Abstract
Purpose
This study aimed to investigate the difference in absolute and fat free mass (FFM)-adjusted resting energy expenditure (mREE) and body composition (body weight, fat mass (FM), FFM) between breast cancer survivors (BCs) and controls. Correlations with body composition were analyzed. We examined if survival year, or being metabolically dysfunctional were predictive variables.
Methods
A cross-sectional analysis was conducted on 32 BCs ≤5 years post treatment and 36 healthy controls. Indirect calorimetry measured absolute mREE. Body composition was determined by BOD POD. FFM-adjusted mREE was calculated (mREE/FFM). The Harris-Benedict equation was used to predict REE and determine hyper−/hypometabolism (mREE/pREE). The database of the multidisciplinary breast clinic of the University Hospital of Antwerp was consulted for survival year and metabolic dysfunctions.
Results
BCs have similar absolute mREE and greater FFM-adjusted mREE compared to controls. Absolute mREE and body composition between BCs differed; adjusted mREE was similar. FFM correlated significantly with absolute mREE in BCs. A significant interaction term was found between survival year and FM for absolute mREE.
Conclusion
BCs have similar absolute mREE, but higher FFM-adjusted mREE. Differences in body composition between BCs are suggested to cause inter-individual variations. We suggest that increased FFM-adjusted mREE is caused by metabolic stress related to cancer/treatment. Accurate measurement of REE and body composition is advised when adapting nutritional strategies, especially in patients at risk for developing metabolic dysfunctions.
Similar content being viewed by others
Introduction
Breast cancer is the most prevalent tumor type in women, representing 30% of the annual cancer incidence [1]. Advancements in screening procedures and (neo) adjuvant therapies are credited with improved survival rates [2]. Chemotherapeutic agents are administered in 56% of the patients with breast cancer stage (II)III-IV as standalone treatment, or in combination with other therapies [3]. Despite the therapeutic effects, a variety of adverse side-effects have been recorded after treatment. Amongst changes in body weight (BW) and body composition (fat mass (FM); fat free mass (FFM)), deteriorating metabolic profiles are often present in women with breast cancer, from time of diagnosis throughout the rest of the patient’s life (i.e. breast cancer survivors (BCs)), which elevates the risk for developing the metabolic syndrome [2].
Metabolic dysfunction is the hallmark of the metabolic syndrome with clinical features such as excess accumulation of adipose tissue and obesity, hypertension, dyslipidemia, insulin resistance, and increase in blood glucose [4]. Metabolic disturbances are common in BCs after treatment, with merging evidence directing towards chemotherapy (CT) as potential cause [5]. Often during CT, changes in FM and FFM occur, which are associated with toxicity-induced comorbidities [6]. In terms of FM, the influence of CT on accumulating visceral and ectopic adipose tissue is rapid (within 2–3 months) and persistent (> 1 year) [4]. Chemotherapeutic agents also induce oxidative stress, increasing the risk for developing metabolic dysfunctions [2]. The presence of ≥2 metabolic dysfunctions is related to cancer development and –recurrence [7]. Metabolic alterations and changes in FM and FFM often go hand in hand, ultimately affecting the body’s energy needs [8, 9].
Indirect calorimetry (IC) is widely acknowledged as gold standard for measuring (resting) energy expenditure (m(R)EE; absolute mREE) [9, 10]. In health, BW seems to be the most decisive factor for REE due to the amount of FFM, consisting of organ tissue, bone tissue, and muscle tissue, and is highly metabolically demanding [11]. In disease, deflections in FFM-adjusted mREE (mREE/FFM) seem to represent metabolic stress, with increasing levels proportional to disease severity [8].
In cancer, both an increase (hypermetabolism) and decrease (hypometabolism) in the level of REE can occur, as well as no change at all [12]. The high variability is most likely due to the extensive range of clinical phenomena (cancer type, −stage, treatment, metabolic derangements) that can alter a patients’ metabolic demand. In this regard, repeated measurements of REE in combination with body composition analysis over the course of different illness trajectories have provided more insight in metabolic alterations, as dynamic patterns were unraveled suggested to correspond with illness progression or resolution [13,14,15,16]. The use of IC to measure REE is therefore preferred over pREE to accurately assess the metabolic demand and determine nutritional goals in patient populations [12].
