Abstract
Background
The increase in the rate of multiple pregnancies in clinical practice is associated with assisted reproductive technology (ART). Given the high risk of dichorionic triamniotic (DCTA) triplet pregnancies, reducing DCTA triplet pregnancies to twin or singleton pregnancies is often beneficial.
Case presentation
This article reports on two cases of DCTA triplet pregnancies resulting from two blastocyst transfers. Given the high risk of complications such as twin-to-twin transfusion syndrome (TTTS) in monochorionic diamniotic (MCDA) twin pregnancies, patients have a strong desire to preserve the dichorionic diamniotic (DCDA) twins. Multifetal pregnancy reduction (MFPR) was performed in both cases to continue the pregnancy with DCDA twins by reducing one of the MCDA twins. Both of the pregnant women in this report eventually gave birth to healthy twins at 37 weeks.
Conclusions
For infertile couples with multiple pregnancies but with a strong desire to remain the DCDA twins, our report suggests that reducing DCTA triplets to DCDA twin pregnancies may be an option based on clinical operability and assessment of surgical difficulty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The clinical utilization of assisted reproductive technology (ART) and ovulation induction drugs, coupled with the rise in maternal age, has resulted in a consistent increase in the occurrence of multiple pregnancies over the last four decades [1]. As mentioned earlier, the likelihood of a monozygotic twin (MZT) following ART treatment is significantly greater than that of natural conception [2, 3]. There are three types of MZT: monochorionic-monoamniotic, monochorionic-diamniotic and dichorionic-diamniotic. Monochorionic twin (MCT) pregnancies are at high risk of maternal and fetal complications, especially fetal complications. In addition to selective intrauterine growth restriction (SIGR) and TTTS, which are unique complications of MCT, common fetal complications include preterm birth, fetal malformations, and perinatal death [4, 5].
Multiple pregnancies are becoming more prevalent as a potential consequence of infertility treatment [6]. In particular, MZT that split into two embryos from one embryo may result in high-order multiple pregnancies (HOMPs), such as DCTA triplet pregnancies [7, 8]. HOMPs are associated with a higher risk of complications such as miscarriage and preterm birth compared to singleton and twin pregnancies [9, 10]. Multifetal pregnancy reduction (MFPR) was first reported 35 years ago as a novel approach to managing multiple pregnancies [11]. Fetal reduction techniques were developed to improve the clinical outcomes associated with high mortality and morbidity associated with multiple pregnancies due to infertility treatment [12]. With clinicians’ increasing surgical experience, familiarity with the patient’s clinical situation, and a better understanding of the risks and benefits of different fetal reduction methods, transabdominal reduction and transvaginal reduction have become the most commonly used fetal reduction methods to reduce the high risk of multiple pregnancies [13,14,15,16]. Transvaginal fetal reduction is less commonly used than transabdominal fetal reduction, however, it may be a better option when the patient wishes to undergo surgery during the first trimester of pregnancy, or when it is difficult or impossible to perform transabdominal fetal reduction due to extreme obesity, abdominal scarring, or if the fetus cannot be reached through the abdomen [17]. Transvaginal fetal reduction is usually performed by aspiration of the embryo under the guidance of vaginal ultrasound and is best used in the first trimester of pregnancy (usually 6 to 8 weeks) [18, 19]. Transabdominal fetal reduction is usually performed by ultrasound-guided injection of KCl with a needle inserted through the abdomen into the fetal chest cavity and is generally used in the early second trimester of pregnancy (usually refers to 11–14 weeks) [17]. Transabdominal intracranial injection of KCl has been reported as an alternative to achieve a reduction in multiple pregnancies, ultimately leading to good pregnancy outcomes [20, 21]. In addition, selective fetal reduction by radiofrequency ablation and umbilical cord coagulation in the second trimester of pregnancy has also been used in some institutions. Due to differences in equipment availability, technology preferences, and clinician experience, the above techniques are not common in our institution [22].
The incidence of DCTA triplet pregnancies has been reported to be 0.004% [23]. MCT pregnancies are known to have a high risk of maternal and fetal complications including miscarriage, preterm birth, low birth weight, TTTS and perinatal death [4]. Reducing DCTA triplet pregnancies to twin or singleton pregnancies can significantly reduce the risk of complications for both mother and baby. However, there are few reports on fetal reduction protocols and pregnancy outcomes for DCTA triplet pregnancies [24]. There are even fewer studies on the reduction of DCTA triplet pregnancies to DCDA twin pregnancies. This article reports two cases of final pregnancy outcomes following the reduction of DCTA triplet pregnancies to DCDA twin pregnancies.
