Abstract
Background
Uganda has approximately 1.2 million people aged 15–64 years living with human immunodeficiency virus (HIV). Previous studies have shown a higher prevalence of premalignant cervical lesions among HIV-positive women than among HIV-negative women. Additionally, HIV-infected women are more likely to have human papilloma virus (HPV) infection progress to cancer than women not infected with HIV. We determined the prevalence of premalignant cervical lesions and their association with HIV infection among women attending a cervical cancer screening clinic at Mbarara Regional Referral Hospital (MRRH) in southwestern Uganda.
Methods
We conducted a comparative cross-sectional study of 210 women aged 22–65 years living with HIV and 210 women not living with HIV who were systematically enrolled from March 2022 to May 2022. Participants were subjected to a structured interviewer-administered questionnaire to obtain their demographic and clinical data. Additionally, Papanicolaou smears were obtained for microscopy to observe premalignant cervical lesions. Multivariate logistic regression was performed to determine the association between HIV status and premalignant cervical lesions.
Results
The overall prevalence of premalignant cervical lesions in the study population was 17% (n = 72; 95% C.I: 14.1–21.4), with 23% (n = 47; 95% C.I: 17.8–29.5) in women living with HIV and 12% (n = 25; 95% C.I: 8.2–17.1) in women not living with HIV (p < 0.003). The most common premalignant cervical lesions identified were low-grade squamous intraepithelial lesions (LSIL) in both women living with HIV (74.5%; n = 35) and women not living with HIV (80%; n = 20). HIV infection was significantly associated with premalignant lesions (aOR: 2.37, 95% CI: 1.27–4.42; p = 0.007).
Conclusion
Premalignant cervical lesions, particularly LSILs, were more common in HIV-positive women than in HIV-negative women, highlighting the need to strengthen the integration of cervical cancer prevention strategies into HIV care programs.
Similar content being viewed by others
Introduction
Cervical cancer is the fourth most common cancer among women worldwide [1, 2] and the leading cause of cancer-related deaths in developing countries [3,4,5]. It is preventable through vaccination, screening and treatment for human papilloma virus (HPV) infection and premalignant cervical lesions [5]. Approximately 570,000 cases of cervical cancer and 311 000 deaths from the disease occurred worldwide in 2018 [6]. The incidence of cervical cancer in Uganda is one of the highest in the world, with an age-standardized rate of 54.8 per 100,000 women per year [7], and the prevalence of premalignant cervical lesions is 22% [8].
A premalignant cervical lesion is the presence of proliferative dysplastic cells confined to the epithelium of the cervix [9]. These lesions may be classified based on the Bethesda classification, which includes atypical cells, low-grade squamous intraepithelial lesions (LSILs) and high-grade squamous intraepithelial lesions (HSILs) [10, 11]. Studies have shown that 10% of patients who have LSIL progress to HSIL [12]. Other classifications include cervical intraepithelial neoplasia (CIN), which can be further classified as CIN 1, 2, or 3 according to the level of dysplasia, where CIN 1 is a low-grade squamous intraepithelial lesion, while CIN 2 or 3 are high-grade squamous intraepithelial lesions [13]. Approximately 1–2% of women worldwide are estimated to develop CIN 2 and 3 each year, and the prevalence is reportedly high in human immunodeficiency virus (HIV)-positive women, at 10% [14]. These premalignant cervical lesions are preceded by persistent infection with high-risk human papilloma virus (HPV), especially types 16 and 18 [15]. This leads to the integration of HPV into host deoxyribonucleic acid (DNA), which leads to resistance to apoptosis, causing uncensored cell growth and hence progression to premalignant cervical lesions [16]. Premalignant cervical lesions are easier to manage before progression to cervical cancer occurs [17, 18].
