Abstract
Background
Herbal medicines are widely used in the world especially in developing countries. Pregnant women use herbal products to treat pregnancy related illnesses due to prior experience of herbal medicine use and easy accessibility of the products with less cost. However, herbal products could affect fetal growth and contribute to maternal and fetal morbidity and mortality. Herbal drug use during pregnancy is not well studied in Ethiopia specifically in northeast Ethiopia.
Methods
A cross-sectional survey was conducted among 254 pregnant women on antenatal care follow-up at Dessie referral hospital. Semi-structured questionnaires were used for data collection. After collection, data were coded, entered and analyzed by SPSS version 20. Chi squared test and Logistic regression were used to evaluate the association between dependent and independent variables.
Result
Among the total of 254 respondents, 130 (51.2%) used herbal drugs during current pregnancy. The most commonly mentioned reason for herbal drug use was “herbal medicines are accessible without prescription” (43.1%). The herbal medicines used were Ginger (Zingiber officinale Roscoe) (43.8%), followed by Garlic (Allium sativum L.) (23.8%), Damakese (Ocimum lamiifolium Hochst. ex Benth.) (21.5%) and Tena-adam (Ruta chalepensis L.) (10.8%). The indications for herbal drug use were nausea/vomiting (43.8%), headache (30.8%) and common cold (25.4%). The most commonly mentioned sources of information on herbal medicine were families and friends (80.0%) followed by neighbors (12.3%), and the most commonly cited sources of herbal products were market (67.7%) and self-preparation (20.0%). Being illiterate or having only primary school education (Adjusted Odds Ratio [AOR]: 3.717, 95% CI: 0.992-13.928), having secondary school education background (AOR: 3.645, 95% CI: 1.394-9.534), and poor monthly income (AOR: 7.234, 95% CI: 2.192-23.877) were the variables that showed significant association with herbal drug use during current pregnancy.
Conclusion
This study showed that half of the sampled pregnant women used herbal medicine during current pregnancy, and education status and monthly income level of the women were associated with herbal drug use.
Similar content being viewed by others
Background
World health organization revealed that about 80% of the population in developing countries rely on nonconventional medicine mainly of herbal sources in their primary healthcare [1]. Pregnancy is associated with different physiological changes resulting in various ailments. These pregnancy-related ailments often cause pregnant women to start self-medication including the use of herbal products [2]. However, research gaps and lack of regulatory framework on herbal medicines across sub-Saharan Africa are critical problems as herbal drug use during pregnancy raises several concerns of safety [3].
Reports have estimated that around 80% of the population in Africa use traditional medicines and about 85% of traditional medicine involves use of herbal preparations [4]. In Ethiopia, 80% of the population use traditional medicine [5], and more than 95% of traditional medicinal preparations are herbal products [6]. The wide use of herbal drugs may be due to easy accessibility, affordability and acceptability of folk medicines by the population in developing countries [7]. Pregnant women are one of those populations exposed to herbal medicine use due to pregnancy induced changes in normal physiology and pregnancy related ailments [5]. However, the use of herbal products during pregnancy has safety concerns. Exposure of pregnant women to herbal chemicals during pregnancy could affect maternal health and fetal development [8, 9]. For instance, a preliminary study in rats revealed that prenatal exposure to high dose of ginger results in increased fetal loss, increased fetal weight and bone maturation [10]. Though human studies are limited due to ethical reasons, some epidemiological studies on pregnant women indicated that herbal use could influence pregnancy outcomes including risk of abortion or preterm labor, presence of malformations, intrauterine growth and neonatal birth weight [11]. A study revealed that the use of Rhizoma coptidis for skin conditions during first trimester of pregnancy causes nervous system and external genital organ malformations in the offspring [12]. Moreover, use of Angelica sinensis and Petroselinum crispum for prevention of miscarriages during the first trimester was associated with connective tissue, eye and musculoskeletal congenital anomalies in the offspring [12]. Additional concerns including poor regulatory framework for manufacturing, importation and distribution, adulteration and lack of standardization of herbal preparations in Africa as well as herb-drug interactions make herbal medicine use risky for pregnant women [3, 13]. Similarly, available registered herbal products does not comply with good manufacturing practices as well as safety and efficacy principles as is required for conventional medicines [2, 14].