Case elaboration
Case 1
A 31-year-old woman complaining of secondary infertility underwent IVF-ET treatment after trying to conceive without contraception for 3 years. The woman has a history of two pregnancies that ended in miscarriage, one as a result of an induced abortion and the other due to embryonic development cessation. The patient was treated with a 10-day antagonist protocol with 150 IU of recombinant follicle-stimulating hormone (FSH) injected daily. 36 h before oocyte extraction, a total of 4000 IU of recombinant human chorionic gonadotropin (HCG) was injected to promote oocyte maturation. A total of 28 oocytes were retrieved vaginally under ultrasound guidance, of which 26 oocytes matured and successfully fertilized and cleavaged. There were 13 high-quality embryos on the third day. Twelve and six embryos reached the blastocyst stage on days 5 and 6, respectively, resulting in a total of 18 blastocysts, all of which were subsequently cryopreserved. In the subsequent frozen embryo transfer cycle, two day 5 blastocysts (Gardner classification: 4BA, 4BB) were transferred to the patient’s uterus in response to the patient’s request to increase the success rate of embryo implantation. The luteal phase was supported with progesterone (60 mg/day).
The patient’s urine HCG test result was positive on the 14th day of the embryo transfer. We chose to measure fetal heartbeat status by transvaginal ultrasonography at 6 to 8 weeks of gestation to determine chorionicity and fetal number. The first ultrasound was performed on day 30 after embryo transfer and showed two chorionic sacs, suggesting a dichorionic pregnancy. One of the sacs contained germs that were 6.7 mm and 7.0 mm long, both of which showed a heartbeat. One germ in another sac was 7.3 mm long and exhibited pulsation (Fig. 1A). Follow-up ultrasound at 8 weeks gestation (42 days after oocyte transplantation) showed a dichorionic pregnancy with three distinct amniotic sacs, confirming a DCTA triplet pregnancy with MCDA twins. Ultrasonography revealed three embryos with heartbeats in the uterine cavity of the pregnant woman with lengths of 19.7 mm, 18 mm, and 20.1 mm (see Fig. 1B). After informing the patient and her family about the risks associated with DCTA triplet pregnancy and fetal reduction, the final selective reduction of the number of fetuses and the specific protocol is decided by the patient after a detailed consultation, and then the patient signed the informed consent form.
Vaginal ultrasound reveals dichorionic triamniotic triplets with two gestational sacs (GS, red arrow) and three germs (blue arrow) in the uterus. A) Ultrasound images were taken for the first time 30 days after transplantation. B1-2) Ultrasound image of the second pregnancy on day 40 after embryo transfer. C) Ultrasound image after selective fetal reduction
After completing the necessary preoperative examinations, an ultrasound-guided transvaginal fetal reduction was performed on the 43rd day after transplantation. To satisfy the desire of infertile couples who want to remain the DCDA twin, one of the MCDA twins was selectively reduced after assessing the difficulty of the surgery and informing them of the risks of the surgery. Intravenous anesthetics and ceftriaxone sodium (as a prophylactic antibiotic) were administered before surgery, followed by a comprehensive vaginal wash. The puncture needle was attached to a syringe, inserted into the vaginal wall using a needle guide, and then inserted into the gestational sac (GS). The puncture needle was positioned near the germ and used to aspirate and halt the activity of the embryonic heart. The surgery went smoothly. The patient bled less and experienced minor pain during the operation. The postoperative follow-up ultrasound revealed that one of the three fetuses had been reduced, and the embryonic cardiac tube pulse of the reduced fetus was no longer detectable (see Fig. 1C). The patient underwent an emergency cesarean section after fetal distress caused by premature rupture of membranes (PROM) at 36 weeks and 6 days of gestation and successfully delivered a boy and a girl. The boy was born weighing 2800 g and was 50 cm in length, while the girl weighed 2500 g and measured 49 cm in length. Both infants scored 10 points on their 1-minute and 5-minute Apgar assessments. Subsequent follow-up visits with the children also confirmed that the twins remained healthy.