The clinical value of absolute and adjusted mREE in relation to body composition and the presence of metabolic stress related to metabolic dysfunctions in different patient populations has already been acknowledged [14, 16, 17]. In BCs post treatment however, evidence is conflicting as a large heterogeneity exists within the population. Therefore, the purpose of this study was 1) to explore the difference in absolute mREE, FFM-adjusted mREE and body composition parameters: FM, FFM, and BW in BCs compared to healthy controls; 2) to examine the correlations between body composition parameters and absolute mREE in BCs and controls to predict the individual contribution of body composition to absolute mREE; and 3) to investigate if survival time, and being metabolically dysfunctional (≥2 metabolic dysfunctions) are predictive variables for absolute mREE in BCs.
Methods
This cross-sectional study was conducted at the Multidisciplinary Metabolic Research Unit (M2RUN) of Movant Research group; University of Antwerp (Belgium). Approval was given by the medical ethical committee of the University of Antwerp/Antwerp University Hospital (B300201837317).
Participants
The database of the Multidisciplinary Breast Clinic of the University Hospital of Antwerp was consulted to find BCs meeting the eligibility criteria. Simultaneously, a healthy control group was recruited after advertising on social platforms (Facebook, Instagram, Twitter) or by direct contact. Eligible subjects were contacted by telephone and provided with an appointment at the laboratory. All participants signed informed consent at the day of the appointment. All study visits took place between November 25th, 2021 and September 17th, 2022.
Breast cancer survivors
Female BCs between 40-65y were contacted. To represent the whole survivor group, women were included when they were either 1-, 3-, or 5 years post active treatment (survival time). To limit bias, age, BH, and BW were matched between survival years. Patients were controlled for tumor type (infiltrating ductal breast carcinoma, stage III – IV) and active treatment regimen (12 × 1 time/week taxol therapy; 4 × 1/2 weeks AC therapy; surgery; radiotherapy). Only women with a first diagnosis of BC were included. Subjects were excluded when one of the inclusion criteria was not met (Table 1).
Metabolic (dys) function in BCs
BCs were additionally assigned to a metabolically functional (Funct) and dysfunctional (Dysf) group based on information extracted from the medical file. Relevant information was related to the presence of metabolic dysfunctions. Survivors were considered as dysfunctional when ≥2 of the following clinical abnormalities were present for > 6 months: 1) Dyslipidemia (hypercholesterolemia and hypertriglyceridemia) or medication, 2) hypertension or medication, 3) insulin resistance or medication, 4) increased adiposity (FM > 30% of total BW, with BMI > 25.0 kg/m2), or 5) increased blood glucose. The specific criteria for determining metabolic dysfunctions are added supplementary (Table A).
Healthy controls
Women enrolled when they were between 40-65y old and in general good health: Absence of metabolic diseases that could alter REE (hyper−/hypothyroidism, burn wounds, liver diseases), < 2 metabolic dysfunctions (hypertension, hypertriglyceridemia, hypercholesterolemia, insulin resistance, increase in blood glucose), no common cold or flu < 2 weeks ago, no surgery < 1 month ago, no current use of pharmaceuticals (medication of any type), and no (history of) cancer (any type). Participants were excluded if one of the criteria was unmet. Healthy subjects were matched with BCs for age, BH, and BW (Table 1).
Procedures and outcome measures
Setting
Participants were invited for a single appointment (1.5 hr), on which all procedures for data collection were done consecutively. Assessments were executed in the morning (7h00am-11h30am). Subjects were not allowed to eat < 8 hrs before measurement, while drinking water was allowed freely until 2 hr. prior to the appointment. Participants were asked to refrain from heavy exercise 24 hr. before measurements.
