Abstract
Background
Mica drugs, a group of herbo-metallic traditional preparations comprising biotite mica as the major mineral ingredient, are prescribed for skin disorders and respiratory ailments and other chronic conditions in South Asian countries, particularly India and Sri Lanka. Mica-based drugs (Abhrak drugs) are subjected to unique and varied preparation procedures and the bioactivity of the drugs can be affected by drug-processing conditions, the ingredients used and the mica composition. The current study aimed to evaluate and compare, on the basis of their physical and chemical characteristics, the antimicrobial potential of two commercial mica drugs AbBb (Abhrak bhashma) and AbCh (Abhrak Chenhuram) and two mica drugs ABL1 (Abhrak Bhasma Laboratory Prepared 1) and ABL2 (Abhrak Bhasma Laboratory Prepared 2) prepared in the laboratory under different conditions.
Methods
Antimicrobial activity of all four drugs was assessed at 10 mg/ml concentration against Pseudomonas aeruginosa, Escherischia coli, Staphylococcus aureus, methicillin-resistant S. aureus (MRSA) and Candida albicans using well diffusion assay, agar dilution assay and Miles and Misra method. Major and trace metal constituents of the drug samples were measured using atomic absorption spectrometry. Mineralogical properties, bacteria-mineral interactions, morphological changes in microbes and the surface characteristics of the drugs were determined using X-ray diffraction (XRD) analysis and scanning electron microscopy (SEM).
Results
The drugs ABL1, ABL2 and AbBh exhibited antimicrobial activity against only Gram-positive organisms (S. aureus and MRSA) when tested with Miles and Misra method (broth method). Mineralogical studies (XRD) revealed that biotite mica was altered into secondary clay minerals and iron oxides in the commercial drug AbCh while the other three drugs had altered mica and iron oxide phases. The essential elements (Na, K, Ca and Mg) required for microbial functions were present in varying extents in all four drugs while they were present in exceedingly high amounts in AbCh having comparatively high cation-exchange capacity, consistent with the observation that AbCh was inactive against all the microbes tested. The three drugs (ABL1, ABL2 and AbBh) showing antimicrobial activity contained comparatively high amounts of Fe, Zn and Cu that are known to display antimicrobial properties at high concentrations. SEM studies revealed that the drug particles adhered and entrapped the bacterial species, presumably modifying the physiochemical characteristics of the bacteria and eventually causing lethality.
Conclusion
Three of the four mica drugs inhibited the tested Gram-negative bacteria and the antibacterial activity of the mica drugs depends on their constituents and the methods of preparation.
Similar content being viewed by others
Introduction
The increasing antibiotic resistance exhibited by pathogenic microbes has prompted efforts to discover new antimicrobials covering a diverse range. Researchers have increasingly paid attention towards traditional medicine, to find out novel sources of antimicrobials [1, 2]. From ancient times, mankind has discovered the healing potential of certain minerals against microbes besides the use of herbs as medicine [3,4,5]. The use of minerals for healing purposes is widespread in Indian, Chinese and African traditional medicinal systems [6, 7].
‘Mica Ash’ is an example for a herbo-metallic traditional preparation comprising biotite mica (as the major mineral ingredient), plant materials and other ingredients. Mica ashes (drugs) are prescribed in traditional medicines in South Asian countries (specially in India and Sri Lanka) for skin disorders, respiratory and other chronic diseases [8, 9].
Although mica drugs are being constantly used in alternative medicinal applications, their importance for the development of allopathic drugs has not been sufficiently assessed. Some of the limitations such as inert nature of mica and poor bioavailability can hinder the use of mica in drugs. Further, there can be risks associated with prolonged oral administration of mica drugs due to the presence of toxic metal constituents in the raw materials [10, 11].
Nevertheless, utilization of ground mica or synthesized mica products in modern cosmetics [12, 13] implies their potential dermatological applications in treating diseases caused by microorganisms. The current study attempts to analyze the possible topical applications of selected mica-based traditional formulations, for the potential of these drugs to be developed as antimicrobial agents.
It is well known that the cationic constituents, surface nature and cationic exchange properties of minerals can influence their antimicrobial properties [14,15,16]. Evaluation of antimicrobial properties of mica ash products is important because mica ashes consist of nano- to micro-scale particles, which are enriched with cations possessing antimicrobial activity [17, 18].
However, antimicrobial properties of mica ash-based drugs can depend on the conditions involved in traditional drug-processing techniques [17, 19] the composition of mica and the other ingredients [4]. Moreover, these techniques and ingredients are not adequately specified for commercial products. The main objective of the current study was to evaluate antimicrobial activity of two commercial mica drugs and two drugs prepared in the laboratory under variable conditions, against Gram-positive and Gram-negative bacteria and a fungal species, and to seek correlations with constituent cations, surface morphology and cation-exchange capacity of the drugs.
