Abstract
Background
Commercial herbal medicines (CHMs) marketed as immune boosters are gaining wide popularity in South Africa, in the absence of control and regulatory guidelines. These commercially packaged and labelled herbal preparations, acquired in various retail outlets, are used without consulting either a conventional health provider or a traditional health practitioner. Although they are indicated for immune-boosting purposes, they might exert many other beneficial and unwanted effects on physiological systems. Platelets are crucial in haemostasis and important for the immunological system. The aim was to investigate the effect of the CHMs used to strengthen the immune system on the activity of human platelets.
Methods
Six CHMs commonly used as African traditional medicines in Pretoria, South Africa, were tested for their effects on healthy, isolated human platelets, using a bioluminescence method. The tested herbal medicines were Intlamba Zifo™, Maphilisa™ Herbal medicine, Matla™ African medicine for all diseases, Ngoma™ Herbal Tonic Immune Booster, Stametta™ Body Healing Liquid, and Vuka Uphile™ Immune Booster and serial-diluted standards of each from 10 to 10,000 times. The luminol-enhanced luminescence activity of the platelets was measured after incubation with the herbal medicines and activation with phorbol myristate acetate (PMA) or N-formyl-methionyl-leucyl-phenylalanine (fMLP).
Results
Five herbal medicines, namely Intlamba Zifo™, Maphilisa™ Herbal medicine, Matla™ African medicine for all diseases, Stametta™ Body Healing Liquid, and Vuka Uphile™ Immune Booster exerted comparable weak inhibitory effects on both PMA and fMLP-induced platelets, which were concentration dependent at high doses, and inversely related to concentration at low doses. Intlamba Zifo™, Matla™ African medicine for all diseases, Stametta™ Body Healing Liquid, and Vuka Uphile™ exhibited weak, but non-systematic stimulatory effects at low doses, which were not statistically significant. Ngoma™ Herbal Tonic Immune Booster had weak, inhibitory effects at high doses and weak stimulatory effects that were inversely related to concentration at low doses.
Conclusion
The findings suggest a potential beneficial role of the CHMs in the suppression of platelets’ reactivity and in enhancing the immune system. Caution, however, should be exercised as platelet inhibition and stimulation predispose to the risk of bleeding and thrombosis, respectively.
Similar content being viewed by others
Background
According to reports, a significant section of the population in South Africa (SA) uses the dual healthcare system, in which both the traditional and orthodox medicines are sought, depending on the sickness [1]. Herbal medicines (HMs), commonly used as traditional medicine (TM), are plant-based medicines either obtained from a traditional health practitioner or self-prepared as home remedies [2]. Currently, in SA, there is a growing use of commercially prepared herbal medicines sold in many retail outlets. These commercially packaged and labelled herbal preparations used as African TM (ATMs) are not regulated. There has been an upsurge of commercial herbal medicines (CHMs) that claim to strengthen the immune system. The CHMs are widely popular and are commonly found in various retail outlets such as muthi shops, pharmacies, health shops and some grocery stores. The CHMs in this study were part of the 10 most commonly sold in retail pharmacies in Pretoria, Gauteng, SA; and were selected on their use and commercial importance. They were indicated as immune boosters or intended to strengthen the immune system or the body [3]. It was perceived that the market for CHMs could be driven by the desire for urbanised populations to use TM but not having adequate time and means to produce the medicines. The self-medication with CHMs could also be from the perception that, as natural products, they signify purity, simplicity, and safety, and for the convenience of their availability without a prescription [4]. This market, therefore, will keep growing, as it is convenient regarding cost and time. Currently, in SA, there are no guidelines that govern the provision of information of the CHMs used as ATMs either on the label or package insert of these herbal mixtures. The information presented is solely at the discretion of the manufacturer and there, therefore, is no consistency in presentation.