Demographic and anthropometric variables
The following demographic and anthropometric data were collected: pREE (HBeq = 447.593 + (9.247 x BW(kg)) + (3.098 x BH(cm)) − (4.330 x age(y))), survival year, current cancer-related endocrine treatment (Table B. appendix), age(y), BW (kg), FM (kg,%) FFM (kg,%) BH (cm), and body mass index (BMI; \(\frac{BW(kg)}{BL(m)2}\)) to evaluate the obesity status (underweight (BMI < 18.5), normal weight (BMI = 18.5–24.9), overweight (BMI = 25.0–29.9), obese (BMI > 30.0)). To assess body composition in relation to body size, fat mass index (FMI; \(\frac{FM(kg)}{BL(m)2}\)) and fat free mass index (FFMI; \(\frac{FFM(kg)}{BL(m)2}\)) were calculated.
Indirect calorimetry
IC measurements were done with an open circuit diluted flow calorimeter (Omnical IV, Maastricht Instruments, The Netherlands). Calibration of the device was performed automatically every 30 min with span gas (18% O2 and 0.8% CO2) and nitrogen gas (100%). Validation of the system by methanol combustion was performed weekly [18]. All measurements were normalized to standard temperature and pressure dry (STPD) values by measuring temperature, humidity, and pressure.
The measurements were executed in a basic version of a respiratory room (14m3). Participants were instructed to lay in a semi-inclined position while staying awake. Minimal activity (reading, desk work, listening to music) was allowed. The room served as reservoir collecting \(\dot{\textrm{V}}\) O2 and \(\dot{\textrm{V}}\) CO2. The measurement lasted 60 min and data were provided every minute. Results of the last 50 min were used. \(\dot{\textrm{V}}\) O2 and \(\dot{\textrm{V}}\) CO2 were converted to REE values (Weir, 1949). Data were collected as kcal/min and recalculated to kcal/24 hrs (absolute mREE) to determine FFM-adjusted mREE adjusted (\(\frac{mREE}{FFM}\)). The metabolic status was defined by the % difference between pREE and mREE (hypermetabolism (mREE/pREE> + 10%), hypometabolism (mREE/pREE<− 10%), normometabolism (mREE/pREE = ±10%)).
Bod pod
FM and FFM were assessed by air-displacement plethysmography (BOD POD, Cosmed, United States) [19]. The device was calibrated prior to each analysis, as prescribed by the manufacturer. A warm-up period of 30 min was followed by a 15 min quality control of hardware, scale, and accuracy and reliability of volume assessment. For the assessment (10 min), participants were asked to remove all accessories and wear snug fitting clothing and swim cap to limit the effects on body surface area. A precise measurement of BW was followed by 2–3 (depending on individual fidgeting) analyses of body volume to determine body density (\(Body\ density=\left(\frac{body\ weight}{body\ volume}\right)\)). The relative contribution of FM to body weight (FM%) was calculated by the SIRI equation: \(FM\%=\left(\frac{495}{body\ density}\right)-450\). Next, the relative contribution of FFM to body weight (FFM%), total amount of FM (kg) and FFM (kg) were derived.
Statistical analysis
Quantitative variables are expressed as mean ± SD. All variables were checked for normality (Kolmogorov-Smirnov, QQ-plot and histogram) and were parametric. Characteristics of the study participants include: age, BH, BW, pREE, obesity status, current hormone therapy, metabolic status, and being metabolically (dys)functional; metabolic parameters include: absolute mREE and FFM-adjusted mREE; parameters related to body composition include: FM, FFM, FMi, FFMi, and BW. The difference in mean of all continuous variables between controls and BCs was tested by independent samples T-test. To investigate if differences were present between Dysf BCs, Funct BCs, and healthy controls, analysis of variance (ANOVA) was conducted with post-hoc Dunnett correction. The correlation between body composition parameters, and metabolic parameters in overall BCs, and healthy controls is expressed by Pearson correlation coefficient (r). Multiple linear hierarchical regression models were fitted to estimate the contribution of the significantly correlated body composition parameters to absolute mREE in overall BCs, and controls. Body composition parameters were entered stepwise in the regression model with the highest significantly correlated parameter first. Variables that intercorrelated were not considered in the model due to multicollinearity. The proportion of variance of the dependent variable that is explained by the independent variable is expressed by the R2 change. In addition, univariate analysis was conducted to fit similar multiple regression on absolute mREE in BCs when accounting for FM and/or FFM for following categorical variables: Survival year, being metabolically (dys)functional. Significant interaction terms with body composition parameters are shown. The contribution of the individual variables is expressed by the partial Eta2 (ηp2). All statistical tests are executed two-sided (Significance: α < 0.05). Statistical analyses were performed with SPSS software (SPSS v29, IBM Business Analytics, New York, USA).
