Abstract
Objective
The aim of this study is to evaluate the findings of existing systematic reviews (SRs) and provide scientific evidence on the efficacy and safety of whole-body vibration (WBV) in improving bone mineral density (BMD) in postmenopausal women, to provide recommendations and guidance for future high-quality clinical research and SRs.
Methods
We conducted searches in six databases (SinoMed, CNKI, Cochrane Library, Embase, PubMed, Web of Science) from the inception of the databases until July 31, 2023. The language was limited to Chinese or English. The methodological quality, risk of bias, and evidence grade of outcomes were evaluated using AMSTAR-2, ROBIS, and GRADE, respectively. Additionally, the degree of overlap in randomized controlled trials (RCTs) among the SRs was calculated using corrected covered area (CCA). Furthermore, we performed quantitative synthesis or descriptive analysis of the relevant data. All relevant operations were independently conducted by two individuals.
Results
A total of 15 SRs were included in the analysis, out of which three were qualitative descriptions and 12 were meta-analyses. According to AMSTAR-2, only two SRs were rated as low or moderate, while the remaining 13 SRs were rated as critically low quality. The ROBIS assessment indicated that seven SRs had a low risk of bias, while 8 SRs had a high risk of bias. The overall findings suggest that WBV does not have a significant advantage in improving BMD in postmenopausal women. Furthermore, the CCA results revealed a high overlap in RCTs across five outcomes among the 15 SRs. Only five SRs reported specific adverse reactions/events experienced by participants after WBV interventions, and none of the SRs reported any severe adverse events.
Conclusion
The existing evidence cannot establish definitive advantages of WBV in improving BMD in postmenopausal women. Therefore, we do not recommend the use of WBV for improving BMD in postmenopausal women. However, WBV may have potential value in maintaining BMD in postmenopausal women, further research is needed to confirm these findings.
Similar content being viewed by others
Introduction
Bone mineral density (BMD) reflects the mineral content in bone tissue and is a crucial indicator for assessing bone mass and strength. It not only reflects the integrity of bone tissue but also acts as a crucial marker for assessing bone health and the ability of bone remodeling [1]. Research has shown that BMD decreases with age in the older adults [2]; compared to males, females typically start losing bone mass after the age of 40. Due to a sharp decline in hormone levels, postmenopausal women experience accelerated bone loss, leading to decreased BMD. The reduction in BMD further elevates the risk of osteoporotic fractures and related complications [3, 4]. Additionally, low BMD predisposes postmenopausal women to osteoporosis. Studies indicate that the prevalence of osteoporosis in Chinese women over 50 years old is approximately 20.7% [5], which is associated with higher mortality rates and treatment costs, imposing a heavier burden on individuals, families, and society. Furthermore, it can have an impact on the normal functional movement and quality of life in postmenopausal women [6,7,8]. With the continuous increase in the aging population and the uneven distribution of older adults’ care and medical resources, it poses a severe challenge to public health management [9, 10].
Compared to pharmacological interventions, exercise therapy significantly improves BMD and prevents fractures and osteoporosis in postmenopausal women, with fewer adverse events observed [11, 12]. However, for postmenopausal women, maintaining a certain intensity and sufficient duration of exercise and strength training may be more challenging. Limitations related to age and training conditions reduce the feasibility of these exercises [13, 14].
In recent years, whole-body vibration (WBV) has become increasingly common to improve BMD in postmenopausal women [4, 15]. Research indicates that WBV interventions involve subjects standing on a vibrating platform, which stimulates and transmits vibrations throughout the whole body, eliciting responses in muscles and bone tissues. Several clinical studies have suggested that WBV can enhance BMD in the femoral neck and proximal femur of postmenopausal women, and it may also have positive effects on muscle strength and alleviate depressive symptoms to some extent [16,17,18].
Numerous systematic reviews (SRs) have summarized the impact of WBV on BMD in postmenopausal women. Still, consensus has not been reached in some SRs regarding the effectiveness of WBV in improving BMD [15, 19, 20]. As the highest level of evidence synthesis, SRs integrate a large amount of data to assess the reliability and accuracy of the results [21]. However, there is substantial variation in the methodological quality, risk of bias, and quality of evidence among different SRs. Low-quality SRs can even mislead clinical decision-making, highlighting the need for a comprehensive summary and objective evaluation of relevant SRs. The overview method represents a novel approach to collecting data from diverse SRs, reassessing the methodological quality and risk of bias, and synthesizing individual data [22]. Compared to traditional SRs, an overview of SRs that reduces information duplication and presents SR findings in a uniform format can serve as a convenient reference for decision makers, healthcare professionals, and patients. Additionally, such an overview often emphasizes the methodological aspects of SRs, which can help identify potential biases that might lower the quality of evidence, thereby guiding the development of future high-quality SRs [23]. Therefore, we utilized this method to collect and summarize relevant data from SRs, aiming to provide an objective evaluation of the efficacy and safety of WBV in improving BMD in postmenopausal women. This serves to offer evidence-based guidance for public health practitioners and policymakers and provides recommendations for future researchers to conduct high-quality SRs and clinical studies.
