Abstract
Background
We aimed to evaluate the effect of an 8-week yoga intervention on the shoulder and spinal actions of women with breast cancer-related arm lymphoedema.
Method
A randomised controlled pilot trial. The intervention group (n = 12) completed eight weeks of daily yoga sessions while the control group (n = 11) continued with best current care including information on compression sleeves, skin care, risks of temperature variations and recommended safe use of affected arm. Lumbo-pelvic posture, range of motion (ROM) in the shoulder and spine, and strength in shoulder and pectoral major and minor, and serratus anterior were taken at baseline, week 8 and after a 4-week follow-up. Outcome assessors were blinded to allocation.
Results
At week eight the intervention group had an improvement in lumbo-pelvic posture, as indicated by a reduction in pelvic obliquity compared to the control group (mean difference = −8.39°, 95 % CI: −15.64 to −1.13°, p = 0.023). A secondary finding was that strength in shoulder abduction significantly increased following the yoga intervention in both the affected (9.5 kg; CI: 0.34 to 18.66, p = 0.042) and non-affected arm (11.58 kg; CI: 0.25 to 22.91; p = 0.045). There were no significant between group changes in any ROM measures as a result of the yoga intervention.
Conclusion
This pilot study demonstrates that participation in yoga may provide benefits for posture and strength in women with Breast Cancer Related Lymphoedema. The improvements may be attributed to the focus of yoga on overall postural and functional movement patterns. Further trials with longer intervention that follow this methodology are warranted.
Trial registration
The Australian New Zealand Clinical Trials Registry ACTRN12611000202965.
Similar content being viewed by others
Background
In spite of improvements to surgery and radiation treatment, breast cancer-related lymphoedema (BCRL) continues to affect at least 20 % of women undergoing breast cancer treatment with axillary clearance [1]. As a chronic condition, lymphoedema requires life-long management to prevent the condition worsening and occurrence of infections such as cellulitis [2].
Upper body impairment is common in women with BCRL, whose reduction in functional activity can be higher than in women who have had breast cancer treatment without lymphoedema [3]. Impairment of the affected arm is evident in loss of shoulder range of motion (ROM) and strength [4] and changed bio-mechanics of the shoulder girdle, all leading to loss of symmetry between sides [5, 6]. These constraints produce difficulty with daily activities including household chores, driving, hobbies, carrying items and activities which require fine motor coordination of the hand [7]. Limitation of activity and level of pain have been associated with lower quality of life (QOL) [8]. Exercise interventions for women with BCRL have resulted in increased shoulder ROM [9], strength [10] and improved QOL [9], indicating that physical therapies may improve upper body morbidity [11].
Yoga is an integrated system that consists of breathing (pranayama), postures (asana), meditation and relaxation designed to improve the biopsychosocial functioning of an individual, irrespective of their limitations [12]. Improvements in physical flexibility, strength, neuro-motor coordination and postural alignment in a range of populations have been reported [13]. For this reason, yoga has been recommended as an adjunct to physiotherapy in a rehabilitation setting [14] including for those with lymphoedema [15] and may assist in correcting the upper body impairment frequently experienced by women with BCRL. However, currently the authors are unaware of any published research on the effect of yoga on posture, shoulder and spinal ROM and shoulder strength in women with BCRL.
The objective of this pilot trial was to obtain preliminary data to evaluate the effects of an 8-week yoga intervention on the upper body of women with stage one BCRL. This paper reports on outcomes of postural alignment, ROM of the shoulder and spine, and strength of the shoulder and other muscles affected by breast cancer surgery and treatment, i.e. pectoralis major, pectoralis minor and serratus anterior.
Methods
Study design
The trial was a multicentre parallel randomised controlled pilot trial (RCT) (Australian New Zealand Clinical Trials Registration ACTRN12611000202965). Ethics approval was granted by University of Tasmania Social Sciences Human Research Ethics Committee (H00011534).
The study was part of a larger study. The full protocol has been described previously [16] and the primary outcomes for the effects of yoga on lymphoedema and its sequelae and QOL have been published [17]. This manuscript presents the results for the secondary outcome measures of shoulder and spinal ROM and shoulder strength. Outcome measurements were performed at baseline, week 8 (on completion of intervention) and at week 12 (one month after intervention). Group allocation was conducted by a person independent of the trial using a computer-generated random number system on a 1:1 allocation ratio to intervention or control group. Notification of group allocation in sequentially numbered opaque sealed envelopes occurred after the baseline measurements. None of the assessors were involved in either the allocation or the delivery of the intervention. Participants were asked not to divulge their treatment to assessors and assessors did not have access to previous results.
