presence or absence of ellagic acid (Sigma-Aldrich, CAS No. 476–66-4) and punicalagin (MedChem Express, Cat. No. HY-N0063, > 99.97%.
In vitro antimicrobial activity of extracts
The agar well diffusion assay, similar to that reported previously [40], was conducted to evaluate the inhibitory spectrum of the extracts and pure compounds (ellagic acid, punicalagin), selected after mass spectrometry against test microorganisms (Table 2). Freshly grown bacterial culture [70 μl) in Mueller Hinton broth was adjusted to the final inoculum density of 107 cfu/mL (by 0.5 MF), spread on agar plates and left to get dried for 30 min. The wells (6 mm in diameter) were made in media using a sterilized stainless steel borer. Each well was filled with 100 μL (700 mg/mL) of diluted extracts. The plates were left at room temperature for 30 min to allow the diffusion of materials in the media. The methanol was used as the vehicle control. Antibacterial activity was expressed as the diameters of the zone of inhibition (ZOI) produced around each well measured after incubation time. The plates were incubated at 37 °C for 16–18 hrs. The experiment was repeated three times to confirm the reproducibility of the observed data.
Determination of minimum inhibitory concentration
The MIC values of peel extract in methanol and punicalagin against clinical isolates were determined by the standard method of broth micro-dilution, to find the lowest concentration at which no visible growth of the bacteria was observed. Briefly, a two-fold serial dilution of methanol peel extract stock (700 mg/mL) was made to acquire 10 concentrations in the range of 350 to 0.6 mg/mL and punicalagin (20 mg/mL) was diluted to prepare the concentrations in the range of 10 to 0.25 μg/mL. In the 96-well microtitre plate, one row of 12 wells contained only LB (200 μL/well) as a ‘blank’, while another row contained only methanol (200 μL/well) as the ‘vehicle control’ serially diluted (with LB; v/v) to the concentration corresponding to the respective wells used for MIC determination of peel methanol extract. The broth culture containing 0.5 MF (1 × 107 cfu/mL) inoculum density was introduced to each of the wells, except the ‘sterility control lane’ (blank lane), at a 1:10 ratio to maintain a final inoculum density of 1× 107 cfu/mL. After incubation for 22 h at 37 °C, the bacterial growth was determined at 600 nm using ELISA Reader (Synergy H1 Biotek Microplate Reader). The optical density of the ‘vehicle control’ lane indicated the maximum growth of the test bacteria, while the ‘blank’ lane showing no growth served as a ‘sterility control’ for the procedure. The MIC value is defined as the lowest concentration of the compound that will inhibit the visible growth of a microorganism after overnight incubation [41].
Determination of antibacterial synergy of antibiotics with punicalagin by agar disc diffusion assay
Agar disc diffusion assay was used for initial combination experiments against three clinical strains S. typhi, S. typhimurium and E. coli. Mueller Hinton agar plates were prepared by spreading the bacterial growth of 0.5 MF using cotton swabs dipped in the 0.5 MF followed by the placement of antimicrobial discs. Punicalagin stock solutions of 20 mg/mL were prepared and applied on antimicrobial discs at sub-inhibitory concentrations of 30 μg/antimicrobial disc, 100 μg/antimicrobial disc, and 500 μg/antimicrobial disc. Overnight incubation of 37 °C followed by ZOI measurement and percentage (%) increase in inhibition zone was calculated as (b2-a2)/a2 × 100, where “a” is the inhibition zone of antibiotic alone and “b” is the antibiotic plus punicalagin zone. A combination assay was performed in triplicate and the standard deviation was calculated. All values are expressed as the mean standard error (±) of the mean of triplicate values of the same replicate [42]. Statistical comparisons on combination effects by disc diffusion method were performed using a Student‘s t-test by Tukey posthoc test. A P-value of < 0.05 was considered statistically significant. The synergistic combinations resulting in > 30% inhibition were confirmed by plotting the time-kill curve [43].
Results
Extraction yield
The average yields of all extracts obtained with different solvents are given in Table 2 and Fig. 1. For pomegranate peel extraction, the total yield was higher in 80% ethanol (11.5%) than in any used concentrations of methanol, ethyl acetate and water (Table 2, Sr. 1–7). For dry seed extraction, the highest (15.3%) and the lowest yields (1.66%) were obtained with 80% methanol and 100% ethyl acetate, respectively (Table 2, Sr. 8–14). Pomegranate whole fruit juice extract gave a yield between the range of 0.51% with ethyl acetate to 10.3% with 80% methanol (Table 2, Sr. 15–21) and 0.73% with ethyl acetate to 19.2% with 80% ethanol for the fresh seed extract (Table 2, Sr. 21–28).
Comparative yields of pomegranate extracts in different solvents. (A) Pomegranate peel powder extract, (B) Pomegranate dried seed powder extract, (C) Pomegranate whole fruit juice extract, and (D) Pomegranate fresh seed juice extract. 100 M: 100% methanol, 80 M: 80% methanol, 100E: 100% ethanol, 70E: 70% ethanol, 100EA: 100% ethyl acetate, DW: distilled water, BDW: distilled water with boiling
Biochemical and molecular confirmation of clinical isolates
Clinical isolates taken from NIBGE stock cultures were confirmed by Gram staining resulting in small red Gram-negative rods visible in microscopic view. A characteristic yellow butt of the test tube with a pink slant showing a black center due to H2S production in the Tryptic soy agar slant was a typical confirmation of Salmonella spp. Lactose fermenting (pink) colonies on MacCkonkey agar and yellow slant and yellow butt with gas formation but no H2S in the TSI agar slant was characteristic of E. coli.
Molecular confirmation of genus Salmonella was done using invA gene fragment (284 bp amplification), and the serovars were confirmed by targeting gene fragments: stm (401 bp amplification) for S. typhimurium, fliC (495 bp amplification) for S. typhi and uidA (486 bp amplification) for E. coli. All oligonucleotides used for confirmation are given in (supplementary materials, Table S1).
Antibiotic resistance profiling
The isolates resistant to at least three different classes of antibiotics were considered as MDR. The resistance profile of each isolate is compiled in (Table 1). All clinical isolates used in this study were found to be MDR based on their antibiotic resistance profiles. The ciprofloxacin-resistant E. coli and S. typhimurium and ceftriaxone-resistant S. typhi were proceeded for further evaluation of synergy interaction of resistant antibiotics with most active peel methanol extract.
Mass spectrometric analysis of pomegranate extract
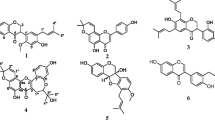
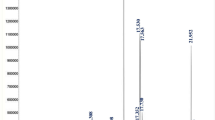
The ESI-MSn method was used to identify the predominant compounds in crude extracts. The full scan mass spectrum of pomegranate peel methanol extract at negative ion mode (m/z 100–1500) showed the presence of molecular ions [M-H]− of quinic acid (m/z 191, 100% abundance), ellagic acid (m/z 301, 14% abundance), cryptochlorogenic acid (m/z 353, 10% abundance), ellagic acid pentoside (m/z 433, 26% abundance), ellagic acid hexoside (m/z 463, 1.5% abundance), a fragment of pedunculagin m/z 481, 20% abundance), digalloyl-glucose isomer (m/z 483, 9% abundance), Pedunculagin (m/z 783, 15% abundance) and punicalagin (m/z 1083, 38% abundance) (Fig. 2).
