Abstract
Background
Icariin (ICA) can promote the migration and bone formation of bone marrow mesenchymal stem cells. This study explored a potential role of ICA in recruiting stem cell niches (SCNs) within the intervertebral disc region (ISN)-derived stem cells (ISN-SCs) to treat intervertebral disc degeneration (IVDD).
Materials and methods
EdU staining, transwell, and wound healing tests were used to analyze the function of ICA on ISN-SCs proliferation and migration ability. Simultaneously, the IVDD rat model was constructed by the acupuncture and divided into Sham, Sham + ICA, IVDD, and IVDD + ICA groups. H&E and PAS staining were performed to detect the pathological changes of IVDD tissues. Immunofluorescence was performed to discover relevant marker expression on the surface of stem cells in the IVDD tissues. Western blot and qPCR were executed to find the protein and mRNA expression of related cytokines in the IVDD tissues.
Results
ISN-SCs treated with 1 μM ICA obtained the better ability of proliferation and migration. H&E staining showed that the annulus fibrosus in the IVDD group was obviously hyperplasia with cavities and fissures; the nucleus pulposus was reduced. PAS staining showed that the content of polysaccharides was significantly reduced in the nucleus pulposus of IVDD group. However, the ICA treatment alleviated the pathological trends of the IVDD tissues. Simultaneously, ICA treatment increased significantly the expression of stem cells and IGF-1, TGF-β, SDF-1, CCL-5, Collagen I, Collagen II, Aggrecan, and SOX9 in IVDD tissues.
Conclusions
ICA treatment promoted the migration of stem cell in IVDD by increasing the expression of chemotactic cytokines, including IGF-1, TGF-β, SDF-1, and CCL-5.
Similar content being viewed by others
Background
Low back pain is one of the most common symptoms of orthopedic illness and a common public health problem related to lumbar intervertebral disc (IVD) degeneration (IVDD) [1, 2]. Over 80% of adults will indicate back pain in their lives, which is the most common cause of restricted mobility in people under 45 [3]. IVDD can be clinically manifested as spinal stenosis, axial back pain, radiculopathy, or myelopathy [4]. Severe IVDD not only disables the patient’s ability to work and affects the quality of life, but also brings a huge economic burden to society [5]. Therefore, it is very important to find an effective treatment for IVDD.
IVD in healthy people has a complex structure, including three different parts: central nucleus pulposus (NP); cartilaginous endplate (EP); and fibrocartilaginous annulus fibrous (AF) tissue and its inner and outer regions, consisted of concentric fibrous tissue layers [4]. Among them, AF contains abundant parallel collagen fibers, NP includes a gel-like matrix composed of abundant proteoglycan aggrecan and little collagen and elastin fibers, and EP contains a hyaline cartilage and round cartilage cells. These structures help the spine to restore its original shape after bending or stretching [4]. When IVDD occurs, the synthesis of glycosaminoglycan, proteoglycan, collagen II is reduced, but acidic pH and catabolic proteinases increase, resulting in the gradual loss of disc components and cell density [6]. Current treatments for IVDD include the administration of pain medications or surgical procedures, however, these methods have not achieved the desired therapeutic effect [7].
After understanding the internal mechanism of stem cell movement and migration, activating endogenous stem cells to restore and rebuild the IVDD is considered to be a better biological treatment and can avoid the trauma caused by surgical treatment in vivo [8]. Studies have shown that degenerated IVD tissue can recruit stem cells through the release of chemotactic cytokines, including transforming growth factor (TGF)-β, stromal cell-derived factor-1 (SDF-1), insulin-like growth factor 1 (IGF-1), chemokine C–C motif ligand (CCL) 5 [9,10,11,12]. Moreover, research has shown that icariin (ICA), is a flavonoid extract of several genus Epimedium species, prevents neuroinflammation and weakens oxidative stress damage [13], which shows the ability to enhance the bones and muscles, and can effectively enhance bone marrow mesenchymal stem cell (BMSC) osteogenesis and proliferation [14, 15]. ICA can also enhance the proliferation and of growth neural stem cells by regulating the expression of cell cycle genes and proteins [16]. In addition, ICA regulate gene expression to promote the proliferation of human neural stem cells, showing potential neuroprotective effect on nerve [17]. ICA also increase the function and of viability human NP-derived mesenchymal stem cells [18]. As shown above, ICA can promote the vitality and proliferation of various stem cells. Other studies have shown ICA has the protective function on human NP cells in IVDD through the nuclear factor erythroid 2-related factor 2 (Nrf-2) signaling [19]. ICA attenuates inflammatory response of human NP cells induced by interleukin-1β [20]. In addition, ICA can highly express TGF-β in BMSCs [21] and IGF-1 in mouse dermal papillary cells [22]. Therefore, this study hypothesizes that ICA may induce the migration of stem cells to repair degenerated IVD by promoting the expression of cytokines.