Premalignant cervical lesions progress in stages from low-grade squamous intraepithelial lesions to high-grade squamous intraepithelial lesions and eventually to cancer [9]. The overall progression to cancer takes 10–20 years [9]. HIV-positive women have higher rates of progression to carcinoma and lower rates of regression than HIV-negative women. Compared with HIV-negative women, HIV-positive women have an increased risk of HPV infection and precancerous lesions [19]. HIV-positive women are approximately 3 times more likely to have their HPV infection progress to HSIL than HIV-negative women are [19]. This is because of a decrease in T-cell surveillance in HIV infection, which allows HPV replication, resulting in persistence of HPV infection, the accumulation of mutations in infected cells, and the subsequent proliferation of dysplastic cells [20]. HPV infection among HIV-positive women is strongly associated with low cluster of differentiation 4 (CD4) counts and high HIV viral load [21]. Women infected with HIV have a higher risk of incidence and persistence of human papillomavirus (HPV)-associated premalignant cervical lesions than women without HIV because HIV increases the entry of HPV into host DNA and enhances cell dysplasia [17, 18].
HIV-associated premalignant cervical lesions are thought to progress through the microsatellite instability pathway, whereas HIV-negative lesions progress through loss of heterozygosity. Interactions are likely via viral proteins, with HIV proteins enhancing the effectiveness of HPV proteins and possibly contributing to cell cycle disruption. Dysregulation of the cellular and humoral arms of the local and systemic immune systems may ensure disease progression [22]. The HIV provirus encodes structural retrovirus proteins that include gag, pol, env, tat, rev, vif, nef, vpr, and vpu. With regard to premalignant cervical lesions, tat and rev are two control mechanisms for viral gene expression. The tat protein enhances the transcription of viral genes, whereas rev acts post-transcriptionally, shuttling viral messenger ribonucleic acid (mRNA) from the nucleus to the cytoplasm [23].
In HIV-negative women with competent immune systems, most infections are cleared spontaneously because of a cell-mediated immune response regulated by CD4 + lymphocytes. However, in HIV-infected individuals, there is a higher risk of persistent HPV infection largely due to their impaired ability to clear HPV infection; hence, they are at increased risk of developing cervical dysplasia [16]. HIV-positive women with low CD4 lymphocyte counts have the highest prevalence of HPV infection and have shown higher detection rates of mixed HPV types with persistent infection [18]. Increased access to antiretroviral therapy (ART) has increased the life expectancy of women living with HIV, but many of these women remain susceptible to high-risk HPV infection, persistent disease, cervical lesion incidence and progression to carcinoma of the cervix [24]. The association between HIV and premalignant cervical lesions is moderated by several other factors, such as early age at first sexual intercourse, multiple sexual partners, previous history of sexually transmitted infections (e.g., chlamydia infections), level of education, oral contraceptive use, multiparity, smoking and low body mass index [25,26,27,28].
The prevalence of HIV in women living in Uganda is 7.2%, and Mbarara city has a prevalence of 7.9%, which is the second highest prevalence among districts in Uganda [29]. In Mbarara City, during July–September 2020, 18 (75%) of the women who had cervical cancer were HIV positive, and 10 (42%) of those women were referred from the cervical cancer screening clinic at Mbarara Regional Referral Hospital (MRRH) [30]. However, in our setting, limited studies have been conducted to understand the association of premalignant cervical lesion among HIV positive women and HIV negative women. Such information is crucial for better informing logistical planning, early identification of lesions to avoid progression to cancer, and addressing the other modifiable risk factors that are associated with premalignant cervical lesions. Thus, this study investigated the prevalence of premalignant cervical lesions and their association with HIV status among women attending the cervical cancer screening clinic at the MRRH.
Methods
Study design and period
This was a comparative cross-sectional study conducted among women attending the cervical cancer screening clinic of MRRH over a period of three months from March 2022 to May 2022.
Study area
The study was conducted at the cervical cancer screening clinic of MRRH, which is a government tertiary hospital that also serves as the teaching hospital for Mbarara University of Science and Technology (MUST). The hospital is located in Mbarara City, southwestern part of Uganda, approximately 260 km southwest of Kampala, the capital city of Uganda. It provides preventive, diagnostic, curative and rehabilitation services to patients from the 13 catchment districts, which have a population of approximately 5 million people in southwestern Uganda.