The molecular ion peak of quinic acid (m/z 191) was subjected to MS2 fragmentation to generate daughter ion peaks for comprehensive analysis (Supplementary Materials, Fig. S1A). A fragmented peak with m/z 173 was produced by the removal of the H2O molecule from which further ion peaks were generated at m/z 129 and m/z 155 by the loss of CO2 and H2O molecules, respectively. The subsequent fragmentation of the ion at m/z 155 yielded a base ion peak at m/z 111 with approximately 100% relative abundance by the loss of CO2. The molecular ion peak of ellagic acid (m/z 301) generated two prominent ion peaks at m/z 283 and m/z 257 after losing one molecule of H2O and one molecule of CO2, respectively (Supplementary Materials, Fig. S1B). The peak with m/z 257 further split into the fragment ions at m/z 213 and m/z 229 with the removal of CO2 and subsequent H2O. Cryptochlorogenic acid at (m/z 353) generated three daughter ions at m/z 293, m/z 265, and m/z 247 with the loss of CO2, CO and H2O molecules, respectively (Supplementary Materials, Fig. S1C). Ellagic acid pentoside (m/z 433) fragmented into two daughter ions with m/z of 301 (ellagic acid) and 153 (Supplementary Materials, Fig. S1D). Ellagic acid hexoside (m/z 463) showed the most abundant fragment ion at m/z 301 by the loss of hexoside sugar (Supplementary Materials, Fig. S1E). The fragment of HHDP-Galloy glucose showed a molecular ion peak at m/z 481 that further fragmented into the ions at m/z 301 (ellagic acid) by losing glucose molecule and at m/z 275 by losing CO from ellagic acid, respectively (Supplementary Materials, Fig. S1F). The fragment ion peak at m/z 463 was also observed by the loss of H2O molecule from the fragment of pedunculagin.
A digalloyl-glucose isomer was characterized by a molecular ion [M-H]− at m/z 483 that fragmented into daughter ions at m/z 451, m/z 465 and m/z 439 representing [M-H-O2]−, [M-H-H2O]− and [M-H-CO2]−, respectively, and also at m/z 331 and m/z 169 (Supplementary Materials, Fig. S1G). The fragment at m/z 331 further lost an H2O molecule generating an ion m/z 313. A pair of fragments attributed to cross-ring fragmentation appeared at m/z 271 and m/z 241. The molecular ion of pedunculagin at m/z 783 showed two peaks of dissociated ions at m/z 765 and m/z 481 and one ion peak at m/z 633 with ring removal. A couple of other fragment peaks appeared at m/z 301 and m/z 275 in this spectrum (Supplementary Materials, Fig. S1H).
The molecular ion of punicalagin [M-H]− appeared at m/z 1083 that dissociated into the ion peak at m/z 1065 corresponding to [M-H-H2O]− (Supplementary Material, Fig. S1I). The peak at m/z 1065 split into another fragment at m/z 763 showing the loss of the ellagic acid part that further generated the peak at m/z 721 characterized by the concomitant loss of CO2. The punicalagin molecular ion peak also showed the fragmentation peaks at m/z 781, m/z 601 and m/z 575.
Comparative evaluation of the antibacterial activity of pomegranate extracts and pure compounds against drug-resistant clinical isolates
The antimicrobial activity of crude pomegranate extracts and pure compounds, evaluated by agar well diffusion assay, against selected strains is given in Table 2. It was evident from the results that pomegranate peel methanol extract exhibited the largest ZOI in comparison to all other extracts against S. typhi, S. typhimurium and E. coli followed by crude 70% ethanolic extract of pomegranate peel while S. typhi and E. coli showed equal sensitivity to the same concentration of pomegranate peel methanol extract, and S. typhimurium was found to be more resistant for the same concentration (Table 2, Serial No. 2, Fig. 3).
Growth inhibition zones of pomegranate peel methanol extract against MDR Enterobacteriaceae clinical isolates. A Growth inhibition zone (18 ± 1 mm) against S. typhimurium produced by pomegranate peel methanol extract (700 mg/mL) on Mueller Hinton agar plate, B Growth inhibition zone against S. typhi (20 ± 1 mm) pomegranate peel methanol extract (700 mg/mL) on Mueller Hinton agar plate, C Growth inhibition zone (20 ± 1 mm) against E. coli produced by pomegranate peel methanol extract (700 mg/mL) on Mueller Hinton agar plate
The most satisfactory results of pomegranate dried seed extract were also recorded with 80% methanol extract but the largest inhibition zone appeared against S. typhimurium (Table 2, Serial No. 9).
The trend was followed by pomegranate whole fruit juice methanol extract (Table 2, Serial No. 16) and pomegranate fresh seed methanol extract (Table 2, Serial No. 23), which demonstrated better antibacterial activity as compared to other solvents.
All the extracting solvents other than 80% methanol showed approximately equal inhibition zones against all pathogenic strains that were lower than inhibition zones produced by 80% methanol extracts (Table 2). It means that hydroalcoholic solvent systems are the best for the extraction of bioactive secondary metabolites of pomegranate.
The overall inhibitory activity of pomegranate extracts against Enterobacteriaceae spp. observed in the current study followed the trend as 80% methanol > 70% ethanol > 100% methanol > 100% ethanol > distilled water with boiling > distilled water at room temperature > ethyl acetate. While among two of the tested pure compounds (ellagic acid and punicalagin), only punicalagin was found to be active showing hazy inhibition zones against MDR pathogens in well diffusion assay (Table 2, Serial No. 29–30, Fig. 4) and selected for further investigation.
Growth inhibition zones of punicalagin against MDR Enterobacteriaceae clinical isolates. A Growth inhibition zone (17 mm, hazy) against S. typhi produced by punicalagin (20 mg/mL) on Mueller Hinton agar plate, B Growth inhibition zone against S. typhimurium (14 mm, hazy) produced by punicalagin (20 mg/mL) on Mueller Hinton agar plate, C Growth inhibition zone (13 mm, hazy) against E. coli produced by punicalagin (20 mg/mL) on Mueller Hinton agar plate
Determination of minimum inhibitory concentration and % inhibition
Minimum inhibitory concentration was evaluated by broth dilution assay in 96 well plates according to Clinical and Laboratory Standards Institute guidelines 2021 [38], which resulted in MIC values ranging from 3.9–7.8 mg/mL for pomegranate peel methanol extract against all the tested clinical strains while surprisingly punicalagin was unable to show MIC value even at a concentration of 10 mg/mL (Table 3). This is why three minimum sub-inhibitory concentrations of punicalagin were chosen to determine the efficacy to potentiate the drugs. Although further investigations, i.e., synergistic disc diffusion assay and growth curve assay revealed the bacteriostatic nature of punicalagin.