Results
In total, 287 BCs were screened for eligibility (72 women in 1-year survival; 83 in 3-year survival; 132 in 5-year survival). 53 (1y), 47 (3y), and 87 (5y) BCs were contacted for study participation.
The main reasons for refusal were time constraints. Demographic and anthropometric data of all women (n = 68) enrolled are presented in Table 1. The control group consisted of 36 women, while the BCs group included 32 women (10 (1y); 11 (3y); 11 (5y) survival). Matching procedures between BCs and controls are found in Table 1.
Resting energy expenditure and body composition in BCs and healthy controls
No significant differences were found in absolute mREE (BCs: 1452 ± 171 vs. controls: 1422 ± 153; p = 0.452). Absolute mREE between Funct BCs, Dysf BCs, and healthy controls, was significantly different (p = 0.049). Dysf BCs had significantly higher levels of absolute mREE compared to Funct BCs (Dysf: 1506 ± 174 vs. Funct: 1372 ± 116; p = 0.026) (Table 2).
FFM-adjusted mREE differed significantly between BCs and controls, with higher levels in the survivor group (BCs: 33 ± 3; vs. controls: 31 ± 3; p = 0.031). A trend towards significance was noticed when comparing Dysf BCs, Funct BCs and healthy controls (p = 0.081). FFM-adjusted mREE did not differ between Dysf and Funct (p = 0.576) (Table 2).
BW was not significantly different between BCs and healthy controls (BCs: 70.9 ± 14.9 vs. controls: 70.4 ± 13.8; p = 0.889). A significant difference in BW was present between Dysf BCs, Funct BCs and healthy controls (p = 0.008). A significant difference in BW was also seen between Dysf and Funct (Dysf>Funct; p = 0.002) (Table 2).
No significant differences were found for FM (kg,%) and FFM (kg,%) between BCs and controls. The difference in FMi and FFMi was also not significant. Significant differences in body composition became apparent between Dysf BCs, Funct BCs and healthy controls (FMkg: Dysf>controls>Funct; p = 0.040; FFMkg: Dysf>controls>Funct; p = 0.029). A significant difference in FM (kg,%) and FFM (kg) was also present between Dysf and Funct (FMkg: p = 0.002; FM%: p = 0.044; FFMkg: p = 0.013). Also for FMi and FFMi, significant differences are present with higher values in Dysf BCs (FMi: Dysf>controls>Funct; p = 0.041; FFMi: Dysf>controls>Funct); p = 0.013) (Table 2).
Correlation analysis in BCs and healthy controls
In all BCs, a very strong positive correlation was seen between BW and FM (r = 0.943; p < 0.001), and between BW and FFM (r = 0.807; p < 0.001). A strong, positive correlation was found between FM and FFM (r = 0.582; p < 0.001). For the healthy controls, BW and FFM were strong and positively correlated(r = 0.722; p < 0.001), as well as BW and FM (r = 0.720; p < 0.001). A moderate, positive correlation was found between FM and FFM (r = 0.492; p = 0.002) (Table 3).
For all BCs, the strongest positive correlation for absolute mREE was found with FFM (r = 0.715; p < 0.001), followed by BW (r = 0.643; p < 0.001) and FM (r = 0.513; p = 0.003). In the control group, absolute mREE was positively correlated with BW (very strong: r = 0.713; p < 0.001) and FFM (strong; r = 0.624; p < 0.001). A moderate positive correlation was found with FM (r = 0.399; p = 0.016) (Table 3).