Methods
Registration
This overview has been registered in advance on the PROSPERO (CRD42023432403).
Search strategy
We searched six databases (SinoMed, CNKI, Cochrane Library, Embase, PubMed, and Web of Science) from the inception of each database up to July 31, 2023. No restrictions were placed on the publication date of SRs or the studies included within them. The language was limited to Chinese or English. Relevant subject search terms were adjusted according to each database. In addition, we manually searched the reference lists of review articles for additional relevant studies. Please refer to Appendix 1 for the detailed search strategy.
Inclusion criteria
Study design and participants
SRs and meta-analysis that had included randomized controlled trials (RCTs) for analysis were eligible for inclusion [24]. The title of the included literature must be defined as a SR. The research questions and inclusion criteria of SR must include PICO (patient, intervention, comparison, outcome). Study participants were postmenopausal women, with no restrictions on their race or activity level. If an SR included RCTs recruiting both males and females, we read the full text, if the SR provided a separate textual summary or meta-analysis for postmenopausal women, it was included.
Study intervention
The primary intervention method utilized was WBV using a sinusoidal vibration platform, with no restrictions on the vibration frequency and intensity of WBV.
Study comparison
Other intervention methods besides WBV and pharmaceutical interventions, such as no intervention, regular exercise training, sham WBV, functional training, etc.
Study outcomes
BMD in different parts of the body, with no restrictions on the measurement methods for BMD.
Exclusion criteria
-
1.
SRs exclusively focusing on males will be excluded.
-
2.
SRs that compared WBV of different courses, frequencies, and intensities.
-
3.
SRs that included patients taking medication to increase BMD.
-
4.
Other types of studies, such as animal experiments, network meta-analyses, protocols, conference papers, case reports, guidelines, etc.
-
5.
Articles for which the full text cannot be obtained and those with duplicated data will be excluded.
Study selection and data extraction
Following a predetermined database and search strategy, all retrieved articles were imported into EndNote X9.1. After removing duplicates, two reviewers (YS and FYZ) completed the initial screening based on the title and abstract and read the full text for evaluation. Cross-checking was performed at each stage.
According to the inclusion criteria, two reviewers (ZQ and WX) independently extracted data, including author, publication year, WBV frequency and magnitude, number of RCTs and sample sizes, intervention and control measures, outcomes, quality assessment methods, adverse events, and major conclusions. Cross-checking was performed at each stage.
In the stages of study selection and data extraction, if there were discrepancies or differences in opinions and results between the two reviewers, the first step was to attempt resolution through discussion. If an agreement could not be reached, they consulted the third reviewer (FY), who made the final decision.
Evaluation methods
Two reviewers (YS and LY) independently assessed the methodological quality, risk of bias, and evidence quality of the SRs using AMSTAR-2 [25], ROBIS [26], and GRADE tools [27] with cross-checking. In the case of discrepancies or differences in opinions between the results and opinions, the first attempt is to resolve through discussion. If an agreement is still not reached, the final decision will be made by the third reviewer (FY).
AMSTAR-2 is a commonly used tool for assessing the methodological quality of SRs. It consists of 16 items covering the entire process of SRs, including topic selection, design, registration, data extraction, statistical analysis, and discussion. Each item is rated as “Yes” (accurate and sufficient), “No” (accurate but insufficient), or “Partial yes” (lacking relevant evaluation content or inappropriate evaluation). The overall confidence in the SR is graded as high, moderate, low, or critically low based on the overall confidence assessment.
The ROBIS tool is used to assess the risk of bias in the domains of “study eligibility criteria”, “identification and selection of studies”, “data collection and study appraisal”, and “synthesis and findings”. The overall risk of bias judgment is then made, with each domain classified as low risk, high risk, or unclear risk.
The GRADE system evaluates the evidence quality of the results based on five aspects: Risk of bias, Inconsistency, Indirectness, Imprecision, and Publication bias. The evidence quality is categorized as high certainty of evidence, moderate certainty of evidence, low certainty of evidence, or very low certainty of evidence.