Recently, a potential stem cell niches within the IVD region (ISN) have been reported to play an important role in IVD regeneration [23]. In this study, ICA was used to study the role on the migration and proliferation of ISN-SCs cells. Western blot and qPCR were executed to analyze the protein and mRNA expression of related cytokines in the IVDD tissues treated with ICA to explore the potential mechanism for endogenous repair of IVDD and to offer a research basis for ICA in treating IVDD.
Methods
Isolation and identification of ISN-SCs
ISN-SCs were separated from 3-month-old male Wister rats (320–380 g, Guangdong Experimental Animal Center) according to the following procedure. The rats were euthanized after intraperitoneal injection of sodium pentobarbital (150 mg/kg). The functional spinal units of L8–L9 were isolated in the Wister rats. Then tissues of the ISN regions were isolated using the scalpel under sterile conditions [23] and were then digested by using 0.15% collagenase II in DMEM/F12 (1:1; Gibco, USA) including 3% fetal bovine serum (FBS) at 37 °C for 6 h. Before centrifuging for 5 min at 1000 rpm, the suspension was then filtered using a 70-μm cell strainer. The cell pellet was resuspended using DMEM/F12 added with 1% penicillin–streptomycin and 10% FBS and maintained in an incubator with 5% CO2 at 37 °C. When the ISN-SCs cultured to passage 4 (P4) for 24 h, cells were stained with CD29, CD90, CD44, CD45 and CD11b antibodies for 2 h and identified by the flow cytometry (BD, USA).
CCK-8 assay for cell viability
P4 ISN-SCs were plated in a 96-well plate with a density of 1 × 103 cells/well for reaching 60% confluency. Then, serum-free DMEM/F12 containing 0.1 μM, 1 μM, and 10 μM ICA were used to incubate cells. After incubation with ICA for 24, 48, and 72 h, CCK8 (7Sea Biotech, China) assay was executed to detect cell viability at 450 nm based on the protocol using the microplate reader (TECAN, Switzerland).
EdU staining for cell proliferation
P4 ISN-SCs were laid in a 24-well plate with a density of 3 × 103 cells/well for 24 h, incubated with serum-free DMEM/F12 containing different concentrations of ICA for 48 h, and treated with serum-free DMEM/F12 comprising 10 μmol/L EdU (RiboBio, China) for 2 h. The treated cells were fixed by 4% paraformaldehyde and stained by DAPI for 5 min. Cells were surveyed using a fluorescence microscope to evaluate the cell proliferation ability.
Cell migration ability
According to the manufacturer’s procedures, the six-well transwell chambers (Millipore) were used to study the cell migration. Briefly, 1 × 105 P4 ISN-SCs from serum-free DMEM/F12 were laid in the upper transwell chamber of insert for 24 h and treated with different concentrations of ICA, and 500 μL of DMEM/F12 supplemented with 10% FBS was added into the lower transwell chamber. The P4 ISN-SCs were cultured for 48 h. Then, P4 ISN-SCs were fixed in 100% methanol for 30 min and stained with 0.5% crystal violet (Sigma-Aldrich, USA) for 20 min. The migrating cells were observed under the fluorescence microscope. Simultaneously, P4 ISN-SCs were seeded in 24-well plates and P4 ISN-SCs layer was scratched using the tip of a 200 μL pipette. The wound width was observed for 48 h after the cells incubated with different concentrations of ICA to assess the healing ability of detected P4 ISN-SCs.