CHMs can be described as products with medicinal properties that contain two or more plants or herbs that can act alone, in synergy, or additively in the restoration or maintenance of health [5]. In their use for immune-boosting purposes, the CHMs could affect many physiological systems and, therefore, inherently exert many other effects. One of the critical elements in physiology is platelets, and the functioning of these platelets could be affected by the many chemical molecules in CHMs through different biochemical pathways. Platelets are crucial in haemostasis and are significantly involved in the inflammatory and the immune responses [6, 7]. Studies have shown that they participate in immunoregulation by secreting chemical mediators and interacting with various immune and endothelial cells. They are furthermore regarded as potent effector cells of the innate immune system, while also acting as mediators between the innate and adaptive immune responses [8]. They are regarded as essential markers in disease pathophysiology, including cardiovascular [9] and inflammatory disorders [6, 8].
Platelet activity is modulated by various cell-surface receptors, as well as chemicals that directly stimulate intracellular biochemical molecules. Activated platelets release chemical substances such as reactive oxygen species (ROS), which include the superoxide anion (O2−), hydrogen peroxide (H2O2), and hydroxyl radicals (OH−) [9, 10]. Platelet ROS play a direct role in thrombosis [9] and directly and indirectly enhance the immune and inflammatory system [6, 8, 11]. Production of ROS because of platelet NADPH oxidase (NOX) action results in the emission of a burst of light termed chemiluminescence (CL), which can be measured in a luminometer [10]. The effects of common Western herbal medicines on platelets are known, and some of their mechanisms are well understood. This information is lacking for medicinal plants and herbal mixtures used as African traditional medicines.
The CHMs in this study contain some well-known African medicinal plants, including Aloe ferox, Siphonochilus aethiopicus, Hypoxis hemerocallidea, Sutherlandia frutescens, and Harpagophytum procumbens. The ethnobotanical uses of these plants are widespread, ranging from minor illnesses such as colds and headaches to serious conditions such as gastric ulcers and cancer. Various pharmacological and biological activities of the plants have been reported, including anti-inflammatory, immunomodulatory, and antioxidant activities [12]. There is no information about their activity on platelets. We investigated the effects of commonly used commercially available herbal mixtures on platelets using chemiluminescence measurements. We also explored whether the effects were mediated via a receptor-based or a non-receptor-based mechanism.
Methods
Reagents and instruments
A chemiluminescence assay, including the reagents used, was performed as described by Mothibe et al. [13] in an Orion™ L Microplate Luminometer supplied by Berthold Detection Systems.
The commercial herbal medicines and preparation
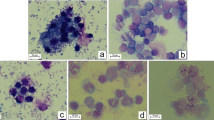
The CHMs selected were bought over the counter from a local pharmacy in Pretoria. The six CHMs denoted HM1 to HM6 were as follows: Intlamba Zifo™ (HM1), Maphilisa™ Herbal medicine (HM2), Matla™ African medicine for all diseases (HM3), Ngoma™ Herbal Tonic Immune Booster (HM4), Stametta™ Body Healing Liquid (HM5), and Vuka Uphile™ Immune Booster (HM6). Four serial dilutions of each of the six herbal mixtures were prepared, from 10x, 100x, 1000x to 10,000x with Hanks’ balanced salt solution (HBSS). Each neat herbal mixture (the undiluted CHM) and its diluted solutions were tested in triplicate in the luminometer. Figure 1 displays the pictures of the CHMs, and Table 1 shows the composition of each HM as it appears on the packaging or the product label.
Collection of blood samples
A qualified professional nurse collected blood samples from healthy adult volunteers. The self-declared healthy volunteers included males and females aged between 20 and 31 years. They were non-smokers, not on any prescribed medication, and had not been on self-medication, supplements, or any herbs or herbal mixtures for the 2 weeks before blood sample donation. Written information about the study was provided. Each volunteer signed a consent form after being informed of voluntary participation and guaranteed confidentiality of their details and the results. All ethical requirements were adhered to, including anonymity during the handling of samples.