In vitro activity evaluation of punicalagin combined with antibiotics by disc diffusion assay proved to be less laborious and easy to interpret with minimum error chances due to repetitive experiments. The combination effects of sub-inhibitory concentrations of punicalagin with the representatives of different classes of antimicrobials against MDR Enterobacteriaceae clinical isolates are given in Fig. 5. Sub-inhibitory concentrations of punicalagin as 30 μg, 100 μg and 500 μg per minimum inhibitory concentrations of antibiotics were used to evaluate the combination effects against all the tested isolates (Table 4). Sulfamethoxazole/Trimethoprim 23/1.25 μg showed no synergism with all tested concentrations of punicalagin against S. typhimurium and E.coli but combining with 500 μg of punicalagin increased the inhibition area to 63.8% against S. typhi (Table 4, Serial No. 1, Fig. S2). Nalidixic acid 30 μg demonstrated no augmenting efficacy with 30, 100 and 500 μg punicalagin for all three tested clinical isolates (Table 4, Serial No. 2). Combination of ampicillin 10 μg with 30 μg of punicalagin increases the inhibition fold area to 9.9% for S. typhimurium while further increment of punicalagin to 100 μg showed less augmenting potential (6.5%). Surprisingly 500 μg showed 39% increase in growth inohibition fold area for S. typhimurium (Table 4, Serial No. 3). For S. typhi 30 μg/10 μg ampicillin showed no synergism and highest combination activity of 73% was seen at the concentration of 100 μg/10 μg ampicillin (Table 4, Serial No.3, Fig. 6A), while 500 μg/10 μg ampicillin enhances the % inhibition fold area to only 9.4% (Table 4, Serial No. 3). However, the combinations ampicillin 10 μg/30, 100, 500 μg punicalagin remained indifferent for E. coli (Table 4, Serial No.3). Chloramphenicol 30 μg showed no synergistic growth inhibition with 30 μg of punicalagin but further concentrating punicalagin to 100 and 500 μg demonstrated synergism by increasing the fold area to 9.7 and 3.4% respectively for S. typhimurium (Table 4, Serial No.4). For S. typhi only the combination 100 μg punicalagin/chloramphenicol 30 μg showed 26% increase in inhibition fold area while 30 and 500 μg of punicalagin with 30 μg of chloramphenicol was proved in effective combinations to increase the inhibiting efficacy (Table 4, Serial No.4).
Combination effects of sub-inhibitory concentrations of punicalagin with the representatives of different classes of antimicrobials against MDR Enterobacteriaceae clinical isolates. A % increase in zone of inhibition resulted in a combination of 30 μg punicalagin/antimicrobial disc, 100 μg punicalagin/antimicrobial disc and 500 μg punicalagin/antimicrobial disc against S. typhimurium by agar disc diffusion assay, B % increase in zone of inhibition resulted in a combination of 30 μg punicalagin /antimicrobial disc, 100 μg punicalagin/antimicrobial disc and 500 μg punicalagin/antimicrobial disc against S. typhi by agar disc diffusion assay, C % increase in zone of inhibition resulted in a combination of 30 μg punicalagin/antimicrobial disc, 100 μg punicalagin/antimicrobial disc and 500 μg punicalagin/antimicrobial disc against E. coli by agar disc diffusion assay
Combination effect of punicalagin with antimicrobials against S. typhi, (A) Combination effect of punicalagin with ampicillin (Amp-10) against MDR S. typhi, (i) 100 μg of punicalagin showing no inhibition zone, (ii) Inhibition zone produced by ampicillin without punicalagin, (iii) Synergistic inhibition zone produced by 100 μg punicalagin with ampicillin showing 73% increase in fold area, (iv) Synergistic Inhibition zone produced by 500 μg punicalagin with ampicillin showing 26% in fold area, (B) Combination effect of punicalagin with aztreonam (ATM-30) against MDR S. typhi, (i) Inhibition zone produced by aztreonam without punicalagin, (ii) Synergistic inhibition zone produced by 100 μg punicalagin with aztreonam showing 35% increase in fold area, (iii) Synergistic inhibition zone produced by 500 μg punicalagin with aztronam showing 47% increase in fold area, (iv) Ciprofloxacin inhibition zone as positive control, (C) Combination effect of punicalagin with amoxicillin clavulanic acid (AMC-30) against MDR S. typhi, (i) Inhibition zone produced by amoxicillin clavulanic acid without punicalagin, (ii) Synergistic Inhibition zone produced by amoxicillin clavulanic acid with 30 μg punicalagin showing 54% increase in fold area, (iii) Indifferent Inhibition zone produced by amoxicillin clavulanic acid with 100 μg punicalagin showing 0% increase in fold area, (iv) Ciprofloxacin inhibition zone as positive control, (D) Combination effect of punicalagin with ceftriaxone (CRO-30) against MDR S. typhi, (i) 500 μg of punicalagin showing no inhibition zone, (ii) Inhibition zone produced by ceftriaxone without punicalagin, (iii) Synergistic inhibition zone produced by 500 μg punicalagin with ceftriaxone showing 47% increase in fold area, (iv) Methanol showing no inhibition zone as negative control
In case of S. typhimurium combining punicalagin at a sub-inhibitory concentration of 30 μg, the antibacterial efficacy of 30 μg of aztreonam was enhanced by 62%, and by further increasing the punicalagin to 100 μg and 500 μg, only showed 31 and 34% aztreonam augmenting efficacy (Table 4, Serial No. 5, Fig. S3). While for S. typhi, the combinations of 30 μg aztreonam /30, and 100 μg of punicalagin showed approximately equal inhibiting efficacy (Table 4, Serial No. 5, Fig. 6B). In case of E. coli, 30 μg and 100 μg punicalagin/30 μg aztreonam demonstrated 26 and 31% synergistic combinations, respectively. However, the 500 μg punicalagin/30 μg aztreonam combination proved to be less efficient with only 4% of synergism efficacy (Table 4, Serial No.5). The combination of 30 μg amoxicillin clavulanic acid/30 μg of punicalagin showed 14% antimicrobial augmenting potential for S. typhimurium but 30 g amoxicillin clavulanic acid/100 and 500 μg of punicalagin just showed 4.9% increment in the growth-inhibiting area (Table 4, Serial No. 6). For S. typhi punicalagin 30 μg and 500 μg demonstrated 54 and 7.3% amoxicillin clavulanic acid augmenting potential but 100 μg of punicalagin with 30 μg amoxicillin clavulanic acid remain indifferent combination against S. typhi (Table 4, Serial No. 6, Fig. 6C). However, 30 and 100 μg of punicalagin /30 μg amoxicillin clavulanic acid combination showed no effect on growth inhibiting area but 500 μg of punicalagin decreases the antimicrobial efficacy of 30 μg of amoxicillin clavulanic acid against E. coli Table 4, Serial No. 6). Gentamicin 10 μg/ 30 μg punicalagin, the only combination that was ineffective against S. typhimurium while all other tested combinations of gentamicin 10 μg/ 30, 100 and 500 μg punicalagin against all of three clinical strains demonstrated antagonism by decreasing the growth inhibiting area (Table 4, Serial No. 7). Ceftriaxone 30 μg with punicalagin at concentration of 30 μg was ineffective combination for S. typhimurium while the combinations 30 μg ceftriaxone/100, 500-μg punicalagin was synergistic with the increase in growth inhibiting area by 24 and 22% (Table 4, Serial No. 8). The clinical strain S. typhi followed the same trend as 30 μg ceftriaxone/ 30 μg punicalagin showed no effect in growth inhibiting area but the combinations 30 μg ceftriaxone with 100 μg and 500 μg of punicalagin demonstrated synergism by increasing growth inhibiting zone by 11 and 47% (Table 4, Serial No. 8, Fig. 6D). However, E. coli was strongly inhibited by 55% with the synergistic combination of 30 μg ceftriaxone/ 30 μg punicalagin. The percentage synergistic inhibition (32%) decreased by increasing the punicalagin concentration to 100 μg while increasing the punicalagin concentration to 500 μg diminished the synergistic behavior (Table 4, Serial No. 8) at a concentration of 500 μg/30 μg ceftriaxone disc further enhanced the activity of ceftriaxone from 12 to 47% (Table 4, Serial No.8). The most antagonistic combination was observed with ciprofloxacin 5 μg/ 30, 100,500 μg punicalagin against all of three selected clinical strains (Table 4, Serial No.9).