Advanced investigations on the potential benefits and risks of herbal product use during pregnancy require baseline data on the magnitude of herbal drug use during pregnancy and type of medicinal plants used. Nevertheless, data available on herbal drug use during pregnancy in Africa including Ethiopia is scarce. Herbal drug use including the specific medicinal plants used among pregnant women is not yet studied specifically in the northeast region of Ethiopia. As a result, this study was conducted to assess herbal medicine use and contributing factors among pregnant women on antenatal care follow-up at Dessie referral hospital.
Methods
Study area and period
The study was conducted at Dessie referral hospital, South Wollo zone in the Amhara region of Ethiopia. Dessie is a town of South Wollo zone located at 401 km from Addis Ababa. The total area of the town is about 15.08 km2 with a population of more than 610,000. In the town, there is one referral hospital which is the biggest service delivering referral hospital to the dweller of the town and surrounding community. The referral hospital has different departments and wards like outpatient department, surgical ward, medical ward and the emergency ward including the emergency service and follow up of chronic diseases like TB, DM and HIV AIDS. It also has antenatal care (ANC) department which provide services that can prevent, detect and treat risk factors early in the pregnancy. Data collection was conducted for one month from May 6 to June 5, 2019 at the ANC department of the hospital.
Study Participants
Study design
A cross sectional survey was carried out among pregnant women on ANC follow-up at DRH using semi-structured questionnaires.
Source and study population of the study: All pregnant women attending DRH were considered as the source population, and all pregnant women on antenatal care follow up at DRH during the data collection period (from May 6 to June 5, 2019) were considered as study population for the study.
Inclusion and Exclusion criteria
The inclusion criterion was being a pregnant woman with age greater than or equal to18 years. Pregnant women who were unable to hear or communicate and mentally disabled women were excluded from the study.
Sample size determination and sampling technique
Prevalence of herbal drug use during pregnancy at Hossana town, 73.1% [15], 95% confidence interval and 5% margin of error were used to calculate the sample size using the single proportion formula. Accordingly, the sample size was calculated to be 302. Since the total number of pregnant women attending ANC department of DRH was 1200, which is less than 10,000, reduction formula was used and the sample size was reduced to 242. Then, 5% contingency was added for possible nonresponse and the final sample size was calculated to be 254 pregnant women. Pregnant women attending the ANC clinic during the one month data collection period were included in the study. Thus, convenience sampling was the sampling technique employed in the study.
Study variables
Herbal medicine use is the dependent variable of this study. Age, Marital status, Number of children, Occupation, Monthly income, residence, Distance from health facilities, Stage of pregnancy and gravida are the independent variables that can possibly affect the dependent variable, herbal medicine use.
Data collection tool and procedure
Data were collected by using semi-structured interviewer administered questionnaire (Additional file 1). The data collection tool (questionnaire) was first prepared in English language based on the aim of the study using a questionnaire of previous similar study as a guide [16]. The questionnaire was then translated to Amharic language. The questionnaire has three sections; section I (Socio-Demographic Information), section II (Obstetrics Information) and section III (Herbal Medicine Use). Pretested data collection questionnaire papers were used for data collection. The aim of the research was mentioned to each study participant and informed consent was received before the data collection. Data were collected by graduating class pharmacy students of Wollo University. The list of local (Amharic) names of medicinal plants or herbs mentioned by the informants was submitted to the Biology department, Wollo University for authentication of the scientific name by the botanist.
Data quality control, processing and analysis
After the questionnaire is prepared, pretest was done for validity and reliability of the questionnaire. Content validity was used to evaluate the validity of the data collection tool. Cronbach’s alpha test was used to measure the reliability, and cronbach’s alpha coefficient was calculated to be >0.70. The data were cleared and checked every day for consistency and completeness.