Phalloidin staining for filamentous actin
P4 ISN-SCs were cultured on coverslips and treated with different concentrations of ICA for 48 h. P4 ISN-SCs were fixed with 100% methanol for 30 min. Then, P4 ISN-SCs were permeabilized with 0.3% of Triton in PBS for 5 min and treated with 1% of bovine serum albumin (BSA, Sigma-Aldrich) in PBS for 30 min. Phalloidin-FITC (Sigma-Aldrich) together with DAPI (Sigma-Aldrich) was used for incubating P4 ISN-SCs for 1 h. Images were obtained using a confocal microscope (Zeiss, Germany) to evaluate the expression of filamentous actin (F-actin) in P4 ISN-SCs.
Construction and treatment of IVDD rat model
3 month-old Wister rats 320–380 g were selected to build rat model. The IVDD model was established by puncturing the 8th and 9th vertebrae with a needle of defined gauge with outer diameter of 0.45 mm. The needle was punctured from the skin to a depth of 6 mm through the NP. Before extraction, the needle was rotated 360° and stayed in place for 1 min. IVDD rat model was divided into Sham, Sham + ICA, IVDD, and IVDD + ICA groups and 12 rats in each group. When IVDD rats were intraperitoneally injected with ICA for 4 weeks and 8 weeks, they were used for subsequent experimental analysis.
Histopathological observation
Rats were killed to observe the pathological changes in the IVD of Sham, Sham + ICA, IVDD, and IVDD + ICA groups. The L8-9 IVD together with the adjacent bilateral half of the vertebral bodies in rats were harvested and fixed in 10% neutral buffered formalin for 48 h. 10% EDTA solution was used to decalcify for the IVD for three weeks and then paraffin was used to embed the tissue. Sections collected from the IVD samples embedded were stained with H&E and PAS staining and observed by microscope.
Immunofluorescence
Paraffin-embedded IVD tissues were dewaxed, and then antigen retrieval was performed. The slides were sealed using 1% BSA at 37 °C for 60 min; and incubated with primary antibodies (CD90: red; CD105: green). at room temperature for 2 h and followed by secondary antibodies at 37 °C for 90 min; and were dyed in DAPI for 5 min. All sections were sealed with cover glass and viewed using a confocal microscope (Zeiss, Germany).
qPCR
TRIzol reagent (Invitrogen, USA) was used to extract the total RNA of IVD tissues. qPCR was used to detected the mRNA expression. Reactions were executed in 50-µL volumes comprising SYBR Green PCR master mix through a GeneAmp PCR System 9600. Thermal cycling conditions was 40 cycles at a temperature of 95 °C for 30 s, a temperature of 60 °C for 30 s, and 72 °C for 2 min. Data were collected and analyzed. The mRNA expression was calculated by 2−ΔΔCT method. The primer sequences used in this study were listed in Table 1.
Western blot
The RIPA buffer (Solarbio Life Sciences, China) was used to extract the total protein of samples from IVD tissues, according to the protocol. The BCA Protein Assay Kit (Thermo Fisher Scientific) was used to measure protein contant. Approximately 25 μg of total protein was boiled, separated using 12% SDS-PAGE, and blotted onto PVDF membranes. Then the membranes were sealed with 5% skimmed milk for 2 h, incubated with primary antibodies against IGF-1 (1:1000, ab223567, Abcam, Cambridge, MA, USA), TGF-β (1:500, ab92486, Abcam), SDF-1 (1:1000, ab18919, Abcam), CCL-5 (1:1000, ab189841, Abcam), SOX9 (1:1000, ab26414, Abcam), Aggrecan (1:1000, ab3778, Abcam), Collagen I (1:1000, ab233080, Abcam), Collagen II (1:1000, ab188570, Abcam) and GAPDH (1:5000, ab22555, Abcam), followed by incubation with horseradish peroxidase-conjugated secondary antibody for 2 h at room temperature. Blots were visualized using a chemiluminescence reagent (Millipore, USA). GAPDH was the internal reference. The relative expressions of proteins were normalized to GAPDH using Image-Pro software. The antibody information used in this study were as follows.Western blot experimental results of the original film in the supplementary file 1.
Statistics
SPSS V16.0 software (IBM, USA) was used for statistical analyses. Differences among multiple groups were evaluated using one-way analysis of variance, followed by Dunnett’s test or Tukey’s test. P < 0.05 was considered a significant difference.