Data synthesis and analysis
We summarized relevant data on the outcomes of BMD according to different anatomical sites and conducted a descriptive analysis. Our objective was to identify SRs containing non-overlapping primary studies for each outcome to avoid duplicating evidence. When multiple eligible SRs were identified for a single outcome, we calculated the corrected covered area (CCA) to determine the extent of overlap in the primary studies using the following formula:
where N represents the number of included publications (sum of checked boxes), r denotes the number of rows (number of RCTs), and c represents the number of columns (number of SRs). The CCA values are categorized as follows: “Slight overlap” for scores ranging from 0 to 5, “Moderate overlap” for scores from 6 to 10, “High overlap” for scores from 11 to 15, and “Very high overlap” for scores above 15 [28].
Furthermore, we provided a descriptive synthesis of the outcomes and relevant data. Continuous data were expressed as the summary mean difference (MD) or standardized mean difference (SMD) with a 95% confidence interval (CI). P < 0.05 indicated a statistically significant difference between groups.
Results
Characteristics of included SRs
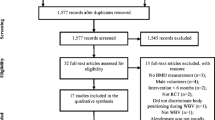
After retrieval, removal of duplicates, and full-text screening, we ultimately identified 15 SRs for further evaluation (12 of which conducted meta-analyses). The flowchart of the screening process is presented in Fig. 1, and the list of exclusions and reasons for the exclusions in the “Full-text assessment for eligibility” stage are shown in Appendix 1.
The 15 included SRs were published between 2009 and 2023, with three articles published in Chinese and the remaining 12 published in English. Among them, one SR had the largest sample size, including 23 RCTs with a total of 2,089 participants. Except for two SRs that did not mention the intensity of WBV, all other SRs reported both the frequency and intensity of WBV. Regarding follow-up records, only seven SRs indicated the dates of follow-up, and only five SRs mentioned adverse reactions, all of which were from the WBV group. Detailed characteristics of the included studies are presented in Table 1.
Methodological quality assessment of the included reviews
After assessing the methodological quality of the included SRs using AMASTAR-2, we found that 13 SRs had more than one serious flaw in the critical item and multiple flaws in the non-critical domains, resulting in a rating of critically low. The remaining two SRs were rated low and moderate, respectively. Among the critical items, only two SRs had pre-registered their study protocols (item 2), 10 SRs conducted comprehensive literature search strategies (item 4), 11 SRs provided lists of excluded studies and the reasons for exclusion (item 7), 10 SRs utilized appropriate tools to assess the risk of bias in RCTs (item 9), and 12 SRs employed appropriate statistical methods for meta-analysis (item 11). In comparison, three SRs did not conduct meta-analyses, 11 SRs considered the risk of bias in RCTs when interpreting or discussing the results (item 13), and only 1 SR investigated publication bias (item 15). Detailed assessment results can be found in Table 2.
Risk of bias
The results of the risk of bias assessment using the ROBIS tool for the 15 SRs showed that, through Phase 3’s summary and comprehensive evaluation, seven SRs (46.67%) were rated as low risk, while eight SRs (53.33%) were rated as high risk. Some of these SRs did not provide the necessary explanations or handling of bias risks in terms of search, data extraction, quality assessment, and heterogeneity, which may have resulted in an elevated risk of bias in the SRs. Detailed results can be found in Table 3 and Fig. 2.
Outcomes evaluation
Femoral neck BMD
Nine SRs examined the changes in femoral neck BMD in postmenopausal women after WBV intervention. Only one SR showed that WBV could improve femoral neck BMD in postmenopausal women compared to the control group [MD = 0.01, 95% CI (0.00, 0.01), p = 0.002, 7 RCTs, 304 participants] (moderate certainty of evidence) [34, 36]. Our statistical analysis found a high overlap of RCTs among the nine SRs (CCA = 13.67%). For more details, refer to Tables 4 and 5, and Appendix 2.
Trochanter BMD
Four SRs have conducted a statistical analysis on the effect of WBV on trochanter BMD in postmenopausal women, with four outcomes. Only two SRs demonstrated that WBV has the potential to improve Trochanter BMD in postmenopausal women compared to the control group [MD = 0.02, 95% CI (0.01, 0.03), P = 0.002, 4 RCTs, 127 participants (very low certainty of evidence); MD = 0.02, 95% CI (0.00, 0.03), P = 0.02, 5 RCTs, 212 participants] (low certainty of evidence) [15, 36]. The overlap among the RCTs in the four SRs was determined to be very high overlap (CCA = 33.33%). For additional results, please refer to Tables 4 and 5, and Appendix 2.