The comparison of % increase or decrease in antibiotics activity is given in (Fig. 6, A-C). The synergistic efficacy of sub-inhibitory concentrations of punicalagin and antibiotics (previously observed by agar disc diffusion assay) were further evaluated by time-dependent growth curve assay. For plotting the time-response curves, the growth of S. typhi, S. typhimurium and E. coli cells in the presence of sub-inhibitory concentrations of punicalagin and sub-inhibitory concentrations of antimicrobials in combination and alone were monitored. OD600 was measured after an interval of 1 hour and up to 12 hours at 37 °C. Time-kill curves confirmed the bacteriostatic behaviour of punicalagin against exposed bacterial cells at sub-inhibitory concentrations. It was found that all the clinical strains in the panel showed less growth subjected to the simultaneous administration of sub-inhibitory concentrations of punicalagin and antimicrobials, compared with punicalagin and antibiotics alone. Moreover, no superimposition of graphs was noted at any point of data collection (Figs, 7, 8 and 9). The combination of Ampicillin/ punicalagin against S. typhi demonstrated the highest synergy while chloramphenicol/punicalagin against S. typhimurium proved to be the lowest synergistic combination.
Comparative growth curves representing the drugs augmenting efficacy of punicalagin against S. typhimurium. A Time kill curve of S. typhimurium for ampicillin with and without punicalagin. Blue: Growth control no ampicillin/punicalagin; Red: punicalagin (500 μg/mL); Grey: Sub-inhibitory concentration of ampicillin (0.3 μg/mL); Yellow: Sub-inhibitory concentration of ampicillin (0.3 μg/mL) with punicalagin (500 μg/mL), (B) Time kill curves of S. typhimurium for aztreonam with and without punicalagin. Blue: Growth control, no aztreonam/punicalagin; Red: punicalagin (30 μg/mL); Grey: Sub-inhibitory concentration of aztreonam (0.05 μg/mL); Yellow sub-inhibitory concentration of aztreonam (0.05 μg/mL) with punicalagin (30 μg/mL)
Comparative growth curves representing the drugs augmenting efficacy of punicalagin against S. typhi. A Time kill curves of S. typhi for Aztreonam with and without punicalagin. Blue: Growth control, no aztreonam/punicalagin; Red: punicalagin (30 μg/mL); Grey: Sub-inhibitory concentration of aztreonam (3.75 μg/mL); Yellow: Sub-inhibitory concentration of ATM (3.75 μg/mL) with punicalagin (30 μg/mL), (B) Time kill curves of S. typhi for amoxicillin clavulanic acid with and without punicalagin. Blue: Growth control, no amoxicillin clavulanic acid/punicalagin; Red; punicalagin (30 μg/mL); Grey: Sub-inhibitory concentration of amoxicillin clavulanic a (1.8 μg/mL); Yellow: sub-inhibitory concentration of amoxicillin clavulanic acid (1.8 μg/mL) with punicalagin (30 μg/mL), (C) Time kill curves of S. typhi for ampicillin with and without punicalagin. Blue: Growth control, no ampicillin/punicalagin; Red: punicalagin (100 μg/mL); Grey: Sub-inhibitory concentration of ampicillin (0.3 μg/mL); Yellow: sub-inhibitory concentration of ampicillin (0.3 μg/mL) with punicalagin (100 μg/mL), (D) Time kill curves of S. typhi for ceftriaxone with and without punicalagin. Blue: Growth control, no ceftriaxone/punicalagin; Red: punicalagin (500 μg/mL); Grey: Sub-inhibitory concentration of ceftriaxone (3.75 μg/mL); Yellow: sub-inhibitory concentration of ceftriaxone (3.75 μg/mL) with punicalagin (500 μg/mL)
Comparative growth curves representing the drugs augmenting efficacy of punicalagin against E. coli, (A) Time kill curves of E. coli for ceftriaxone with and without punicalagin. Blue: Growth control, no ceftriaxone/punicalagin; Red: punicalagin (30 μg/mL); Grey: Sub-inhibitory concentration of ceftriaxone (60 μg/mL); Yellow: sub-inhibitory concentration of ceftriaxone (60 μg/mL) with sub-inhibitory concentration of punicalagin (30 μg/mL), (B) Time kill curves of E. coli for aztreonam with and without punicalagin. Blue: Growth control, no aztreonam/punicalagin; Red: punicalagin (15 μg/mL); Grey: Sub-inhibitory concentration of aztreonam (15 μg/mL); yellow: Sub-inhibitory concentration of aztreonam (15 μg/mL) with a sub-inhibitory concentration of punicalagin (100 μg/mL)
Discussion
The selection of appropriate solvents for extraction plays a significant role in obtaining an acceptable yield of required compounds with good antimicrobial activity, which directly correlates with the polarity of solvents [44]. Extraction in 100% (v/v) concentration led to a less yield of plant metabolites, whereas a better yield was observed using a concentration of 70–80% (v/v) regardless of the solvent [44, 45]. Moreover, higher extraction yield does not correlate with high antimicrobial and antioxidant activity as it depends upon the extraction weightage of active compounds [46] also observed in this study that 80% pomegranate peel methanol extract was found antimicrobial with the highest activity against the tested clinical strains (Table 2). It has been observed that Gram-negative bacteria were more sensitive toward methanol peel extract than water extracts [47]. Moreover, a strong positive correlation was observed between the antibacterial efficacy of the 80% methanol pomegranate peel extracts with their calculated phenolic contents suggesting a higher extent of its bioactivity in polar solvents [48,49,50].
The inhibition zones against E. coli, S. typhi and S. typhimurium in our study were comparable to those of earlier studies, although the active concentrations (700 mg/mL stock solution, 100 μL/ well, 7000 μg/well) vary from the previously reported concentrations that were 800 μg/well – 12 mg/mL in earlier investigations [47, 51]. The difference in the activity of pomegranate extract among various studies could be explained based on the phenolic contents of the prepared extracts and pathogenic strain sensitivity [52]. Water extract and boiled water extracts both possessed only a weak activity or hazy zones against all tested bacteria at 12 h that disappeared upon prolonged incubation for 24–48 h. The disappearance of hazy zones and small zones may indicate that water extracts have a low activity or bacteriostatic nature due to the factor that the desired inhibition of the physiological processes of the microbes is overcome by pathogenic microbes upon prolonged exposure. Interestingly, ethyl acetate extracts were inactive for all tested organisms. These results are supported by the previous reports that plant extracts with non-polar solvents e.g., ethyl acetate, n-hexane and chloroform were inactive against pathogenic strains, making hydrophilic extractants an excellent choice for extracting bioactive polyphenolic constituents [49, 50, 52, 53].