Results
Identification of ISN-SCs and the effect of ICA on ISN-SCs proliferation
To study the role of ICA in regulating stem cell migration for endogenous repair of IVDD, ISN-SCs were separated from 3-month-old male Wister rats. The flow cytometry was used to analyze the expression of P4 ISN-SCs surface antigens (Fig. 1A). The results showed that the positive expression of ISN-SCs positive markers, including CD29 (92.83%), CD90 (97.10%), and CD44 (96.10%), was about 100%, and the positive expression of ISN-SCs negative markers CD45 (3.34%) and CD11b (3.74%) was extremely weak, suggesting that ISC-SCs were successfully isolated (Fig. 1A). Regarding the function of different concentrations of ICA on the proliferation ability of ISN-SCs, the CCK8 assay showed that the proliferation abilities of ISC-SCs treated with 0.1 μM and 10 μM ICA for 48 h were significantly higher than those of ISC-SCs untreated with ICA for 48 h (Fig. 1B). In addition, compared to ISC-SCs treated with 0.1 μM or 10 μM ICA, ISC-SCs treated with 1 μM ICA obtained highest proliferation ability, and as time increased to 72 h, cell viability gradually increased (Fig. 1B). Simultaneously, EdU staining results also showed that ISC-SCs treated with 1 μM obtained highest proliferation ability (Fig. 1C). The above results indicated that 1 μM ICA had a better ability to promote cell proliferation.
The effect of ICA on proliferation of SCNs within the ISN-SCs. A CD29, CD90, CD44, CD45, and CD11b expression levels on ISN-SCs were detected by a flow cytometry. B The absorbance of ISN-SCs treated with different concentration of ICA for different time was detected at 450 nm by CCK-8 assay. Differences among multiple groups were evaluated using one-way analysis of variance, followed by Dunnett’s test. *** P < 0.001 vs. Control. C The proliferation ability of ISN-SCs treated with different concentration of ICA was determined by EdU staining
The effect of ICA on ISN-SCs migration and cytoskeleton formation
Based on the above research, we further studied the function of different concentrations of ICA on cell migration and skeletal formation. The transwell results indicated that the migration abilities of ISC-SCs treated with 0.1 μM and 10 μM ICA for 48 h were higher than those of ISC-SCs untreated with ICA for 48 h, moreover, ISC-SCs treated with 1 μM ICA obtained highest migration ability (Figs. 2A and D). The wound healing results showed that these cells incubated with 0.1 μM and 10 μM ICA were higher migratory than scrambled control at 48 h after scratching, more importantly, 1 μM ICA distinctively increased the cell migration of ISC-SCs (Figs. 2B and C). In addition, phalloidin staining results showed that ISC-SCs incubated with 1 μM ICA obtained the highest expression of F-actin (Fig. 3). These results implied that 1 μM ICA gained a better ability to promote cell migration and skeleton formation.
The effect of ICA on migration of SCNs within the ISN-SCs. A The migration ability of ISN-SCs treated with different concentration of ICA was estimated by transwell assay. B The healing ability of ISN-SCs treated with different concentration of ICA was estimated by wound healing for 48 h. C Semi quantitative analysis of healing ability of graph B. D Semi quantitative analysis of migration ability of graph A. Differences among multiple groups were evaluated using one-way analysis of variance, followed by Tukey’s test. * P < 0.05, ** P < 0.01, *** P < 0.001, and **** P < 0.0001
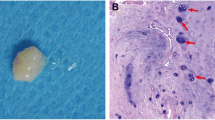
Pathological changes of IVDD tissue after ICA treatment
After in vitro cell experiments proved that ICA has a good ability to promote cell proliferation and migration, in vivo animal experiments were used to explore the therapeutic effect of ICA on IVDD through H&E and PAS staining. H&E staining showed that compared to Sham group, the AF in the IVDD group was obviously hyperplasia with cavities and fissures and the NP was reduced 4 weeks after the construction of IVDD rat model (Fig. 4A). PAS staining results showed that compared to Sham group, the content of polysaccharides was significantly reduced in the NP of IVDD group 4 weeks after the construction of IVDD rat model (Fig. 4B). However, the ICA treatment for 4 weeks alleviated the pathological phenomenon of the IVDD tissues, and with the treatment time extending to 8 weeks, the pathological changes of the IVDD tissue were significantly improved (Figs. 4A and B).