Linear regression analysis of absolute mREE with body composition in BCs and healthy controls
A linear regression was calculated to predict absolute mREE based on FFM, FM and BW. For BCs, a significant regression equation was found for absolute mREE (F(3, 20)=10.333; p < 0.001), with R2 = 0.511. For the healthy controls, a significant regression equation was found for mREE (F(3, 32)=13.432; p < 0.001), with R2 = 0.508 (Table 3).
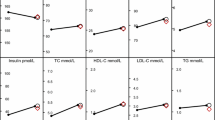
Analysis of predictive variables for absolute mREE in BCs
After controlling for FFM and FM, a significant regression equation was found with survival year (F(6, 25)=8.192; p < 0.001) with R2 = 0.663 (no significant main effect). A significant interaction between survival year and FM was determined (F(2, 25)=3.825; p = 0.036 with ηp2 = 0.234). The regression equation was also significant with being metabolically dysfunctional (F(3, 28)=10.495; p < 0.001) with R2 = 0.529, although no main effect was determined (Table 4).
Discussion
The present study was designed to examine the differences between absolute (mREE) and FFM-adjusted (mREE/FFM) measured energy expenditure and body composition (BW, FFM and FM) in breast cancer survivors (BCs) ≤5y post initial treatment compared to healthy, age-, BH- and BW matched controls without prior cancer diagnosis. The main findings are that BCs have similar absolute mREE, BW, FFM and FM compared to the control group, whereas FFM-adjusted mREE is significantly greater. Our data hereby suggest that BCs ≤5y post initial treatment have similar (absolute mREE) or greater (FFM-adjusted mREE) energy expenditure when compared to healthy controls without prior cancer diagnosis. The results of our study confirm the discrepancy between absolute and adjusted mREE, as previously observed by Madzima et al.(2020) in BCs >5y post treatment [20].
Absolute mREE is influenced by the body’s metabolically active components: FM and FFM [21]. Since a larger body size encompasses more FM and FFM, absolute mREE elevates accordingly [22]. The similarities in absolute weights of BW and body composition found in our study can explain the equal levels of mREE. Secondly, it can also be that breast cancer and -treatment may not lead to significant metabolic burden as compared to other tumors of more metabolically demanding organs as postulated by Nguyen and colleagues (2016) [23].
However, intra-individual differences in the distribution and proportion of organ tissue and -mass, each contributing individually to REE, makes it indispensable to normalize absolute mREE to FFM [24]. When adjusted to FFM, our study found greater mREE in BCs. Additionally, Vanittalie et al. suggested that a better analysis of the individual components can be made with FM and FFM normalized for BH (FMi and FFMi), as it allows comparison between individuals with different heights, taking the proportion of organ tissue into account [25]. When adjusting to FFMi, mREE is significantly greater in BCs compared to healthy controls, irrespective of being metabolically (dys)functional. Our findings suggests that BCs may experience more metabolic stress compared to a healthy control group, potentially due to the long-term metabolic effects of cancer or its therapy.
Significant deterioration of the metabolic profile in BCs is a known long-term complication of treatment [26, 27]. Concordantly, BCs endure treatment associated bodily changes including weight gain that most likely results from a net increase in FM, as pro-wasting mechanisms related to treatment (especially CT) facilitate loss of FFM [27,28,29]. According to Dieli-Conwright et al. (2022), an 8% increase in BW can be expected after treatment for breast cancer, with approximately a 17% increase in FM [2]. Further deterioration of FM can occur as BCs experience menopausal symptoms naturally persisting throughout survivorship, or prolonged by cancer-directed endocrine therapies [30]. Higher FM is related to the development of metabolic dysfunctions which seem to elevate mREE in a stepwise manner according to the number of dysfunctions [20, 31,32,33,34,35,36]. Our results show significantly higher BW and FM in Dysf BCs compared to the Funct BCs. In addition, absolute mREE elevates accordingly. After adjusting to FFM (and FFMi), however, no difference in energy expenditure was present. The precise energetic cost of the individual metabolic dysfunctions leading to altered mREE remains unknown, which can explain for the variability in absolute mREE between Dysf and Funct BCs [35]. From our study, we cannot determine the relationship between FM and metabolic dysfunctions, and an increase in absolute or adjusted mREE. Longitudinal research (progressing into survivorship) on larger sample sizes is necessary to examine the relationship between cancer treatment, deterioration of body composition and the onset of metabolic dysfunctions, and their impact on mREE.