Sample size calculation
A preliminary sample size calculation indicated that to detect a clinically significant increase in shoulder ROM of at least 10° between the two groups with expected within-group-differences of 10 % of the mean with 80 % power, so that 13–18 participants would be required for each group.
Participants
Women were eligible for inclusion if they had unilateral secondary lymphoedema of the arm, stage one as defined by the International Society of Lymphology [18], confirmed by a professional lymphoedema therapist, had completed treatment for breast cancer (surgery, radiotherapy and chemotherapy) at least six months previously, were over 18 years and had sufficient English language comprehension to provide informed consent and understand yoga instruction. Women were advised that no new exercise should be commenced during the trial. Women were excluded if they had recurrent cancer, an infection or were having Complex Lymphoedema Therapy, if they were pregnant, wore a pacemaker, which would affect bioimpedance (BIS) readings, had severe psychological illness or were currently doing yoga. Women’s safety being paramount, it was thought that including only stage one BCRL may reduce the chance of a flare-up of lymphoedema occurring. The trial was advertised on local radio and in local newspapers, with lymphoedema therapists and breast care nurses throughout Tasmania and on community and health related noticeboards.
A manual containing information on best current care for BCRL was given to all participants at the commencement of the trial on the instructions of the overseeing ethics committee. Recommended current care included information on wearing of professionally fitted compression sleeve and when to wear it, continuing recommended skin care and avoiding cuts to the skin and extreme temperatures, wearing non-restrictive clothing, maintaining a healthy weight, and using the affected arm without undue strain such as repeating the same movement or holding the arm in one position for a long period of time. Women were advised to continue any current exercise, but not to commence any new activity during the trial period, and to seek immediate medical help in the event of an exacerbation of lymphoedema during the trial. Compliance to this request was measured using the International Physical Activity Questionnaire (IPAQ), a reliable measure of activity in this population [19] in the week prior to each measurement period. Daily physical activity was measured using a VAS scale as previously described [16].
Control group
As lymphoedema is a medical condition that will worsen without treatment, participants randomised to the control group were requested to maintain their usual self-care throughout the trial period and were offered the same 8-week teacher led yoga with home-practice DVD as the intervention group at the completion of the final measurement.
Yoga intervention group
The intervention consisted of a weekly 90-min teacher-led yoga class and a daily 45-min home-practice yoga session provided by DVD in addition to their usual self-care. Participants recorded their daily practice along with any relevant comments in a personal logbook. Women had the choice of wearing their compression sleeve during each session, as long as the compression sleeve was worn immediately on completion of each yoga session [20].
The Satyananda Yoga® style [21] was chosen as its systematised and progressive practices are based on an integrated system consisting of pranayama, asana, meditation and relaxation with options for modifications. The practices were chosen following the principles of manual lymphatic drainage [22], with gentle ROM actions of the shoulder and spine focussing on posture and kinematic movement patterns while engaging core and shoulder-stabilising muscles, and stress reduction. Safety precautions and exercise guidelines for women with BCRL were adhered to [23]. A full rationale [24] and basic outline of the yoga program [17] for the yoga group has been described previously.
Outcome measurements
Anthropometric measurements were conducted and followed by shoulder ROM and strength tests with the same trained assessor at each time-point. A sub-group of women (n = 15), who volunteered for spinal ROM were tested on the day following other measurements. Participants were asked to volunteer separately for this assessment due to the need to partially undress for assessment, and were assured of the privacy they would be given.
Range of motion of shoulder
Active shoulder ROM was measured according to an established reliable and validated method [25] using a two-armed goniometer [26]. Briefly, participants sat in a low-back chair with stable shoulder blades and suitable back support, their knees bent to 90° and their feet at hip width and flat on the floor. Flexion, abduction and extension of the shoulder in the sagittal or coronal planes were measured with the arms in anatomical position. Internal and external rotation of the shoulder were measured from the starting position of the arm abducted to 90°, forearm pronated and parallel to the floor, palm down, with elbow bent to 90°. To prevent fatigue of the affected arm, measuring was conducted in the following order: flexion, internal rotation, extension, abduction, external rotation. The endpoint of measurement was full range, compensatory movements of the shoulder or trunk occurring, or participant experiencing pain or tightness. The final score was recorded in degrees as the best of three attempts [25].