Isolation of platelets
Approximately 10 ml of blood was collected from each volunteer in tubes with citrate preservative. Each sample was centrifuged at 1000 rpm (250 g) for 10 min. The plasma rich in platelets (PRP) was collected, onto which 40 μl of citric acid was added, mixed well and centrifuged at 2200 rpm (1000 g) for 10 min. After discarding the supernatant, the pellet was suspended in 4 ml of a tyrode plus ethylene diamine-tetra-acetic acid (EDTA) solution and allowed to stand for 10 min at room temperature. The suspension was centrifuged at 2200 rpm (1000 g) for six minutes. The supernatant was discarded, and the tyrode solution was added to the pellet to a final volume of 6 ml. A platelet count was performed at the Haematology division of the National Health Laboratory Services.
Luminescence procedure
The experimental process was as outlined by Mothibe et al. [13]. Briefly, each test well of a 96-well microplate was filled with 25 μl of the test solution of each HM and 25 μl of the platelet suspension. The control wells included 25 μl Hanks Balanced Salt Solution (HBSS) and 25 μl of the platelet suspension. Luminol (25 μl) was added to all the wells for amplification of the light signal. A 25 μl volume of either N-formyl-methionyl-leucyl-phenylalanine (fMLP) or phorbol myristate acetate (PMA) and HBSS was added to a final volume of 200 μl in each well. Luminol-enhanced luminescence (LEL) activity measurements of each sample were taken over a period of 60 min.
Data collection and handling
The platelet counts were corrected to 1 × 103 cells/μl for the LEL activity measured. The average LEL activity of the platelets was calculated per time interval, and the percentage inhibitions (% inh) for each HM standard was calculated and compared to the controls using the formula: \( \%\mathrm{inh}=\frac{\left({\mathrm{RLU}}_{\mathrm{ctrl}}\hbox{-} {\mathrm{RLU}}_{\mathrm{test}}\right)}{{\mathrm{RLU}}_{\mathrm{ctrl}}}\times 100 \)
where RLUctrl is the relative luminescence units (RLU) of the control, and RLUtest is that of the test samples. The % inhibitions were graded as weak (< 50%), moderate (50–79%) and potent (≥ 80%). This grading was adopted from a similar chemiluminescence study by Koko et al. [14]. For statistical analysis, the Microsoft Excel™ data analysis tool, t-Test Two sample Assuming Unequal Variance, was used. Where the p-value was less than or equal to 0.05, the results were declared as statistically significant.
Results
Figures 2, 3, 4, 5, 6 and 7 show the percentage inhibitions of the platelets at various time intervals exposed to each HM and its diluted standards, after they were activated with either fMLP (A) or PMA (B). Positive values (above zero) indicate inhibition effect and negative ones indicate stimulation effect. Each point is displayed as mean ± SD, and n = 8.
The HMs exerted inhibitory effects on both PMA- and fMLP-induced platelets, sustained over 60 min. When analysed per time interval, the effect ranged from weak to moderate inhibition (Figs. 2, 3, 4, 5, 6 and 7), with the magnitudes varying with the different concentrations of the HMs. There was also weak stimulation for all HMs at lower concentrations, except HM6, which was also moderate at the lower concentrations (Fig. 7).
Table 2 shows the calculated average % inhibitions of the HMs. The weak inhibitory effects were generally concentration-dependent when analysed from the neat, the 10x and 100x diluted standards of HM1, HM2, HM3, HM5, and HM6. When observed in the lower concentration standards (100x, 1000x and 10,000x diluted standards), the inhibitory effects were inversely related to the concentration for HM1 and HM2 in fMLP-induced platelets (A), and for HM1 (A), HM2 and HM5 (B) when studied between the 1000x and the 10,000x diluted standards. The stimulatory effects, when present, were non-systematic and were statistically not significant. The HM4 showed inhibitory effects in the neat and 10x diluted standards, and weak stimulatory effects, inversely related to the concentration in the 100x and 1000x standards.
