Abstract
Background
Senna occidentalis (L.) Link has been used worldwide in traditional treatment of many diseases and conditions including snakebite. In Kenya, a decoction from the plant roots taken orally, is used as a cure for malaria. Several studies have demonstrated that extracts from the plant possess antiplasmodial activity, in vitro. However, the safety and curative potency of the plant root against established malaria infection is yet to be scientifically validated, in vivo. On the other hand, there are reports on variation in bioactivity of extracts obtained from this plant species, depending on the plant part used and place of origin among other factors. In this study, we demonstrated the antiplasmodial activity of Senna occidentalis roots extract in vitro, and in mice.
Methods
Methanol, ethyl acetate, chloroform, hexane and water extracts of S. occidentalis root were tested for in vitro antiplasmodial activity against Plasmodium falciparum, strain 3D7. Cytotoxicity of the most active solvent extracts was determined using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay and the curative potency in Plasmodium berghei infected mice evaluated by Rane’s test.
Results
All of the solvent extracts tested in this study inhibited the propagation of P. falciparum, strain 3D7, in vitro, with polar extracts being more active than non-polar ones. Methanolic extracts had the highest activity (IC50 = 1.76) while hexane extract displayed the lowest activity (IC50 = 18.47). At the tested concentrations, methanolic and aqueous extracts exhibited high selectivity index against P. falciparum strain 3D7 (SI > 10) in the cytotoxicity assay. Further, the extracts significantly suppressed the propagation of P. berghei parasites (P < 0.05) in vivo and increased the survival time of the infected mice (P < 0.0001).
Conclusions
Senna occidentalis (L.) Link root extract inhibits the propagation of malaria parasites in vitro and in BALB/c mice.
Similar content being viewed by others
Background
Malaria continues to be a public health challenge particularly in Sub-Saharan Africa [1, 2]. There were an estimated 247 million malaria cases and 619,000 deaths globally in 2021 [3]. Although malaria control has proven to be very effective when vector control is combined with prompt treatment, drug resistance to the insecticides used in vector control and antimalarial drugs pose a significant challenge to malaria control programs [1, 4,5,6,7]. Furthermore, some of the available antimalarial drugs have been linked to adverse side effects such as headache, diarrhea, nausea, pruritus, anxiety, seizures and hair discoloration. Long-term use of the drugs may lead to heart, eye and neuron defects [8].
Currently, the World Health Organization (WHO) recommends combining artemisinin and its derivatives with other antimalarial drugs in combination therapy [2, 9, 10]. This approach has proven to be effective in the treatment of P. falciparum malaria in various parts of the world. However, Plasmodium malaria resistance to current first line drugs, including artemisinin, has been reported [2, 10,11,12,13,14]. As such, priority should be given to the discovery and development of antimalarial drugs with novel and distinct mechanisms of action.
Medicinal plants are a rich source of untapped antimalarial activities [1, 2, 4, 15]. This is supported by the successful discovery of Artemisinin, Quinine and their derivatives as effective antimalarial drugs [16, 17]. Senna occidentalis (L.) Link is a widely used plant in traditional medicine throughout the world [18]. This plant is frequently used to treat a variety of infections and other conditions like snake and insect bites [18,19,20,21]. In traditional medicine, all parts of the plant are used [19]. The plant possesses antioxidant, nephroprotective and hepatoprotective activity, immunomodulatory activity, antidiabetic activity, analgesic and antipyretic activity, antianxiety, antidepressant and antimutagenic activity as well as antibacterial and antifungal activity [22,23,24,25].
In Kenya, Senna occidentalis root decoction is taken orally three times daily for 3 to 4 days by the Luhya, Digo and Duruma communities for treatment of malaria [26,27,28]. Previous in vitro studies have shown that S. occidentalis extract is active against P. falciparum. In one of the studies, S. occidentalis inhibited the growth of chloroquine sensitive (strain 3D7) and resistant (strain Dd2) P. falciparum with half-maximal inhibitory concentration (IC50) values of 65 μg/ml and 110 μg/ml respectively [29]. In a different study [30], an ethanolic extract of the plant similarly suppressed the growth of chloroquine sensitive P. falciparum (IC50 < 3 μg/ml), in vitro. In yet another study, S. occidentalis extract showed in vitro activity against chloroquine sensitive P. falciparum, strain 3D7, (IC50 = 48.80 μg/ml) and the resistant parasites, stain INDO, (IC50 = 54.28 μg/ml) [18]. In a more recent study [31], an extract from the plant exhibited in vitro activity against P. falciparum (3D7 strain) with an IC50 value of 3.37 μg/ml. The variation in IC50 values obtained in these studies could be due to differences in geographical origin of the plant, parts of the plant used, season of the year when plant material collection was done, methods of preparation and storage [25, 32, 33], or differences in assay protocols [34,35,36]. This current study sought to investigate further the antimalarial potency of the plant extract against P. falciparum, in vitro and P. berghei, in vivo.
Methods
Ethical clearance
Approval to conduct this study was granted by the Institute of Primate Research (IPR) Institutional Scientific and Ethics Review Committee (ISERC/02/18). The plant material used in this study was collected according to the WHO guidelines on Good Agriculture and Collection Practices (GACP) for medicinal plants [37]. The handling and care of experimental mice was done in compliance with the international guidelines on the care and use of laboratory animals. In addition, the study was done based on the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines. The Institute of Primate Research facility is registered by the National Commission for Science, Technology and Innovation (NACOSTI), Kenya and accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International.