Case 2
A couple who complained of primary infertility for 6 years came to our hospital for IVF-ET treatment due to the sequelae of pelvic inflammatory disease and oligospermia, asthenospermia and teratozoospermia. The patient is a 34-year-old woman with a hysterosalpingogram (HSG) showing obstruction of the right fallopian tube and irregularity of the left fallopian tube. The patient was also treated with an antagonist protocol. A total of 21 oocytes were retrieved vaginally under ultrasound guidance, of which 19 oocytes matured and 17 oocytes were successfully fertilized and cleavaged. In vitro, embryo culture showed seven high-quality embryos on day 3. All embryos were cultured in vitro to day 5 or 6, resulting in a total of 13 blastocysts. All blastocysts were cryopreserved, including seven day 5 embryos and six day 6 embryos. In the subsequent frozen embryo transfer cycle, two day 5 blastocysts (Gardner classification: 4BB*2) were transferred to the patient’s uterus in response to the patient’s request to increase the success rate of embryo implantation. The luteal phase was supported with progesterone (60 mg/day).
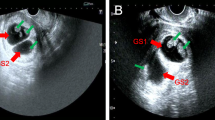
The patient’s urine HCG test was positive on the 14th day after the embryo transfer. The first ultrasound, performed on day 29 after embryo transfer, revealed two chorionic sacs in the uterine cavity of the pregnant woman, one of which contained germs measuring 7.2 mm and 7.0 mm in length, both exhibiting a heartbeat. One germ in another sac was 6 mm long and had a heartbeat (see Fig. 2A). A repeat ultrasound on day 40 after oocyte transplantation confirmed a DCTA triplet pregnancy, with two of the fetuses being an MCDA twin. Ultrasound revealed three distinct amniotic sacs and three embryos with lengths of 19.8 mm, 19 mm, and 19.9 mm in length within the uterine cavity (see Fig. 2B). All three embryos were found to have a heartbeat. We informed the couple about the risks associated with multiple pregnancies and advised them to consider selectively reducing embryos. Eventually, the couple chose to selectively reduce the DCTA triple pregnancy to a DCDA twin pregnancy. After completing the necessary preoperative examinations, an ultrasound-guided transvaginal fetal reduction was performed on the 45th day after transplantation. Under ultrasound guidance, a puncture needle was used to puncture and rapidly aspirate one of the embryos in the MCDA twin, causing the embryonic echo to disappear. The operation went smoothly, and the patient experienced minimal bleeding and no significant pain during the procedure. The postoperative follow-up ultrasound revealed that one of the three fetuses had been reduced, as the fetal embryonic cardiac tube pulse of the reduced fetus was no longer detectable. The remaining embryos were growing normally. The patient was diagnosed with diabetes during subsequent pregnancies. Considering the great preciousness of the fetus to the couple, the pregnant woman and her family requested a cesarean section. Two girls were delivered by cesarean section at 37 weeks and 3 days of gestation. At birth, one of the girls weighed 2800 g and measured 48 cm in length, while the other weighed 2400 g and measured 46 cm in length. Both infants received Apgar scores of 10–10 at 1 min and 5 min after birth. Follow-up in the neonatal period also indicated that the twins were in good health.
Vaginal ultrasound reveals dichorionic triamniotic triplets with two gestational sacs (GS, red arrow) and three germs (blue arrow) in the uterus. A) Ultrasound images were taken for the first time 29 days after transplantation. B1-2) Ultrasound image of the second pregnancy taken on day 40 after transfer
Discussion and conclusions
As previously reported [25], an increasing number of women are choosing to delay marriage and childbirth, with the majority not starting a family until after the age of 30. Late marriage and delayed childbearing have become interrelated factors that affect women’s reproductive health. Consequently, there has been an increase in the demand for assisted reproductive technologies. While utilizing ART, there are potential risks associated with IVF. The study data suggests that the likelihood of monochorionic twins after natural conception was 0.4%, whereas the probability after ART ranged from 1.57 to 13.2% [2, 3]. The use of ART significantly increases the likelihood of multiple pregnancies. However, it remains unclear how embryos undergo division after ART. Studies on this issue suggest that factors such as maternal age, age of oocytes, zona pellucida manipulation techniques, prolonged embryo culture to the blastocyst stage, and embryonic morphology may strongly correlate with an increased incidence of monochorionic twins [8, 26,27,28]. However, there is still no unified explanation of how these factors influence the occurrence of monochorionic twins. Given the high risk of multiple pregnancies and their influencing factors, we consider the transfer of no more than two day 3 cleavage embryos or one blastocyst to be an advantageous option.