Materials and methods
Drug samples
Two ‘Rasashastra’ drugs, designated ABL1 (Abhrak Bhasma Laboratory Prepared 1) and ABL2 (Abhrak Bhasma Laboratory Prepared 2), were prepared in the laboratory, using biotite mica as the mineral ingredient. Biotite mica was subjected to specific alteration processes as in traditional preparations [20], which included heating, quenching and incineration with additional ingredients. Table 1 summarizes the conditions employed in the preparation of drugs. A muffle furnace was used for heating the samples and cow’s urine for quenching. The drugs were ground using a ball mill (Fritsch Pulverisette) and particles less than 125 μm were used in the current study.
Two traditional mica drugs, namely Abhrak Bhasma (AbBh, a Rasashastra drug) and Abhrak Chenhuram (AbCh, a Siddha drug), were purchased from Dabur India Ltd. and Indian Medical Practitioners’ Co-operative Pharmacy and Stores Ltd., respectively. According to traditional medical records, the method of preparation for AbBh is different from that for AbCh although biotite mica was the mineral ingredient in both drugs [8, 21]. The organic and other inorganic ingredients used in the commercial drug preparations are unknown (Table 1).
Antimicrobial assays
Microbial strains
The microorganisms assessed included two Gram-positive bacteria [Staphylococcus aureus (ATCC 25923) and methicillin-resistant Staphylococcus aureus (MRSA)], two Gram-negative bacteria [Pseudomonas aeruginosa (ATCC-27853) and Escherichia coli (ATCC 25922)] and one fungal species Candida albicans (ATCC 90028), which were obtained from the culture collection of the Department of Microbiology, Faculty of Medicine, University of Peradeniya, Sri Lanka.
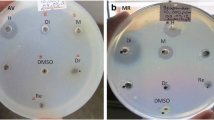
Preliminary semi-quantitative assays (well diffusion and agar dilution assays)
All four drugs were assessed for antimicrobial activity using the well diffusion assay and agar dilution assay. Fine powders of the drugs were suspended separately in diluted dimethyl sulfoxide (1:7, DMSO:water). Each drug and its components were tested (at 10 mg/ml concentration) against the microbes mentioned above. Inoculum of each microbial strain was prepared by suspending the respective 18- to 24-h old culture in aqueous NaCl (0.85%). Turbidity of each inoculum was adjusted to 0.5 McFarland standard.
Well diffusion assay for each microbial strain was done by flooding the inoculum onto the surface of a Petri plate containing 25 ml of Mueller-Hinton agar (MHA). Wells were bored into agar using a sterile cork borer with a diameter of 9 mm. The bases of the wells were sealed by adding a drop of molten agar into each well. Aliquots (180 μl) of the drug suspensions (10 mg/ml) were added into separate wells. After incubation overnight at 37 °C, the plates were examined for zones of inhibition. Diluted DMSO was used as the negative control.
Agar dilution plates were prepared by mixing sterilized and cooled molten agar with each drug separately. Final concentration of each drug was 10 mg/ml in each test plate. Agar plates containing the drugs were kept until solidified and 5 μl suspension from each organism was placed on the dried agar surface of each plate. After incubation overnight at 37 °C, the plates were examined for microbial growth on the drug bearing agar medium.
Quantitative antimicrobial assays (miles and Misra method)
Inoculated Brain Heart Infusion (BHI) broth cultures of turbidity similar to 0.5 McFarland standards of the above microorganisms were mixed with each drug (10,000 ppm = 10 mg/ml) and incubated at 37 °C for 18–24 h. The experimental vials were kept in a horizontal shaker during the time of incubation for thorough mixing of the drugs and to avoid deposition of drugs at the bottom of the growth medium. The antimicrobial activity of each drug was quantitatively investigated using Miles and Misra method for viability [22] after incubation as follows: a 100-μl aliquot from each of the experimental vials was serially diluted and 20 μl from each dilution was placed on MHA medium, which was designated into 6 sectors. The plates were incubated at 37 °C for 24 h. After incubation, colony forming units (cfu) were recorded in the respective dilutions of all the drugs.
The above experimental vials containing the broth and drugs were centrifuged for 1 min at 300 rpm [23] to enable drug particles to settle at the bottom of the vial; any settling of some of the microbes during centrifugation was common and considered almost same in all the vials including controls. The supernatants were used to determine the turbidity by means of absorbance at 625 nm, using UV-visible spectrophotometer (SHIMADZU-UV 1800). The antimicrobial experiments were replicated 3 times with an initial concentration of 10 mg/ml of each drug. Absorbance of the drug controls and the organism controls (organism without the drug) was measured to deduce the effective turbidity generated in the treated vials.