Plant collection, extraction and processing
Senna occidentalis roots were collected from Migori county (0.9366o S, 34.4198o E), Kenya in the months of August and September. This plant was identified by Mr. Jonathan Ayayo, a taxonomist of the National Museums of Kenya (NMK), and a voucher specimen (38/81) deposited at East African Herbarium of NMK for future reference. Further, the plant name was verified with http://www.theplantlist.org on 10/05/2022.
The collected plant roots were air dried in the shade, ground into powder and stored in airtight plastic containers at 4 °C until extraction.
Hexane, chloroform, ethyl acetate and methanol, in their absolute forms, as well as distilled water were used for extraction by maceration. For organic solvents, the plants root powder was macerated separately with the solvents for 48 hours in an orbital shaker and a filtrate obtained (Whatman No. 1 filter paper). For water, the roots powder was soaked in double distilled water for 24 hours. In addition, a decoction was prepared by boiling the roots powder in double distilled water for 30 minutes at a mean temperature of 95 °C [38]. Filtration of aqueous extracts was done through a cotton wool plug followed by filtration (Whatman No. 1 filter paper). The aqueous decoction was included to mimic the local’s traditional method of preparing the antimalarial therapy. The filtrates were concentrated by rotary vaporization (BÜCHI R-200 rotary evaporator) at 50 °C and reduced pressure for organic solvents, and lyophilization (NANBEI freeze dryer: NBJ-10-1, Zhengzhou, China) for aqueous solutions. Upon drying, the extracts were stored in sealed sample bottles at 4 °C until needed.
Plant secondary metabolites are excellent predictors of their bioactivity potential [39]. In order to predict the bioactivity of S. occidentalis roots extract, .standard procedures were used to screen the extracts for the presence of saponins, tannins, alkaloids, flavonoids and sterols [40].
Plasmodium falciparum propagation and extracts preparation
Senna occidentalis root extracts were tested in vitro for antiplasmodial potency using P. falciparum, strain 3D7 obtained from Kenya Medical Research Institute (KEMRI) repository. A modified version of a previously used method [41] was utilised to establish a continuous culture of these malaria parasites. In summary, the parasites were propagated at 37 °C in blood group O+ red blood cells (RBCs) maintained in RPMI 1640 growth medium (Life technologies Ltd., Paisley, UK) supplemented with 1 M 4-(2-hydroxyethyl)-1-piperazine ethanesulfonic acid (HEPES), (Gibco, Life technologies Ltd., Paisley, UK), 1 M Sodium hydroxide (EMD Millipore corporation, Darmstadt, Germany), 20% D-glucose (PANREAC QUIMICA SA Barcelona, Spain), 200 mM L-glutamine (Gibco, Life technologies Ltd., Paisley, UK), 10% human serum (group O+) and a gas mixture of 90% N2, 5% O2 and 5% CO2. The culture was refreshed every 48 hours at 3% haematocrit.
Dilutions of the extract and standard drug were carried out in the same manner as described [42], with minor modifications. To make a stock solution (5 mg/ml), each extract was first dissolved in dimethyl sulfoxide (DMSO), vortexed and RPMI 1640 (incomplete medium) added to the required volume. For extract combinations, the extracts were weighed and blended in a 1:1 ratio [43]. A 0.5 mg/ml stock solution of pyrimethamine was also prepared.
In vitro growth inhibition assay
Growth inhibition of P. falciparum malaria parasites by S. occidentalis root extract was assessed as described [44], with minor modification. A ten-fold dilution was prepared from the stock solutions using complete RPMI 1640 and serially diluted 7-fold across a 96-well cell culture plate. This provided a dose-titration range of 250 μg/ml to 1.95 μg/ml for the extracts and 25 μg/ml to 0.20 μg/ml for pyrimethamine. Sorbitol synchronized ring stage parasitized RBCs (1% parasitemia) suspended in complete RPMI at 3% hematocrit was then added to respective wells. Non-infected RBCs as well as DMSO were also included in the assay as controls. The plates were incubated at 37 °C. After 72 hours, thin smears were prepared and parasites quantified by light microscopy. Percentage parasitemia suppression was computed and 50% inhibitory concentration (IC50) values determined for each extract [45, 46].
Evaluation of the extract for cytotoxicity
To assess the in vitro cytotoxicity of S. occidentalis root extract, Vero cell line (sourced from KEMRI) was grown to confluent monolayer in Minimum Essential Medium Eagle (MEM) containing sodium bicarbonate and l-glutamine. The growth medium was supplemented with 1% pen-strep (Sigma), 1% HEPES (Gibco) and 10% Fetal bovine serum (FBS). The assay was performed as previously described [47, 48]. Briefly, 10,000 Vero cells contained in 100 μl cell suspension were seeded onto each well of a 96-cell culture plate and incubated for 24 hours at 37 °C in a 5% CO2 incubator to allow the cells achieve a layer of > 90% confluence. The cells were exposed to 100 μl of the extracts for 48 hours, in concentration ranges of 250–3.91 and 25–0.39 μg/ml for the extracts and pyrimethamine, respectively. Pyrimethamine and DMSO (0.4%) exposed, as well as untreated cells were included as controls. Following 48 hours’ incubation period, 10 μl of MTT reagent (5 mg/ml) was added aseptically to each well, tapped gently to mix and incubated for 3 hours at 37 °C. All media was then aspirated from the wells and 100 μl DMSO added. Optical density (OD) readings as obtained by an ELISA reader were then used to compute the extracts’ 50% cytotoxicity concentration (CC50) and selectivity index (SI) as described elsewhere [48, 49].