Strength of shoulder and pectoralis major, pectoralis minor and serratus anterior
Muscle strength was measured according to an established protocol [27] using a reliable and valid handheld dynamometer (Commander Powertrack II Muscle Tester; JTechMedical, Salt Lake City, Utah, USA) [28]. The participant sat in a stable position and the non-affected, then the affected, arm was measured in turn, three times for each action. The arm was raised to 90° for the strength measurements of flexion, horizontal adduction and abduction. To measure the strength in extension, the participant’s arm was by her side. The arm was positioned slightly across the body for the strength measurement of the pectoralis major and the arm elevated to 120° for the serratus anterior. The strength of pectoralis minor was measured with the participant in supine position. This was also the order of measuring used to prevent fatigue.
The strength of the shoulder/separate muscles (pectoralis major, pectoralis minor, serratus anterior) was measured from the force applied against the resisted hand-held dynamometer, held by the assessor, for a count of three seconds. Measurement ceased when full strength was applied, compensatory movements of the shoulder or trunk occurred or pain was experienced. The best of three attempts was recorded in Newtons (N).
Grip strength
Hand grip strength was assessed using a hand-held grip dynamometer (Smedleys, TTM, www.stoeltingco.com), validated for use in a clinical setting [29], as previously described [16].
Spinal mobility
Spinal mobility was measured dynamically using video analysis in order to quantify the functional mobility of the spine during lateral flexion and flexion/extension from a stable standing position and thoracic spinal rotation in a stable sitting position according to established protocols [30]. Each movement was performed three times in a slow controlled fashion with no break between repetitions.
Movements were recorded by a video camera with backlighting, utilising reflective surface markers placed on participants’ skin at the following locations: left and right posterior superior iliac spines (LPSI, RPSI), spinal processes (S1, L3, L1, T6, T1) and left and right acromion (LACR, RACR). Reflective markers were also placed on the wall and floor for calibration. At the initial measurements, the distance between markers applied to the participant’s skin was recorded to ensure consistency.
Video data was analysed using Quintic™ Sports Biomechanics Video Analysis Software (9.03 version 14; Quintic Consultancy Limited; www.quintic.com). Measurements were made of the position of each marker in the reference plane from resting position to range in each direction. This allowed calculation of the angles in degrees defined in Table 1, following methods described elsewhere [30]. The range of excursion of each angle was recorded, except for pelvic obliquity and angle of kyphosis at rest which were static angles.
Data analysis
Baseline information for demographic and medical characteristics between treatment groups were compared by independent two-tailed t-tests for continuous variables and by Yates corrected chi-square tests for categorical variables (SPSS version 19; IBM, Armonk, New York, USA). Statistical analyses of outcome measures at baseline and changes between groups at weeks 8 and 12 were performed using STATA statistical software (version 12; STATA Corporation, College Station, Texas, USA). Parametric longitudinal data were analysed via mixed methods linear regression (ANOVA). Where assumptions of linear regression were violated, data were analysed using non-parametric analysis via ordinal logistic regression. Post-hoc testing was performed on all data using the Holms test to locate the means that were significantly different. Statistical significance was set at p < 0.05. Due to the low sample size neither multivariate nor covariate analyses were performed. Data is presented as Mean (M) and Standard Deviation (SD) unless otherwise indicated.
Results
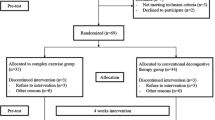
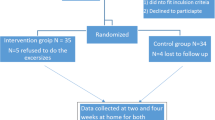
Participant flow through the trial is presented in Fig. 1. From 59 potential participants who expressed an interest in the study, 28 consented and underwent baseline testing with 15 randomised to the yoga intervention and 13 to the usual care control.
Compliance with the intervention
Two participants withdrew after being diagnosed with recurrent cancer during the trial while seven others experienced adverse events requiring their withdrawal from the study that were unrelated to either their condition or the treatment. Briefly, five participants withdrew due to adverse events unrelated to the yoga intervention during the eight-week intervention period while another four withdrew between the end of the intervention and the follow up measurement (Fig. 1).