The cervical cancer screening runs daily, with an average daily attendance of 15 patients equally distributed among HIV-positive and HIV-negative women aged 22 to 65 years. The clinic is run by specialist physicians and midwives, and it offers cervical cancer screening using visual inspection with acetic acid or Lugol’s iodine and Papanicolaou (Pap) smears, especially for postmenopausal women. Ablative therapy is offered for precancerous lesions by thermocoagulation and loop electrosurgical procedures.
Colposcopy-guided biopsy, endocervical curettage and diagnostic conization are also performed [31]. Once the Pap smears are collected, they are sent to the histopathology department of the hospital for staining and reading by a pathologist at Mbarara Regional Referral hospital and every 10th smear examined by an independent pathologist at Mulago Specialized Women and Neonatal Hospital.
Study population, sample size and sampling
The study population included women who attended the cervical cancer screening clinic at MRRH. Women who were in their menses, who had active vaginal bleeding and who had suspicious lesions for cervical cancer were excluded. A sample size of 420 (210 HIV-positive and 210 HIV-negative women) was estimated using the formula for comparison of two proportions [32], with a 95% confidence interval (CI), a power of 80%, a prevalence of premalignant cervical lesions of 12.6% in HIV-positive women and 4.6% among HIV-negative women [33], and a 10% non-satisfactory Pap smear. On average, an estimated 900 women are screened for cervical cancer at MRRH every three months [30]. Dividing 900 by the sample size (420) gives a sampling interval (k) of two. Considering the two strata of HIV-positive and HIV-negative women, we used systematic sampling to recruit every second woman in each stratum following their order of coming to the clinic until the sample size was reached in each group. The rotary method of simple random sampling was used to select the first participant in each stratum. If the selected participant was not eligible for the study, we chose the next immediate woman whom we subjected to the sampling interval to obtain the next participant. This was performed until a maximum sample size of 420 (210 from each group) was obtained.
Inclusion and exclusion criteria
All women who came for cervical cancer screening at the cervical cancer screening clinic at Mbarara Regional Referral Hospital were potential participants but excluded if they had menses or had active vaginal bleeding, or visible suspicious lesions for cervical cancer. This is because the red blood cells contained in menses and vaginal bleeding interfere with reading the slides under a microscope where as those with suspicious lesions, biopsy was recommended instead.
Variables
Dependent variable
The dependent variable was the presence of a premalignant cervical lesion on Pap smear examination based on the Bethesda 2014 classification system [10, 11, 34]. Briefly, lesions were considered premalignant if they had atypical cells, low-grade squamous intraepithelial lesions (LSILs), high-grade squamous intraepithelial lesions (HSILs), or atypical glandular cells.
Independent variables
We collected data on medical factors, which included HIV status, body mass index (BMI), and history of other sexually transmitted infections (STIs). The socio-demographic factors assessed were age, religion, education level, residence, employment status, marital status and smoking status (ever smoked or not). In addition, we obtained data on reproductive health factors, including parity, age at first sexual intercourse, abortion history, number of sexual partners in the past 20 years and oral contraceptive use.
Data collection
After obtaining written informed consent, socio-demographic data was collected using a questionnaire. Information on HIV serostatus was obtained by looking at documented evidence of participants HIV status or testing using the national HIV algorithm as shown in Fig. 1 [35]. These women were then grouped into two different strata depending on their HIV status (HIV-positive and HIV-negative). Research assistants then interviewed the respondents face to face using a pretested structured coded questionnaire, after which the respondents were then taken for Pap smear collection.
Weight and height measurements were performed using standardized scales and stadiometers according to the hospital standard operating procedures.
All anthropometric measurements were taken twice, and the mean was entered into the questionnaire. The data collection was supervised, and the completed questionnaires were reviewed for completeness on a daily basis.
Pap smear collection
A pap smear was collected as per standard operating procedures by a qualified study staff, stained and read by a histopathologist. Slides were read by two readers, any discrepancy in results was read by a third reader who acted as a tie breaker.
Interpretation of pap smear results
We used the Bethesda 2014 classification system for interpretation of precancerous cervical smears stained by the Pap method [10,11,12].