Experimental animals and rodent malaria parasites
In this study, male and female inbred BALB/c mice aged 8–9 weeks were used. The rodent facility at IPR provided the animals. They were housed in standard Macron type II cages within 12 hours’ dark/light cycle at 23 °C. Food and water was provided ad libitum according the IPR’s Animal Science Department standard operating procedures.
Plasmodium berghei, strain ANKA (sourced from KEMRI) was retrieved from the IPR repository and maintained in mice [50] for use in this study. This parasite strain was utilized because it causes severe disease in BALB/c mice with clinical characteristics similar to P. falciparum infection [51]. Despite the phylogenetic distance between rodent and human malaria parasites, P. berghei and the human malaria parasites possess conserved genes that have over time allowed their use in Peters’ model of antimalarial drug efficacy testing [52].
Mice infection, treatment and monitoring of parasitemia and survivorship
A modification of the method by Ryley and Peters (1970) was used to evaluate the curative potency of the extract against P. berghei in mice [53, 54]. Mice were inoculated intraperitoneally with 1 × 106P. berghei infected erythrocytes and assigned randomly to 5 experimental groups; A, B, C, D and E (5 mice per group). At approximately 5% parasitemia (day 5 post-infection), treatment was started. Groups A and B were treated with 200 mg/kg and 100 mg/kg of the methanolic extract, respectively. Group C was treated with 200 mg/kg of the aqueous extract. Group D was treated with 1 mg/kg pyrimethamine (Sigma – Aldrich Chemie, Steinheim, Germany). Group E (the placebo group) was administered with 1% DMSO in phosphate buffered saline (vehicle). The treatment was administered orally for 4 consecutive days. The oral route was chosen based on documented ethnomedical usage of the plant [28]. The mice were monitored for survival till day 30 post infection. Meanwhile, parasitemia suppression was determined. The amount of extract administered was informed by dose recommendations for in vivo administration of crude extracts [55] as well as previous antimalarial studies involving Senna family [5, 56].
Determination of parasite growth suppression
The effect of the extract on P. berghei growth inhibition in mice was determined on days 6, 8, 10 and 12 post infection as described previously [53]. Tail blood was used to prepare thin smears that were fixed with absolute methanol and observed under × 100 lens of a light microscope. The number of parasitized red blood cells (pRBCs) was examined per at least 1000 RBCs. Percentage parasitemia and parasite suppression was then computed using the following formulas [57];
Determination of mean survival time
To assess the effect of the extract on survival time of the infected mice, the number of days that each mouse lived from the day of parasite inoculation to death was recorded in a 30 days’ period. The following formula was used to determine the mean survival time of each group [58];
Statistical analysis
The collected data was recorded as means ± standard error of the means (M ± SEM). In vivo parasite suppression was analyzed through Ordinary One-Way ANOVA followed by Tukey’s multiple comparisons test at 95% confidence level (alpha = 0.05). Log rank analysis was used to compare survival time of mice in the different treatment groups. Graph Pad prism (Version 7.00, California, USA) was used for the analyses.
Results
Senna occidentalis root extract possesses secondary plant metabolites
Plants with active phytomedicine properties possess secondary metabolites (Okokon et al., 2017). Methanol, ethyl acetate, chloroform, hexane and aqueous extracts of S. occidentalis roots were screened for presence of secondary metabolites. All extracts contained saponins, tannins, flavonoids, alkaloids and sterols. Aqueous decoction provided the highest percentage yield (7%) whereas hexane maceration provided the least yield (2%). The characteristics and yields of the extracts are as shown (Supplementary data 1). These extracts were subsequently assayed for biological activity against Plasmodium spp. especially suppression of malaria parasites growth.
Senna occidentalis roots extract suppresses plasmodium falciparum growth, in vitro
Methanol, ethyl acetate, chloroform, hexane and aqueous roots extracts of S. occidentalis were tested for growth suppression potency against P. falciparum. The use of solvents with differing polarity would enable evaluation of antiplasmodial activity of both polar and nonpolar metabolites of the plant root. The results (Table 1) show that methanolic extract exhibited minimum IC50 value (IC50 = 1.76) whereas hexane extract exhibited maximum IC50 value (IC50 = 18.47). The parasite growth suppression levels are as shown (Supplementary data 2). The results imply that methanolic extract was 10-fold active against P. falciparum compared to hexane extracts. When the antiplasmodial activity of the other extracts was compared to that of hexane, the activity was 8, 4, 2.7 and 1.5-fold higher for aqueous macerate, ethyl acetate, aqueous decoction and chloroform respectively. These results suggest that polar extracts of S. occidentalis roots are more active against P. falciparum, in vitro, than non-polar ones. Furthermore, the findings demonstrate that both polar and non-polar metabolites of S. occidentalis roots are potent against P. falciparum in vitro.
Senna occidentalis roots extract is non-toxic to Vero cells, in vitro
Growth inhibitory effects observed in antiplasmodial assays may result from general toxicity of the substances being tested rather than specific activity on the Plasmodium parasites [49, 59]. The cytotoxicity of methanol and aqueous extracts were assessed using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. These two extracts were selected for cytotoxicity evaluation because they showed greater antiplasmodial activity in the in vitro assay and, were as such, candidates for pre-clinical analysis for antiplasmodial activity in animal models. Both the methanolic and aqueous extracts exhibited selectivity indices greater than 10 (Table 1), an indication of high selectivity for malaria parasites [48]. This observation implies that S. occidentalis root extract is non-toxic to animal cells at the tested concentrations.