Over the last 20 years, many studies reported the anti-Enterobacteriaceae efficacy of P. granatum extracts as have been compared in Table 5. Some comprehensive studies evaluated the anti-Salmonella activity of P. granatum peels, including against S. typhi and S. typhimurium, but the antibiotic resistance profile of Salmonella spp. was not determined (Table 5, Serial No.2,3,6,10,13), which have been pursued in the current study. In another study, non-probioticated as well as probioticated P. granatum juice was shown to be active against non-MDR S. typhi and S. typhimrium (Table 5, Serial No.7). Anti-E. coli efficacy of P. garanatm crude extracts has been studied more rigorously than that of anti-Salmonella spp. Hydro-alcoholic extracts of P. granatum peel, juice, seeds and whole fruit showed good antimicrobial activity against E.coli, but mostly these studies had not determined the antibiotic resistance profile of used E. coli strains (Table 5, Serial No.1,4-7,10,11,13–15). Only a few studies considered the MDR strains of E. coli (Table 5, Serial No.18) evaluating the antimicrobial efficacy of P. granatum leaves only but in our study, the antimicrobial activity of all fruit parts of P. garanatum was compared against MDR E. coli strains showing resistance against third-generation cephalosporins and fluoroquinolones.
Several studies reported MICs of the hydroalcoholic peel extracts of pomegranate ranging from 0.39 to 50 mg/mL against E. coli and 0.25 to 50 mg/mL for Salmonella spp. supporting the results of the current study [47, 53, 57, 67]. The findings of the broth dilution assay revealed the values of MIC for pomegranate peel methanol extract were lower than those reported previously: 50 mg/mL for both E. coli and Salmonella spp. [63] while higher than those reported by Al-Zoreky as 1 mg/mL for E. coli and 4 mg/mL for Salmonella Enteritidis ATCC 4931 [51]. A range in the minimum inhibitory concentrations of pomegranate extracts among various studies could be explained based on different extraction conditions leading to the difference in MICs as E. coli MIC values range from 62.5–625 mg/mL with the change in extraction method [68]. Moreover, the fruit variety with its phenolic contents and targeted pathogenic strain sensitivity has a direct impact on inhibiting the efficacy of the prepared extracts [51, 52, 69].
The origin of fluoroquinolone resistance is predominantly the chromosomal mutations involving the modifications in target sites and variations in efflux pump expression rendering both processes the primary culprits of enhanced resistance in microbes [70]. E. coli has been reported to exhibit multidrug resistance because the AcrAB-TolC efflux system uses fluoroquinolone as the substrate [71]. Another study proposed a positive correlation between AcrA efflux system expression and enhanced resistance to ciprofloxacin [72]. Subsequently, natural bioactive polyphenolic compounds were evaluated and have been reported to act as efflux pump inhibitors leading to synergistically reversing the resistant nature of the microbes against the drugs [73]. Initially, it was reported that crude extract of pomegranate peels may be an efflux inhibitor [74]. In contrast, Anam et al., 2019 proved that pomegranate peel methanol extract showed no efflux pump inhibitory activity against S. typhi [75].. While the methanol extract of pomegranate serves as an efflux inhibitor in Gram-positive bacteria e.g., S. aureus RN-7044 as reported by Braga et al. [76].
Punicalagin and ellagic acid were reported as the major bioactive phenolic compounds in pomegranate peel powder [77,78,79]. However, in our study, punicalagin only showed hazy inhibition zones against targeted isolates which had been reduced upon prolonged incubation time but ellagic acid could not exert any inhibition zone, and was not active against the tested Enterobacteriaceae strains. Based on its antibacterial activity, punicalagin was selected for further evaluation of its co-activity with conventional antimicrobials against selected pathogens because a single chemical compound as a drug augmenting agent is preferable for further drug formulation rather than a crude herbal extract.
Punicalagin was the bioactive ellagitannin, detected by LCMS/MS in pomegranate peel methanol extract, that showed antimicrobial activity against all isolates as observed by agar well diffusion assay (Table 2, Serial No. 30, Fig. 4). However, the findings of MIC and growth curve assays demonstrated that punicalagin alone up to 10 mg/mL was unable to completely inhibit the growth of targeted bacteria in liquid cultures. Although the used dose significantly restricted the rate of reproduction of microbial cells or slow down the required microbiological process for normal growth at a certain level, albeit at a concentration higher than 10 mg/mL (Figs. 7, 8 and 9). In earlier studies, punicalagin has been reported to downregulate the quorum-sensing genes in Salmonella spp. at sub-inhibitory concentrations [80, 81] supporting the reduction of the total cell number of targeted pathogens due to compromised communication in the presence of punicalagin observed in this study. Punicalagin reduced the motility of S. typhimurium by affecting the flagellum-associated genes. The bacteriostatic efficacy of punicalagin may be attributed to reduced motility. As it was already proved that many plant extracts accede the motility reduction efficacy [82]. Moreover, the MDR pathogens may require a very high dose of punicalagin for bactericidal effects because of structural and genetic changes induced by mutations causing drug resistance. The MICs of punicalagin against non-MDR Salmonella spp. strains were observed in the range of 250–1000 μg/mL [81].
Although, in our study, punicalagin only disrupted the normal growth rate up to 10 mg/mL, it proved to be a powerful, concentration-dependent, sensitizing agent in combination with the tested drugs depending upon the specific bacteria.
Punicalagin enhances the efficiency of oxacillin against methicillin-resistant S. aureus as evaluated by checkerboard assay. Punicalagin has been reported to be a good potentiator to increase the efficacy of cefotaxime and oxacillin against Gram-positive bacteria by interfering with bacterial transcription mechanisms and as a virulence inhibitor [83, 84]. Whereas the Gram-negative bacteria possess an outer plasma membrane as a complex diffusional barrier, which can exert an additional resistance for many conventional drugs, making Gram-negative bacteria notably less sensitive as compared to Gram-positive bacteria. However, punicalagin has been reported to destabilize bacterial membranes, so membrane damage would likely allow greater absorption of antibiotics to toxic levels. Moreover, compromised efflux pumping causes lethal interactions making bacterial cells more sensitive to drugs that accelerate bacterial cell death [80, 85]. The sub-inhibitory concentrations of punicalagin were reported to decrease the S. typhimurium swarming ability and virulence factor expression as well. One of the noticeable characteristics of punicalagin is that it targets the AHL-dependent QS system directly involving its virulence, invasion and pathogenicity.
Conclusions
In the current study, we have demonstrated that Pakistan-originated Kandhari pomegranate peel methanol extract exhibited antibacterial activity against all tested MDR clinical isolates. The results of ESI-MS/MS analysis together with antimicrobial assays revealed that a flavonoid, punicalagin, which is abundantly present in active pomegranate peel methanol extract could be an effective antimicrobial potentiating agent against resistant strains of Enterobacteriaceae. It showed antimicrobial sensitizing capabilities in a concentration-dependent manner when combined with the antimicrobials against the resistant strains. Our experimental data strongly suggest that drug boosting combinations are significant candidates for animal model testing and punicalagin, and may be explored in combination with currently available antimicrobials against highly resistant strains of Enterobacteriaceae. Moreover, there is a need of investigating the exact antimicrobial sensitizing mechanism of punicalagin.
Availability of data and materials
All the important data generated or analysed during this study are included in this published article and its supplementary information files. Any additional data, if required, will be available from the corresponding author on request.