Discussion
In this study, the in vitro luminescence activity of platelets over 60 min was determined after being exposed to various concentrations of HMs. This is a direct measure of the amount of light emitted because of the production of ROS by the NADPH oxidase system when platelets are stimulated. PMA and fMLP were used to stimulate the platelets to elucidate the mechanisms by which the ROS production is affected. While the two agonists result in the activation of the NOX system by protein kinase C (PKC), PMA directly activates PKC whereas fMLP acts indirectly by binding to specific G-protein-linked formyl peptide receptors on the membrane. The light emitted was compared to that of the controls and was expressed as a percentage (%) inhibition. The higher the value, therefore, the more the inhibition on platelets, and the lower the value, the less the inhibition, with negative values indicating stimulation.
The results in this study showed a general weak inhibitory effect by the HMs on both fMLP- and PMA-induced platelets at both high and low concentrations. There was also a weak stimulatory effect at low concentrations for some of the HMs (Table 1). In the case of inhibition in the presence of the HMs, the NOX system that resulted in the production of ROS could not be activated, either directly through PKC activation or indirectly by receptor activation. Compounds in the HMs interacted with the PKC and with the formyl peptide receptors on the membrane resulting in less production of ROS. In the case of stimulation, which occurred at lower concentrations, the presence of HMs slightly enhanced (weak stimulation) the activity of the platelets via both pathways. It meant that the HMs interacted with PKC and the formyl peptide receptors such that the activity of the platelets was increased, resulting in more production of ROS as compared to the controls. The inhibition and stimulation effects hence translate to antioxidant and pro-oxidant activities of the HMs, respectively. This study, therefore, reports the in vitro inhibition and stimulation of platelets’ activity by CHMs used as ATM, mediated via the PKC and formyl peptide receptor pathways.
Many African medicinal plants have been shown to have antioxidant properties [15]. Several compounds isolated from the plant parts were confirmed for various activities, including the anti-inflammatory, antioxidant, and immunomodulatory activities [12, 16, 17]. Flavonoids are the plant compounds proven to have an inhibitory effect on the respiratory burst (ROS production) of cells [18].
Inhibition and stimulation of platelets imply anticoagulant and pro-coagulant effects by the HMs, respectively. Platelet ROS play a direct role in thrombosis [9], and platelet activation and platelet reactivity affect haemostasis and thrombosis [19]. Increased platelet ROS is implicated in the development, progression and complications of several disorders, including cardiovascular conditions such as hypertension, atherosclerosis, diabetes mellitus and stroke [9, 20]. By stimulating platelets, the HMs in this study, therefore, could inadvertently play a role in increasing the risk of thrombosis and the development of the cardiovascular and inflammatory conditions. Antiplatelet medicines are the cornerstone of the prevention and management of the mentioned conditions [21]. It has been suggested that plant extracts could serve as alternatives to antiplatelet drugs [22]. In inhibiting platelet activity and reducing ROS production, the tested HMs could, therefore, have a role to play in the prevention and attenuation of the diseases. These opposing effects signify the importance of appropriate dosing, which is key to differentiating the beneficial and unwanted effects. The inhibition of platelet activity by the HMS occurring at low doses could mimic the way antiplatelet drugs are used long-term at low doses for their effects. The risk of bleeding is a known complication of antiplatelet drugs [23] as well as some herbal medicines such as garlic, ginkgo, and ginger [22, 24]. Likewise, the weak inhibition of platelets by the HMs, which was largely concentration-dependent, could increase the risk of bleeding in individuals who take the HMs. It was stated that high and low levels of inhibition of platelets are closely linked to the risk of bleeding events and ischaemic events, respectively [23].
Regarding the immune system and inflammatory response, generally, activated platelets secrete chemical mediators that enhance the interaction of platelets with other cells of the immune system, including the recruitment of neutrophils to inflammatory tissue and the formation of aggregates with neutrophils, monocytes and lymphocytes [6, 8, 25, 26]. The platelet-neutrophil (P-N) complexes perform immune functions such as phagocytosis, cytotoxicity, and cytolysis more effectively than neutrophils on their own [27]. The presence of platelet-derived ROS increased the recruitment of neutrophils to a growing thrombus [9]. Platelet-derived ROS and other chemical substances directly destroy pathogens [9, 10]; hence, the weak stimulation effect on platelets could be one of the many mechanisms by which the HMs enhance the immune system. The inhibition of platelets by the HMs could therefore, contribute to the impairment of the immune system and inflammatory processes.