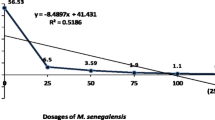
Senna occidentalis roots extract suppresses plasmodium berghei parasitemia in mice
The P. berghei-BALB/c mouse model was utilized to assess the antiplasmodial activity of S. occidentalis polar extracts in situ in an animal system. The effect of S. occidentalis extract on P. berghei parasitemia suppression was determined by monitoring parasite multiplication in the infected mice upon treatment with the extract. At a dose of 200 mg/kg body weight, both the methanolic and aqueous extracts significantly suppressed P. berghei growth (P < 0.05) on days 6, 8, 10 and 12, relative to the phosphate buffered saline (placebo) group. At a dose of 200 mg/kg body weight, the inhibitory activity of methanol extract was not significantly different from that of aqueous extract (P > 0.05), except on day 6 post infection when the methanolic extract depicted higher activity (P = 0.03). The suppressive activity of 100 mg/kg methanol extract was not significantly different from that of 200 mg/kg aqueous extract (P > 0.05). Likewise, the suppressive activity of 100 mg/kg methanolic extract was not significantly different from that of 200 mg/kg extract of the same solvent (P > 0.05). This suggests using 100 mg/kg methanolic extract as optimum for use in mice. Parasite multiplication increased steadily in the placebo group until day 8 post-infection when it began to lag. This was indicative of reticulocyte depletion resulting in fewer cells available for malaria parasite infection [60, 61]. The pyrimethamine control group achieved 100% parasite clearance by day 9 post infection. Overall, these findings show that aqueous and methanolic extracts of S. occidentalis roots suppress P. berghei propagation, in vivo and that the aqueous extract is as effective as the methanolic extract at the tested concentrations. The parasite suppression levels for the different treatment groups are as shown in Table 2. Figure 1 shows parasitemic profiles of P. berghei in mice treated with the extract and the controls.
Senna occidentalis roots extract enhances the survival time of plasmodium berghei infected mice
The effect of S. occidentalis extract on the survival of P. berghei infected mice was assessed by monitoring survival time of the extract-treated animals for 30 days, post- infection. The extract prolonged the survival time of the infected mice in the range of 4 to 6 days, which is approximately 0.3- to 0.5-fold extension of survival time relative to the placebo-treated animals. Treatment with the standard drug, pyrimethamine, resulted in 100% survival of the infected mice. When compared to the placebo group, the increase in survival time of the extract treated mice was significant (P < 0.0001). The mean number of days survived by the infected animals post infection is as shown in Table 3. Figure 2 represents survivorship curves for the animals in the different treatment groups.
Discussion
Natural products, especially medicinal plants, have been used to treat malaria or manage conditions associated with it in various parts of the world [5, 7]. We show, in this study, that S. occidentalis root extract inhibits malaria parasites growth in vitro and in mice. Our findings augment various studies that have illustrated the antimalarial potency of medicinal plants, as reviewed [62,63,64]. The documented ethnomedical use of the plant root as a cure for malaria in Kenya influenced the selection of the plant for antiplasmodial in vitro evaluation [27, 28]. This ethnopharmacological approach to drug development has been associated with high success rates of discovering active compounds from natural sources [49]. It is also a cost effective and time saving approach compared to mass screening of plants for specific biological activity [65, 66].
To obtain polar and nonpolar root extracts of S. occidentalis for evaluation of antimalarial potential, the plants roots powder was extracted with methanol, ethyl acetate, chloroform, hexane and water. Preliminary phytochemical analysis of the extracts revealed the presence of biologically important secondary metabolites, some of which have been linked to antimalarial activities of plant extracts [25, 39, 54, 67, 68]. These findings paved way for further analysis of S. occidentalis extracts as antimalarials. A bioactivity guided extract fractionation will reveal the actual molecules containing antiplasmodial activity.
In this current study, the extracts were found to be active, in vitro, against P. falciparum. This malaria parasite species is the foremost contributor to the global burden of malaria [1, 4, 9]. Our findings revealed that antiplasmodial activity of S. occidentalis roots is polarity dependent with extracts from polar solvents showing higher activity than non-polar ones. This suggests that during extraction, the bioactive principles of the plant roots get localized more in polar solvents than non-polar ones. Extraction efficiency has been shown to be dependent on the method and solvent of extraction [69]. Differences in extraction temperature may account for the variation in bioactivity between aqueous macerate and decoction extracts. High temperatures lead to loss of thermolabile compounds or even transformation of the phytochemicals [69]. Overall, these findings imply that the antimalarial ingredients of the roots extract of S. occidentalis are mainly polar.
In this current study, S. occidentalis root extract showed no toxicity to Vero cells and was highly selective of P. falciparum. This is suggestive of possible safety of the extracts when used in in vivo models of antimalarial efficacy testing.
Drug interaction with malaria parasites is heavily influenced by the host biological system [34, 70]. In this current study, S. occidentalis root extract was evaluated for antiplasmodial activity in situ using the P. berghei mouse model of antimalarial drug efficacy testing. In this in vivo assay, use of human malaria parasites (P. falciparum), just like in the in vitro test, would have been more appropriate. However, we did not have access to an animal model for P. falciparum antimalarial drug efficacy testing. Alternatively, our laboratory has established protocols for in vivo antimalarial drug efficacy testing using P. berghei in a mouse model. The structure, life cycle and physiology of P. berghei compare with those of the human malaria parasites [71]. Accordingly, mouse specific parasite species have been used in Peters’ standard test to provide important data in support of antimalarial drug development [72, 73]. As such the P. berghei mouse model would provide valuable information regarding the in vivo antiplasmodial potential of the extract under investigation in the current study. The effect of S. occidentalis extract on P. berghei parasitemia was determined by monitoring parasite propagation in infected BALB/c mice upon treatment with the extract. The extract significantly suppressed P. berghei parasitemia in mice and increased the survival time of the infected animals. The longer survival time of mice treated with the extract corresponded with reduced parasitemia, suggesting that the extract may play a role in reducing the pathologic effects of the infection. A positive correlation between parasite density, disease severity and mortality due to malaria has been described [74, 75]. In the current study, we did not evaluate the extract for protective activity against malaria infection. The next step would, therefore, be the analysis of the antimalarial potency of S. occidentalis extracts in a prophylactic, as well as non-human primate model for a more complete preclinical testing.