Mineralogical and chemical characterization
Mineralogical characterization of the drug samples was performed using Siemens D-5000 X-ray diffraction (XRD) instrument which was operated using CuKα radiation at 40 kV and 34 mA. Each drug sample was digested with hydrochloric, nitric, perchloric and hydrofluoric acids as described by Gaudino et al. [24, 25] for chemical analysis. Selected major and trace metal cation concentrations were measured on Perkin Elmer-2800 Atomic Absorption Spectrophotometer (AAS). The analyses were done in triplicates together with the reagent blanks and averaged values were used to compare the drug samples. Detection limits of AAS for the measured elements varied 0.01–0.004 ppm.
Cation-exchange Capacity (CEC)
The CEC was determined by mixing the drug samples (1.000 g) with an excess of 1 M sodium acetate solution (100 ml) to exchange with the mobile interlayer cations in the mica drugs. Na+-saturated samples were then washed three times with isopropyl alcohol to remove excess sodium ions. 1 M ammonium acetate solution (100 ml) was added to replace the adsorbed sodium ions with ammonium ions. The removal of sodium ions was assessed by AAS analysis [26].
Scanning Electron Microscopy (SEM) analysis
SEM analysis (SEM-EVO-LS15) of drug samples and bacteria was carried out separately and in combination to determine the bacteria-mineral interactions, morphological changes in microbes and the surface characteristics of the drugs. Prior to loading the samples for imaging, all the treated samples and untreated bacterial samples (blank) were fixed with formaldehyde at room temperature for 2 h, washed three times with sterilized water and dehydrated twice with an ethanol series (30, 50, 70, 80, 90 and 100%). The samples were kept at each ethanol solution for 10 min [27, 28]. To minimize artifacts during imaging, all samples were observed under variable pressure mode.
Assessment of cytotoxicity
To investigate the cytotoxicity of the four drugs, brine shrimp lethality bioassay [29,30,31,32] was carried out as follows: brine shrimps (Artemia salina) eggs were hatched in artificial seawater under continuous aeration for 48 h. After hatching, 10 nauplii were drawn through a glass capillary and placed in each vial containing 5 ml of brine solution to which the drug preparation was added. Each experiment was conducted along with the untreated shrimp control. All the tested brine solutions were maintained at room temperature under mild shaking conditions. Survival of brine shrimp nauplii at each concentration was recorded after 12, 18 and 24 h; experiments were conducted for different concentrations of the drugs ranging 1–10 mg/ml. All experiments were triplicated.
Results
Antimicrobial assays on the drugs
All four drugs did not show activity in the agar well diffusion assay (Fig. 1a) nor in the agar dilution assay. Inhibitory activity was observed with ABL1, ABL2 (Fig. 1b and c) and to a lesser extent with AbBh against S. aureus and MRSA in the Miles and Misra method (Table 2). AbCh did not exhibit antimicrobial activity. Although ABL1 and ABL2 were prepared from the same mica source, antimicrobial activity of the drugs showed different activity against S. aureus and MRSA, indicating that the ingredients used and the method of preparation influence the antimicrobial effect of the drug. None of the drugs showed antibacterial activity against P. aeruginosa, E. coli and C. albicans.
Absorbance measurements of the test organisms reflecting microbial density (Miles and Misra method) are given in Table 2. Reductions in absorbance were shown for S. aureus and MRSA by ABL1, ABL2 and AbBh indicating growth inhibition of bacteria. AbCh showed an increment in absorbance compared with the organism control for all the microbial species tested, indicating a growth enhancement rather than an inhibition.
Characterization of drug samples
Mineralogical characterization
XRD patterns (Fig. 2a-d) of drug samples showed that all the samples consisted of unaltered biotite mica and iron oxide as main crystalline phases. For each drug, the peak intensities of the phases varied reflecting the amounts of corresponding phases in a particular drug. Although biotite was a major ingredient in the preparation of all four drugs, its presence was clearly detected only in AbBh (Fig. 2c), which had been subjected to minimal thermal alteration (a single incineration cycle only). Other drug samples (ABL1, ABL2 and AbCh) showed minor amounts of unaltered biotite reflecting the modification of biotite during drug preparation. XRD patterns also indicate that the number of cycles of heating and incineration had influenced the formation of amorphous materials and some amounts of iron oxide phases. Further, the XRD data indicate that the mineral phases of ABL1 and AbCh (Fig. 2a and d) had been significantly altered and secondary clay minerals had been formed in AbCh (Fig. 2d).