Quality control
Pap smears were read by a pathologist at Mbarara Regional Referral hospital and every 10th smear was examined by an independent pathologist at Mulago Specialized Women and Neonatal Hospital. Inter rater reliability testing was done by calculating Cohen’s kappa coefficient and results were found consistent. All participants were screened for HIV status.
Data analysis
The data were collected using REDCap software, and exported to STATA version 15.0 (StataCorp, College Station, Texas, USA) for cleaning and subsequent analysis. To describe the prevalence of premalignant cervical lesions among HIV-positive and HIV-negative women attending the cervical cancer screening clinic at MRRH, the number of participants with premalignant lesions in each group was divided by the total number of participants in each group and expressed as a percentage. We used the chi-square test (χ2) to compare the prevalence of premalignant cervical lesions among HIV-positive and HIV-negative women. To establish the association between HIV status and premalignant cervical lesions, we used bivariate and multivariate logistic regression analyses to generate crude odds ratios (cORs) and adjusted odds ratios (aORs) with 95% confidence intervals (CIs), respectively. Variables with p < 0.2 in the bivariate analysis or those that were biologically plausible were entered into a multivariate logistic regression model to identify factors independently associated with premalignant lesions. p < 0.05 indicated statistically significant associations between the outcome and the independent variables at both the bivariate and multivariate analyses.
Results
Baseline social demographic characteristics
Study flow chart
Among 616 women who attended the clinic during the study, 420 participants were enrolled using stratified sampling and excluded 29 women who had vaginal bleeding and 23 women who had suspicious lesions for cancer. Whereas the 7 HIV-positive women who had suspicious lesions for cancer on Pap smear were also excluded from the study (Fig. 2).
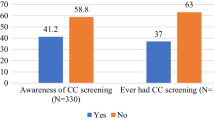
The participants differed in age, marital status, employment status, and level of education. HIV-positive women were older than HIV-negative women, and women who were unmarried were more likely to be HIV positive. The distribution of employment types, marital status and education level differed significantly between the two groups. The mean age of all the participants was 45 years (± 11.6), as shown in Table 1. Most HIV-positive women had their first sexual intercourse at the age < 18 years, whereas most HIV-negative women started their first sexual intercourse at the age ≥ 18 years (54.8% vs. 70.5%, respectively). Compared with HIV-positive women, HIV-negative women had a greater history of STIs and had used combined oral contraceptives in the last 5 years. Compared with HIV-negative women, HIV-positive women had a history of two or more sexual partners in the last 20 years (Table 1).
Prevalence of premalignant lesions and associated factors
The overall prevalence of premalignant cervical lesions in the study population was 17% (n = 72), with 23% (n = 47) in HIV-positive women and 12% (n = 25) in HIV-negative women (p < 0.003). The most common premalignant cervical lesions identified were low-grade squamous intraepithelial lesions (LSIL) in both HIV-positive (74%; n = 35) and HIV-negative women (80%; n = 20) (Table 2).
According to our multivariate analysis, none of the sociodemographic factors were associated with premalignant lesions. HIV status was independently associated with premalignant cervical lesions in women attending the cervical cancer screening clinic at MRRH. An HIV-positive woman was approximately 2.4 times more likely to have premalignant cervical lesions (aOR: 2.37, 95% CI: 1.27–4.42; p = 0.007) (Table 3).
Discussion
In this cross-sectional comparative study, approximately one-fifth (17%) of the women attending the cervical cancer screening clinic at MRRH had premalignant cervical lesions. The prevalence of premalignant cervical lesions was significantly higher among HIV-positive women than among HIV-negative women. Notably, a history of HIV infection was independently associated with increased odds of having premalignant cervical cancer lesions.
This finding is consistent with findings at Kampala International University Teaching Hospital in Uganda, which reported a similar prevalence of 21.9% [8]. Our findings are similar because the studies were both performed in teaching hospitals and they both used similar methods.