Due to these events, fewer participants returned for the week-12 follow-up than completed the week 8 measurements. Consequently, the results from baseline to end of the 8 week intervention (b-8) and end of the week 8 intervention to week 12 follow-up (8b-12) were analysed separately.
Apart from that prescribed for the intervention group, during the trial, no women in either group were doing yoga, nor had they done it since developing BCRL. Attendance at the yoga sessions was high (97 %), as was self-reported compliance with the home-practice DVD (86 %). There were no statistically significant changes in physical activity by either group across all time points as measured by either the IPAQ questionnaire or VAS scale.
Characteristics of the group
There were no demographic or medical differences from diagnosis and treatment for breast cancer and lymphoedema in the groups at baseline (Table 2). Twenty-three participants, with a mean age of 57.6 ± 10.5 years (range 34–80) and a mean BMI of 27.2 ± 4.9 kg/m2 (range 20.4–37.3), completed the eight week intervention and 19 women returned for the week 12 follow-up measurement.
Outcomes
BMI
At baseline, the intervention group had a higher BMI (Mean Difference (MD) 4.03 kg; 95 % Confidence Intervals (CI): 0.24 to 7.81; p = 0.023) than the control group. However, at week 8 (MD −0.6 kg; 95 % CI: −1.98 to −0.01; p = 0.147) and at week 12 (MD −0.41 kg; 95 % CI: −1 to 0.187; p = 0.378) this difference was not significant. Due to the low numbers in the trial no correlation analysis was carried out for the BMI baseline measurement.
Shoulder ROM
At baseline there was an inhibited ROM in all shoulder ROM measures across both groups with the affected arm exhibiting non-significant reduced ROM compared to the affected arm. There were no statistically significant differences in shoulder ROM between groups at baseline. From b-8, there was a difference in the change between groups in abduction (MD −14.70°; 95 % CI: −29.30 to −0.10; p = 0.049) and flexion (MD −19.00°; 95 % CI: −33.65 to −4.36; p = 0.011) of the non-affected arm due to the increase in abduction (MD 10.7°; 95 % CI:-0.08 to 21.48; p = 0.052) and flexion (MD 20.5°; 95 % CI: 9.68 to 31.32; p = 0.001) in the control group and little change in the intervention group (Table 3). Each group had significant changes for other actions (Table 3).
From 8b-12, the intervention group demonstrated decreased internal rotation of the affected arm compared to the control group (MD −10.97°; 95 % CI: −17.37 to −4.56; p = 0.001) due to the decrease in the intervention group (MD −6.67°; 95 % CI: −11.31 to −2.02; p = 0.005) and the increase in the control group (MD 4.3°; 95 % CI: −0.11 to 8.78; p = 0.056). Results for shoulder ROM are presented in Table 3.
Shoulder strength
There were no differences between groups in actions of shoulder strength at baseline. From b-8 and 8b-12, there were no significant changes between groups. However, from b-8, abduction of both the affected (MD 9.5 kg; 95 % CI: 0.34 to 18.66; p = 0.042) and the non-affected (MD 11.58 kg; 95 % CI: 0.25 to 22.91; p = 0.045) shoulder increased in the intervention group (Table 4).
Strength of pectoralis major, pectoralis minor and serratus anterior
There were no differences between groups in strength actions for these muscles at baseline. From b-8, there were no changes between groups. From 8b-12, there was a decrease in the strength of the non-affected pectoralis major in the intervention compared to the control group (MD −11.80 N; 95 % CI: −19.21 to −4.38; p = 0.002) due to the decrease in the intervention group (MD −7.88 N; 95%CI −13.27 to −2.50; p = 0.004). Both groups had significant increases for serratus anterior at week 8 and significant decreases for pectoralis minor at week 12 (Table 4).
Grip strength
There were no differences between groups in grip strength at baseline or from b-8. From 8b-12 there was a decrease in grip strength of the affected arm (MD 3.58 kg; 95 % CI:1.50 to 5.67; p = 0.01) due to the decrease in the control group (MD −3.25 kg; 95 % CI −4.69 to −1.82; p = 0.002) (Table 4).