Total hip BMD
Four SRs assessed the effect of WBV intervention on total hip BMD in postmenopausal women, and the GRADE evaluation of outcomes rated them as low certainty of evidence and very low certainty of evidence, respectively. Among the four SRs, WBV did not demonstrate any advantage over the control group, and there was a very high overlap of RCTs among the SRs (CCA = 22.22%). Detailed results can be found in Tables 4 and 5, and Appendix 2.
Lumbar spine BMD
Eight SRs analyzed the effect of WBV intervention on lumbar spine BMD in postmenopausal women. Three SRs indicated that WBV had a statistically significant difference in improving lumbar spine BMD in postmenopausal women compared to the control group. [MD = 0.01, 95% CI (0.00, 0.03), p = 0.03, 5 RCTs, 280 participants] (low certainty of evidence) [35]; [MD = 0.01, 95% CI (0.00, 0.02), p = 0.0005, 9 RCTs, 913 participants] (low certainty of evidence) [36]; [MD = 0.01, 95% CI (0.00, 0.01), p = 0.004, 14 RCTs, 1351 participants] (low certainty of evidence) [15]. There was a very high overlap of RCTs among the eight SRs (CCA = 16.13%). Please refer to Tables 4 and 5, and Appendix 2 for details.
Whole body BMD
Two SRs conducted a statistical analysis of the whole body BMD results. Compared to conventional exercise, only one SR showed that WBV could improve BMD in postmenopausal women [SMD = 0.09, 95% CI (0.01, 0.08), p = 0.02, 7 RCTs, 602 participants] (low certainty of evidence) [38]. Please refer to Table 4 for specific results.
Review of the conclusions made by the authors of the included SRs
According to the conclusions of the SRs’ authors, we conducted a statistical analysis, including three viewpoints: supporting, neutral, and opposing. The statistical results showed that the authors of nine SRs believed that WBV may be effective in improving bone density in postmenopausal women. Still, the current evidence is insufficient, and further research is needed for confirmation. Additionally, four conclusions maintained a neutral stance, stating that the current quality of evidence is poor, making it difficult to provide a definitive answer. Two conclusions considered WBV to be ineffective.
Adverse effects
Only five SRs reported the specific adverse reactions/events that occurred in participants after WBV intervention, mainly including pain in various parts of the limbs, nausea, skin itching, weakness, and fear. All SRs did not report any severe adverse events, see Table 1.
Discussion
In this overview, 15 SRs on WBV improving postmenopausal women’s BMD were ultimately included, and their methodological quality, risk of bias, and evidence quality were comprehensively evaluated. Additionally, we analyzed and summarized the BMD of different parts of postmenopausal women, including the femoral neck, trochanter, total hip, lumbar spine,and whole body BMD. A descriptive analysis was performed on the relevant data. In the AMSTAR-2 evaluation results, 13 SRs (86.67%) were rated as critically low due to the lack of research plans and serious publication bias. According to the ROBIS assessment of SRs, seven SRs (46.67%) were rated low risk, while eight SRs (53.33%) were assessed as high risk. The main reasons for high risk included incomplete retrieval, insufficient data extraction, quality assessment, and inadequate heterogeneity explanation. Regarding the summary results of the outcomes, almost all evidence levels were very low. Only a few SRs demonstrated that WBV could effectively improve postmenopausal women’s BMD, specifically in the lumbar spine (3/8, three with low certainty of evidence), femoral neck (1/9, moderate certainty of evidence), and trochanter (2/4, one with low certainty of evidence and one with very low certainty of evidence). No study found additional benefits for the total hip (0/4).
In the study results, only five SRs reported specific adverse reactions/events in participants after WBV intervention, primarily including pain in various parts of the limbs, nausea, skin itching, weakness, and fear. All SRs did not report any severe adverse events, and the reporting of these adverse reactions provides a preliminary understanding of the safety of WBV in postmenopausal women. While these reactions may be temporary and mild discomfort, future research should focus on monitoring and reporting adverse events, especially in the context of long-term interventions. Further exploration of the specific mechanisms and potential effects of these mild adverse reactions is needed for a more comprehensive and objective assessment of the safety of WBV. This will provide more reliable evidence for its application in clinical practice.
Due to the ability of WBV to induce mechanical oscillations sensed by bone cells, it has gained attention as a non-pharmacological treatment or rehabilitation training for improving bone health, particularly in postmenopausal women at increased risk of osteoporosis [39]. However, research on the effects of WBV training on bone adaptation in humans has produced inconsistent results. Some studies have found significant improvements in BMD in the hip and lumbar spine of postmenopausal women after 6–12 months of WBV training [40, 41]. However, other studies have found no changes in bone mineral content in the spine, hip, and distal radius of individuals after 12 months of WBV training [42].