The presence of secondary metabolites in the extract investigated herein may explain the growth suppressive activities of the extract against malaria parasites observed in this study. Plant secondary metabolites have been shown to induce malaria parasite death through diverse mechanisms. For instance, flavonoids have been shown to possess antioxidant potential and kill Plasmodium parasites by chelating nucleic acids of malaria parasites [38, 76]. It is also reported elsewhere that antioxidants can inhibit heme polymerization, and that unpolymerized heme is very toxic to Plasmodium parasites, hence kills malaria parasites [77]. More studies are required to determine the mechanism used by S. occidentalis root extract in suppressing P. falciparum and P. berghei parasites growth.
Conclusions
Overall, our findings demonstrate that Senna occidentalis (L.) Link root extract has remarkable antimalarial activity, in vitro and in mice. In addition, the results show that polar extracts of S. occidentalis are more potent than non-polar ones, implying that polar extracts can be developed further into antimalarials. We recommend the isolation and identification of the bioactive entities and the establishment of the antimalarial mechanism of action of the extract.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article. The raw data used for analysis can be availed by the corresponding author on request.
Abbreviations
- AAALAC:
-
Association for Assessment and Accreditation of Laboratory Animal Care
- ARRIVE:
-
Animal Research: Reporting of In Vivo Experiments
- ANOVA:
-
Analysis of variance
- DMSO:
-
Dimethyl sulfoxide
- FBS:
-
Fetal bovine serum
- IPR:
-
Institute of Primate Research
- ISERC:
-
Institutional Scientific and Ethics Review Committee
- KEMRI:
-
Kenya Medical Research Institute
- MEM:
-
Minimum Essential Medium Eagle
- NACOSTI:
-
National Commission for Science, Technology and Innovation
- RBCs:
-
Red blood cells
- RPMI:
-
Roswell Park Memorial Institute
- WHO:
-
World Health Organization
- CC50 :
-
50% cytotoxicity concentration
- IC50 :
-
50% inhibitory concentration
References
Baah MK, Mensah AY, Asante-Kwatia E, Amponsah IK, Forkuo AD, Harley BK, et al. In vivo antiplasmodial activity of different solvent extracts of Myrianthus libericus stem bark and its constituents in plasmodium berghei-infected mice. Evid Based Complement Alternat Med. 2020;2020. ID: 8703197.
Cimanga RK, Nsaka SL, Tshodi ME, Mbamu BM, Kikweta CM, Makila FB-M, et al. In vitro and in vivo antiplasmodial activity of extracts and isolated constituents of Alstonia congensis root bark. J Ethnopharmacol. 2019;242:111736.
WHO. World malaria report 2022: World Health Organization; 2022.
Chaniad P, Techarang T, Phuwajaroanpong A, Punsawad C. Antimalarial activity and toxicological assessment of Betula alnoides extract against plasmodium berghei infections in mice. Evid Based Complement Alternat Med. 2019;2019. ID: 2324679.
Ekasari W, Wahyuni TS, Arwaty H, Putri NT. Determination of effective dose of antimalarial from Cassia spectabilis leaf ethanol extract in plasmodium berghei-infected mice. Afr J Infect Diseases. 2018;12(1S):110–5.
Ntie-Kang F, Onguéné PA, Lifongo LL, Ndom JC, Sippl W, Mbaze LM. The potential of anti-malarial compounds derived from African medicinal plants, part II: a pharmacological evaluation of non-alkaloids and non-terpenoids. Malar J. 2014;13(1):1–20.
Otegbade OO, Ojo JA, Adefokun DI, Abiodun OO, Thomas BN, Ojurongbe O. Ethanol extract of Blighia sapida stem bark show remarkable prophylactic activity in experimental plasmodium berghei–infected mice. Drug Target Insights. 2017;11:1177392817728725.
Lozano-Cruz OA, Jiménez JV, Olivas-Martinez A, Ortiz-Brizuela E, Cárdenas-Fragoso JL, Azamar-Llamas D, et al. Adverse effects associated with the use of antimalarials during the COVID-19 pandemic in a tertiary care center in Mexico city. Front Pharmacol. 2021;12:668678.
Kavishe RA, Koenderink JB, Alifrangis M. Oxidative stress in malaria and artemisinin combination therapy: pros and cons. FEBS J. 2017;284(16):2579–91.
Nondo RSO, Moshi MJ, Erasto P, Masimba PJ, Machumi F, Kidukuli AW, et al. Anti-plasmodial activity of Norcaesalpin D and extracts of four medicinal plants used traditionally for treatment of malaria. BMC Complement Altern Med. 2017;17(1):1–8.
Ariey F, Witkowski B, Amaratunga C, Beghain J, Langlois A-C, Khim N, et al. A molecular marker of artemisinin-resistant plasmodium falciparum malaria. Nature. 2014;505(7481):50–5.
Haidara M, Haddad M, Denou A, Marti G, Bourgeade-Delmas S, Sanogo R, et al. In vivo validation of anti-malarial activity of crude extracts of Terminalia macroptera, a Malian medicinal plant. Malar J. 2018;17(1):1–10.