Chemical constituents and Cation-Exchange Capacity (CEC)
Among the cations measured by AAS, the nutritional elements such as Na, K, Ca and Mg, required for microbial functions [33], were detected in all four drug samples (Fig. 3). However, these major ions were present in considerable amounts in AbCh that was inactive against microbes. All the active drugs showed significantly high Fe concentrations, while the inactive drug AbCh had low Fe concentration. The metals Zn, Mn, Cu, Sr and Pb were identified as trace metals in the drug samples. The concentrations of Mn and Zn were relatively high in ABL1. Relatively high amounts of Cu and Pb were present in the inactive drug AbCh. The CEC values of ABL1, ABL2, AbBh and AbCh were 8.6, 8.4, 9.4 and 45.6 meq/100 g, respectively, which can be arranged in decreasing order as follows: CECAbCh > CECAbBh > CECABL1 > CECABL2.
Analysis of interactions between bacteria and drugs by SEM
The interactions between bacteria and drug particles were observed by SEM. The electron micrographs of bacteria (S. aureus) treated with ABL1 are shown in Fig. 4. spherical -shaped cells (cocci) of untreated S. aureus were observed in the blank sample (Fig. 4b). However, aggregates of morphologically altered S. aureus (circled area in Fig. 4c) were embedded in mica ash. Further, some of the microbes were adhered to the surface of the mineral particles of ABL1 (Fig. 4d). Altered microbes were relatively flattened and elongated in shape (Fig. 4d) compared to the spherical -shape observed in the untreated S. aureus (Fig. 4b).
Cytotoxicity bioassay
None of the drugs caused time- or dose-dependent lethality to larvae in the brine shrimp cytotoxicity assay, indicating that the lethal dose of the water-soluble portion of the drugs is higher than that in the maximum amount of the drugs tested (10 mg/ml).
Discussion
Physical and chemical factors influencing antimicrobial activity of the drugs
SEM images reveal that S. aureus adhered to the surface of the active drug samples. Surface nature (surface roughness and charge) of the drug particles can influence the adhesion of the bacterial species to the surface of the drug particles [34]. Ion oxides are characterized by rough surfaces despite the smooth cleavage surfaces in mica and surface of clay minerals [17, 34, 35]. Therefore, the contact between mineral particles and the bacteria could be expected to be strong in the drugs that were rich in iron oxides (ABL1, ABL2 and AbBh) compared to AbCh that contained a relatively low amount of iron oxide (Fig. 3).
Electrostatic attraction between the microbes and the drug particles is another factor that would contribute to microbe lethality. Bacterial cell wall has a net negative charge both in Gram-positive and -negative bacteria due to the presence of teichoic acids (rich in phosphate), phospholipids and lipo-polysaccharides in their structure [33, 36]. Iron oxides on the other hand have a net positive charge over a wide range of pH [2,3,4,5,6,7] conditions. Negatively charged bacteria could readily adhere to the drug particles (ABL1, ABL2 and AbBh) that are rich in positively charged iron oxide sites [37, 38]. Drug particles of AbCh could be having a relatively low negative surface charge compared to the other drugs due to the presence of high fractions of clay minerals [39, 40]. The electrostatic repulsions between the microorganism and AbCh drug particles could be a factor contributing to the inactivity of AbCh drug.
Although electrostatic attractions could be expected in both Gram-positive and -negative bacterial species, the antimicrobial effect was observed in the current study only in Gram-positive bacteria. This difference in observation could be explained by the dissimilarities of Gram-positive and Gram-negative bacterial cell walls. The cell wall of Gram-positive bacteria has a thick layer of peptidoglycan while Gram-negative bacteria have a thick lipid bilayer on the outside, which is selectively permeable, in addition to the thin peptidoglycan layer. The peptidoglycan layers of Gram-positive bacteria are more permeable than the lipid bilayer of the Gram-negative bacteria. Due to this reason, Gram-positive bacteria are much more susceptible to antibiotics than Gram-negative bacteria [41,42,43,44]. Similarly, the antimicrobial cations (see below) of the drugs used in the current study are less likely to permeate through the lipid bilayer of Gram-negative bacteria than through the peptidoglycan layer of Gram-positive bacteria. Thus, the drugs were more effective against the Gram-positive organisms than the Gram-negative organisms. Further, drug permeability through the fungal membranes could be slower than the bacterial membranes due to the presence of the chitin cell wall in fungi, and this could be a reason for the drugs to be ineffective against C. albicans.