The prevalence of premalignant cervical lesions in the current study was higher in HIV-positive women than in HIV-negative women (23% versus 12%). This finding is consistent with findings at the Debre Markos Referral Hospital in Ethiopia, which found a prevalence of 17.8% in HIV-positive women and 10.3% in HIV-negative women [36]. Similarly, three hospitals in three regions of Swaziland also found a prevalence of 22.9% in HIV-positive women and 5.7% in HIV-negative women [17]. These studies were performed in low-income settings, such as our study, and low-income settings are characterized by gaps in the utilization and availability of healthcare, such as the low uptake of cervical cancer screening services [37]. Additionally, precancerous cervical lesions are aggressive and progress rapidly in immune-compromised patients because HIV-positive women are more likely to be infected with HPV and to have persistent HPV infection leading to precancerous lesions compared with HIV-negative women [19]. However, a study at the maternal and child healthcare hospital in Brazil found a lower prevalence in the HIV-positive group and HIV-negative group (12.1% versus 5.4% respectively) [38], and a study at the University of Nigeria Teaching Hospital (UNTH) in Enugu, Southeastern Nigeria, reported a prevalence of infection (12.6%) versus 4.6% (𝑃<0.014) [33]. This could have been because all the HIV-infected participants were receiving highly active antiretroviral therapy (HAART), which increases the CD4 count and hence reduces HPV persistence, leading to a low risk of premalignant cervical lesions. However, a tertiary hospital in North Central Nigeria found a higher prevalence of 56% in HIV-positive women and 13% in HIV-negative women [39], and another retrospective study in Tanzania showed a higher prevalence of 71.8% in HIV-positive women and 27.3% in HIV-negative women [40]. This could be due to differences in the methods used and the duration of the study.
All categories of premalignant cervical lesions identified in this study occurred more frequently among HIV-positive women, and the most common category was LSIL in both groups. This finding is similar to that reported at Maternal and Child Healthcare Hospital in Brazil, which found 6.4% LSIL in HIV-positive women and 2.7% LSIL in HIV-negative women; only one case of HSIL was found in all smears analyzed, and this patient was HIV positive [38]. Precancerous cervical lesions are considered to be more aggressive and progress rapidly in immune-compromised patients. Compared with HIV-negative women, HIV-positive women are more likely to be infected with HPV and to have persistent HPV, leading to larger and more difficult-to-treat precancerous lesions [17]. In HIV-negative women with competent immune systems, most infections are cleared spontaneously because of a cell-mediated immune response regulated by CD4 + lymphocytes [16].
A history of HIV infection was independently associated with premalignant cervical lesions in this study. HIV-positive women were approximately 2.4 times more likely to have premalignant cervical lesions than HIV-negative women. Compared with HIV-negative women, HIV-positive women have an increased risk of HPV infection and precancerous lesions [19]. This finding is consistent with findings at three hospitals in three regions of Swaziland [17]. Similarly, in a retrospective study from Tanzania on the influence of HIV/AIDS infection on precancerous cervical lesions, HIV infection was shown to increase the risk of premalignant cervical lesions [40]. Suggested explanations include a decrease in T-cell surveillance in HIV infection, which allows HPV replication, allowing for persistence of HPV infection, accumulation of mutations in the infected cells, and subsequent proliferation of dysplastic cells [20]. HIV alters the natural history of HPV infection, with decreased regression rates and more rapid progression to high grade and invasive lesions, which are refractory to treatment, requiring interventions that are more stringent including monitoring [22]. HIV-associated premalignant cervical lesions are thought to progress through the microsatellite instability pathway, whereas HIV-negative lesions progress through loss of heterozygosity. Interactions are likely via viral proteins, with HIV proteins enhancing the effectiveness of HPV proteins and possibly contributing to cell cycle disruption.
Study strengths
This study had several strengths. We used cytology convention method where we captured both endocervical and ectocervical cells; these cells were subjected to quality control by another independent pathologist from another hospital. In addition, participants were screened for their HIV status and also the comparativeness of the design.
Study limitations
We were able to answer our study objectives however; the study dataset had some missing viral load and HAART data. Additionally, we did not test for the presence of HPV or its effect on premalignant cervical lesions.