After completing data collection, the collected data were coded, entered and analyzed using SPSS version 20. Chi squared test and Logistic regression (binary and multivariate) were used to evaluate the association between independent variables (associated factors) and herbal medicine use using COD and AOD at 95% confidence interval, and a P-value <0.05 was considered statistically significant. Variables that showed significant (p<0.05) association with herbal medicine use in the chi squared test were selected for binary logistic regression analysis. Then, variables with P value less than 0.25 in the binary logistic regression analysis were included in the multivariate analysis. Study variables were summarized in tables using frequencies and percentages.
Ethical consideration
Permission to conduct the study in DRH was requested with a formal letter from Wollo University. Ethical approval was received from the ethical review committee of college of medicine and health sciences, Wollo University (reference number, WU/1224/08/11) before data collection. Verbal informed consent was received from each study participant after clarifying the objective of the study. Confidentiality of the information obtained was ensured throughout the study.
Result
Socio-Demographic information of the study participants
A total of 254 pregnant women were included in this study with 100% response rate. Out of 254 pregnant women who participated in this study, 74% were in the 20-30 years of age group and most (97%) were married. Considering their occupation, 82 (32.3%) were self-employed and 81 (31.9%) were house wife. With regard to monthly income, 48.4% had a low income (1,381 to 6,900 Ethiopian birr). Concerning educational level; 49 (19.3%) of the respondents have primary education and 98(38.6%) respondents have secondary education background. Majority of respondents 251 (98.8%) were Amhara, and 138(54.3%) respondents were Muslims and 111(43.2%) were orthodox Christianity followers (Table 1).
Obstetric characteristics of the study participants
Among the 254 pregnant women interviewed 132 (52.0%) were gravida two and 67 (26.4%) were gravida one. Among the total of 187 respondents with gravida 2 and above, 140 (55.1%) had 1 child and 20 (7.9%) had abortion history, of which 10 (50.0%) were due to known illnesses and 9 (45%) were due to unknown causes (Table 2).
Prevalence of herbal medicine use among the respondents
Of the total respondents, 130 (51.2%) used herbal drugs during their current pregnancy, and 78 (30.9%) of them used during their second trimester. Additionally, 103 (40.6%) used herbal drug during their previous pregnancy (Table 3).
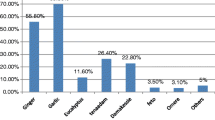
Indications of herbal products and the name of medicinal herbs used among respondents
The herbal products used were Ginger (Zingiber officinale Roscoe) (43.8%), followed by Garlic (Allium sativum L.) (23.8%), Damakese (Ocimum lamiifolium Hochst. ex Benth.) (21.5%) and Tena-adam (Ruta chalepensis L.) (10.8%). The reported indications for the herbal medicines were nausea/vomiting (43.8%), headache (30.8%) and common cold (25.4%) as presented in Table 4.
Source of information on herbal medicine and source of herbal products
The most commonly cited sources of information were families and friends (80.0%) followed by neighbors (12.3%), and the most common sources of herbs were market place (67.7%), followed by self-preparation (20.0%) (Table 5).
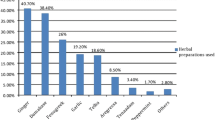
Reasons mentioned for herbal drug use
The most commonly mentioned reason for using herbal medicines was “herbal medicines are accessible without prescription” (43.1%), followed by “herbal medicines are effective than conventional medicines” (28.1%) (Table 6).
Reasons mentioned for not using herbal drugs
The most commonly mentioned reason for not using herbal medicine was “didn’t get sick during gestation” (46.3%), followed by “fear of the side effects” (26.8%) (Table 7).
All the herbal medicine users reported no undesirable response was experienced after the use of herbal products. Unfortunately, only 12.3% of the women responded that they were satisfied with the efficacy of the herbal products used.