Globally, the proportion of triplets resulting from IVF-ET treatment is 0.7% or greater [29], and the incidence of DCTA triplets is only 0.004% [23]. Compared to singleton pregnancies, triplet pregnancies carry a high risk of extremely preterm birth, low birth weight, fetal malformations, miscarriage, and perinatal death [4, 5]. It is worth noting that DCTA triplets also carry a high risk of SIGR, TTTS, and neurological disorders associated with MCDA twins. However, there is little follow-up of women with these conditions, resulting in limited data on pregnancy outcomes and inadequate follow-up of their children.
MFPR is often considered a favorable option to reduce the risk of multiple pregnancies. Selectively reducing triplet pregnancies or HOMPs to twin or singleton pregnancies is an effective approach to reduce the risks and enhance clinical outcomes for multiple pregnancies. It must be mentioned that MFPR, while used as a means to control the number of developing fetuses and thereby reduce the high risk of multiple pregnancies, also involves numerous ethical and clinical issues. Considering fetal reduction strategies alone, there are three options for reducing DCTA triplets: reducing the singleton to preserve the MCDA twins, reducing the MCDA twin to preserve the singleton, or reducing one of the MCDA twins to continue the pregnancy with the DCDA twins. Regarding the different strategies for MFPR, is conservative management a visible option, or must a DCTA triplet pregnancy be reduced to twin pregnancy or singleton pregnancy? There are still relatively few studies on this topic. Previous studies have shown that the complete miscarriage rate and preterm birth rate of DCTA triplets are 29.41% and 66.67% [30]. Reducing DCTA triplet pregnancies to MCDA twin pregnancies has been reported to result in lower miscarriage rates and higher live birth rates compared to expectant management [31]. However, our previous study showed that reducing DCTA triplets to singleton pregnancies resulted in lower miscarriage and preterm birth rates, as well as higher live birth rates, compared to reducing DCTA triplets to twin pregnancies [30]. In addition, reducing DCTA triplets to singleton pregnancies is associated with a significant reduction in perinatal mortality and neonatal morbidity [32, 33]. These findings are consistent with previous reports that reducing DCTA triplets to MCDA twins was associated with higher rates of preterm birth, low birth weight, perinatal mortality, and higher prevalence of cesarean section compared with reduction of DCTA triplets to singletons [34, 35]. Therefore, we believe that reducing DCTA triplets to singleton pregnancies results in better pregnancy outcomes. This is also consistent with the results of most studies that reducing DCTA triplets to singleton pregnancies is a safe and reliable strategy [31, 36]. However, some infertile couples have expressed their desire to remain the twins. It is well known that the risk of complications such as TTTS in MCDA twin pregnancies is extremely high, so patients have a strong desire to preserve DCDA twins based on the risk of MCDA twins. Given this, better fetal reduction strategies need to be considered to avoid the risks associated with MCDA and to meet patient wishes. Selectively reducing one fetus in MCDA twins can prevent potential complications associated with MCDA twin pregnancy. However, this fetal reduction strategy leads back to another increased risk that when selectively reducing one of the MCDA twins may result in the death of the other surviving fetus due to the shared placenta [37]. Therefore, for infertile couples who strongly want to remain DCDA twins, we should fully inform them of this risk to choose the best strategy for fetal reduction.