Conclusions
We found a high prevalence of premalignant cervical lesions in women attending the MRRH cervical cancer screening clinic. Low-grade squamous intraepithelial lesions were the most common premalignant cervical lesions among all the women who participated in this study. The presence of all forms of premalignant cervical cancer lesions in women was positively associated with being HIV-positive. These findings further emphasize the need for the integration of HIV care and cervical cancer prevention programs. We recommend a longitudinal study to determine the outcomes of premalignant cervical lesions among HIV-positive women.
Data availability
For confidentiality reasons, the datasets used are not publicly available. However, the datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request (Dr. Justus Kirabira, Email: kjustus.justus19@gmail.com).
Abbreviations
- AIDS:
-
Acquired Immune-Deficiency Syndrome
- ASC:
-
Atypical Squamous Cell
- ASC-H:
-
Atypical Squamous Cell that cannot exclude High-grade Lesion
- ASC-US:
-
Atypical Squamous Cell of Undetermined Significance
- BMI:
-
Body Mass Index
- CD4:
-
cluster of differentiation 4
- CIN:
-
Cervical Intraepithelial Neoplasia
- DNA:
-
deoxyribonucleic acid
- HAART:
-
highly active antiretroviral therapy
- HIV:
-
Human Immune-Deficiency Virus
- HPV:
-
human papilloma virus
- HSIL:
-
High Grade Squamous Intraepithelial Lesion
- LSIL:
-
Low Grade Squamous Intraepithelial Lesion
- MRNA:
-
messenger ribonucleic acid
- MRRH:
-
Mbarara Regional Referral Hospital
- MUST:
-
Mbarara University of Science and Technology
- Pap Smear:
-
Papanicolaou Smear
- SD:
-
standard deviation
- STIs:
-
Sexually Transmitted Infections
- WHO:
-
World Health Organization
- Cor:
-
Crude Odds Ratio
- aOR:
-
Adjusted Odds Ratio
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394–424.
Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global Cancer in women: Burden and TrendsGlobal Cancer in women: Burden and Trends. Cancer Epidemiol Biomarkers Prev. 2017;26(4):444–57.
Arbyn M, Castellsagué X, de Sanjosé S, Bruni L, Saraiya M, Bray F, et al. Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011;22(12):2675–86.
Parkin D, Ferlay J, Hamdi-Cherif M, Sitas F, Thomas J, Wabinga H, et al. Cancer Afr Epidemiol Prev. 2003;4:268–76.
Anorlu RI. Cervical cancer: the sub-saharan African perspective. Reprod Health Matters. 2008;16(32):41–9.
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Global Health. 2020;8(2):e191–203.
Bruni L, Barrionuevo-Rosas L, Albero G, Aldea M, Serrano B, Valencia S et al. Human papillomavirus and related diseases in the world. Summary Rep. 2015;20140822.
Mulumba R, Lule H, Atuhaire C, Bonet I, Diaz AA. Scholars J Appl Med Sci (SJAMS) ISSN 2320–6691 (Online). 2018.
Arbyn M, Ronco G, Anttila A, Meijer CJ, Poljak M, Ogilvie G, et al. Evidence regarding human papillomavirus testing in secondary prevention of cervical cancer. Vaccine. 2012;30:F88–99.
WHO. Comprehensive cervical cancer control: a guide to essential practice. World Health Organization; 2006.
Nayar R, Wilbur DC. The Bethesda system for reporting cervical cytology: definitions, criteria, and explanatory notes. Springer; 2015.
Köse FM, Naki MM. Cervical premalignant lesions and their management. J Turkish German Gynecol Association. 2014;15(2):109.
Solomon D, Davey D, Kurman R, Moriarty A, O’Connor D, Prey M, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002;287(16):2114–9.
Zhang H-Y, Tiggelaar SM, Sahasrabuddhe VV, Smith JS, Jiang C-Q, Mei R-B, et al. HPV prevalence and cervical intraepithelial neoplasia among HIV-infected women in Yunnan Province, China: a pilot study. Asian Pac J cancer Prevention: APJCP. 2012;13(1):91.