Predictive variables for absolute mREE in BCs
FFM was the single significant predictor of absolute mREE in BCs (explaining 51.1% of its variance), while BW was found to be the sole determinant in the control group (50.8%). For both BCs and controls, FFM significantly predicted FFM-adjusted mREE. We could not determine a main effect of survival year on absolute and adjusted mREE. However interestingly, a significant interaction between survival year and FM was seen for absolute mREE. Hyper−/hypometabolism had a main effect on absolute mREE, explaining ±30% of the variance. Being metabolically dysfunctional did not contribute to absolute mREE. The best prediction of absolute mREE was made with survival year, or hyper−/hypometabolism(both 66.3%).
The significant effect of the interaction between survival year and FM on absolute mREE can partially be explained by the fact that adult women naturally gain weight over time, as a mean weight increase of 1.06 kg – 2.38 kg per 4 year has been found [37]. More, BCs often undergo weight gain in terms of FM as a result of physical fatigue and often co-existing sedentarism experienced in the months or even years after diagnosis and treatment [38]. This makes BCs vulnerable for developing metabolic dysfunctions related FM [39]. Although we hypothesized a significant effect of being metabolically dysfunctional, no contribution to absolute mREE was determined, in contrast to previous research [2]. However, an hyper- or hypometabolism did add significantly to the prediction of absolute mREE when accounted for FFM and FM. Altered metabolism results in higher (hypermetabolism) or lower (hypometabolism) energy expenditure due to metabolic- and hemodynamic aberrations, and related changes in body composition [35]. In the absence of a deranged body composition profile, it can by suggested that hyper−/hypometabolism is caused (sub)clinical metabolic alterations [16].
Limitations
We acknowledge several limitations. Despite our efforts to include a larger sample, we encountered difficulties in willingness of participants (time constraints, distance from home to research lab, psychological reasons). The results of our study should therefore be seen in light of research with similar objectives. Secondly, due to low sample sizes, we were unable to further investigate hormonal fluctuations, menopausal status, or estrogen suppression status. In addition, we did not control for meal consumption and physical activity. Third, since we do not have baseline and follow-up measures of body composition during and after treatment, we can only hypothesize the effects of CT, and concordant metabolic derangements. Finally, we retrospectively searched for the presence of metabolic dysfunctions in the aftermath of CT. Follow-up on metabolic derangements during and after treatment might provide more insights on fluctuations and interindividual variations in mREE. More research on a larger cohort is needed on (the onset of) metabolic dysfunctions and body composition in BCs after treatment and altered energy requirements to understand the mechanisms behind alterations in mREE.
Conclusion
Our study reveals similar (absolute) or higher (FFM-adjusted) mREE in BCs ≤5y post active treatment compared to healthy controls. In absence of differences in body composition, we suggest that elevated mREE is the result of metabolic stress as a consequence of previous cancer diagnosis and/or treatment. Future research should continue to explore accurate FFM and FM (in relation to survival year) in relation to energy expenditure and metabolic health among BCs. Our study highlights the importance of accurate measurement of FFM and FM (in relation to survival year) in BCs. Precise measuring REE by IC is preferred when adapting nutritional strategies, especially in patients at risk for developing the metabolic syndrome since the individual contribution of the metabolic derangements to REE remains unknown and can lead to hyper−/hypometabolism.
Availability of data and materials
The data supporting the findings of this study are available upon reasonable request from the corresponding author. Data are not shared openly to protect privacy of study participants. Data are located in a controlled access data storage at the University of Antwerp.
References
Siegel R, Miller K, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1)
Dieli-Conwright C, Wong L, Waliany S, Mortimer J. Metabolic syndrome and breast cancer survivors: a follow-up analysis after completion of chemotherapy. Diabetol Metab Syndr. 2022;14(36)
American Cancer Society. Cancer treatment & survivorship: Facts & Figures 2019–2021. Atlanta: American Cancer Society; 2019.