We generally advise patients to reduce DCTA triplets to singleton pregnancies for better pregnancy outcomes, however, some infertile couples have a strong desire to preserve the twins. For infertile couples with a strong desire to preserve the twins, there are two fetal reduction strategies: reducing monozygotic singletons to preserve the MCDA twins and reducing one of the MC twins to preserve the DCDA twins. However, there is little research on whether MCDA twins or DCDA twins are preserved. Existing studies have shown that the perinatal mortality, stillbirth, and neonatal mortality rates associated with MCDA twin pregnancies are higher than those of DCDA twin pregnancies [38, 39]. In addition, the study also found that there was a 28.6% miscarriage rate after reducing the DCTA triplets to MCDA twin pregnancies, which was higher than the miscarriage rate after the DCTA triplets were reduced to DCDA twin pregnancies, and most of them showed no signs of poor fetal condition [39, 40]. Studies on neonatal outcomes have shown that DCDA twins result in higher birth weight and lower neonatal morbidity (e.g., digestive morbidity) compared with MCDA twins [39]. To provide a more complete picture of pregnancy outcomes after elective reduction of triplets with DCTA, we performed a retrospective analysis of patients who were reduced to MCDA and those who were reduced to DCTA. Our recent study found that DCTA triplets to DCDA twin pregnancies resulted in lower rates of complete miscarriage, preterm birth rates, and very low birth weight compared to DCTA triplets to MCDA twin pregnancies [41]. In addition, the full-term delivery rate and neonatal survival rate after reducing the DCTA triplets to the DCDA twin pregnancy were also higher than the DCTA triplets to the MCDA twin pregnancy [41]. In neonates, the mean birth weight and twin weight after reducing the DCTA triplets to DCDA twins were also significantly higher than those after the DCTA triplets were reduced to MCDA twins [41]. Studies showed that the pregnancy outcomes and neonatal outcomes of DCTA triplets to DCDA twin pregnancies were better than those of DCTA triplets to MCDA twins [41]. However, it is important to note that our small sample size may lead to biased results. Due to the unique characteristics of monochorionic twins, selective reduction of one fetus in monozygotic twins is not considered feasible. Because the risk of early TTTS occurs due to 96% of the blood vessel’s anastomosis on the placental bed, reducing one of the monochorionic twins is likely to result in a miscarriage of the other. Patients should be fully informed about the risks associated with this fetal reduction strategy, and the final number of fetal reductions and strategies should be decided by the patients after the patients are fully aware of the risks of different fetal reduction strategies. In summary, we believe that reducing DCTA triplets to DCDA twin pregnancies may be an acceptable option, also based on clinical feasibility, for infertile couples who have a strong desire to remain twins and want to minimize or reduce the risk of complications. Given the scarcity of reports of elective fetal reduction in DCTA triplet pregnancies, a definitive fetal reduction regimen remains unclear. Therefore, the optimal fetal reduction strategy is based on the patient’s preference, assessment of the difficulty of the procedure, and the clinician’s technique.
Several methods of fetal reduction have been reported, including ultrasound-guided transabdominal puncture injection of lethal substances such as KCl or hypertonic saline, radiofrequency ablation, cord occlusion, and transcervical puncture [42, 43]. However, there are some technical difficulties associated with these methods. For example, transcervical puncture requires cervical dilation and transabdominal puncture for injection of cardiotoxic substances may necessitate multiple punctures or multiple surgeries. When one of the MCDA twins is chosen to be reduced, the placenta of MC is rich in blood vessels, and the flow through the placental vessels after KCl injection may lead to acute hemodynamic changes in the surviving fetus, and ultimately lead to the death of the other surviving fetus [44]. Other studies have shown that 84.7% of MC twins will die after KCl is injected into one of the MC twins [45]. The study found that the majority of MC twin deaths occurred within 1 day of injecting KCl into one of the MC twins [46]. KCl injection into one of the MC twins resulted in extremely high MC twin mortality. To what extent is this result related to the dose of KCl injections and the number of fetal punctures? There are very few studies on this issue, which may need to be confirmed in studies with larger sample sizes. This method may also be difficult to perform due to the position of the fetus. Intrafetal laser ablation has also been reported to result in up to 50% miscarriage after fetal reduction [47]. In addition, the clinical application of umbilical cord occlusion mainly depends on the availability of equipment and the experience or expertise of clinicians, which is not common in our country. Studies have shown that there is a possibility of spontaneous fetal reduction or single intrauterine fetal demise during the pregnancy of DCTA triplets, which refers to the natural cessation of one or both fetuses in DCTA [30, 48]. Studies have shown that a single intrauterine fetal death in multiple pregnancies results in a 30–50% risk of death for surviving twins [49, 50]. In this case, the patient should be adequately informed of the risks and communicated to the patient about the pros and cons of different fetal reductions. The decision of whether to perform MFPR and the number and specific strategy of fetal reduction is ultimately up to the patient.