Although the physical properties of the drugs appear to influence antimicrobial activity, all the drugs were inactive when the tests were done using the solid growth media (well diffusion assay and agar dilution assay) probably due to the limited diffusion of material at a 10 mg/ml concentration. Chavadi [45] has observed antimicrobial activity of a mica drug at a much higher concentration (20 mg/ml) against S. aureus and E. coli by the well diffusion assay. Since the results of a diffusion assay could depend on the concentration and water-solubility of a particular antibiotic in addition to physical properties of the antibiotic, Chavadi’s results [45] observed in the well diffusion assay could be attributed to both physical properties and chemical constituents of the drugs. According to the results obtained in the current study where the broth dilution method (Miles and Misra) displayed antimicrobial activity (at 10 mg/ml), it could be that the drug particles were easily dispersed in water (broth) enabling better contact with the microbes when compared to the solid medium in the well diffusion assay.
When considering the antimicrobial results in relation to chemical constituents of the drugs, iron-rich drugs exhibited relatively high antimicrobial activity. Iron is present mostly as iron oxides in the drugs. However, the conventional iron oxide is not considered as an antimicrobial agent unless it is in the form of nanoparticles [36, 46]. In addition, iron oxides are known to be antibacterial when the metal ions are released to the bacterial environment in aqueous medium [1, 47]. The current results support the above contentions as the drugs showed their activity only when allowed to disperse in the aqueous BHI growth medium. This could be due to the greater interaction of drug particles with the microbes in liquid media. Further, antimicrobial cations released to the growth medium could easily penetrate through the bacterial cell wall in aqueous medium.
The CEC of a mineral indicates the amount of its exchangeable cations. If an antimicrobial mineral (specifically clay) carries effective antimicrobial cations, the mineral could act as a suitable antimicrobial agent; Fe2+, Zn2+, Mn2+, Cu2+ and Pb2+ cations have shown antimicrobial properties in previous studies [33, 48]. AbCh drug possess high CEC presumably due to the presence of significantly high clay fractions. However, its inactivity as well as growth enhancement in microorganisms indicate that the presence of relatively high amounts of exchangeable cations (Na+, K+, and Ca2+) in AbCh sustains and promotes the growth of rather than causing lethality to the microorganisms; Na+ ions are essential to the microorganisms for optimum growth [49] while Ca2+ and K+ ions can enhance the growth of microorganisms [50]. Hence, the antimicrobial activity of the investigated drugs of the current study is determined by their physical and chemical properties.
The doses of the drugs that are lethal to brine shrimp nauplii appear to exceed the 10 mg/ml level. Therefore, the water soluble preparations of the drugs at a concentration of 10 mg/ml could be used as promising antimicrobial agents devoid of cytotoxicity.
Effect of the preparation technique of the drug on antimicrobial activity
Since the major mineral ingredient (biotite mica) used in the drug preparation was common to the four drugs, the differences in antimicrobial activity of the drugs could be due to the differences in the other ingredients used, and/or the method of drug preparation. The CEC, cationic constituents and mineralogical composition of the drug, which are important parameters for antimicrobial activity, depend on the preparation technique. Modern technology can be used to improve the traditional drug processing techniques to enhance the antimicrobial properties of mica drugs. This can be done in many ways, viz by increasing solubility and reducing particle size (nanometer range) of mica ash. Further, the antimicrobial properties of drugs with high CEC can be enhanced by the addition of cations such as Ag+, Cu2+, Zn2+ and Fe2+ which are known to have a high antimicrobial potential [16, 51].