Platelet-neutrophil interactions were implicated in the development and progression of diseases such as myocardial ischaemia and atherosclerosis [28]. Furthermore, interactions among leucocytes, endothelial cells and platelets were reported to contribute to inflammation, and subsequently to the pathogenesis of various inflammatory diseases. Pathways of platelet ROS were found to be involved in the airway inflammation of allergic reactions. For these reasons, it was suggested that suppression of platelet activity could be an alternative mechanism for the management of allergic conditions [8].
Many herbal medicines have well-known antiplatelet effects, attributed to the different plant compounds, including polyphenols [21, 22]. Similarly, the antiplatelet activity of the HMs in this study would be attributed to the various phytochemicals that are present, although not specifically identified nor quantified. All the HMs in the study except HM4 are water-based concoctions, which intones the presence of polar compounds. HM4 is the only alcohol-based mixture, signifying the presence of a wider polarity range of compounds.
The extraction of polyphenols from plant material requires the use of aqueous mixtures of organic solvents such as acetone, acetonitrile, methanol, and ethanol [29, 30]. Ethanol is deemed the best solvent to extract polyphenols, and it is safe for human consumption. Aqueous mixtures of the solvents generally provide a higher extraction yield than water and the pure solvents. Aqueous ethanol has shown a higher extraction yield than water [30]. It, therefore, signifies that HM4 contains more polyphenols compared to the other water-based CHMs, which would explain its effects that were dissimilar to the other HMs. This deviant behaviour was also observed in another study by Mothibe et al. [31].
Several phytochemicals have been isolated in the medicinal plants contained in some of the CHMs. The inhibitory and stimulatory effects of HM1, HM2, HM4, and HM5 could be ascribed to the aloe component of the HMs, since aloe has been proven, in vitro that it had antioxidant, anti-inflammatory and immunostimulatory activity [12, 32]. Compounds that have been isolated in aloe include flavonoids, alkaloids and bioactive compounds such as aloin, aloesin and aloemodin, dithranol and magnesium lactate [33]. L-canavanine, GABA and D-pinitol are compounds isolated from Sutherlandia, which forms a component of HM2 and HM4. Compounds present in H. hemerocallidea (African potato) could include secondary metabolites such as glycosides, polyphenols, saponins, steroids, tannins and its main compounds, hypoxoside and rooperol. The activity of Harpagophytum procumbens (devil’s claw) present in HM4 could be attributed to its glycosides [12]. Echinacea, alfalfa-lucerne (Medicago sativa), and dandelion (Taraxacum officinale) are well-known Western herbal medicines used mainly for immune-boosting effects. Many phytochemicals have been identified and isolated from these plants, including tannins, saponins, flavonoids, terpenoids, and phenolic compounds, which were proven for anti-inflammatory, antioxidant, immunostimulant and antithrombotic activities [17, 34]. The effects of the CHMs on the platelets, therefore, could be ascribed to the many compounds acting in synergy, additively, and possibly antagonistically. Both the antioxidant and the pro-oxidant activities of the CHMs reported in this study provide some rationale for using these medicines for their intended purpose. In a healthy physiological system, the production of ROS and the endogenous antioxidant defence mechanisms are in equilibrium. Disturbance of this balance results in oxidative stress and its associated harmful effects which include damage to biological macromolecules, leading to various pathologies [35, 36].
Polyphenols have been reported to target and block various platelet activation pathways, and therefore, had the potential to replace or complement antiplatelet therapy [36]. This study reports on additional pathways that are potential targets of polyphenols in platelets, namely the intracellular PKC pathway and the membrane-bound G-protein linked formyl peptide receptor pathway. The findings are in agreement with the report by Santhakumar et al. [36] that the antioxidant effect of polyphenols is achieved by the blockage of different receptors on the platelet surface that are responsible for platelet activation, and thereby, eliminating free radicals.