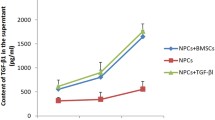
The potential mechanism of ICA on stem cell recruitment and treatment of IVDD
In this study, the potential mechanism of ICA to treat IVDD in rats was further studied. The immunofluorescence results showed that, for 4 weeks of ICA treatment, green and red fluorescence in IVD tissues of Sham + ICA group were stronger than those of Sham group and were no significant change compared to ICA applied to treated rats with IVDD for 8 weeks (Fig. 5A). And the green and red fluorescence in IVD tissues of IVDD were weaker than those of Sham group (Fig. 5A). In addition, for 4 weeks of ICA treatment, the green and red fluorescence in IVD tissues of IVDD + ICA group were stronger than those of IVDD group and were weaker than those in IVDD + ICA group with ICA applied to treated rats with IVDD for 8 weeks (Fig. 5A). Moreover, the protein and mRNA expression levels of IGF-1, TGF-β, SDF-1, CCL-5, SOX9, Aggrecan, Collagen I, and Collagen II in IVDD tissues of Sham group and Sham + ICA group 4 weeks after IVDD rat model were lower than those of Sham group and Sham + ICA group 8 weeks after IVDD rat model, and significantly higher than those of IVDD group 4 weeks after IVDD rat model (Figs. 5B and 6). Conversely, ICA treatment could greatly reverse the protein and mRNA expression of most related factors, including IGF-1, TGF-β, SDF-1, SOX9, Aggrecan, Collagen I, and Collagen II, in IVD tissues of IVDD group, and with ICA treatment to 8 weeks, the expression level of these factors gradually increased, suggesting that ICA might promote the repair of ISN-SCs in IVDD by increasing the expression of chemotactic cytokines, including IGF-1, TGF-β, SDF-1, and CCL-5 (Figs. 5B and 6).
The effect of ICA on the expression level of intervertebral disc stem cells (A) and mRNA (B) was detected by immunofluorescence and qPCR. CD90: red; CD105: green. Differences among multiple groups were evaluated using one-way analysis of variance, followed by Tukey’s test. *** P < 0.001 vs. Sham; and # P < 0.05, ## P < 0.01, and ### P < 0.001 vs. Sham + ICA
The effect of ICA on the protein expression level of intervertebral disc tissue was detected by western blot. Differences among multiple groups were evaluated using one-way analysis of variance, followed by Tukey’s test. ** P < 0.01, *** P < 0.001, and **** P < 0.0001 vs. Sham; and ## P < 0.01, ### P < 0.001, and #### P < 0.0001 vs. Sham + ICA
Discussion
Since the conception of SCNs was proposed [24], niches in various organs and tissues have been observed, containing the nervous, digestive, and respiratory systems, along with heart, bone marrow, skin, placental, and adipose tissues [25]. SCNs is consisted of extracellular matrix and other adjacent cells, which is a dynamic microenvironment that can balance the activities of stem cells to maintain tissue homeostasis and repair during the entire life cycle of organisms [25, 26]. The migration of niche endogenous stem cells to adjacent target areas is a key process of tissue self-healing. A potential SCNs, which is perichondrium region adjacent to the EP and outer zone of the AF, is shown the great significance in IVD regeneration processes [23, 27]. In this study, ISN-SCs were isolated and treated with 1 μM ICA obtained the better proliferation and migration. ICA treatment showed that obvious hyperplasia with cavities and fissures in the AF in the IVDD group and decreased polysaccharides in the NF of IVDD group were relieved and increased the expression level of stem cells in the IVDD tissues in vivo, suggesting that a potential role of ICA regulating stem cell migration for endogenous repair of IVDD.
Research shows that hypoxic preconditioning can upregulate the migration and proliferation of BMSCs in degenerated IVD and accelerate the effect of BMSC implantation in the treatment of IVDD [28]. ICA can improve metabolic dysfunction of long bone and also prevent bone loss caused by estrogen deficiency [29, 30]. ICA induces the growth and proliferation of neural stem cells by regulating mRNA and protein expression of cell cycle genes, including p21 and cyclin D1 [16]. ICA induces chondrogenic differentiation of BMSCs in self-assembling peptide nanofiber hydrogel scaffolds [31]. Simultaneously, CCK8, EdU and phalloidin staining, transwell assays showed that 1 μM ICA obtained a better proliferation, migration, and bone formation abilities for ISN-SCs, demonstrating that ICA had the ability to promote ISN-SCs migration and bone differentiation in this study.