Spinal mobility
At baseline, the intervention group had a higher (worse) angle of pelvic obliquity compared to the control group (MD +9.97°; 95 % CI: 2.76 to 17.17; p = 0.007). From b-8, the angle of pelvic obliquity was lower (improved) in the intervention group compared to the control group (MD −8.39°; 95 % CI: −15.64 to −1.13; p = 0.023) due to the reduction in pelvic obliquity in the intervention group (MD −9.96°; CI: −14.54 to −5.37; p = 0.001).
At baseline, the angle of thoracic kyphosis at rest was higher (worse) in the intervention group (MD 8.13°; 95 % CI: −0.10 to 16.37; p = 0.053). From b-8, there was a tendency towards reduction (improvement) for the angle of kyphosis in the intervention group compared to the control group (MD −3.88°; 95 % CI −8.08 to 0.32; p = 0.070).
No between-group changes from b-8 or 8b-12 were observed for any other measure of spinal mobility (Table 5).
Discussion
To the best of our knowledge this was the first study to examine the effects of a yoga intervention on shoulder and spinal ROM and shoulder strength in women with BCRL. The major finding was that pelvic obliquity was reduced following the eight week yoga intervention. A secondary finding was that strength was increased following the yoga intervention for shoulder abduction in both the affected and non-affected arm.
There was noticeable lateral tilt of the pelvis (as measured by pelvic obliquity) for both the control and intervention group at baseline indicating variation from ideal posture. Changes in posture may be affected by a number of factors for this cohort including complications associated with BCRL. The one study on body posture of those with BCRL [5] reported that participants displayed mediolateral pelvic movement and dropped shoulder to the affected side when walking. In addition faulty body posture has been reported after breast cancer treatment of mastectomy [31] a high risk factor for BCRL, indicating a forward leaning of the trunk and lack of symmetry in the trunk and shoulders. These changes may be a result of the swelling, the different weight distribution of the lymphoedematous limb and changed biomechanics of the trunk and shoulder girdle from breast cancer treatment, similar to what has been reported for those with lower limb lymphoedema [32]. Nevertheless it must be acknowledged that it is not uncommon for women in this age group (median age 58) to have pelvic obliquity from various age and life related stresses on the lower body and pelvis including the effects of childbirth [33] affecting postural alignment, pelvic stability, and walking gait and hence the observed pelvic obliquity may not be solely associated with BCRL.
The yoga intervention resulted in an improvement (reduction) in a static postural measure, the angle of pelvic obliquity, between the groups (p = 0.023) due to an improvement in the yoga intervention group (p = 0.001). In addition thoracic kyphosis, demonstrated a non-significant improvement for the yoga group compared to the control group (p = 0.07). While the intervention group was outside the normative values for this measure at baseline [30], there were no significant changes in either group. While the differences between the groups at baseline limit the ability to form conclusions about the changes observed for this measure, changes in the angle of kyphosis may need a longer intervention than the current trial with reductions in kyphosis in one yoga trial reported following three one hour yoga sessions per week for 24 weeks [34]. Yoga focusses on teaching postural alignment from the feet through to the pelvis, shoulders, neck and head before commencing any of the physical, breathing or meditative practices. There is also a strong focus on body awareness (kaya sthairyam). In the current trial postural alignment and awareness were taught before, during and after each practice in order to create a stable foundation. Core stabilisation is also a key feature of yoga and is achieved by engaging the muscles of the transversus abdominis and pelvic floor (moolabhanda) before engaging other muscles in many yoga postures or as part of breathing practices. While core strength was not measured in the current trial, the improvement in pelvic obliquity indicated at least an awareness of maintaining pelvic stability [15]. Pelvic stability while standing was improved following core stability exercises [35] and in a Pilates intervention [36]. Although there were improvements in pelvic stability in the intervention group it must be acknowledged that differences existing at baseline meant that the potential for improvement was high.