Fetal reduction by transvaginal aspiration of embryos has been reported as an effective method for fetal reduction in DCTA triplets [36], both patients we reported opted for transvaginal ultrasound-guided embryo aspiration to reduce the number of embryos. We chose to diagnose chorionic and amniotic pregnancy in twin pregnancies by vaginal ultrasound in the first trimester of pregnancy (typically between 8 and 11 weeks of gestation, i.e., between 6 and 8 weeks after embryo transfer) to assess the appropriate timing of fetal reduction. This decision is based on the fact that at 7–9 weeks and 11–14 weeks of gestation, transvaginal ultrasound is reliable and very accurate in the identification and diagnosis of chorionic and amniotic membranes [51, 52]. Transvaginal ultrasound-guided embryo puncture overcomes the technical difficulties of transabdominal or transcervical puncture to a certain extent and also has obvious advantages. First, the high-frequency probe can greatly increase the image resolution of the gestational sac and its contents to make the imaging clear. Secondly, the tip of the sensor probe can be close to the uterine wall and the gestational sac to be aspirated with the help of the elasticity of the vagina, and compared with the transabdominal route, the puncture process is more definite and the puncture route is shorter, which reduces the risk of inadvertent damage to the gestational sac. Furthermore, it is allowed to be carried out in the first trimester of pregnancy, such as 6 weeks of gestation, when the size of the gestational sac and its contents to be absorbed is smaller, and the embryo is easier to be sucked out. Early intervention and management of patients is psychologically beneficial. Additionally, repeated puncture of the embryo or injection of lethal substances such as KCl is avoided, making the whole process faster, more accurate, and easier, and also reducing the risk of vaginal bleeding and infection due to repeated vaginal insertion.
Currently, there are few studies on reducing DCTA triplets to twin pregnancies, especially DCDA twin pregnancies. Depending on the patient’s preference and specific clinical situation, reducing DCTA triplets to DCDA twins may be an option. This case report describes the successful outcome of two DCTA triplets that were reduced to DCDA twins. Both twins had good pregnancy outcomes. This will serve as a clinical reference for triplet pregnancies in pregnant women who need selective fetal reduction. Our report will be beneficial for infertile couples with DCTA triplets who have a strong desire to retain the DCDA twins.
Data availability
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- ART:
-
Assisted reproductive technology
- DCTA:
-
Dichorionic triamniotic
- MCDA:
-
Monochorionic diamniotic
- DCDA:
-
Dichorionic diamniotic
- TTTS:
-
Twin-to-twin transfusion syndrome
- IVF-ET:
-
In vitro fertilization and embryo transfer
- MFPR:
-
Multifetal pregnancy reduction
- MZT:
-
Monozygotic twin
- MCT:
-
Monochorionic twin
- SIGR:
-
Selective intrauterine growth restriction
- HOMPs:
-
High-order multiple pregnancies
- FSH:
-
Follicle-stimulating hormone
- HCG:
-
Human chorionic gonadotropin
- GS:
-
Gestational sacs
- HSG:
-
Hysterosalpingogram
- PROM:
-
Premature rupture of membranes
- HSG:
-
Hysterosalpingogram
References
Mateizel I, et al. Do ARTs affect the incidence of monozygotic twinning? Hum Reprod. 2016;31(11):2435–41.
Nakasuji T, et al. The incidence of monozygotic twinning in assisted reproductive technology: analysis based on results from the 2010 Japanese ART national registry. J Assist Reprod Genet. 2014;31(7):803–7.
Song B, et al. Prevalence and risk factors of monochorionic diamniotic twinning after assisted reproduction: a six-year experience base on a large cohort of pregnancies. PLoS ONE. 2017;12(11):e0186813.
Razaz N, et al. Perinatal outcomes in multifetal pregnancy following fetal reduction. CMAJ. 2017;189(18):E652–8.
Carroll SG, et al. Is zygosity or chorionicity the main determinant of fetal outcome in twin pregnancies? Am J Obstet Gynecol. 2005;193(3 Pt 1):757–61.
Evans MI, et al. Fetal reduction and twins. Am J Obstet Gynecol MFM. 2022;4(2S):100521.
van de Mheen L, et al. Outcome of Multifetal Pregnancy Reduction in women with a Dichorionic Triamniotic Triplet pregnancy to a Singleton pregnancy: a Retrospective Nationwide Cohort Study. Fetal Diagn Ther. 2016;40(2):94–9.
Busnelli A, et al. Risk factors for monozygotic twinning after in vitro fertilization: a systematic review and meta-analysis. Fertil Steril. 2019;111(2):302–17.
Papageorghiou AT, et al. Risks of miscarriage and early preterm birth in trichorionic triplet pregnancies with embryo reduction versus expectant management: new data and systematic review. Hum Reprod. 2006;21(7):1912–7.
Luke B, Brown MB. Maternal morbidity and infant death in twin vs triplet and quadruplet pregnancies. Am J Obstet Gynecol, 2008. 198(4): p. 401 e1-10.
Selective first-trimester termination in octuplet and quadruplet pregnancies: clinical and ethical issues. 1988.
Evans MI, Andriole S, Britt DW. Fetal reduction: 25 years’ experience. Fetal Diagn Ther. 2014;35(2):69–82.