Among the 15 SRs analyzed, there was also inconsistency in the findings regarding the effects of WBV training on BMD in different body regions. Additionally, the lack of standardized terminology and broad usage scenarios for WBV hinders the design of high-quality studies and compromises reproducibility, result reporting, comparability across studies, and the ability to reconcile conflicting findings [43]. Therefore, further exploration is warranted in studying the effects of WBV on BMD in postmenopausal women.
Although WBV does not significantly improve BMD in postmenopausal women, its potential value in maintaining BMD is particularly important because postmenopausal women face significant challenges in preventing bone loss. As estrogen levels decline after menopause, the rate of bone loss accelerates, increasing the risk of osteoporosis and fractures [44]. Traditional interventions, such as pharmacotherapy and weight-bearing exercises, can improve or maintain BMD to some extent, but they also have limitations. Pharmacotherapy often comes with side effects, and long-term use may lead to decreased patient adherence [45]. Weight-bearing exercises require a high level of physical fitness and exercise habits, but many postmenopausal women find it difficult to adhere to them for various reasons, such as poor physical condition, lack of exercise habits, or fear of injury [46]. WBV is simple to implement, has high safety, and is suitable for postmenopausal women of all fitness levels. For women who cannot or do not wish to engage in more intense physical activities, WBV provides a valuable supplementary or alternative strategy. It has potential benefits in maintaining BMD, improving muscle strength and balance, thereby reducing the risk of falls and fractures [16,17,18]. Future research should continue to explore the effects of WBV on maintaining BMD in postmenopausal women and identify the best implementation strategies to better serve this specific population.
Strengths and limitations
Through comprehensive searches and full-text reading, a total of 15 SRs were included. We summarized the relevant parameters of WBV, such as vibration frequency and magnitude, to provide a reference for future research. The methodological quality and risk of bias of the included SRs were rigorously assessed using AMSTAR-2 and ROBIS. Outcomes were extracted, and GRADE was used to objectively evaluate the level of evidence. Additionally, we calculated the CCA of the original RCTs within the SRs to avoid duplication bias. Regarding literature screening, data extraction, summarization, and evaluation, two independent researchers performed the procedures to minimize bias and improve the reliability of the results.
The subjectivity of the assessment tools and potential biases in our understanding of these tools may influence on our final results.
Conclusion
The existing evidence cannot establish definitive advantages of WBV in improving BMD in postmenopausal women. Therefore, we do not recommend the use of WBV for improving BMD in postmenopausal women. However, WBV may have potential value in maintaining BMD in postmenopausal women, further research is needed to confirm these findings.
Availability of data and materials
Data is provided within the manuscript or supplementary information files.
Abbreviations
- BMD:
-
Bone mineral density
- CCA:
-
Corrected Covered Area
- WBV:
-
Whole-body vibration
- SR:
-
Systematic review
- RCT:
-
Randomized controlled trial
References
Liu YL, Ruan XY, Wu HQ. Changes of body composition and resting energy metabolism in perimenopausal women. Chin Tissue Eng Res. 2015;19(42):6808–12.
Jiang Y, Zhang Y, Jin M, Gu Z, Pei Y, Meng P. Aged-related changes in body composition and association between body composition with bone mass density by body mass index in Chinese Han men over 50-year-old. PLoS One. 2015;10(6):e0130400. https://doi.org/10.1371/journal.pone.0130400. Epub 2015/06/20. PubMed PMID: 26090818; PubMed Central PMCID: PMCPMC4475062.
Fu X, Ma X, Lu H, He W, Wang Z, Zhu S. Associations of fat mass and fat distribution with bone mineral density in pre- and postmenopausal Chinese women. Osteoporos Int. 2011;22(1):113–9. https://doi.org/10.1007/s00198-010-1210-9. Epub 2010/03/23. PubMed PMID: 20306018.
Guedes De Aguiar EO, Moreira Marconi E, Monteiro-Oliveira BB, Gomes-Santos AC, Coelho Oliveira AC, Paineiras-Domingos LL, et al. Whole-body vibration exercise improves the functionality in postmenopausal women: a systematic review. Iran J Public Health. 2023;52(3):476–87. https://doi.org/10.18502/ijph.v52i3.12131. Epub 2023/05/01. PubMed PMID: 37124907; PubMed Central PMCID: PMCPMC10135517.