The extracellular matrix of intervertebral disc mainly include type I and II collagen [32]. This collagen structure is also destroyed by proteolysis due to the maladjustment of collagenase activity, leading to the weakening of mechanical strength and the formation of non-enzymatic cross-linking between reducing sugars and the basic amino acids of collagen [33, 34]. With the degeneration of IVD and dehydration, most of the matrix develops with the decrease of elastin, aggrecan, and glycosaminoglycan, the increase of collagen and collagen cross-linking, and the fracture of aggrecan [35]. In addition, SOX9 is the transcription factor of aggrecan, which also plays a role in IVDD [36]. Simultaneously, our results showed that ICA treatment could reverse the mRNA and protein expression levels of Aggrecan, SOX9, Collagen I, and Collagen II in IVD tissues of IVDD group, demonstrating the role of ICA in repairing IVDD. Moreover, IGF-1 promotes BMSC migration and proliferation in myocardial infarction [37]. Integrin beta-like 1 enhances hepatocellular carcinoma cell invasion and migration via stimulating the TGF-β expression [38]. SDF-1 enhances BMSC migration [39] and NP cells can secrete CCL-5 that induces MSC chemotaxis [11]. In addition, our results showed that ICA treatment also could reverse the protein and mRNA expression levels of IGF-1, TGF-β, SDF-1, and CCL-5 in IVD tissues of IVDD group, and increase the stem cell expression levels, suggesting that ICA might promote the repair of IVDD by inducing chemokines.
Conclusions
In brief, ICA, the active component of traditional Chinese medicine Herba epimedii, promoted the migration of ISN-SCs to repair degenerated IVD by increasing the expression of chemotactic cytokines, including IGF-1, TGF-β, SDF-1, and CCL-5.
Availability of data and materials
The data obtained in this research are available from the corresponding author on reasonable request.
Abbreviations
- ICA:
-
Icariin
- SCNs:
-
Stem cell niches
- ISN:
-
Intervertebral disc region
- ISN-SCs:
-
Intervertebral disc region-derived stem cells
- IVDD:
-
Intervertebral disc degeneration
- TGF-β:
-
Transforming growth factor
- SDF-1:
-
Stromal cell-derived factor-1
- CCL-5:
-
Chemokine C–C motif ligand-5
References
Alzayed KA, Alsaadi SM. Efficacy of pulsed low-frequency magnetic field therapy on patients with chronic low back pain: a randomized double-blind placebo-controlled trial. Asian Spine J. 2020;14(1):33–42.
Özcan-Ekşi EE, Ekşi MŞ, Akçal MA. Severe lumbar intervertebral disc degeneration is associated with modic changes and fatty infiltration in the paraspinal muscles at all lumbar levels, except for L1–L2: a cross-sectional analysis of 50 symptomatic women and 50 age-matched symptomatic men. World Neurosurg. 2019;122:e1069–77.
Kadow T, Sowa G, Vo N, Kang JD. Molecular basis of intervertebral disc degeneration and herniations: what are the important translational questions? Clin Orthop Relat Res. 2015;473(6):1903–12.
Stergar J, Gradisnik L, Velnar T, Maver U. Intervertebral disc tissue engineering: a brief review. Bosn J Basic Med Sci. 2019;19(2):130–7.
Wei Q, Zhang X, Zhou C, Ren Q, Zhang Y. Roles of large aggregating proteoglycans in human intervertebral disc degeneration. Connect Tissue Res. 2019;60(3):209–18.
Zhang ZQ, Wang CS, Yang P, Wang KZ. Mesenchymal stem cells induced by microencapsulated chondrocytes on repairing of intervertebral disc degeneration. Orthop Surg. 2018;10(4):328–36.
Sharifi S, Bulstra SK, Grijpma DW, Kuijer R. Treatment of the degenerated intervertebral disc; closure, repair and regeneration of the annulus fibrosus. J Tissue Eng Regen Med. 2015;9(10):1120–32.