Sadiq MB, Tharaphan P, Chotivanich K, Tarning J, Anal AK. In vitro antioxidant and antimalarial activities of leaves, pods and bark extracts of Acacia nilotica (L.) Del. BMC Complement Altern Med. 2017;17(1):1–8.
WHO. World malaria report 2021: Tracking progress against malaria. 2021.
Berthi W, González A, Rios A, Blair S, Cogollo Á, Pabón A. Anti-plasmodial effect of plant extracts from Picrolemma huberi and Picramnia latifolia. Malar J. 2018;17(1):1–12.
Musila FM. In vivo antimalarial activity, toxicity and phytochemical screening of aqueous and organic extracts of selected antimalarial plants in Msambweni district. Kenya: University of Nairobi; 2012.
Rasoanaivo P, Wright CW, Willcox ML, Gilbert B. Whole plant extracts versus single compounds for the treatment of malaria: synergy and positive interactions. Malar J. 2011;10(1):1–12.
Murugan K, Aarthi N, Kovendan K, Panneerselvam C, Chandramohan B, Kumar PM, et al. Mosquitocidal and antiplasmodial activity of Senna occidentalis (Cassiae) and Ocimum basilicum (Lamiaceae) from Maruthamalai hills against Anopheles stephensi and plasmodium falciparum. Parasitol Res. 2015;114(10):3657–64.
Al-Snafi AE. The therapeutic importance of Cassia occidentalis-an overview. Ind J Pharmaceutical Sci Res. 2015;5(3):158–71.
Veerachari U, Bopaiah A. Phytochemical investigation of the ethanol, methanol and ethyl acetate leaf extracts of six Cassia species. Int J Pharm Bio Sci. 2012;3(2):260–70.
Yadav J, Arya V, Yadav S, Panghal M, Kumar S, Dhankhar S. Cassia occidentalis L.: a review on its ethnobotany, phytochemical and pharmacological profile. Fitoterapia. 2010;81(4):223–30.
Ali M, Ansari S, Ahmad S, Sanobar S, Hussain A, Khan SA, et al. Phytochemical and Pharmacological Approaches of Traditional Alternate Cassia occidentalis L. Plant and Human Health, Volume 3: Springer; 2019. p. 321–41.
Silva MG, Aragão TP, Vasconcelos CF, Ferreira PA, Andrade BA, Costa IM, et al. Acute and subacute toxicity of Cassia occidentalis L. stem and leaf in Wistar rats. J Ethnopharmacol. 2011;136(2):341–6.
Singh VV, Jain J, Mishra AK. Determination of antipyretic and antioxidant activity of Cassia occidentalis Linn methanolic seed extract. Pharmacognosy J. 2017;9(6):913–6.
Vijayalakshmi S, Ranjitha J, Devi Rajeswari V, Bhagiyalakshmi M. Pharmacological profile of Cassia occidentalis L–A review. Int J Pharm Pharm Sci. 2013;5(3):29–33.
Muthaura C, Keriko J, Derese S, Yenesew A, Rukunga G. Investigation of some medicinal plants traditionally used for treatment of malaria in Kenya as potential sources of antimalarial drugs. Exp Parasitol. 2011;127(3):609–26.
Muthaura C, Keriko J, Mutai C, Yenesew A, Gathirwa J, Irungu B, et al. Antiplasmodial potential of traditional antimalarial phytotherapy remedies used by the Kwale community of the Kenyan coast. J Ethnopharmacol. 2015;170:148–57.
Nguta J, Mbaria J, Gakuya D, Gathumbi P, Kiama S. Antimalarial herbal remedies of Msambweni, Kenya. J Ethnopharmacol. 2010;128(2):424–32.
El Tahir A, Satti GM, Khalid SA. Antiplasmodial activity of selected Sudanese medicinal plants with emphasis on Maytenus senegalensis (lam.) Exell. J Ethnopharmacol. 1999;64(3):227–33.
Tona L, Cimanga R, Mesia K, Musuamba C, De Bruyne T, Apers S, et al. In vitro antiplasmodial activity of extracts and fractions from seven medicinal plants used in the Democratic Republic of Congo. J Ethnopharmacol. 2004;93(1):27–32.
Daskum AM, Godly C, Qadeer MA, Ling LY. Effect of Senna occidentalis (Fabaceae) leaves extract on the formation of β-hematin and evaluation of in vitro antimalarial activity. Int J Herb Med. 2019;7(3):46–51.
Garg V, Dhar VJ, Sharma A, Dutt R. Facts about standardization of herbal medicine: a review. Zhong Xi Yi Jie He Xue Bao. 2012;10(10):1077–83.
Ginsburg H, Deharo E. A call for using natural compounds in the development of new antimalarial treatments–an introduction. Malar J. 2011;10(1):1–7.
Sinha S, Sarma P, Sehgal R, Medhi B. Development in assay methods for in vitro antimalarial drug efficacy testing: a systematic review. Front Pharmacol. 2017;8:754.
Wells TN. Natural products as starting points for future anti-malarial therapies: going back to our roots? Malar J. 2011;10(1):1–12.
Woodrow CJ, Dahlström S, Cooksey R, Flegg JA, Le Nagard H, Mentré F, et al. High-throughput analysis of antimalarial susceptibility data by the WorldWide antimalarial resistance network (WWARN) in vitro analysis and reporting tool. Antimicrob Agents Chemother. 2013;57(7):3121–30.
WHO. WHO guidelines on good agricultural and collection practices (GACP) for medicinal plants: World Health Organization; 2003.