Factors contributing to herbal medicine use
Independent variables that showed significant association with herbal drug use in the Chi Squared test and bivariate logistic analysis were further analyzed in multivariate regression. Finally, education level and average monthly income showed significant association (P < 0.05) with the dependent variable in multivariate regression analysis (Table 8). The odds of herbal drug use during current pregnancy was 3.717 times higher among illiterate and women with primary school education as compared to respondents with college diploma/degree (AOR: 3.717, 95% CI: 0.992-13.928), and the odds of herbal medicine use was 3.645 times higher among pregnant women with secondary school education as compared to women who have college diploma/degree (AOR: 3.645, 95% CI: 1.394-9.534). Similarly, women who were poor (monthly income less than 1,380 birr) were 7.234 times more likely to use herbal products than those who had middle monthly income of 6,901-13,000 Ethiopian birr (AOR: 7.234, 95% CI: 2.192-23.877). There was no statistically significant association (P > 0.05) between herbal medication use and occupation, place of residence, distance from health institution, number of gravid and number of children in multivariate logistic analysis.
Discussion
The findings of this study showed that 51.2% of the pregnant women at Dessie referral hospital, northeast Ethiopia used herbal medicine during their current pregnancy. This is almost equal to the prevalence reported in a study done at University of Gondar teaching hospital (northwest Ethiopia), 48.6% [16] and Nekemte hospital (west Ethiopia), 50.4% [5]. Additionally, prevalence of herbal drug use reported in the current study is within the range of 22.3 to 82.3% which was reported in a review of published literatures from Middle East countries [2]. In the contrary, prevalence of herbal drug use in the current study is lower compared to a study done at health facilities of Hosanna Town, Southern Ethiopia (73.1%) [15] and higher than the study done in Imo state of Nigeria (36.8%) [17]. The possible explanation for this might be differences in accessibility and affordability of herbal products and cultural differences among study participants.
This study showed easy accessibility, effectiveness, lower cost and fewer side effects of herbal medicines were the reasons mentioned by the respondents for using herbal drugs. This finding is in line with other studies carried out at Nekemte Hospital [5], health facilities of Hossana town [15] and a review of published literatures from Middle East countries [2] indicating similar reasoning for herbal drug use.
The current study revealed that Zingiber officinale, Allium sativum, Ocimum lamiifolium and Ruta chalepensis were the medicinal herbs used during pregnancy. This finding is comparable to the results of other studies conducted at Harar hosptals [18], Nekemte hospital [5], and health facilities of Hossana town [15] in Ethiopia and a tertiary Hospital in Northern Nigeria [19]. This implies similarity of herbal medicines utilized by pregnant women in different parts of Ethiopia as well as Africa.
According to this study, herbal drugs were used to treat nausea/vomiting, headache and common cold. The reasons mentioned for using herbal products were “herbal medicines are accessible without prescription, more effective than conventional medicines, have lower cost and safe during pregnancy”.
A randomized controlled trial which was done among pregnant women with symptoms of nausea and vomiting showed consumption of 1.5g of dried ginger for 4 days improves nausea and vomiting without affecting birth outcomes [20]. An experimental study on rats suggests the antiemetic effect of ginger may be largely due to its antagonistic effect on 5-HT3 receptor [21]. Similarly, a review of experimental and clinical studies showed Allium sativum L. has antioxidant, anti-inflammatory, antibacterial, antihypertensive, antidyslipidemic and anticancer activities [22]. However, experimental studies on animals showed embryotoxic effects of Ruta chalepensis [23] and Zingiber officinale [24, 25]. Additionally, pregnant women should avoid the use of garlic (Allium sativum) prior to surgery including caesarean section due to its anti-hemostatic effect which can lead to excessive bleeding [22, 26]. There is no pregnancy related safety data on Ocimum lamiifolium.
This study showed poor monthly income is significantly associated with herbal drug use during pregnancy. This finding is comparable with a study done at University of Gondar teaching hospital which states that respondents who had monthly income lower than 100 USD were 3.1 times more likely to use herbal products than those who had an income greater than 200 USD [16]. Similarly, poor monthly income was reported to be associated with herbal drug use in a study done at public hospitals in Harar town of Ethiopia [18]. This is possibly explained by affordability of herbal medicine compared to modern medical services as indicated in other similar studies conducted in different parts of Ethiopia [5, 15, 16, 18] and Nigeria [27].