Zhang ZH, Liu ZH, Li N, Zhang MM, Huang QR, Ma YZ, et al. Expert Consensus on the diagnostic criteria of Osteoporosis in Chinese people (Third draft ·2014 edition). Chin J Osteoporosis. 2014;20(9):1007–10.
Ma C, Liu A, Sun M, Zhu H, Wu H. Effect of whole-body vibration on reduction of bone loss and fall prevention in postmenopausal women: a meta-analysis and systematic review. J Orthop Surg Res. 2016;11:24. https://doi.org/10.1186/s13018-016-0357-2. Epub 2016/02/19. PubMed PMID: 26888467; PubMed Central PMCID: PMCPMC4758089.
Benzinger P, Riem S, Bauer J, Jaensch A, Becker C, Büchele G, et al. Risk of institutionalization following fragility fractures in older people. Osteoporos Int. 2019;30(7):1363–70. https://doi.org/10.1007/s00198-019-04922-x. Epub 2019/03/17. PubMed PMID: 30877349.
Autier P, Haentjens P, Bentin J, Baillon JM, Grivegnée AR, Closon MC, et al. Costs induced by hip fractures: a prospective controlled study in Belgium. Belgian Hip Fracture Study Group. Osteoporos Int. 2000;11(5):373–80. https://doi.org/10.1007/s001980070102. Epub 2000/07/27. PubMed PMID: 10912837.
Man W, Wang S, Yang H. Exploring the spatial-temporal distribution and evolution of population aging and social-economic indicators in China. BMC Public Health. 2021;21(1):966. https://doi.org/10.1186/s12889-021-11032-z. Epub 2021/05/23. PubMed PMID: 34020620; PubMed Central PMCID: PMCPMC8140474.
Barron RL, Oster G, Grauer A, Crittenden DB, Weycker D. Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporos Int. 2020;31(11):2103–11. https://doi.org/10.1007/s00198-020-05294-3. Epub 2020/07/03. PubMed PMID: 32613410; PubMed Central PMCID: PMCPMC7560920.
Tarantino U, Iolascon G, Cianferotti L, Masi L, Marcucci G, Giusti F, et al. Clinical guidelines for the prevention and treatment of osteoporosis: summary statements and recommendations from the Italian Society for Orthopaedics and Traumatology. J Orthop Traumatol. 2017;18(Suppl 1):3–36. https://doi.org/10.1007/s10195-017-0474-7. Epub 2017/10/24. PubMed PMID: 29058226; PubMed Central PMCID: PMCPMC5688964.
Kemmler W, Shojaa M, Kohl M, von Stengel S. Effects of different types of exercise on bone mineral density in postmenopausal women: a systematic review and meta-analysis. Calcif Tissue Int. 2020;107(5):409–39. https://doi.org/10.1007/s00223-020-00744-w. Epub 2020/08/14. PubMed PMID: 32785775; PubMed Central PMCID: PMCPMC7546993.
Burton E, Hill AM, Pettigrew S, Lewin G, Bainbridge L, Farrier K, et al. Why do seniors leave resistance training programs? Clin Interv Aging. 2017;12:585–92. https://doi.org/10.2147/cia.S128324. Epub 2017/04/11. PubMed PMID: 28392682; PubMed Central PMCID: PMCPMC5375632.
Sherrington C, Fairhall N, Wallbank G, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med. 2020;54(15):885–91. https://doi.org/10.1136/bjsports-2019-101512. Epub 2019/12/04. PubMed PMID: 31792067.
de Oliveira RDJ, de Oliveira RG, de Oliveira LC, Santos-Filho SD, Sá-Caputo DC, Bernardo-Filho M. Effectiveness of whole-body vibration on bone mineral density in postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2023;34(1):29–52. https://doi.org/10.1007/s00198-022-06556-y. Epub 2022/10/26. PubMed PMID: 36282343.
ElDeeb AM, Abdel-Aziem AA. Effect of whole-body vibration exercise on power profile and bone mineral density in postmenopausal women with osteoporosis: a randomized controlled trial. J Manipulative Physiol Ther. 2020;43(4):384–93. https://doi.org/10.1016/j.jmpt.2019.12.003. Epub 20200828. PubMed PMID: 32868028.
Sen EI, Esmaeilzadeh S, Eskiyurt N. Effects of whole-body vibration and high impact exercises on the bone metabolism and functional mobility in postmenopausal women. J Bone Miner Metab. 2020;38(3):392–404. https://doi.org/10.1007/s00774-019-01072-2. Epub 20200102. PubMed PMID: 31897748.