Abbreviations
- NIBGE-C:
-
National Institute for Biotechnology and Genetic Engineering College
- PIEAS:
-
Pakistan Institute of Engineering and Applied Sciences
- MDR:
-
Multidrug resistance
- MIC:
-
Minimum inhibitory concentration
- ESI:
-
Electrospray ionization
- PCR:
-
Polymerase chain reaction
- DNA:
-
Deoxyribonucleic acid
- LB:
-
Lauria-Bertani
- MF:
-
McFarland
- LC-MS:
-
Liquid chromatography-mass spectrometry
- PTFE:
-
Polytetrafluoroethylene
- HCl:
-
Hydrochloric acid
- ELISA:
-
Enzyme-linked immunoassay
References
Abrar S, Hussain S, Khan RA, Ul Ain N, Haider H, Riaz S. Prevalence of extended-spectrum-β-lactamase-producing Enterobacteriaceae: first systematic meta-analysis report from Pakistan. Antimicrob Resist Infect. 2018;7(1):1–11.
Kang CI, Song JH. Antimicrobial resistance in Asia: current epidemiology and clinical implications. Infect Chemother. 2013;45(1):22–31.
Apanga PA, Ahmed J, Tanner W, Starcevich K, VanDerslice JA, Rehman U, et al. Carbapenem-resistant Enterobacteriaceae in sink drains of 40 healthcare facilities in Sindh, Pakistan: A cross-sectional study. PLoS One. 2022;17(2):e0263297.
Hadjadj L, Syed MA, Abbasi SA, Rolain J-M, Jamil B. Diversity of carbapenem resistance mechanisms in clinical gram-negative bacteria in Pakistan. Microb Drug Resist. 2021;27(6):760–7.
Qamar FN, Yousafzai MT, Khalid M, Kazi AM, Lohana H, Karim S, et al. Outbreak investigation of ceftriaxone-resistant Salmonella enterica serotype Typhi and its risk factors among the general population in Hyderabad, Pakistan: a matched case-control study. Lancet Infect Dis. 2018;18(12):1368–76.
Abrar S, Ain NU, Liaqat H, Hussain S, Rasheed F, Riaz S. Distribution of Bla CTX− M, bla TEM, Bla SHV and Bla OXA genes in extended-spectrum-β-lactamase-producing clinical isolates: A three-year multi-center study from Lahore. Pakistan Antimicrob Resist Infect. 2019;8(1):1–10.
Salehi B, Abu-Darwish MS, Tarawneh AH, Cabral C, Gadetskaya AV, Salgueiro L, et al. Antimicrobial resistance collaborators global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629–55.
Bayode MT, Olalemi AO, Oladejo BO. Multiple antibiotic resistant index and detection of qnrS and qnrB genes in bacterial consortium of urine samples from clinical settings. Eur J Biol Res. 2021;11(1):45–56.
Park SH, Byun JH, Choi SM, Lee DG, Kim SH, Kwon JC, et al. Molecular epidemiology of extended-spectrum beta-lactamase-producing Escherichia coli in the community and hospital in Korea: emergence of ST131 producing CTX-M-15. BMC Infect Dis. 2012;12(1):149.
Raji MA, Jamal W, Ojemeh O, Rotimi VO. Sequence analysis of genes mediating extended-spectrum beta-lactamase (ESBL) production in isolates of Enterobacteriaceae in a Lagos teaching hospital, Nigeria. BMC Infect Dis. 2015;15(1):259.
Bilal H, Khan MN, Rehman T, Hameed MF, Yang X. Antibiotic resistance in Pakistan: a systematic review of past decade. BMC Infect Dis. 2021;21(1):244.
Bidell MR, Palchak M, Mohr J, Lodise TP. Fluoroquinolone and third-generation-cephalosporin resistance among hospitalized patients with urinary tract infections due to Escherichia coli: do rates vary by hospital characteristics and geographic region? Antimicrob Agents Chemother. 2016;60(5):3170–3.
Bhan MK, Bahl R, Bhatnagar S. Typhoid and paratyphoid fever. Lancet. 2005;366(9487):749–62.
Karkey A, Thwaites GE, Baker S. The evolution of antimicrobial resistance in Salmonella Typhi. Curr Opin Gastroenterol. 2018;34(1):25–30.
Al Kraiem AA, Yang G, Al Kraiem F, Chen T. Challenges associated with ceftriaxone resistance in Salmonella. Front Life Sci. 2018;11(1):26–34.
Kim JH, Mogasale V, Im J, Ramani E, Marks F. Updated estimates of typhoid fever burden in sub-Saharan Africa. Lancet Glob Health. 2017;5(10):969.
Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O'Brien SJ, et al. The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis. 2010;50(6):882–9.
Antunes P, Mourao J, Campos J, Peixe L. Salmonellosis: the role of poultry meat. Clin Microbiol Infect. 2016;22(2):110–21.
Nakatsuchi A, Inagaki M, Sugiyama M, Usui M, Asai T. Association of Salmonella Serotypes with quinolone resistance in broilers. Food Saf (Tokyo). 2018;6(4):156–9.
Wajid M, Awan AB, Saleemi MK, Weinreich J, Schierack P, Sarwar Y, et al. Multiple drug resistance and virulence profiling of Salmonella enterica Serovars typhimurium and Enteritidis from poultry farms of Faisalabad. Pakistan Microb Drug Resist. 2019;25(1):133–42.
Khameneh B, Diab R, Ghazvini K, Bazzaz BSF. Breakthroughs in bacterial resistance mechanisms and the potential ways to combat them. Microb Pathog. 2016;95(1):32–42.
Moloney MG. Natural products as a source for novel antibiotics. Trends Pharmacol Sci. 2016;37(8):689–701.
Chawla M, Verma J, Gupta R, Das B. Antibiotic Potentiators against multidrug-resistant Bacteria: discovery, development, and clinical relevance. Front Microbiol. 2022;13(1):887251.
Jubair N, Rajagopal M, Chinnappan S, Abdullah NB, Fatima A. Review on the antibacterial mechanism of plant-derived compounds against multidrug-resistant Bacteria (MDR). Evid Based Complement Alternat Med. 2021;2021(1):3663315.
Moga MA, Dimienescu OG, Bălan A, Dima L, Toma SI, Bîgiu NF, et al. Pharmacological and therapeutic properties of Punica granatum phytochemicals: possible roles in breast cancer. Molecules. 2021;26(4):1054.
Akhtar S, Ismail T, Fraternale D, Sestili P. Pomegranate peel and peel extracts: chemistry and food features. Food Chem. 2015;174(1):417–25.
Maphetu N, Unuofin JO, Masuku NP, Olisah C, Lebelo SL. Medicinal uses, pharmacological activities, phytochemistry, and the molecular mechanisms of Punica granatum L. (pomegranate) plant extracts: A review. Biomed Pharmacother. 2022;153(1):113256.
Sharma K, Mahato N, Lee YR. Extraction, characterization and biological activity of citrus flavonoids. Rev Chem Eng. 2019;35(2):265–84.
Pirzadeh M, Caporaso N, Rauf A, Shariati MA, Yessimbekov Z, Khan MU, et al. Pomegranate as a source of bioactive constituents: A review on their characterization, properties and applications. Crit Rev Food Sci Nutr. 2021;61(6):982–99.
Sharma A, Thakur N. Influence of active packaging on quality attributes of dried wild pomegranate (Punica granatum L.) arils during storage. J Appl Nat Sci. 2016;8(1):398–404.
Baldassarre F, Vergaro V, De Castro F, Biondo F, Suranna GP, Papadia P, et al. Enhanced bioactivity of pomegranate peel extract following controlled release from CaCO3 nanocrystals. Bioinorg Chem Appl. 2022;2022(1):6341298.