The main problems with herbal products are contamination, miss-labeling and absence of standardized dose in developing countries like Ethiopia [28, 29]. Similarly, participants of this study found information from neighbors, friends and family and got the herbal medicines from market or prepare it by themselves. This implies there is no dose standardization and controlled framework for manufacturing and distribution of herbal products. This may expose pregnant women and their fetuses to harmful effects.
Limitation of the Study
Small sample size of this study may not reflect the average characteristics of pregnant women in the region. Thus, under-reporting of rarely used herbal medicines is expected. Additionally, this study is dependent on self-reported data which is subjected to bias.
Conclusion
This study showed that half of the pregnant women attending ANC follow up at DRH used herbal medicine during their pregnancy. Zingiber officinale, Allium sativum, Ocimum lamiifolium and Ruta chalepensis were the herbs used. Being illiterate, having only primary and secondary school education background, and poor monthly income were the major factors contributing to herbal medicine use. Though there is excessive utilization of herbal medications during pregnancy, safety of the herbs (Ocimum lamiifolium) to the embryo or fetus is unknown indicating the need for future experimental studies to evaluate teratogenicity of herbal drugs in animal models. Health care providers, who are involved in antenatal care, should be aware of evidences regarding potential benefits and harmful effects of herbal products during pregnancy, and they should provide health education to pregnant women.
Availability of data and materials
The questionnaire for data collection is available as additional file. The raw data are available from the corresponding author upon reasonable request.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COD:
-
Crude odds ratio
- DRH:
-
Dessie referral hospital
References
WHO. The Role of Traditional Medicine in Primary Health Care. In: Traditional Medicine and Health Care Coverage. World Health Organization, Geneva 1993:318-27.
John LJ, Shantakumari N. Herbal medicines use during pregnancy: a review from the Middle East. Oman Med J. 2015;30(4):229.
El Hajj M, Holst L. Herbal Medicine Use During Pregnancy: A Review of the Literature With a Special Focus on Sub-Saharan Africa. Front Pharmacol. 2020;11:866.
Falodun A. Herbal medicine in Africa-distribution, standardization and prospects. Res J Phytochemistry. 2010;4(3):154–61.
Bayisa B, Tatiparthi R, Mulisa E. Use of herbal medicine among pregnant women on antenatal care at Nekemte Hospital, Western Ethiopia. Jundishapur J Nat Pharm Prod. 2014;9(4).
Negero Gemeda AT. Biruktawit Girma. Frehiwot Teka. Traditional & Modern Medicine Directorate: Ethiopian Public Health Institute; 2015.
Elvin-Lewis M. Should we be concerned about herbal remedies. J Ethnopharmacology. 2001;75(2-3):141–64.
Kennedy DA, Lupattelli A, Koren G, Nordeng H. Herbal medicine use in pregnancy: results of a multinational study. BMC Complement Altern Med. 2013;13(1):355.
Westfall RE. Use of anti-emetic herbs in pregnancy: women's choices, and the question of safety and efficacy. Complement Ther Nurs Midwifery. 2004;10(1):30–6.
Hepner DL, Harnett M, Segal S, Camann W, Bader AM, Tsen LC. Herbal medicine use in parturients. Anesth Analg. 2002;94(3):690–3.
Cuzzolin L, Francini― Pesenti F, Verlato G, Joppi M, Baldelli P, Benoni G. Use of herbal products among 392 Italian pregnant women: focus on pregnancy outcome. Pharmacoepidemiol Drug Saf 2010;19(11):1151-1158.
Chuang C-H, Doyle P, Wang J-D, Chang P-J, Lai J-N, Chen P-C. Herbal medicines used during the first trimester and major congenital malformations. Drug safety. 2006;29(6):537–48.
Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 2014;4:177.
Holst L, Wright D, Haavik S, Nordeng H. The use and the user of herbal remedies during pregnancy. J Altern Complement Med. 2009;15(7):787–92.