Several biochemical pathways in platelets are regulated by PKC and affect platelet physiology [19] while ROS are involved in various signal transduction mechanisms [20]. The platelet-enhancing and platelet-inhibiting effects, which occurred at high and low concentrations of the HMs, signify the potential for variable effects depending on the dose of the HM. These HMs are used for self-medication as immune boosters and the effects, therefore, highlight the possibility of herb-drug interactions (HDIs). The HDIs could occur if the HMs are used concomitantly with conventional medicines, particularly antiplatelet medicines such as NSAIDs.
The lifespan of platelets in circulation is on average 10–14 days. Because of their effects, it is generally recommended that herbal medicines be stopped before any surgical procedure, with periods ranging from one to 2 weeks before [24, 37,38,39]. The safety of the CHMs is not well-defined; however, based on the results obtained, it is recommended that using the CHMs in this study be stopped 14 days before any surgical procedure. It is also crucial that the consumers and healthcare providers be aware of the possible effects and the potential of interactions with other medicines.
Conclusion
The findings in this study show the in vitro antiplatelet and platelet-enhancing activities of CHMs used as ATMs at high and low concentrations. These activities were mediated via the intracellular PKC pathway and via the G-protein linked formyl peptide receptors on the membrane. Although the CHMs are commonly used as immune boosters, their diversity in composition renders their effects on platelets unpredictable. The findings suggest potential beneficial roles of the CHMs in the suppression of platelets’ reactivity and in enhancing the immune system. Caution, however, should be exercised, as platelet inhibition and stimulation predispose to the risk of bleeding and thrombosis, respectively.
Availability of data and materials
All the data that supported this article are presented in Figs. 2, 3, 4, 5, 6, 7 and Tables 1 and 2. The raw data sets that were analysed in the study are uploaded in the repository – Mendeley Data and is available at https://doi.org/10.17632/tvnyyz6t8w.1. The DOI is doi:https://doi.org/10.17632/tvnyyz6t8w.1
Abbreviations
- % inh:
-
Percentage inhibition
- ATM/s:
-
African traditional medicine/s
- CHMs :
-
Commercial herbal medicines/mixtures
- CL:
-
Chemiluminescence
- EDTA:
-
Ethylene-diamine-tetra-acetic acid
- fMLP:
-
N-formyl-methionyl-leucyl-phenylalanine
- H2O2 :
-
Hydrogen peroxide
- HBSS :
-
Hanks’ balanced salt solution
- HDIs:
-
Herb-drug interactions
- HM/s:
-
Herbal medicine/s
- LEL:
-
Luminol-enhanced luminescence
- NADPH :
-
Nicotinamide adenine dinucleotide phosphate
- NOX :
-
NADPH oxidase
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- O2 − :
-
Superoxide anion
- OH− :
-
Hydroxyl radical
- PKC:
-
Protein kinase C
- PMA:
-
Phorbol myristate acetate
- PRP:
-
Platelet-rich plasma
- RLU:
-
Relative luminescence units
- ROS:
-
Reactive oxygen species
- rpm:
-
Revolutions per minute
- SA:
-
South Africa
- SMUREC:
-
Sefako Makgatho Health Sciences University Research and Ethics Committee
- TM/s:
-
Traditional medicine/s
References
Mander M, Ntuli L, Diederichs N, Mavundla K. Economics of the traditional medicine trade in South Africa. South African Health Review [Health Systems Trust]. 2007; https://journals.co.za/docserver/fulltext/healthr/2007/1/healthr_2007_a16.pdf. Accessed 15 Apr 2018.
Cocks M, Moller V. Use of indigenous and indigenized medicines to enhance personal wellbeing: a south African case study. Soc Sci Med. 2002;54:387–97.
Mothibe ME. Knowledge and perceptions of community pharmacists about the commonly sold herbal medicines used as African traditional medicines in community pharmacies in Tshwane townships, South Africa. Afr J Phys Health Educ Recreat Dance. 2015;2(2):339–50.