Christensen R, Haykowksy M, Nadler M, Prado C, Small S, Rickard J, et al. Rationale and design of IMAPCT-women: a randomized controlled trial of the effect of time-restricted eating, healthy eating, and reduced sedentary behavior on metabolic health during chemotherapy for early-stage breast cancer. Br J Nutr. 2023;14;130(5):852–9.
Dieli-Conwright C, Louise W, Waliany S, Bernstein L, Salehian B, Mortimer J. An observational study to examine changes in metabolic syndrome components in patients with breast cancer receiving neoadjuvant or adjuvant chemotherapy. Cancer. 2016;122(17):2646–53.
van den Berg M, Kok D, Visser M, de Vries J, de Kruif J, de Vries Y, et al. Changes in body composition during and after adjuvant or neo-adjuvant chemotherapy in women with breast cancer stage I-IIIB compared with changes over a similar timeframe in women without cancer. Support Care Cancer. 2020;28(4)
Karra P, Winn M, Pauleck S, Bulsiewicz-Jacobsen A, Peterson L, Coletta A, et al. Metabolic dysfunction and obesity-related cancer: beyond obesity and metabolic syndrome. Obesity. 2022:30.
Delsoglio M, Achamrah N, Berger M, Pichard C. Indirect calorimetry in clinical pratice. J Clin Med. 2019;8(9):1387.
Van Soom T, El Bakkali S, Gebruers N, Verbelen H, Tjalma W, van Breda E. The effects of chemotherapy on energy metabolic aspects in cancer patients: a systematic review. Clin Nutr. 2020;39(6)
Weir J. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949:109(1–2).
McMurray R, Soares J, Caspersen C, McCurdy T. Examining variations of resting metabolic rate of adults: a public health perspective. Med Sci Sports Exerc. 2014;46(7)
Barcellos P, Borges N, Torres D. Resting energy expenditure in cancer patients: agreement between predictive equations and indirect calorimetry. Clin Nutr ESPEN. 2021:42.
Holmes C, Racette S. The utility of body composition assessment in nutrition and clinical practice: an overview of current methodology. Nutrients. 2021;13:8.
Kovarik M, Najpaverova S, Koblizek V, Zadak Z, Hronek M. Association of resting energy expenditure and nutritional substrate oxidation with COPD stage and prediction indexes. Respir Med. 2020;174
Milner E, Cioffi W, Mason A, McManus W, Pruitt B. A longitudinal study of resting energy expenditure in thermally injured patients. J Trauma. 1994;37(2)
Rattanachaiwong S, Singer P. Indirect calorimetry as point of care testing. Clin Nutr. 2019:38.
Belarmino G, Singer P, Gonzalez M, Machado N, Cardinelli C, Barcelos S, et al. Prognostic value of energy expenditure and respiratory quotient measuring in patients with liver cirrhosis. Clin Nutr. 2019;38
Schoffelen P, den Hoed M, van Breda E, Plasqui G. Test-retest variability of VO2max using total-capture indirect calorimetry reveals linear relationship of VO2 and power. Scand J Med Sci Sports. 2019;29(2):213–22.
Ducharme J, Hsiao Y, Gibson A, Mermier C. Predictive model specific to young adults for estimating thoracic gas volume for air-displacement plethysmography. Clin Physiol Funct Imaging. 2022;42(2)
Madzima T, Deaterly C. Body composition, metabolism, and inflammation in breast cancer survivors and healthy age-matched controls: a cross-sectional analysis. Intl J Exerc Sci. 2020;13(3)
Carneiro I, Elliott S, Siervo M, Padwal R, Bertoli S, Battezzati A, et al. Is obesity associated with altered energy expenditure? Adv Nutr. 2016;7(3)
Westerterp K. Control of energy expenditure in humans. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, editors. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2000–. PMID: 25905198.
Nguyen T, Batterham M, Edwards C. Comparison of resting energy expenditure between cancer subjects and healthy controls: a meta-analysis. Nutr Cancer. 2016;68(3):374–87.