Conclusions and recommendations
Three mica-based drugs (Abhrak Bhasma, two prepared in the laboratory and one procured commercially) exhibited antimicrobial activity against S. aureus and MRSA (Gram-positive organisms) in aqueous medium, indicating the potential of these drugs to be developed as antimicrobial agents. The drugs did not show antibiotic activity against Gram-negative bacteria investigated nor antifungal activity against C. albicans. All four drugs were similar in terms of mineralogical composition. Chemical variables due to the method of drug preparation were significant, either to inhibit or promote microbial growth. Antimicrobial activity vs. cation exchange capacity showed an inverse relationship due to the ease of releasing cations from the drugs, which enhances microbial growth. Surface morphology and the preserved original platy nature of biotite in the drug particles can influence the adhesion and trapping of the bacterial species. Therefore, it could be stated that products based on mica ash exerted their lethal activity on bacteria by modifying the physiochemical characteristics directly through surface interactions or indirectly by changing the chemical properties of the growth medium. Antimicrobial parameters of the drugs such as particle size, aqueous solubility of antimicrobial cations and inducibility of morphological perturbations in microbial organisms should be further investigated to expound the inhibitory mechanisms and to grasp the full potential of mica-based drugs in clinical applications. Consistent antibacterial efficacy of the drugs should be ensured by standardization of the composition of raw materials and the techniques. Based on the results, it can be concluded that, antimicrobial activity of mica drugs could differ with the constituents of each drug and the method of preparation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AbBh:
-
Abhraka Bhasma
- AbCh:
-
Abhrak Chenhuram
- ABL1:
-
Abhrak Bhasma Laboratory Prepared 1
- ABL2:
-
Abhrak Bhasma Laboratory Prepared 2
- ATCC:
-
American Type Culture Collection
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- DMSO:
-
Dimethyl sulfoxide
- MHA:
-
Mueller-Hinton agar
- BHI:
-
Brain Heart Infusion
- cfu:
-
Colony forming units
- XRD:
-
X-ray diffraction
- AAS:
-
Atomic Absorption Spectrophotometer
- CEC:
-
Cation-exchange capacity
- SEM:
-
Scanning electron microscopy
References
Otto CC, Haydel SE. Exchangeable ions are responsible for the in vitro antibacterial properties of natural clay mixtures. PLoS One. 2013;8:1–9. https://doi.org/10.1371/journal.pone.0064068.
Williams LB, Metge DW, Eberl DD, Harvey RW, Turner AG, Prapaipong P, et al. What makes a natural clay antibacterial? Environ Sci Technol. 2011;45(8):3768–73. https://doi.org/10.1021/es1040688.
Finkelman RB. Health benefits of geologic materials and geologic processes. Int J Environ Res Public Health. 2006;3:38–342. https://doi.org/10.3390/ijerph2006030042.
Mishra LC. Scientific basis for Ayurvedic therapies. Boca Raton London New York Washington: CRC Press; 2004.
Williams LB. Antibacterial clays and their potential for medicinal applications. Italy: 4th International Conference on Medical Geology; 2011.
Limpitlaw UG. The medicinal uses of minerals, rocks, and fossils. Geol Soc Am Denver Annual Meeting. 2006;3(4):338-42.
Pan SY, Litscher G, Si-Hua G, Zhou SF, Yu ZL, Chen HQ, et al. Historical perspective of traditional indigenous medical practices: the current renaissance and conservation of herbal resources. Evid Based Complement Alternat Med. 2014:1–2. https://doi.org/10.1155/2014/525340.
Sathish R, Madhavan R, Hannah R, Vasanthi A. In-vitro alpha-glucosidase inhibitory activity of abraga chendhooram, a siddha drug. Int J Pharmacol Clin Sci. 2012;1:79–81.
Amrita M, Arun M, Ashoke G, Shivesh JS. Significance of mica in aurvedic products: an overview. IJRAP. 2011;2:389–92.
Taviad K, Galib Prashant B, Patgiri BJ. Metal toxicity of Ayurvedic drugs. National Seminar on Parada Vijnana. Jamnagar: Gujarat Ayurved University; 2014. p. 1–7.
Mikulski M, Wichman M, Donald L. Toxic metals in ayurvedic preparations from a public health lead poisoning cluster investigation. Int J Occup Environ Health. 2017:187–92. https://doi.org/10.1080/10773525.2018.1447880.
Moitra S, Bandyopadhyay A, Moitra S. Mica pneumoconiosis: a neglected occupational lung disease. Lancet. 2018;8:39. https://doi.org/10.1016/S22132600(18)301784.
Becker LC, Bergfeld WF, Belsito DV, Hill RA, Klaassen CD, Daniel CL. Safety assessment of synthetic Fluorphlogopite as used in cosmetics. Int J Toxicol. 2015;34:43–9. https://doi.org/10.1177/1091581815613513.
Wijenayake AU, Abayasekara CL, Pitawala HMTGA, Bandara BMR. Antimicrobial activity of two herbometallic rasashastra drugs. BMC Complement Altern Med. 2016;16:365. https://doi.org/10.1186/s12906-016-1336-1.
Williams LB, Haydel SB, Giese RF, Eberl DD. Chemical and mineralogical characteristics of french green clays used for healing. Clay Clay Miner. 2008;56:437–52. https://doi.org/10.1346/CCMN.2008.0560405.
Guo T, Cao S, Su RS, Li Z, Hu P, Xu Z. Adsorptive property of Cu2+-loaded montmorillonite clays for Escherichia coli K88 in vitro. J Environ Sc. 2011;23:1808–15. https://doi.org/10.1016/S1001-0742(10)60651-1.