Laelago T, Yohannes T, Lemango F. Prevalence of herbal medicine use and associated factors among pregnant women attending antenatal care at public health facilities in Hossana Town, Southern Ethiopia: facility based cross sectional study. Arch Public Health. 2016;74(1):7.
Mekuria AB, Erku DA, Gebresillassie BM, Birru EM, Tizazu B, Ahmedin A. Prevalence and associated factors of herbal medicine use among pregnant women on antenatal care follow-up at University of Gondar referral and teaching hospital, Ethiopia: a cross-sectional study. BMC Complement Altern Med. 2017;17(1):86.
Duru CB, Uwakwe KA, Chinomnso NC, Mbachi II, Diwe KC, Agunwa CC, et al. Socio-demographic determinants of herbal medicine use in pregnancy among nigerian women attending clinics in a tertiary hospital in Imo State, South-East, Nigeria. Am J Med Stud. 2016;4(1):1–10.
Jambo A, Mengistu G, Sisay M, Amare F, Edessa D. Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of Harar town, Ethiopia. Front Pharmacol. 2018;9:1063.
Omole-Ohonsi TI, A., and Fadare J. Use of herbal medicine among pregnant women attending a tertiary hospital in northern Nigeria. Int J Gynaecol Obstetrics. 2010;15(2).
Willetts KE, Ekangaki A, Eden JA. Effect of a ginger extract on pregnancy induced nausea: A randomised controlled trial. Aust N Z J Obstet Gynaecol. 2003;43(2):139–44.
Vishwakarma S, Pal S, Kasture VS, Kasture S. Anxiolytic and antiemetic activity of Zingiber officinale. Phytotherapy Research: An International Journal Devoted to Pharmacological and Toxicological Evaluation of Natural Product Derivatives 2002;16(7):621-626.
Al Disi SS, Anwar MA, Eid AH. Anti-hypertensive herbs and their mechanisms of action: part I. Front Pharmacol. 2016;6:323.
De Sa RZ, Rey A, Argañaraz E, Bindstein E. Perinatal toxicology of Ruta chalepensis (Rutaceae) in mice. J Ethnopharmacol 2000;69(2):93-98.
MOALEM SA, Tafazoli M. Evaluation of teratogenic effects of Zingiber Officinale in mice. Niapour M, Iranian J Basic Med Sci. 2003.
Wilkinson JM. Effect of ginger tea on the fetal development of Sprague-Dawley rats. Reprod Toxicol. 2000;14(6):507–12.
Laelago T. Herbal medicine use during pregnancy: benefits and untoward effects. Herbal medicine. 2018.
Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009;9(1):53.
Boullata JI, Nace AM. Safety issues with herbal medicine. Pharmacotherapy: The Journal of Human Pharmacology and Drug. Therapy. 2000;20(3):257–69.
De Smet PA. Health risks of herbal remedies: an update. Clin Pharmacol Ther. 2004;76(1):1–17.
Acknowledgements
We are thankful to the staffs of Dessie referral hospital for their assistance during the data collection.
Consent to publish
Not applicable
Funding
No funding was obtained for this study
Author information
Authors and Affiliations
Contributions
YMB and SA were involved in the conception, design and write up of the study. TY was involved in the acquisition and analysis of data. All authors were equally involved in the interpretation of data. All authors read and approved the submitted version of the manuscript, and they have agreed to be accountable for the accuracy or integrity of any part of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the ethical review committee of college of medicine and health sciences, Wollo University. Additionally, verbal informed consent was received from each study participant before the data collection process. The verbal consent of each respondent was documented on the informed consent sheet of the questionnaire by the data collector (interviewer) after explaining the aim and significance of the study. The procedure of verbal consent was approved by the ethical review committee.
Competing interests
All the authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Questionnaire used for data collection
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Belayneh, Y.M., Yoseph, T. & Ahmed, S. A cross-sectional study of herbal medicine use and contributing factors among pregnant women on antenatal care follow-up at Dessie Referral Hospital, Northeast Ethiopia. BMC Complement Med Ther 22, 146 (2022). https://doi.org/10.1186/s12906-022-03628-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-022-03628-8