Adjorlolo-Johnson G, Unger ER, Boni-Ouattara E, Touré-Coulibaly K, Maurice C, Vernon SD, et al. Assessing the relationship between HIV infection and cervical cancer in Cote d’Ivoire: a case-control study. BMC Infect Dis. 2010;10(1):1–8.
Nweke I, Nwadike V, Kalu I, Ojide K. Human papilloma virus and cervical neoplasia in HIV positive women: a non systematic review. Afr J Microbiol Res. 2014;8(22):2193–201.
Jolly PE, Mthethwa-Hleta S, Padilla LA, Pettis J, Winston S, Akinyemiju TF, et al. Screening, prevalence, and risk factors for cervical lesions among HIV positive and HIV negative women in Swaziland. BMC Public Health. 2017;17(1):1–8.
Strickler HD, Burk RD, Fazzari M, Anastos K, Minkoff H, Massad LS, et al. Natural history and possible reactivation of human papillomavirus in human immunodeficiency virus–positive women. J Natl Cancer Inst. 2005;97(8):577–86.
Whitham HK, Hawes SE, Chu H, Oakes JM, Lifson AR, Kiviat NB, et al. A comparison of the natural history of HPV infection and cervical abnormalities among HIV-positive and HIV-negative women in Senegal, Africa. Cancer Epidemiol Prev Biomarkers. 2017;26(6):886–94.
Memiah P, Makokha V, Mbuthia W, Kiiru GW, Agbor S, Odhiambo F, et al. Epidemiology of cervical squamous intraepithelial lesions in HIV infected women in Kenya: a cross-sectional study. Afr J Reprod Health. 2015;19(1):133–9.
Peter Memiah WM. 2 grace Kiiru,2 Solomon Agbor,1 Francesca Odhiambo,3 Sylvia Prevalence and Risk factors Associated with Precancerous Cervical Cancer lesions among HIV-Infected women in Resource-Limited Settings 2012.
Clarke B, Chetty R. Postmodern cancer: the role of human immunodeficiency virus in uterine cervical cancer. Mol Pathol. 2002;55(1):19.
Yang L, Morris GF, Lockyer JM, Lu M, Wang Z, Morris CB. Distinct transcriptional pathways of TAR-dependent and TAR-independent human immunodeficiency virus type-1 transactivation by Tat. Virology. 1997;235(1):48–64.
Kelly H, Weiss HA, Benavente Y, de Sanjose S, Mayaud P, Qiao Y-l, et al. Association of antiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: a systematic review and meta-analysis. Lancet HIV. 2018;5(1):e45–58.
Taye BT, Mihret MS, Muche HA. Risk factors of precancerous cervical lesions: the role of women’s socio-demographic, sexual behavior and body mass index in Amhara region referral hospitals; case-control study. PLoS ONE. 2021;16(3):e0249218.
Nkfusai NC, Mubah TM, Yankam BM, Tambe TA, Cumber SN. Prevalence of precancerous cervical lesions in women attending Mezam Polyclinic Bamenda, Cameroon. Pan Afr Med J. 2019;32.
Kassa RT. Risk factors associated with precancerous cervical lesion among women screened at Marie Stops Ethiopia, Adama town, Ethiopia 2017: a case control study. BMC Res Notes. 2018;11(1):1–5.
Ibrahim A, Rasch V, Pukkala E, Aro AR. Cervical cancer risk factors and feasibility of visual inspection with acetic acid screening in Sudan. Int J Women’s Health. 2011;3:117.
MOH. THE 2020 UGANDA POPULATION-BASED HIV IMPACT ASSESSMENT. 2022.
MRRH. Cervical cancer register. [Hospital records]. In press 2020.
MoH. Strategic plan for cervical cancer prevention and control in Uganda 2010–2014. Ministry of Health Kampala; 2010. p. 70.
Wang H, Chow SC. Sample size calculation for comparing proportions. Wiley Encyclopedia Clin Trials. 2007;10:9781118445112.