Debib A, Menadi S, Sahnouni F, Boukhatem MN, KACED A. Bacterial inhibitory effect of Algerian pomegranate (Punica Granatum L.) extracts (Peel, juice, and seed) against multidrug resistant Bacteria. Microbiol Biotechnol Food Sci. 2022;11(4):4622.
Malviya S, Arvind JA, Hettiarachchy N. Antioxidant and antibacterial potential of pomegranate peel extracts. J Food Sci Technol. 2014;51:4132–7.
Moussa I, Gassem M, Al-Doss A, Sadik W, Mawgood AA. Using molecular techniques for rapid detection of Salmonella serovars in frozen chicken and chicken products collected from Riyadh. Saudi Arabia Afr J Biotechnol. 2010;9(5):612–9.
Saeed MA, Haque A, Ali A, Mohsin M, Bashir S, Tariq A, et al. A profile of drug resistance genes and integrons in E. Coli causing surgical wound infections in the Faisalabad region of Pakistan. J Antibiot (Tokyo). 2009;62(6):319–23.
Maniatis T, Fritsch E, Sambrook J. Molecular cloning, manual cold spring, harbor laboratory. Cold Spring Harb Protoc; 1989.
Liora M, Mihaiu M, Tăbăran A, Sd D, Iv C, Pivariu B, et al. Antimicrobial resistance evaluation of pathogen Salmonella strains isolated in pork and poultry meat. Bull Univ Agric Sci Vet Med Cluj Napoca. 2013;70(2):266–70.
Humphries R, Bobenchik AM, Hindler JA, Schuetz AN. Overview of changes to the clinical and laboratory standards institute performance standards for antimicrobial susceptibility testing. J Clin Microbiol. 2021;59(12):0021321.
Mphahlele RR, Fawole OA, Makunga NP, Opara UL. Effect of drying on the bioactive compounds, antioxidant, antibacterial, and antityrosinase activities of pomegranate peel. BMC Complement Altern Med. 2016;16(1):143.
Ahmad I, Beg AZ. Antimicrobial and phytochemical studies on 45 Indian medicinal plants against multi-drug resistant human pathogens. J Ethnopharmacol. 2001;74(2):113–23.
Andrews JM. Determination of minimum inhibitory concentrations. J Antimicrob Chemother. 2001;48(1):5–16.
Moghaddam KM, Iranshahi M, Yazdi MC, Shahverdi AR. The combination effect of curcumin with different antibiotics against Staphylococcus aureus. Int J Green Pharm. 2009;3(2):2853045.
Pillai SK, Moellering R, Eliopoulos GM. Antimicrobial combinations. Antib Lab Med. 2005;5(1):365–440.
Magangana TP, Makunga NP, Amos Fawole O, Opara UL. Effect of solvent extraction and blanching pre-treatment on phytochemical, antioxidant properties, enzyme inactivation and antibacterial activities of ‘Wonderful’pomegranate peel extracts. Processes. 2021;9(6):1012.
Masci A, Coccia A, Lendaro E, Mosca L, Paolicelli P, Cesa S. Evaluation of different extraction methods from pomegranate whole fruit or peels and the antioxidant and antiproliferative activity of the polyphenolic fraction. Food Chem. 2016;202(1):59–69.
Singh M, Jha A, Kumar A, Hettiarachchy N, Rai AK, Sharma D. Influence of the solvents on the extraction of major phenolic compounds (punicalagin, ellagic acid and gallic acid) and their antioxidant activities in pomegranate aril. J Food Sci Technol. 2014;51(9):2070–7.
Prashanth D, Asha MK, Amit A. Antibacterial activity of Punica granatum. Fitoterapia. 2001;72(2):171–3.
Shan B, Cai YZ, Brooks JD, Corke H. The in vitro antibacterial activity of dietary spice and medicinal herb extracts. Int J Food Microbiol. 2007;117(1):112–9.
Alzoreky N, Nakahara K. Antibacterial activity of extracts from some edible plants commonly consumed in Asia. Int J Food Microbiol. 2003;80(3):223–30.
Negi P, Jayaprakasha G. Antioxidant and antibacterial activities of Punica granatum peel extracts. J Food Sci. 2003;68(4):1473–7.
Al-Zoreky NS. Antimicrobial activity of pomegranate (Punica granatum L.) fruit peels. Int J Food Microbiol. 2009;134(3):244–8.
Cowan MM. Plant products as antimicrobial agents. Clin Microbiol Rev. 1999;12(4):564–82.
Voravuthikunchai SP, Sririrak T, Limsuwan S, Supawita T, Iida T, Honda T. Inhibitory effects of active compounds from Punica granatum pericarp on verocytotoxin production by enterohemorrhagic Escherichia coli O157: H7. J Health Sci. 2005;51(5):590–6.
Pradeep B, Manojbabu M, Palaniswamy M. Antibacterial activity of Punica granatum L. against gastrointestinal tract infection causing organisms. Ethnobot leafl. 2008;2008(1):143.
Choi JG, Kang OH, Lee YS, Chae HS, Oh YC, Brice OO, et al. In vitro and in vivo antibacterial activity of Punica granatum Peel ethanol extract against Salmonella. Evid Based Complement Alternat Med. 2011;2011(1):690518.
Dahham SS, Ali MN, Tabassum H, Khan M. Studies on antibacterial and antifungal activity of pomegranate (Punica granatum L.). Am Eurasian J Agric. Environ Sci. 2010;9(3):273–81.
Hayouni EA, Miled K, Boubaker S, Bellasfar Z, Abedrabba M, Iwaski H, et al. Hydroalcoholic extract based-ointment from Punica granatum L. peels with enhanced in vivo healing potential on dermal wounds. Phytomed. 2011;18(11):976–84.
Fazeli MR, Bahmani S, Jamalifar H, Samadi N. Effect of probiotication on antioxidant and antibacterial activities of pomegranate juices from sour and sweet cultivars. Nat Prod Res. 2011;25(3):288–97.
Dey D, Debnath S, Hazra S, Ghosh S, Ray R, Hazra B. Pomegranate pericarp extract enhances the antibacterial activity of ciprofloxacin against extended-spectrum β-lactamase (ESBL) and metallo-β-lactamase (MBL) producing gram-negative bacilli. Food Chem Toxicol. 2012;50(12):4302–9.
Fawole OA, Makunga NP, Opara UL. Antibacterial, antioxidant and tyrosinase-inhibition activities of pomegranate fruit peel methanol extract. BMC Complement Altern Med. 2012;12(1):200.
Gaber A, Hassan MM, Dessoky E-DS, Attia AO. In vitro antimicrobial comparison of Taif and Egyptian pomegranate peels and seeds extracts. J Appl Biol Biotechnol. 2015;3(2):0–1.
Dey D, Ray R, Hazra B. Antimicrobial activity of pomegranate fruit constituents against drug-resistant mycobacterium tuberculosis and beta-lactamase producing Klebsiella pneumoniae. Pharm Biol. 2015;53(10):1474–80.
Gullon B, Pintado ME, Pérez-Álvarez JA, Viuda-Martos M. Assessment of polyphenolic profile and antibacterial activity of pomegranate peel (Punica granatum) flour obtained from co-product of juice extraction. Food Cont. 2016;59(1):94–8.