Cheng L, Qian L, Chang S, He B. Effects of whole-body vibration training with the same amplitude and different frequencies on the proximal femoral bone density in elderly women. J Sports Med Phys Fitness. 2021;61(7):923–7. https://doi.org/10.23736/s0022-4707.20.11514-7. Epub 20201104. PubMed PMID: 33146497.
Mikhael M, Orr R, Fiatarone Singh MA. The effect of whole body vibration exposure on muscle or bone morphology and function in older adults: a systematic review of the literature. Maturitas. 2010;66(2):150–7. https://doi.org/10.1016/j.maturitas.2010.01.013. Epub 2010/02/23. PubMed PMID: 20171817.
Luo X, Zhang J, Zhang C, He C, Wang P. The effect of whole-body vibration therapy on bone metabolism, motor function, and anthropometric parameters in women with postmenopausal osteoporosis. Disabil Rehabil. 2017;39(22):2315–23. https://doi.org/10.1080/09638288.2016.1226417. Epub 2016/10/11. PubMed PMID: 27718643.
Mulrow CD. Rationale for systematic reviews. BMJ. 1994;309(6954):597–9. https://doi.org/10.1136/bmj.309.6954.597. Epub 1994/09/03. PubMed PMID: 8086953; PubMed Central PMCID: PMCPMC2541393.
Pollock M, Fernandes RM, Becker LA, Featherstone R, Hartling L. What guidance is available for researchers conducting overviews of reviews of healthcare interventions? A scoping review and qualitative metasummary. Syst Rev. 2016;5(1):190. https://doi.org/10.1186/s13643-016-0367-5. Epub 20161114. PubMed PMID: 27842604; PubMed Central PMCID: PMCPMC5109841.
Gates M, Gates A, Pieper D, Fernandes RM, Tricco AC, Moher D, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. 2022;378:e070849. https://doi.org/10.1136/bmj-2022-070849. Epub 20220809. PubMed PMID: 35944924; PubMed Central PMCID: PMCPMC9361065.
Linares-Espinós E, Hernández V, Domínguez-Escrig JL, Fernández-Pello S, Hevia V, Mayor J, et al. Methodology of a systematic review. Actas Urol Esp (Engl Ed). 2018;42(8):499–506. https://doi.org/10.1016/j.acuro.2018.01.010. Epub 20180503. PubMed PMID: 29731270.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. https://doi.org/10.1136/bmj.j4008. Epub 20170921. PubMed PMID: 28935701; PubMed Central PMCID: PMCPMC5833365.
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34. https://doi.org/10.1016/j.jclinepi.2015.06.005. Epub 20150616. PubMed PMID: 26092286; PubMed Central PMCID: PMCPMC4687950.
Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004;4(1):38. https://doi.org/10.1186/1472-6963-4-38. Epub 20041222. PubMed PMID: 15615589; PubMed Central PMCID: PMCPMC545647.
Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75. https://doi.org/10.1016/j.jclinepi.2013.11.007. Epub 2014/03/04. PubMed PMID: 24581293.
Merriman H, Jackson K. The effects of whole-body vibration training in aging adults: a systematic review. J Geriatr Phys Ther. 2009;32(3):134–45. https://doi.org/10.1519/00139143-200932030-00009.
Slatkovska L, Alibhai SM, Beyene J, Cheung AM. Effect of whole-body vibration on BMD: a systematic review and meta-analysis. Osteoporos Int. 2010;21(12):1969–80. https://doi.org/10.1007/s00198-010-1228-z.
Sitjà-Rabert M, Rigau D, Fort Vanmeerghaeghe A, Romero-Rodríguez D, Bonastre Subirana M, Bonfill X. Efficacy of whole body vibration exercise in older people: a systematic review. Disabil Rehabil. 2012;34(11):883–93. https://doi.org/10.3109/09638288.2011.626486.
Fratini A, Bonci T, Bull AM. Whole Body Vibration Treatments in Postmenopausal Women Can Improve Bone Mineral Density: Results of a Stimulus Focussed Meta-Analysis. PLoS One. 2016;11(12):e0166774. https://doi.org/10.1371/journal.pone.0166774.
Oliveira LC, Oliveira RG, Pires-Oliveira DA. Effects of whole body vibration on bone mineral density in postmenopausal women: a systematic review and meta-analysis. Osteoporos Int. 2016;27(10):2913–33. https://doi.org/10.1007/s00198-016-3618-3.
Xie C, Jin CJ, Zhang J, Zhang ZY. Meta-analysis of the effect of whole body vibration on bone mineral density in women [J]. Modern Preventive Medicine. 2016;43(23):4290–5, 4305. (in Chinese).