Huang Z, Zhang L, Feng X, Chen T, Bi S. A new in vivo method to retard progression of intervertebral disc degeneration through stimulation of endogenous stem cells with simvastatin. Med Hypotheses. 2017;101:65–6.
Kang SK, Shin IS, Ko MS, Jo JY, Ra JC. Journey of mesenchymal stem cells for homing: strategies to enhance efficacy and safety of stem cell therapy. Stem Cells Int. 2012;2012:342968.
Zhao Y, Zhang H. Update on the mechanisms of homing of adipose tissue-derived stem cells. Cytotherapy. 2016;18(7):816–27.
Pattappa G, Peroglio M, Sakai D, Mochida J, Benneker LM, Alini M, et al. CCL5/RANTES is a key chemoattractant released by degenerative intervertebral discs in organ culture. Eur Cell Mater. 2014;27:124–36.
Ma K, Chen S, Li Z, Deng X, Huang D, Xiong L, et al. Mechanisms of endogenous repair failure during intervertebral disc degeneration. Osteoarthritis Cartilage. 2019;27(1):41–8.
Liu B, Xu C, Wu X, Liu F, Du Y, Sun J, et al. Icariin exerts an antidepressant effect in an unpredictable chronic mild stress model of depression in rats and is associated with the regulation of hippocampal neuroinflammation. Neuroscience. 2015;294:193–205.
Yang A, Yu C, Lu Q, Li H, Li Z, He C. Mechanism of action of icariin in bone marrow mesenchymal stem cells. Stem Cells International. 2019;2019:5747298.
Qin S, Zhou W, Liu S, Chen P, Wu H. Icariin stimulates the proliferation of rat bone mesenchymal stem cells via ERK and p38 MAPK signaling. Int J Clin Exp Med. 2015;8(5):7125–33.
Fu X, Li S, Zhou S, Wu Q, Jin F, Shi J. Stimulatory effect of icariin on the proliferation of neural stem cells from rat hippocampus. BMC Complement Altern Med. 2018;18(1):34.
Yang P, Guan YQ, Li YL, Zhang L, Zhang L, Li L. Icariin promotes cell proliferation and regulates gene expression in human neural stem cells in vitro. Mol Med Rep. 2016;14(2):1316–22.
Chen S, Deng X, Ma K, Zhao L, Huang D, Li Z, et al. Icariin improves the viability and function of cryopreserved human nucleus pulposus-derived mesenchymal stem cells. Oxidative Medicine and Cellular Longevity. 2018;2018:3459612.
Hua W, Li S, Luo R, Wu X, Zhang Y, Liao Z, et al. Icariin protects human nucleus pulposus cells from hydrogen peroxide-induced mitochondria-mediated apoptosis by activating nuclear factor erythroid 2-related factor 2. Biochim Biophys Acta Mol Basis Dis. 2020;1866(1):165575.
Hua W, Zhang Y, Wu X, Kang L, Tu J, Zhao K, et al. Icariin Attenuates Interleukin-1β-Induced inflammatory response in human nucleus pulposus cells. Curr Pharm Des. 2018;23(39):6071–8.
Wu H, Zha ZG, Yao P. Experimental study of icariin in inducing bone marrow mesenchymal stem cell differentiation. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2010;30(4):410–5.
Su YS, Fan ZX, Xiao SE, Lin BJ, Miao Y, Hu ZQ, et al. Icariin promotes mouse hair follicle growth by increasing insulin-like growth factor 1 expression in dermal papillary cells. Clin Exp Dermatol. 2017;42(3):287–94.
Shi R, Wang F, Hong X, Wang YT, Bao JP, Cai F, et al. The presence of stem cells in potential stem cell niches of the intervertebral disc region: an in vitro study on rats. Eur Spine J. 2015;24(11):2411–24.
Schofield R. The relationship between the spleen colony-forming cell and the haemopoietic stem cell. Blood Cells. 1978;4(1–2):7–25.
Jedrzejas M, Skowron K, Czekaj P. Stem cell niches exposed to tobacco smoke. Przegl Lek. 2012;69(10):1063–73.
Voog J, Jones DL. Stem cells and the niche: a dynamic duo. Cell Stem Cell. 2010;6(2):103–15.