Strength in shoulder abduction improved in both arms following the yoga intervention. However, these were not significantly different to changes observed following the control period, possibly due to the small sample size in this pilot study. Nevertheless these results support previous uncontrolled studies showing improvements in handgrip strength following a yoga intervention [37] although this was not supported by any improvements in hand grip strength in the current study. The yoga intervention had no weight-bearing on the arms; however, the focus on stabilisation of the scapula/shoulder complex (amsa bandha,) occurred for every action. Correct scapula/shoulder stabilisation is dependent on space in the sub-acromial area and scapulohumeral rhythm relies on the correct firing of key stabilising muscles such as the upper and lower trapezius, serratus anterior, pectoral muscles and the rhomboids [38], which can be adversely affected by breast cancer treatment [39]. Shoulder abduction requires contraction of the supraspinatus and deltoid muscles, which occurs in a fluid action when this sub-acromial space exists. In the current trial, the focus on shoulder stability may have led to improved scapulohumeral rhythm facilitating abduction strength. Another trial based on gentle exercises, similar to the yoga intervention, to achieve scapulohumeral control in a group of participants with scapular dyskinesis (n = 18) showed that specific gentle shoulder movements activated the upper and lower trapezius and serratus anterior in both groups [40]. We have previously reported reduced symptoms and tissue density in the upper arm and reduction in fluid of the affected arm for the intervention group [17]. It is likely that these improvements made the action of abduction easier in the same way reduction of fluid and improved postural alignment and stability improved walking gait of those with lower limb lymhoedema [32].
The intervention was not associated with increases in ROM across any shoulder movement. The focus on creating stability of the glenohumeral complex may explain the lack of increase in ROM. Similar studies involving shoulder stability [41] or Pilates [36] also found no changes in shoulder ROM. Interestingly, the Pilates intervention reported improved biomechanical control of the scapula and trunk in lateral flexion [36], perhaps indicating that stability is achieved prior to changes in ROM. It is possible that the ROM results are due to a learning effect from baseline to week eight as there was a mean increase in 18 of the 20 measures of shoulder ROM in both the intervention and control group over this timeframe. The fact that this pattern did not continue from week 8 to 12 gives weight to this hypothesis. While further study is required to determine the true effects of a yoga intervention on ROM in this population the results highlight the potential importance of inclusion of a familiarity phase prior to data collection in any future study.
There were no significant between group changes in spinal ROM. In comparison to norms for spinal mobility [30], group mean baseline measurements revealed participants in the current trial recorded lower flexion/extension and lateral flexion although they were within the normal range for rotation. However, there was no change in spinal mobility as a result of the yoga intervention. Similar findings were observed following 12 weeks of Pilates [36] where it was suggested that participants reduced compensatory movements of the spine by focussing on segmental motion, postural alignment and stability rather than on increasing their range. The results of the current trial support this hypothesis.
As already acknowledged there are several limitations in this study. These include the lack of familiarity testing prior to data collection, the differences between the groups in certain variables at baseline, as well as the small sample size. Due to a lack of prior data to use to calculate sample size, the a priori sample size calculation performed for this study was based on clinically significant changes in the major outcome variables with an assumed level of variability [16]. This indicated that between 13–19 participants would be required per group and we proposed that 20 participants per group would be recruited. Unfortunately we did not achieve the proposed sample size and there was greater variability in the results than anticipated resulting in wider confidence intervals than expected. These factors impacted on the statistical significance of results including potentially the differences between the groups at baseline. Nevertheless the pilot study results obtained provide important initial data which will inform sample size calculations for any future studies.
Conclusions
This pilot study highlights possible improvements in posture evident in the reduction in the angle of pelvic obliquity and trend to a reduced angle of kyphosis as a result of the yoga intervention. Further, the intervention group increased shoulder strength for both arms in the action of abduction, an indicator that improved shoulder stability may have occurred. The improvements observed in this study may possibly be attributed to the focus of the yoga intervention on overall placement of body posture and function in each aspect of the yoga during meditation, breathing, relaxation and execution of the physical postures both moving and stationary. Such increased awareness in body placement and method of movement rather than a focus on increasing flexibility of movement may account for the lack of change in shoulder and spinal ROM. As women with BCRL can experience problems with posture and shoulder actions these results possibly indicate that yoga may offer some positive outcomes. While there are several limitations including a small sample size, the data provides sufficient evidence of the potential benefits of yoga to warrant larger controlled trials following the general methodology outlined in this paper.
Abbreviations
- BCRL:
-
Breast cancer related lymphoedema
- ROM:
-
Range of motion
- QOL:
-
Quality of life
- RCT:
-
Randomised controlled trial
- BIS:
-
Bioimpedance spectroscopy
- LPSI:
-
Left posterior superior iliac spine
- RPSI:
-
Right posterior superior iliac spine
- LACR:
-
Left acromion
- RACR:
-
Right acromion
References
National Breast and Ovarian Cancer Centre, Review of research evidence on secondary lymphoedema: Incidence, prevention, risk factors and treatment. Sydney: National Breast and Ovarian Cancer Centre; 2008. p. 1–88.