Dim C, Ezegwui H, Ikeme A, Nwagha U, Onyedum C. Prevalence of cervical squamous intraepithelial lesions among HIV-positive women in Enugu, South-eastern Nigeria. J Obstet Gynaecol. 2011;31(8):759–62.
Alrajjal A, Pansare V, Choudhury MSR, Khan MYA, Shidham VB. Squamous intraepithelial lesions (SIL: LSIL, HSIL, ASCUS, ASC-H, LSIL-H) of Uterine Cervix and Bethesda System. CytoJournal. 2021;18.
MOH. National HIV Testing Services Policy and Implementation Guidelines Uganda. Ministry of Health Kampala, Uganda; 2016.
Getinet M, Gelaw B, Sisay A, Mahmoud EA, Assefa A. Prevalence and predictors of pap smear cervical epithelial cell abnormality among HIV-positive and negative women attending gynecological examination in cervical cancer screening center at Debre Markos referral hospital, East Gojjam, Northwest Ethiopia. BMC Clin Pathol. 2015;15(1):1–10.
Aynalem BY, Anteneh KT, Enyew MM. Utilization of cervical cancer screening and associated factors among women in Debremarkos town, Amhara region, Northwest Ethiopia: Community based cross-sectional study. PLoS ONE. 2020;15(4):e0231307.
De Lemos PAP, García-Zapata MTA, Tavares SBN. Cervical cytopathology in a population of HIV-positive and HIV-negative women. Journal of tropical medicine. 2012;2012.
Lawal I, Agida TE, Offiong RA, Oluwole PO. Cervical cytology among HIV positive and HIV negative women in a tertiary hospital in North Central Nigeria: a comparative study. Annals of Medical and Health Sciences Research; 2017.
Chambuso RS, Shadrack S, Lidenge SJ, Mwakibete N, Medeiros RM. Influence of HIV/AIDS on cervical cancer: a retrospective study from Tanzania. J Global Oncol. 2017;3(1):72–8.
Nakisige C, Schwartz M, Ndira AO. Cervical cancer screening and treatment in Uganda. Gynecologic Oncol Rep. 2017;20:37–40.
Acknowledgements
The authors would like to thank the Director of Mbarara Regional Referral Hospital and the medical team at the cervical cancer screening clinic at Mbarara Regional Referral Hospital for allowing the study to be conducted in their hospital and clinic, respectively.
Funding
This study did not receive any funding from funding agencies in the public, commercial, or nonprofit sectors.
Author information
Authors and Affiliations
Contributions
J.K. took the lead in conceptualizing the study idea, data collection, data analysis, writing, and editing the manuscript. M.K., S.M.B., E.J.N., F.Y., A.N., R.N., H.N., R.A., A.B., H.M.L., L.T., D.K., M.J., D.C.A., P.S., S.M.A., M.T., R.M., and R.K. participated in the conceptualization of the study idea, data collection, data analysis and editing and reviewing of the manuscript. All authors read and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol and documents were approved by the Mbarara University of Science and Technology (MUST) Research and Ethics Committee (ref; 3518) and the MUST Faculty of Medicine Research and Ethics Committee. Administrative clearance was obtained from the Director of Mbarara Regional Referral Hospital. The study was also approved by the Uganda National Council for Science and Technology (HS2258ES). The protocol was implemented in accordance with the Declaration of Helsinki guidelines. Written informed consent was obtained from all study respondents prior to undergoing study procedures, Women who were found to have premalignant cervical lesions were linked to care (further evaluated with colposcopy and managed as per the Uganda Ministry of Health guidelines for the management of premalignant lesions [41] in the cervical cancer screening clinic of Mbarara Regional Referential Hospital). Participants who tested HIV positive were linked to ART care at the ART clinic of Mbarara Regional Reviewer Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kirabira, J., Kayondo, M., Bawakanya, S.M. et al. Association between HIV Serostatus and premalignant cervical lesions among women attending a cervical cancer screening clinic at a tertiary care facility in southwestern Uganda: a comparative cross-sectional study. BMC Women's Health 24, 266 (2024). https://doi.org/10.1186/s12905-024-03108-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-024-03108-w