Bonkian LN, Yerbanga RS, Koama B, Soma A, Cisse M, Valea I, et al. In vivo antiplasmodial activity of two sahelian plant extracts on plasmodium berghei ANKA infected NMRI mice. Evid Based Complement Alternat Med. 2018;2018:6859632.
Okokon JE, Antia BS, Mohanakrishnan D, Sahal D. Antimalarial and antiplasmodial activity of husk extract and fractions of Zea mays. Pharm Biol. 2017;55(1):1394–400.
Gul R, Jan SU, Faridullah S, Sherani S, Jahan N. Preliminary phytochemical screening, quantitative analysis of alkaloids, and antioxidant activity of crude plant extracts from Ephedra intermedia indigenous to Balochistan. Sci World J. 2017;2017:5873648.
Trager W, Jensen JB. Human malaria parasites in continuous culture. Science. 1976;193(4254):673–5.
Bagavan A, Rahuman AA, Kaushik NK, Sahal D. In vitro antimalarial activity of medicinal plant extracts against plasmodium falciparum. Parasitol Res. 2011;108(1):15–22.
Tepongning RN, Lucantoni L, Nasuti CC, Dori GU, Yerbanga SR, Lupidi G, et al. Potential of a Khaya ivorensis–Alstonia boonei extract combination as antimalarial prophylactic remedy. J Ethnopharmacol. 2011;137(1):743–51.
Lima RB, e Silva LFR, Melo MR, Costa JS, Picanço NS, Lima ES, et al. In vitro and in vivo anti-malarial activity of plants from the Brazilian Amazon. Malar J. 2015;14(1):1–14.
Camara A, Haddad M, Reybier K, Traoré MS, Baldé MA, Royo J, et al. Terminalia albida treatment improves survival in experimental cerebral malaria through reactive oxygen species scavenging and anti-inflammatory properties. Malar J. 2019;18(1):1–15.
Tchatat Tali MB, Jiatsa Mbouna CD, Yamthe Tchokouaha LR, Tsouh Fokou PV, Tsakem Nangap JM, Keumoe R, et al. In vivo antiplasmodial activity of Terminalia mantaly stem bark aqueous extract in mice infected by plasmodium berghei. J Parasitol Res. 2020;2020:4580526.
Kweyamba PA, Zofou D, Efange N, Assob J-CN, Kitau J, Nyindo M. In vitro and in vivo studies on anti-malarial activity of Commiphora africana and Dichrostachys cinerea used by the Maasai in Arusha region, Tanzania. Malar J. 2019;18(1):1–6.
Waiganjo B, Moriasi G, Onyancha J, Elias N, Muregi F. Antiplasmodial and cytotoxic activities of extracts of selected medicinal plants used to treat malaria in Embu county, Kenya. J Parasitol Res. 2020;2020:8871375.
Valdés AF-C, Martínez JM, Lizama RS, Gaitén YG, Rodríguez DA, Payrol JA. In vitro antimalarial activity and cytotoxicity of some selected Cuban medicinal plants. Rev Inst Med Trop Sao Paulo. 2010;52:197–201.
Janse CJ, Ramesar J, Waters AP. High-efficiency transfection and drug selection of genetically transformed blood stages of the rodent malaria parasite plasmodium berghei. Nat Protoc. 2006;1(1):346–56.
Craig AG, Grau GE, Janse C, Kazura JW, Milner D, Barnwell JW, et al. The role of animal models for research on severe malaria. PLoS Pathog. 2012;8(2):e1002401.
Jambou R, El-Assaad F, Combes V, Grau GE. In vitro culture of plasmodium berghei-ANKA maintains infectivity of mouse erythrocytes inducing cerebral malaria. Malar J. 2011;10(1):1–5.
Atsbha GH, Balasubramanian R, Gebre AK. Antimalarial Effect of the Root of Silene macrosolen A. Rich (Caryophyllaceae) on Plasmodium-berghei-Infected Mice. Evid Based Complement Alternative Med. 2021;2021. ID 8833865.
Enechi OC, Amah CC, Okagu IU, Ononiwu CP, Azidiegwu VC, Ugwuoke EO, et al. Methanol extracts of Fagara zanthoxyloides leaves possess antimalarial effects and normalizes haematological and biochemical status of plasmodium berghei-passaged mice. Pharm Biol. 2019;57(1):577–85.
Heinrich M, Appendino G, Efferth T, Fürst R, Izzo AA, Kayser O, et al. Best practice in research–overcoming common challenges in phytopharmacological research. J Ethnopharmacol. 2020;246:112230.
Tona L, Mesia K, Ngimbi N, Chrimwami B, Okond'Ahoka CK, et al. In-vivo antimalarial activity of Cassia occidentalism Morinda morindoides and Phyllanthus niruri. Ann Trop Med Parasitol. 2001;95(1):47–57.
Dibessa TT, Engidawork E, Nedi T, Teklehaymanot T. Antimalarial activity of the aqueous extract of the latex of aloe pirottae Berger.(Aloaceae) against plasmodium berghei in mice. J Ethnopharmacol. 2020;255:112763.
Alehegn AA, Yesuf JS, Birru EM. Antimalarial activity of crude extract and solvent fractions of the leaves of Bersama abyssinica fresen.(Melianthaceae) against plasmodium berghei infection in Swiss albino mice. Evid Based Complement Alternat Med. 2020;2020. ID 9467359.
Njeru SN, Muema JM. In vitro cytotoxicity of Aspilia pluriseta Schweinf. Extract fractions. BMC Res Notes. 2021;14(1):1–4.