Brennan MJ. Lymphedema following the surgical treatment of breast cancer: a review of pathophysiology and treatment. J Pain Symptom Manage. 1992;7(2):110–6.
Hayes SC, et al. Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol. 2008;26(21):3536–42.
Pyszel A, et al. Disability, psychological distress and quality of life in breast cancer survivors with arm lymphedema. Lymphology. 2006;39(4):185–92.
Balzarini A, et al. Biomechanical evaluation of scapular girdle in patients with chronic arm lymphedema. Lymphology. 2006;39(3):132–40.
Shamley D, et al. Three-dimensional scapulothoracic motion following treatment for breast cancer. Breast Cancer Res Treat. 2009;118(2):315–22.
Thomas-MacLean R, Miedema B, Tatemichi SR. Breast cancer-related lymphedema: women’s experiences with an underestimated condition. Can Fam Physician. 2005;51(2):246–7.
Dawes DJ, et al. Impact of lymphoedema on arm function and health-related quality of life in women following breast cancer surgery. J Rehabil Med. 2008;40(8):651–8.
McClure MK, et al. Randomized controlled trial of the Breast Cancer Recovery Program for women with breast cancer-related lymphedema. Am J Occup Ther. 2010;64(1):59–72.
Schmitz KH, et al. Weight lifting in women with breast cancer-related lymphedema. N Engl J Med. 2009;361(7):664–73.
Hayes SC, et al. Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. 2012;118(8 Suppl):2237–49.
Desikachar K. The yoga of healing: exploring yoga’s holistic model for health and well-being. Int J Yoga Therapy. 2005;15:17–39.
Evans S, et al. Using the biopsychosocial model to understand the health benefits of yoga. J Complement Integrative Med. 2009;6(1):1–22.
Posadzki P, Parekh S. Yoga and physiotherapy: a speculative review and conceptual synthesis. Chin J Integr Med. 2009;15(1):66–72.
Schrale G, Ryan TJ. Mananging oedema and fibrosis with coordinated movement. J Lymphoedema. 2011;6(2):82–6.
Loudon A, et al. The effect of yoga on women with secondary arm lymphoedema from breast cancer treatment. BMC Complement Altern Med. 2012;12:66.
Loudon A, et al. Yoga management of breast cancer-related lymphoedema: a randomised controlled pilot-trial. BMC Complement Altern Med. 2014;14:214.
Lymphoedema Framework, International Consensus. Best Practice for the Management of Lymphoedema. London: MEP Ltd; 2006.
Schmitz KH, et al. Physical Activity and Lymphedema (the PAL trial): assessing the safety of progressive strength training in breast cancer survivors. Contemp Clin Trials. 2009;30(3):233–45.
Johansson K, et al. Low intensity resistance exercise for breast cancer patients with arm lymphedema with or without compression sleeve. Lymphology. 2005;38(4):167–80.
Saraswati N. Asana, Pranayama, Mudra, Bandha. Munger, India: Bihar School of Yoga; 1996.
Casley-Smith JR. Exercises for patients with lymphoedema of the arm, a guide to self-massage and hydrotherapy exercises. Malvern, South Australia, Australia: Lymphoedema Association of Australia; 1999.
National Lymphedema Network, Position Statement of the National Lymphedema Network. Topic: Exercise. 2011.
Loudon A, et al. Using yoga in breast cancer-related lymphoedema. J Lymphoedema. 2012;7(1):27–36.
Box RC, et al. Physiotherapy after breast cancer surgery: results of a randomised controlled study to minimise lymphoedema. Breast Cancer Res Treat. 2002;75(1):51–64.
Riddle DL, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting. Shoulder measurements Phys Ther. 1987;67(5):668–73.
Kendall FP, et al. Muscles: Testing and Function with Posture and Pain. 5th ed. Baltimore, Maryland: Lippincott, Williams and Wilkins; 2005.
Leggin BG, et al. Intrarater and interrater reliability of three isometric dynamometers in assessing shoulder strength. J Shoulder Elbow Surg. 1996;5(1):18–24.
Bohannon RW. Dynamometer measurements of hand-grip strength predict multiple outcomes. Percept Mot Skills. 2001;93(2):323–8.