Ndhlala AR, Van Staden J. Smokescreens and mirrors in safety and quality of herbal medicines: a case of commercialized herbal preparations. S Afr J Bot. 2012;82:4–10.
Gurib-Fakim A. Medicinal plants: traditions of yesterday and drugs of tomorrow. Mol Asp Med. 2006;27:1–93.
Ghoshal K, Bhattacharyya M. Overview of platelet physiology: its hemostatic and nonhemostatic role in disease pathogenesis. Sci World J. 2014;2014. https://doi.org/10.1155/2014/781857.
Trzeciak-Rycek A, Torkaz-Deptula B, Deptula W. Platelets- an important element of the immune system. Pol J Vet Sci. 2013;16:407–13.
Huang HS, Chang HH. Platelets in inflammation and immune modulations: functions beyond hemostasis. Arch Immunol Ther Exp. 2012;60:443–51.
Krotz F, Sohn H-Y, Pohl U. Reactive oxygen species: players in the platelet game. Arterioscler Thromb Vasc Biol. 2004;24:1988–96.
Nauseef WM. Detection of superoxide anion and hydrogen peroxide production by cellular NADPH oxidases. Biochim Biophys Acta. 1840;2014:757–67.
Miedzobrodski J, Panz T, Plonka PM, Zajac K, Dracz J, Pytel K, Mateuszuk L, Chlopicki S. Platelets augment the respiratory burst in neutrophils activated by selected species of gram-positive or gram-negative bacteria. Folia Histochem Cytobiol. 2008;46:383–8.
Street RA, Prinsloo G. Commercially important medicinal plants of South Africa: a review. J Chem. 2013. https://doi.org/10.1155/2013/205048.
Mothibe ME, Kahler-Venter C, Osuch E. In vitro effects of a commercial herbal medicine used as African traditional medicine on human neutrophils. Afr J Tradit Complement Altern Med. 2017;14:51–60.
Koko WS, Mesaik MA, Yousaf S, Galal M, Choudhary MI. In vitro immunomodulating properties of selected Sudanese medicinal plants. J Ethnopharmacol. 2008;118:26–34.
Fennel CW, Lindsey KL, McGaw LJ, Sparg SG, Stafford GJ, Elgorashi EE, Grace OM, Van Staden J. Assessing African medicinal plants for efficacy and safety: pharmacological screening and toxicology. J Ethnopharmacol. 2004;94:205–17.
Somova LI, Shode FO, Ramnanan P, Nadar A. Antihypertensive, antiatherosclerotic and antioxidant activity of triterpenoids isolated from Olea europaea, subspecies Africana leaves. J Ethnopharmacol. 2003;84:299–305.
Manayi A, Vazirian M, Saeidnia S. Echinacea Purpura: pharmacology, phytochemistry and analysis methods. Pharmacogn Rev. 2015;9(17):63–72.
Ciz M, Denev P, Kratchanova M, Vasicek O, Ambrozova G. Lojek A. Oxid Med Cell Longev: Flavonoids inhibit the respiratory burst of neutrophils in mammals; 2012. https://doi.org/10.1155/2012/181295.
Yeung J, Apopa PL, Vesci J, Kenyon V, Rai G, Jadhav A, Simeonov A, Holman TR, Maloney DJ, Boutaud O, Holinstat M. Protein kinase C regulation of 12-lipoxygenase-mediated human platelet activation. Mol Pharmacol. 2012;81:420–30.
El Haouari M, Rosado JA. Platelet signaling abnormalities in patients with type 2 diabetes mellitus: a review. Blood Cells Mol Dis. 2008;41:119–23.
NHM N, Othman F, ERM T, Noor SM. Medicinal herbals with antiplatelet properties benefit in coronary atherothrombotic diseases. Thrombosis. 2016. https://doi.org/10.1155/2016/5952910.
Cordier W, Steenkamp V. Herbal remedies affecting coagulation: a review. Pharm Biol. 2012;50:443–52.
Ferreiro JL, Sibbing D, Angiolillo DJ. Platelet function testing and risk of bleeding complications. Thromb Haemost. 2010;103:1128–35.