Wijenayake AU, Pitawala HA, Bandara BMR, Abayasekara CL. Mineralogical and chemical changes of biotite mica during the alchemical pharmaceutical preparations, vol. 18: Peradeniya University International Research Session. Sri Lanka: University of Peradeniya; 2014. p. 487.
Wijenayakea A, Pitawala A, Bandara R, Abayasekara C. The role of herbometallic preparations in traditional medicine - a review on mica drug processing and pharmaceutical applications. J Ethnopharmacol. 2014;155:1001–10. https://doi.org/10.1016/j.jep.2014.06.051.
Pitawala A, Fernando GWR, Weerasinghe C. Chemical and structural changes in biotite during preparation of Ayurvedic medicine. J Geol Soc Sri Lanka. 2009;13:15–22.
Rama SMR. Bruhath Rasa Raja Saundaryya. Translated by Silva H.M. Publisher Department of Ayurveda Colombo.1964;25:113–127.
Kumar A, Nair GC, Reddy RV, Gar N. Bhasmas, unique aurvedic metallic-herbal preparations, chemical characterization. Biol Trace Elem Res. 2005;3:231–54. https://doi.org/10.1385/BTER:109:3:231.
George AT, Namasivayam SK, Raju S. Synthesis, characterization and anti bacterial activity of chitosan stabilized nano zero valant iron. Bull Pharm Med Sci. 2013;1:7–11.
Stevens K, Jaykus LA. Bacterial separation and concentration from complex sample matrices: a review. Crit Rev Microbiol. 2008:7–24. https://doi.org/10.1080/10408410490266410.
Gaudino S, Galas C, Belli M, Barbizzi S, Zorzi P, Jaćimovi R. The role of different soil sample digestion methods on trace elements analysis: a comparison of ICP-MS and INAA measurement results. Accred Qual Assur. 2007;12:84–93. https://doi.org/10.1007/s00769-006-0238-1.
Matusiewicz H. Wet Digestion Methods. Comprehensive analytical chemistry; 2003.
Donald SR, Ketterings Q. Recommended Methods for Determining Soil Cation Exchange Capacity. In: Recommended Soil Testing Procedures for the Northeastern United States. Northeastern Regional Publication: Cooperative Bulletin; 2011. p. 493.
Milani M, Drobne D, Tatti F. How to study biological samples by FIB/SEM? Modern Res Educ Topics Microscopy. 2007:787–94. Corpus ID: 44218830.
Kaláb M, Yang AF. Conventional scanning Electron microscopy of Bacteria. Infocus. 2008;10:44–61.
Sorgeloos P, Wielen CR, Persoone G. The use of Artemia Napulii for toxicity tests A crytical analysis. Ecotxicol Environ Saf. 1978;2:249–55. https://doi.org/10.1016/S0147-6513(78)80003-7.
Carballo JL, Hernández-Inda ZL, Pérez P, Garc MD. A comparison between two brine shrimp assays to detect in vitrocytotoxicity in marine natural products. BMC Biotechnol. 2002;2:17. https://doi.org/10.1186/1472-6750-2-17.
Meyer BN, Ferrigni NR, Putnam JE, Nicols JL. Brine shrimp: a convenient general bioassay for active plant constituents. Planta Med. 1982;45:31–4. https://doi.org/10.1055/s-2007-971236.
Wakawa HY, Fasihuddin BA. Brine shrimp leathality bio assay of Abrus precatorius (Linn) leaves and root. Int J Pharm Pharm Sci. 2017;9:179–81. https://doi.org/10.22159/ijpps.2017v9i1.15057.
Lemire JA, Harrison JJ, Turner RJ. Antimicrobial activity of metals: mechanisms, molecular targets and applications. Nat Rev. 2013;11:371–85. https://doi.org/10.1038/nrmicro3028.
Wang L, Hu C, Shao L. The antimicrobial activity of nanoparticles: present situation and prospects for the future. Int J Nanomedicine. 2017:1227–49. https://doi.org/10.2147/IJN.S121956.
Colombo C, Palumbo G, Ceglie A, Angelico R. Characterization of synthetic hematite (α-Fe2O3) nanoparticles using a multi-technique approach. J Colloid Interface Sci. 2012:118–26. https://doi.org/10.1016/j.jcis.2012.02.003.
Hajipour MJ, Ashkarran AA, Aberasturi DJ, Lrramendi IR, Serpooshan V, Parak WJ, et al. Antibacterial properties of nanoparticles. Trends Biotechnol. 2012:1–13. https://doi.org/10.1016/j.tibtech.2012.06.004.
Lower SK, Tadanier CJ, Hochella MF. Dynamics of the mineral–microbe Interface: use of biological force microscopy in Biogeochemistry and Geomicrobiology. Geomicrobiol J. 2001;18:63–76. https://doi.org/10.1080/01490450151079798.