Menegoni F, et al. Kinematics of trunk movements: protocol design and application in obese females. J Appl Biomater Biomech. 2008;6(3):178–85.
Malicka I, et al. Body posture of women after breast cancer treatment. Ortop Traumatol Rehabil. 2010;12(4):353–61.
Aggithaya MG, Narahari SR, Ryan TJ. Yoga for correction of lymphedema’s impairment of gait as an adjunct to lymphatic drainage: A pilot observational study. Int J Yoga. 2015;8(1):54–61.
Byrne JE, et al. Comparison of gait patterns between young and elderly women: an examination of coordination. Percept Mot Skills. 2002;94(1):265–80.
Greendale GA, et al. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57(9):1569–79.
Kaji A, et al. Transient effect of core stability exercises on postural sway during quiet standing. J Strength Cond Res. 2010;24(2):382–8.
Emery K, et al. The effects of a Pilates training program on arm-trunk posture and movement. Clin Biomech. 2010;25(2):124–30.
Mandanmohan JL, Udupa K, Bhavanani AB. Effect of yoga training on handgrip, respiratory pressures and pulmonary function. Indian J Physiol Pharmacol. 2003;47(4):387–92.
Lin JJ, Lim HK, Yang JL. Effect of shoulder tightness on glenohumeral translation, scapular kinematics, and scapulohumeral rhythm in subjects with stiff shoulders. J Orthop Res. 2006;24(5):1044–51.
Shamley DR, et al. Changes in shoulder muscle size and activity following treatment for breast cancer. Breast Cancer Res Treat. 2007;106(1):19–27.
Kibler WB, et al. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med. 2008;36(9):1789–98.
Lee SA, et al. Effects of a scapula-oriented shoulder exercise programme on upper limb dysfunction in breast cancer survivors: a randomized controlled pilot trial. Clin Rehabil. 2010;24(7):600–13.
Acknowledgements
Equipment was provided by Flinders University and University of Tasmania. The Women’s Health Centre, Hobart and the Launceston Community Health Centre, Kings Meadows provided venue for conducting the yoga intervention and testing. We acknowledge the voluntary provision of professional services in testing by Marlene Kalis, Christine Lambrechts, Michele Smith, Belinda Mann, Kara Spaulding, Lara Matuszek and Megan Reid and the professional assistance of Chris Dale and Professor David McNeil. We are indebted to the women of Tasmania who volunteered for this trial.
Funding
This study was supported by grants from the Swan Research Institute (SRI) and the Faculty of Health Sciences Seed Funding, UTAS. The funders had no role in the design, collection, analysis or interpretation of the data, or in the writing of the manuscript.
Availability of data and materials
The datasets generated and analysed during the current study are available on Research gate (https://www.researchgate.net/publication/297713856_Yoga_and_BCRL_original_results_deidentified?ev=prf_pu) and are also available from the corresponding author on reasonable request.
Authors’ contributions
AL conceived the trial and with TB and ADW were responsible for the design of this trial and the construction of the measurement protocol for shoulder ROM and strength. DV was responsible for the design of the spinal testing measurement protocol and its associated statistical analysis. AL conducted the yoga intervention. MAI assisted in advice for the yoga intervention. AL and ADW conducted the statistical analysis. AL, ADW and DV drafted and TB, NP, MAI helped draft the mansuscript. All authors read and approved the final manuscript.
Authors’ information
AL is a yoga researcher and trains yoga teachers in yoga therapy.
TB is Director of Rural Health, University of Tasmania.
ADW is a senior lecturer in Clinical Exercise Science, University of Tasmania.
DV is a physicist and lecturer in Clinical Exercise Science, University of Tasmania.
NP is Director of the lymphoedema clinic at Flinders University.
MAI is Director of physical movement and yoga researcher at University of South Australia.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not Applicable.
Ethics approval and consent to participate
Ethics approval was sought and granted by University of Tasmania Social Science Human Research Ethics Committee on 5th December, 2010, project number H0011534. All women gave informed written consent to participate in this trial.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Loudon, A., Barnett, T., Piller, N. et al. The effects of yoga on shoulder and spinal actions for women with breast cancer-related lymphoedema of the arm: A randomised controlled pilot study. BMC Complement Altern Med 16, 343 (2016). https://doi.org/10.1186/s12906-016-1330-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-016-1330-7