Marín-Cascales E, Alcaraz PE, Ramos-Campo DJ, Martinez-Rodriguez A, Chung LH, Rubio-Arias J. Whole-body vibration training and bone health in postmenopausal women: a systematic review and meta-analysis. Medicine (Baltimore). 2018;97(34):e11918. https://doi.org/10.1097/md.0000000000011918. PubMed PMID: 30142802; PubMed Central PMCID: PMCPMC6112924.
Huang L, Peng L. Effect of exercise on bone mineral density in postmenopausal women: a meta-analysis based on vibration training [J]. Health Medicine Research and Practice. 2019;16(01):37–43+47.
Chai NB. A systematic review and meta-analysis of the intervention effect of whole body vibration training on bone mineral density and fall risk in menopausal women [D]. Beijing sport university. 2021. (master's thesis). https://doi.org/10.26961/d.cnki.gbjtu.2021.000505.
DadeMatthews OO, Agostinelli PJ, Neal FK, Oladipupo SO, Hirschhorn RM, Wilson AE, et al. Systematic review and meta-analyses on the effects of whole-body vibration on bone health. Complement Ther Med. 2022;65:102811. https://doi.org/10.1016/j.ctim.2022.102811. Epub 2022/01/31. PubMed PMID: 35093509.
Judex S, Rubin CT. Is bone formation induced by high-frequency mechanical signals modulated by muscle activity? J Musculoskelet Neuronal Interact. 2010;10(1):3–11. Epub 2010/03/02. PubMed PMID: 20190375; PubMed Central PMCID: PMCPMC2919567.
Iwamoto J, Takeda T, Sato Y, Uzawa M. Effect of whole-body vibration exercise on lumbar bone mineral density, bone turnover, and chronic back pain in post-menopausal osteoporotic women treated with alendronate. Aging Clin Exp Res. 2005;17(2):157–63. https://doi.org/10.1007/bf03324589. Epub 2005/06/28. PubMed PMID: 15977465.
Verschueren SM, Roelants M, Delecluse C, Swinnen S, Vanderschueren D, Boonen S. Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. J Bone Miner Res. 2004;19(3):352–9. https://doi.org/10.1359/jbmr.0301245. Epub 2004/03/26. PubMed PMID: 15040822.
Rubin C, Recker R, Cullen D, Ryaby J, McCabe J, McLeod K. Prevention of postmenopausal bone loss by a low-magnitude, high-frequency mechanical stimuli: a clinical trial assessing compliance, efficacy, and safety. J Bone Miner Res. 2004;19(3):343–51. https://doi.org/10.1359/jbmr.0301251. Epub 2004/03/26. PubMed PMID: 15040821.
Wuestefeld A, Fuermaier ABM, Bernardo-Filho M, da Cunha de Sá-Caputo D, Rittweger J, Schoenau E, et al. Towards reporting guidelines of research using whole-body vibration as training or treatment regimen in human subjects-a Delphi consensus study. PLoS One. 2020;15(7):e0235905. https://doi.org/10.1371/journal.pone.0235905. Epub 2020/07/23. PubMed PMID: 32697809; PubMed Central PMCID: PMCPMC7375612.
Senthilraja M, Cherian KE, Jebasingh FK, Kapoor N, Paul TV, Asha HS. Osteoporosis knowledge and beliefs among postmenopausal women: a cross-sectional study from a teaching hospital in southern India. J Family Med Prim Care. 2019;8(4):1374–8. https://doi.org/10.4103/jfmpc.jfmpc_95_19. PubMed PMID: 31143724; PubMed Central PMCID: PMCPMC6510091.
Paskins Z, Babatunde O, Sturrock A, Toh LS, Horne R, Maidment I. Supporting patients to get the best from their osteoporosis treatment: a rapid realist review of what works, for whom, and in what circumstance. Osteoporos Int. 2022;33(11):2245–57. https://doi.org/10.1007/s00198-022-06453-4. Epub 20220611. PubMed PMID: 35688897; PubMed Central PMCID: PMCPMC9568441.
de Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BC. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009;20(12):2111–25. https://doi.org/10.1007/s00198-009-0938-6. Epub 20090507. PubMed PMID: 19421702.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
S.Y., Q.C. and F.Z. wrote the main manuscript text, and Q.Z., X.W. and M.C. prepared figures 1-2. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yin, S., Liu, Y., Zhong, Y. et al. Effects of whole-body vibration on bone mineral density in postmenopausal women: an overview of systematic reviews. BMC Women's Health 24, 444 (2024). https://doi.org/10.1186/s12905-024-03290-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-024-03290-x