Kim MS, et al. Obstetrical outcomes of embryo reduction and fetal reduction compared to non-reduced twin pregnancies. Arch Gynecol Obstet. 2019;299(4):953–60.
Haas J, et al. Outcome of early versus late multifetal pregnancy reduction. Reprod Biomed Online. 2016;33(5):629–34.
Haas J, et al. Perinatal outcome of twin pregnancies after early transvaginal multifetal pregnancy reduction. Fertil Steril. 2014;101(5):1344–8.
Lin H, et al. Early fetal reduction of dichorionic triplets to dichorionic twin or singleton pregnancies: a retrospective study. Reprod Biomed Online. 2016;32(5):490–5.
Timor-Tritsch IE, et al. Two hundred ninety consecutive cases of multifetal pregnancy reduction: comparison of the transabdominal versus the transvaginal approach. Am J Obstet Gynecol. 2004;191(6):2085–9.
Coffler MS, et al. Early transvaginal embryo aspiration: a safer method for selective reduction in high order multiple gestations. Hum Reprod. 1999;14(7):1875–8.
Itskovitz J, et al. Transvaginal ultrasonography-guided aspiration of gestational sacs for selective abortion in multiple pregnancy. Am J Obstet Gynecol. 1989;160(1):215–7.
Lembet A, et al. Intracranial injection with KCl: an alternative method in selected cases of multifetal pregnancy reduction. Fetal Diagn Ther. 2009;26(3):134–6.
Li R, et al. Intracranial KCl injection–an alternative method for multifetal pregnancy reduction in the early second trimester. Fetal Diagn Ther. 2013;34(1):26–30.
Roman A, et al. Selective reduction in complicated monochorionic pregnancies: radiofrequency ablation vs. bipolar cord coagulation. Ultrasound Obstet Gynecol. 2010;36(1):37–41.
Yanaihara A, et al. Dichorionic triplets following frozen-thawed poor-stage embryo transfer: a report of two cases and a review. Reprod Biol Endocrinol. 2017;15(1):80.
Anthoulakis C, et al. Risks of miscarriage or preterm delivery in trichorionic and dichorionic triplet pregnancies with embryo reduction versus expectant management: a systematic review and meta-analysis. Hum Reprod. 2017;32(6):1351–9.
Beets G. A contemporary issue in demography: the rising age at first birth, pros and cons. AUC Geogr. 2011;46:5–14.
Knopman JM, et al. What makes them split? Identifying risk factors that lead to monozygotic twins after in vitro fertilization. Fertil Steril. 2014;102(1):82–9.
Hviid KVR, et al. Determinants of monozygotic twinning in ART: a systematic review and a meta-analysis. Hum Reprod Update. 2018;24(4):468–83.
Franasiak JM, et al. Blastocyst transfer is not associated with increased rates of monozygotic twins when controlling for embryo cohort quality. Fertil Steril. 2015;103(1):95–100.
Banker M, et al. International Committee for Monitoring Assisted Reproductive Technologies (ICMART): world report on assisted reproductive technologies, 2013. Fertil Steril. 2021;116(3):741–56.
Liu S, et al. Pregnancy and obstetric outcomes of dichorionic and trichorionic triamniotic triplet pregnancy with multifetal pregnancy reduction: a retrospective analysis study. BMC Pregnancy Childbirth. 2022;22(1):280.
Liu Y, et al. Clinical outcomes of multifetal pregnancy reduction in trichorionic and dichorionic triplet pregnancies: a retrospective observational study. Taiwan J Obstet Gynecol. 2019;58(1):133–8.
Acosta-Rojas R, et al. Twin chorionicity and the risk of adverse perinatal outcome. Int J Gynaecol Obstet. 2007;96(2):98–102.
Lopriore E, et al. Term perinatal mortality and morbidity in monochorionic and dichorionic twin pregnancies: a retrospective study. Acta Obstet Gynecol Scand. 2008;87(5):541–5.
Zemet R, et al. Pregnancy outcome after multifetal pregnancy reduction of triplets to twins versus reduction to singletons. Reprod Biomed Online. 2020;40(3):445–52.
Cai P, et al. Pregnancy outcomes of dichorionic triamniotic triplet pregnancies after in vitro fertilization-embryo transfer: multifoetal pregnancy reduction versus expectant management. BMC Pregnancy Childbirth. 2020;20(1):165.