Cromer D, Evans KJ, Schofield L, Davenport MP. Preferential invasion of reticulocytes during late-stage plasmodium berghei infection accounts for reduced circulating reticulocyte levels. Int J Parasitol. 2006;36(13):1389–97.
Thakre N, Fernandes P, Mueller A-K, Graw F. Examining the reticulocyte preference of two plasmodium berghei strains during blood-stage malaria infection. Front Microbiol. 2018;9:166.
Ceravolo IP, Aguiar AC, Adebayo JO, Krettli AU. Studies on activities and chemical characterization of medicinal plants in search for new Antimalarials: a ten year review on Ethnopharmacology. Front Pharmacol. 2021;12:734263.
Habibi P, Shi Y, Fatima Grossi-de-Sa M, Khan I. Plants as sources of natural and recombinant Antimalaria agents. Mol Biotechnol. 2022;64:1–21.
Noronha M, Pawar V, Prajapati A, Subramanian R. A literature review on traditional herbal medicines for malaria. S Afr J Bot. 2020;128:292–303.
Kigen GK, Ronoh HK, Kipkore WK, Rotich JK. Current trends of traditional herbal medicine practice in Kenya: a review. Afr J Pharmacol Ther. 2013;2(1).
Pan S-Y, Zhou S-F, Gao S-H, Yu Z-L, Zhang S-F, Tang M-K, et al. New perspectives on how to discover drugs from herbal medicines: CAM's outstanding contribution to modern therapeutics. Evid Based Complement Alternat Med. 2013;2013:627375.
Uzor PF. Alkaloids from plants with antimalarial activity: a review of recent studies. Evid Based Complement Alternat Med. 2020;2020:8749083.
Zahari A, Ablat A, Sivasothy Y, Mohamad J, Choudhary MI, Awang K. In vitro antiplasmodial and antioxidant activities of bisbenzylisoquinoline alkaloids from Alseodaphne corneri Kosterm. Asian Pac J Trop Med. 2016;9(4):328–32.
Zhang Q-W, Lin L-G, Ye W-C. Techniques for extraction and isolation of natural products: a comprehensive review. Chin Med. 2018;13(1):1–26.
Laufer MK. Monitoring antimalarial drug efficacy: current challenges. Curr Infect Dis Rep. 2009;11(1):59–65.
Raz A. Plasmodium berghei infection in BALB/c mice model as an animal model for malaria disease research: Vaccine Design: Springer; 2022. p. 589–95.
Andrews KA, Wesche D, McCarthy J, Möhrle JJ, Tarning J, Phillips L, et al. Model-informed drug development for malaria therapeutics. Annu Rev Pharmacol Toxicol. 2018;58:567–82.
McCarthy JS, Marquart L, Sekuloski S, Trenholme K, Elliott S, Griffin P, et al. Linking murine and human plasmodium falciparum challenge models in a translational path for antimalarial drug development. Antimicrob Agents Chemother. 2016;60(6):3669–75.
Kotepui M, Piwkham D, PhunPhuech B, Phiwklam N, Chupeerach C, Duangmano S. Effects of malaria parasite density on blood cell parameters. PLoS One. 2015;10(3):e0121057.
Phillips A, Bassett P, Szeki S, Newman S, Pasvol G. Risk factors for severe disease in adults with falciparum malaria. Clin Infect Dis. 2009;48(7):871–8.
Al-Adhroey AH, Nor ZM, Al-Mekhlafi HM, Amran AA, Mahmud R. Antimalarial activity of methanolic leaf extract of Piper betle L. Molecules. 2010;16(1):107–18.
Monti D, Vodopivec B, Basilico N, Olliaro P, Taramelli D. A novel endogenous antimalarial: Fe (II)-protoporphyrin IXα (heme) inhibits hematin polymerization to β-hematin (malaria pigment) and kills malaria parasites. Biochemistry. 1999;38(28):8858–63.
Acknowledgements
We thank the staff members of the Department of Animal Sciences, Institute of Primate Research, for their valuable support in this work. We also acknowledge the support offered by Dr. Lucy Ochola of the Institute of Primate Research, Kenya.
Funding
This study was supported by a Government of Kenya grant awarded to Institute of Primate Research through the state Department of Culture and Heritage.
Author information
Authors and Affiliations
Contributions
S.M. conducted experiments, formal analysis and wrote the original draft of the manuscript. H.M. performed phytochemical screening. E.K. performed in vitro experiments. K.O. supervised the project and edited the manuscript. R.W. supervised the project and edited the manuscript. F.O. contributed in conducting in vitro experiments, supervision and manuscript editing. H.O. acquired funding, supervised the project and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval to conduct this study was granted by the Institute of Primate Research (IPR) Institutional Scientific and Ethics Review Committee (ISERC/02/18). The plant material used in this study was collected according to the WHO guidelines on Good Agriculture and Collection Practices (GACP) for medicinal plants. The handling and care of experimental mice was done in compliance with the international guidelines on the care and use of laboratory animals. In addition, the study was done based on the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines. The Institute of Primate Research facility is registered by the National Commission for Science, Technology and Innovation (NACOSTI), Kenya and accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International.
Consent for publication
Not applicable.
Competing interests
There are no competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Characteristics of Senna occidentalis roots extract and the percentage yields.
Additional file 2.
Growth inhibitory activity of Senna occidentalis root extracts against Plasmodium falciparum, in vitro.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mogaka, S., Molu, H., Kagasi, E. et al. Senna occidentalis (L.) Link root extract inhibits Plasmodium growth in vitro and in mice. BMC Complement Med Ther 23, 71 (2023). https://doi.org/10.1186/s12906-023-03854-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-023-03854-8