Liu C, Guo Q, Li J, Wang S, Wang Y, Li B, et al. Identification of rabbit annulus fibrosus-derived stem cells. PLoS One. 2014;9(9):e108239.
Wang W, Wang Y, Deng G, Ma J, Huang X, Yu J, et al. Transplantation of hypoxic-preconditioned bone mesenchymal stem cells retards intervertebral disc degeneration via enhancing implanted cell survival and migration in rats. Stem Cells Int. 2018;2018:7564159.
Xu H, Zhou S, Qu R, Yang Y, Gong X, Hong Y. Icariin prevents oestrogen deficiency-induced alveolar bone loss through promoting osteogenesis via STAT3. Cell Prolif. 2020;53(2):e12743.
Wei Q, Zhang J, Hong G, Chen Z, Deng W, He W, et al. Icariin promotes osteogenic differentiation of rat bone marrow stromal cells by activating the ERα-Wnt/β-catenin signaling pathway. Biomed Pharmacother. 2016;84:931–9.
Wang Z, Li K, Sun H, Wang J, Fu Z, Liu M. Icariin promotes stable chondrogenic differentiation of bone marrow mesenchymal stem cells in self-assembling peptide nanofiber hydrogel scaffolds. Mol Med Rep. 2018;17(6):8237–43.
Sun Y, Shi X, Peng X, Li Y, Ma H, Li D, et al. MicroRNA-181a exerts anti-inflammatory effects via inhibition of the ERK pathway in mice with intervertebral disc degeneration. J Cell Physiol. 2020;235(3):2676–86.
Hollander AP, Heathfield TF, Liu JJ, Pidoux I, Roughley PJ, Mort JS. Enhanced denaturation of the alpha (II) chains of type-II collagen in normal adult human intervertebral discs compared with femoral articular cartilage. J Orthop Res. 1996;14(1):61–6.
Pokharna HK, Phillips FM. Collagen crosslinks in human lumbar intervertebral disc aging. Spine (Phila Pa 1976). 1998;23(15):1645–8.
Scott JE, Bosworth TR, Cribb AM, Taylor JR. The chemical morphology of age-related changes in human intervertebral disc glycosaminoglycans from cervical, thoracic and lumbar nucleus pulposus and annulus fibrosus. J Anat. 1994;184:73–82.
Tan Y, Yao X, Dai Z, Wang Y, Lv G. Bone morphogenetic protein 2 alleviated intervertebral disc degeneration through mediating the degradation of ECM and apoptosis of nucleus pulposus cells via the PI3K/Akt pathway. Int J Mol Med. 2019;43(1):583–92.
Lin M, Liu X, Zheng H, Huang X, Wu Y, Huang A, et al. IGF-1 enhances BMSC viability, migration, and anti-apoptosis in myocardial infarction via secreted frizzled-related protein 2 pathway. Stem Cell Res Ther. 2020;11(1):22.
Huang W, Yu D, Wang M, Han Y, Lin J, Wei D, et al. ITGBL1 promotes cell migration and invasion through stimulating the TGF-β signalling pathway in hepatocellular carcinoma. Cell Prolif. 2020;53(7):e12836.
Guo K, Yao X, Wu W, Yu Z, Li Z, Ma Z, et al. HIF-1α/SDF-1/CXCR4 axis reduces neuronal apoptosis via enhancing the bone marrow-derived mesenchymal stromal cell migration in rats with traumatic brain injury. Exp Mol Pathol. 2020;114:104416.
Acknowledgements
None
Funding
This work was supported by Project of Administration of Traditional Chinese Medicine of Guangdong Province of China (No. 20191248). The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YQ and ZFZ conceived and designed the experiments, ZFZ, FWQ, YHF, CLX, HH, JJ, FJ and SNZ performed the experiments, CHS and SYH analyzed the data, ZFZ wrote the first draft, and YQ made the amendments and provided financial support. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All experimental protocols were performed according to the guidelines of the National Institutes of Health and were approved by the Institutional Animal Care and Use Committee of Sun Yat-sen University.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Z., Qin, F., Feng, Y. et al. Icariin regulates stem cell migration for endogenous repair of intervertebral disc degeneration by increasing the expression of chemotactic cytokines. BMC Complement Med Ther 22, 63 (2022). https://doi.org/10.1186/s12906-022-03544-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-022-03544-x