Shivsharan U, Ravva S. Antimicrobial activity of pomegranate juice. Res J Pharm Technol. 2018;11(10):4329–31.
Daoutidou M, Plessas S, Alexopoulos A, Mantzourani I. Assessment of antimicrobial activity of pomegranate, cranberry, and black chokeberry extracts against foodborne pathogens. Foods. 2021;10(3):486.
Elafify M, Darwish WS, El-Toukhy M, Badawy BM, Mohamed RE, Shata RR. Prevalence of multidrug resistant Salmonella spp. in dairy products with the evaluation of the inhibitory effects of ascorbic acid, pomegranate peel extract, and D-tryptophan against Salmonella growth in cheese. Int J Food Microbiol. 2022;364:109534.
Voravuthikunchai S, Lortheeranuwat A, Jeeju W, Sririrak T, Phongpaichit S, Supawita T. Effective medicinal plants against enterohaemorrhagic Escherichia coli O157:H7. J Ethnopharmacol. 2004;94(1):49–54.
Alexandre EMC, Silva S, Santos SAO, Silvestre AJD, Duarte MF, Saraiva JA, et al. Antimicrobial activity of pomegranate peel extracts performed by high pressure and enzymatic assisted extraction. Food Res Int. 2019;115(1):167–76.
McCarrell EM, Gould SW, Fielder MD, Kelly AF, El Sankary W, Naughton DP. Antimicrobial activities of pomegranate rind extracts: enhancement by addition of metal salts and vitamin C. BMC Complement Altern Med. 2008;8(1):64.
Hooper DC. Emerging mechanisms of fluoroquinolone resistance. Emerg Infect Dis. 2001;7(2):337–41.
Yu EW, Aires JR, Nikaido H. AcrB multidrug efflux pump of Escherichia coli: composite substrate-binding cavity of exceptional flexibility generates its extremely wide substrate specificity. J Bacteriol. 2003;185(19):5657–64.
Mazzariol A, Zuliani J, Cornaglia G, Rossolini GM, Fontana R. AcrAB efflux system: expression and contribution to fluoroquinolone resistance in Klebsiella spp. Antimicrob Agents Chemother. 2002;46(12):3984–6.
Stavri M, Piddock LJ, Gibbons S. Bacterial efflux pump inhibitors from natural sources. J Antimicrob Chemother. 2007;59(6):1247–60.
Jurenka JS. Therapeutic applications of pomegranate (Punica granatum L.): a review. Altern Med Rev. 2008;13(2):128–44.
Tariq A, Sana M, Shaheen A, Ismat F, Mahboob S, Rauf W, et al. Restraining the multidrug efflux transporter STY4874 of Salmonella Typhi by reserpine and plant extracts. Lett Appl Microbiol. 2019;69(3):161–7.
Braga LC, Shupp JW, Cummings C, Jett M, Takahashi JA, Carmo LS, et al. Pomegranate extract inhibits Staphylococcus aureus growth and subsequent enterotoxin production. J Ethnopharmacol. 2005;96(1–2):335–9.
Aqil F, Munagala R, Vadhanam MV, Kausar H, Jeyabalan J, Schultz DJ, et al. Anti-proliferative activity and protection against oxidative DNA damage by punicalagin isolated from pomegranate husk. Food Res Int. 2012;49(1):345–53.
Wu D, Ma X, Tian W. Pomegranate husk extract, punicalagin and ellagic acid inhibit fatty acid synthase and adipogenesis of 3T3-L1 adipocyte. J Funct Foods. 2013;5(2):633–41.
Nuncio-Jauregui N, Nowicka P, Munera-Picazo S, Hernández F, Carbonell-Barrachina ÁA, Wojdyło A. Identification and quantification of major derivatives of ellagic acid and antioxidant properties of thinning and ripe Spanish pomegranates. J Funct Foods. 2015;12(1):354–64.
Li G, Xu Y, Pan L, Xia X. Punicalagin damages the membrane of Salmonella typhimurium. J Food Prot. 2020;83(12):2102–6.
Li G, Yan C, Xu Y, Feng Y, Wu Q, Lv X, et al. Punicalagin inhibits Salmonella virulence factors and has anti-quorum-sensing potential. Appl Environ Microbiol. 2014;80(19):6204–11.
Inamuco J, Veenendaal AK, Burt SA, Post JA, Tjeerdsma-van Bokhoven JL, Haagsman HP, et al. Sub-lethal levels of carvacrol reduce Salmonella typhimurium motility and invasion of porcine epithelial cells. Vet Microbiol. 2012;157(1–2):200–7.
Mun SH, Kang OH, Kong R, Zhou T, Kim SA, Shin DW, et al. Punicalagin suppresses methicillin resistance of Staphylococcus aureus to oxacillin. J Pharmacol Sci. 2018;137(4):317–23.
Song W, Wang L, Jin M, Guo X, Wang X, Guan J, et al. Punicalagin, an inhibitor of Sortase A, is a promising therapeutic drug to combat methicillin-resistant Staphylococcus aureus infections. Antimicrob Agents Chemother. 2022;66(6):22422.
Chusri S, Villanueva I, Voravuthikunchai SP, Davies J. Enhancing antibiotic activity: a strategy to control Acinetobacter infections. J Antimicrob Chemother. 2009;64(6):1203–11.
Acknowledgments
The authors gratefully acknowledge the Higher Education Commission for the IRSIP fellowship scheme with a six-month scientific visit of Saba Kiran to the USA.
Funding
A six-month scientific visit of Saba Kiran to the US was funded by HEC through the IRSIP fellowship scheme at Cornell University, Ithaca New York.
Author information
Authors and Affiliations
Contributions
Saba Kiran collected local fruits and clinical isolates, prepared extracts, performed antibacterial studies, compound identification through LCMS/MS, Minimum inhibitory concentration studies, and synergy assays of active compounds, and drafted the manuscript. Waqar Rauf planned the LCMS/MS analysis of the plant extracts and drafted and reviewed the manuscript. Fazal-e-Habib, Shoaib Iqbal, and Ashfaq Hussain assisted in conducting the LCMS/MS analysis. Zubera Naseem, Sobia Jabeen, and Rizwan Bashir helped with extract preparations and manuscript writing. Aamir Ali provided the guidelines for conducting the antibacterial experiments and drafted the manuscript accordingly. Yasra Sarwar helped in conducting all bacterial isolation and identification. Anam Tariq and Moazur Rahman helped in MIC calculations and growth curve studies. Waqar Siddique helped with manuscript writing. Georg Jander provided the required standards and helped to conduct the research work related to the current study by providing technical support, and also gave valuable suggestions to draft the manuscript. Mazhar Iqbal conceived the project, planned experiments, analyzed the data, as well as drafted the manuscript. All authors have read and approved the manuscript for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. The collection of plant materials was made after obtaining the permission from Director, NIBGE. All experimental studies on plants and their microbiological assays were conducted with the approval of the Institutional Ethical Committee of National Institute for Biotechnology and Genetic Engineering (NIBGE). The study does not report on or involve the use of any animal or human data or tissue sampling.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kiran, S., Tariq, A., Iqbal, S. et al. Punicalagin, a pomegranate polyphenol sensitizes the activity of antibiotics against three MDR pathogens of the Enterobacteriaceae. BMC Complement Med Ther 24, 93 (2024). https://doi.org/10.1186/s12906-024-04376-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-024-04376-7