Hodges PJ, Kam PCA. The peri-operative implications of herbal medicines. Anaesthesia. 2002;57:889–99.
Zarbock A, Polanowska-Grabowska R, Ley K. Platelet-neutrophil interactions: linking haemostasis and inflammation. Blood Rev. 2007;21:99–111.
Semple J, Freedman J. Platelets and innate immunity. Cell Mol Life Sci. 2010;67:499–511.
Semple JW, Italiano JE, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11:264–74.
Ruf A, Schlenk RF, Maras A, Morgenstein E, Patscheke H. Contact-induced neutrophil activation by platelets in human cell suspensions and whole blood. Blood. 1992;80:1238–46.
Kaur P, Robin MRG, Singh B, Arora S. Development of aqueous-based multi-herbal combination using principal component analysis and its functional significance in HepG2 cells. BMC Complement Altern Med. 2019;19(1):18.
Do QD, Angkawijaya AE, Tran-Nguyen PL, Huynh LH, Soetaredjo FE, Ismadji S, Ju Y-H. Effect of extraction solvent on total phenol content, total flavonoid content, and antioxidant activity of Limnophila aromatic. J Food Drug Anal. 2014;22:296–302.
Mothibe ME, Osuch E, Kahler-Venter C. Commercial herbal medicines used as African traditional medicines: Ngoma herbal tonic immune booster interferes with a rapid urine drug screening test. S Afr Med J. 2017;107:734–7.
Fawole OA, Amoo SO, Ndhlala AR, Light JF, Van Staden J. Anti-inflammatory, anticholinesterase, antioxidant and phytochemical properties of medicinal plants used for pain-related ailments in South Africa. J Ethnopharmacol. 2010;127:235–41.
Amoo SO, Aremu AO, Van Staden J. Unravelling the medicinal potential of south African Aloe species. J Ethnopharmacol. 2014;153(1):19–41.
Clare BA, Conroy RS, Spelman K. The diuretic effect in human subjects of an extract of Taraxacum officinale Folium over a single day. J Altern Complement Med. 2009;15(8):929–34.
Arulselvan P, Fard MT, Tan WS, Gothai S, Fakurazi S, Norhaizan ME, Kumar SS. Role of antioxidants and natural products in inflammation. Oxidative Med Cell Longev. 2016. https://doi.org/10.1155/2016/5276130.
Santhakumar AB, Bulmer AC, Singh I. A review of the mechanisms and effectiveness of dietary polyphenols in reducing oxidative stress and thrombotic risk. J Hum Nutr Diet. 2014;27:1–21.
Owen JA. Natural choices: a guide to herbal and non-herbal medicines. Can J CME. 2005;3:96–9.
Wong A, Townley SA. Herbal medicines and anaesthesia. BJA Educ. 2011;11:14–7.
Dippenaar JM. Herbal and alternative medicine: the impact on anaesthesia. SAJAA. 2015;21:15–20.
Acknowledgements
Sister S Mabitsela in the Department of Pharmacology & Therapeutics, at SMU for collection of blood samples; and the volunteer blood donors.
Funding
Funding for the whole study was provided by Sefako Makgatho Health Sciences University.
Author information
Authors and Affiliations
Contributions
MEM performed the experiments as part of her PhD studies under the supervision of EO and CPKV. MEM contextualised and wrote this manuscript. EO and CPKV edited and corrected the manuscript. All authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Permission for this study and ethical approval was granted by the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC) (project number: MREC/M/09/2011:PG). Written information about the study was provided to the self-declared healthy volunteers, and each volunteer provided informed consent.
Consent for publication
Written informed consent was obtained from the volunteers for the publication of the findings of this study. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mothibe, M.E., Kahler-Venter, C.P. & Osuch, E. Evaluation of the in vitro effects of commercial herbal preparations significant in African traditional medicine on platelets. BMC Complement Altern Med 19, 224 (2019). https://doi.org/10.1186/s12906-019-2644-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-019-2644-z