Katsikogianni M, Missirlis YF. Concise review of mechanisms of bacterial adhesion to biomaterials and of techniques used in estimating bacteria-material interactions. Eur Cell Mater. 2004;8. https://doi.org/10.22203/eCM.v008a05.
Sposito G, Skipper NT, Sutton R, Park S, Soper AK, Greathouse JA. Surface geochemistry of the clay minerals. Proc Natl Acad Sci U S A. 1999;30:3358–64. https://doi.org/10.1073/pnas.96.7.3358.
Maes A, Stul MS, Cremers A. Layer charge-cation-exchange capacity relationships in montmorillonite. Clay Clay Miner. 1979;27:387–92. https://doi.org/10.1346/CCMN.1979.0270510.
Enger ED, Ross FC, Bailey DB. Concepts in biology: McGraw-Hill Science/Engineering/Math. New York: Avenue of the Americas; 2003.
Jarlier V, Nikaido H. Mycobacterial cell wall: structure and role in natural resistance to antibiotics. FEMS Microbiol Lett. 1994:11–8. https://doi.org/10.1111/j.1574-6968.1994.tb07194.x.
Navarre WW, Schneewind O. Surface proteins of gram-positive bacteria and mechanisms of their targeting to the cell wall envelope. Microbiol Mol Biol Rev. 1999;63:174–229. https://doi.org/10.1128/MMBR.63.1.174-229.1999.
Vassallo A, Silletti MF, Faraone I, Milella M. Nanoparticulate antibiotic systems as antibacterial agents and antibiotic delivery platforms to fight infections. J Nanomater. 2020:1–31. https://doi.org/10.1155/2020/6905631.
Chavadi VB. Antimicrobial activity of Abhraka Bhasma prepared with gomutra, for evaluation of its broad spectrum activity, an experimental study. Dissertation of Ayurveda Rasashastra and Bhaishajya Kalpana: Rajiv Gandhi University of Health Sciences; 2011. https://doi.org/10.21760/jaims.v2i05.10254.
Nigam S, Barick KC, Bahadur D. Development of citrate-stabilized Fe3O4 nanoparticles: conjugation and release of doxorubicin for the rapeutic applications. J Magn Magn Mater. 2011;323:237–43. https://doi.org/10.1016/j.jmmm.2010.09.009.
Franzblau RE. Metal ion adsorption onto bacteria-mineral composites. Electronic Theses and Dissertations, Ontario, Canada: University of Windsor; 2014.
Weinberg ED. The mutual effects of antimicrobial compounds and metallic cations. Bacteriol Rev. 1957;21:46. https://doi.org/10.1128/br.21.1.46-68.1957.
Valero A, Pérez-Rodríguez F, Carrasco E, Fuentes-Alventosa JM, García-Gimeno MR, Zurera G. Modelling the growth boundaries of Staphylococcus aureus: Effect of temperature,pH and water activity. Int J Food Microbiol. 2009;133:186–94. https://doi.org/10.1016/j.ijfoodmicro.2009.05.023.
Ataee RA, Derakhshanpour J, Mehrabi Tavana A, Eydi A. Antibacterial effect of calcium carbonate nanoparticles on agrobacterium tumefaciens. Iran J Milit Med Summer. 2011;13:65–70.
Williams LB, Haydel SE. Evaluation of the medicinal use of clay minerals as antibacterial. Int Geol Rev. 2010;52:745–70. https://doi.org/10.1080/00206811003679737.
Acknowledgments
Financial assistance by the HETC-Window 3 programme is gratefully acknowledged.
Funding
This research was funded by the grant from the Higher Eduction for Twenty first Centuary project of the Ministry of Higher Education, Sri Lanka. The funders had no role in the study design, data collection, analysis, decision to publish, preparation of the manuscript or for the providing of publication fee.
Author information
Authors and Affiliations
Contributions
Apsara Wijenayake conducted the chemical, mineralogical experiments and antimicrobial and toxicological assays. The same author also drafted the manuscript. Charmalie Abayasekara supervised antimicrobial assays and modified the manuscript. Amarasooriya Pitawala supervised the mineralogical and chemical studies and helped with the interpretation of chemical and mineralogical data. Ratnayake Bandara revised the manuscript critically and improved the study with new ideas. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wijenayake, A., Abayasekara, C., Pitawala, A. et al. Antimicrobial potential of four mica drugs and their chemical and mineralogical properties. BMC Complement Med Ther 22, 65 (2022). https://doi.org/10.1186/s12906-022-03545-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-022-03545-w