Li R, et al. Retain singleton or twins? Multifetal pregnancy reduction strategies in triplet pregnancies with monochorionic twins. Eur J Obstet Gynecol Reprod Biol. 2013;167(2):146–8.
Lewi L, Deprest J, Hecher K. The vascular anastomoses in monochorionic twin pregnancies and their clinical consequences. Am J Obstet Gynecol. 2013;208(1):19–30.
Glinianaia SV, et al. Stillbirth and neonatal mortality in monochorionic and dichorionic twins: a population-based study. Hum Reprod. 2011;26(9):2549–57.
Hack KE, et al. Increased perinatal mortality and morbidity in monochorionic versus dichorionic twin pregnancies: clinical implications of a large Dutch cohort study. BJOG. 2008;115(1):58–67.
Rahimi-Sharbaf F, et al. Radiofrequency ablation for selective fetal reduction in complicated Monochorionic twins; comparing the outcomes according to the indications. BMC Pregnancy Childbirth. 2021;21(1):189.
Liu S, et al. Pregnancy and obstetric outcomes of dichorionic triamniotic triplet pregnancies with selective foetal reduction after assisted reproductive technology. Reprod Biol Endocrinol. 2024;22(1):30.
Dumez Y, Oury JF. Method for first trimester selective abortion in multiple pregnancy. Contrib Gynecol Obstet. 1986;15:50–3.
Salat-Baroux J, et al. The management of multiple pregnancies after induction for superovulation. Hum Reprod. 1988;3(3):399–401.
JA M et al. Births: final data for 2002. 2003. 52: pp. 1-113.
Zhou AJ, et al. Comparisons between two methods of multifetal pregnancy reduction in women with a dichorionic triamniotic triplet pregnancy. Taiwan J Obstet Gynecol. 2019;58(6):793–7.
Xia S, et al. Intertwin nuchal translucency difference predicts the chance of co-twin death after fetal reduction in dichorionic triplet pregnancies: a retrospective analysis study. BMC Pregnancy Childbirth. 2023;23(1):747.
Chaveeva P, et al. Trichorionic and dichorionic triplet pregnancies at 10–14 weeks: outcome after embryo reduction compared to expectant management. Fetal Diagn Ther. 2013;34(4):199–205.
Yang Y, Ye X, Sun X. Clinical outcomes of fetal selective reduction in dichorionic triplet pregnancies. J Chin Med Assoc. 2024;87(1):103–8.
Pharoah PO, Adi Y. Consequences of in-utero death in a twin pregnancy. Lancet. 2000;355(9215):1597–602.
Ong SS, et al. Prognosis for the co-twin following single-twin death: a systematic review. BJOG. 2006;113(9):992–8.
Dias T, et al. First-trimester ultrasound determination of chorionicity in twin pregnancy. Ultrasound Obstet Gynecol. 2011;38(5):530–2.
Bora SA, et al. Reliability of transvaginal ultrasonography at 7–9 weeks’ gestation in the determination of chorionicity and amnionicity in twin pregnancies. Ultrasound Obstet Gynecol. 2008;32(5):618–21.
Funding
This research was funded by the National Key R&D Program of China, grant number 2021YFC2700901, the National Natural Science Foundation of China, grant number 82001635, the Hefei Comprehensive National Science Center Medical-Industrial Integration Medical Equipment Innovation Research Platform Project, grant number 4801001202, the Clinical Medical research transformation Project of Anhui Province, grant number 202204295107020012, the Foundation for Selected Scientists Studying Abroad of Anhui Province, grant number 2022LCX015, and the Innovation and Entrepreneurship Training Program for Undergraduate Students of Anhui Medical University, grant number 202310366015, S202310366009.
Author information
Authors and Affiliations
Contributions
Q.X. and M.L. were responsible for data collection and writing the first draft; W.Z. was mainly responsible for supervising the research, conception, and review of papers; X.W. was responsible for the major revisions of the report; H.L. participated in the revision of this report. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of the images in Figs. 1 and 2.
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Ethics Committee of Anhui Medical University (PJ20180707). All methods were carried out in strict accordance with the relevant guidelines and regulations.
Consent to participate
Informed consent was obtained from all the parents.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Q., Li, M., Wang, X. et al. Dichorionic triamniotic triplets after two blastocysts transfer underwent multifetal pregnancy reduction: two case reports and literature review. BMC Women's Health 24, 492 (2024). https://doi.org/10.1186/s12905-024-03324-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-024-03324-4