Bosy-Westphal A, Braun W, Schautz B, Müller M. Issues in characterizing resting energy expenditure in obesity and after weight loss. Front Physiol. 2013:4.
Vanitallie T, Yang M, Heymsfield S, Funck R, Boileau R. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am j clin nutrit. 1990;52(6):953–9.
Guinan E, Connolly E, Healy L, Carroll P, Kennedy M, Hussey J. The development of the metabolic syndrome and insuline resistance after adjuvant treatment for breast cancer. Cancer Nurs. 2014;37(5)
Guinan E, Connolly E, Kennedy M, Hussey J. The presentation of metabolic dysfunction and the relationship with energy output in breast cancer survivors: a cross-sectional study. Nutr J. 2013;12(9)
Demark-Wahnefried W, Peterson BL, Winer EP, Marks L, Aziz N, Marcom PK, et al. Changes in weight, body composition, and factors influencing energy balance among premenopausal breast cancer patients receiving adjuvant chemotherapy. J Clin Oncol. 2001;19:2381–9.
Pin F, Couch M, Bonetto A. Preservation of muscle mass as a strategy to reduce the toxic effects of cancer chemotherapy on body composition. Curr Opin Support Palliat Care. 2018;12(4)
Ganz P. Breast cancer, menopause and long-term survivorship: Critial issues for the 21st century. Am J Med. 2005;118(12B)
Lipscombe L, Chan W, Yun L, Austin P, Anderson G, Rochon P. Incidence of diabetes among postmenopausal breast cancer survivors. Diabetologia. 2013;56
Mentoor I, Engelbrecht AM, Nell T. Fatty acids: adiposity and breast cancer chemotherapy, a bad synergy? Prostaglandins Leukot Essent Fat Acids. 2019;140
Prieto-Hontoria P, Pérez-Matute P, Fernandez-Galilea M, Bustos M, Martinez J, Moreno-Aliaga M. Role of obesity-associated dysfunctional adipose tissue in cancer: a molecular nutrition approach. Biochim Biophys Acta Bioenerg. 2011;1807(6)
Ebadi M, Mazurak V. Evidence and mechanisms of fat depletion in cancer. Nutrients. 2014;6(11)
Soares M, Zhao Y, Calton E, Pathak K, Ping-Delfos W, Cummings N, et al. The impact of the metabolic syndrome and its components on resting energy expenditure. Metabolites. 2022;12(8)
Healy L, Ryan A, Carroll P, Ennis D, Crowley V, Boyle T, et al. Metabolic syndrome, central obesity and insulin resistance are associated with adverse pathological features in postmenopausa breast cancer. Clin Oncol. 2010;22
Lisevick A, Cartmel B, Harrigan M, Li F, Sanft T, Fogarasi M, et al. Effects of the lifestyle, exercise, and nutrition (LEAN) study on long-term weight loss maintenance in women with breast cancer. Nutrients. 2021;13(9)
Inglis J, Kleckner A, Lin PJ, Gilmore N, Culakova E, VanderWoude A, et al. Excess body weight and cancer-related fatigue, systemic inflammation and serum lipids in breast cancer survivors. Nutrit cancer. 2021;73(9)
Tylutka A, Morawin B, Walas L, Michalek M, Gwara A, Zembron-Lacny A. Assessment of metabolic syndrome predictors in relation to inflammation and visceral fat tissue in older adults. Sci Rep. 2023;13(89)
Acknowledgements
Not applicable.
Funding
No financial or material support was received for the preparation and submission of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was done by Eric van Breda and Timia Van Soom. Data collection and analysis were performed by Timia Van Soom. The first draft of the manuscript was written by Timia Van Soom and all authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript and have no competing interests
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study is approved by the medical ethical committee of the University of Antwerp/Antwerp University Hospital (Belgian registration: B300201942189). Written informed consent was provided on date of appointment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table A.
Criteria for defining metabolic dysfunctions. Table B. Estrogen suppression therapy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Van Soom, T., Tjalma, W., Van Daele, U. et al. Resting energy expenditure, body composition, and metabolic alterations in breast cancer survivors vs. healthy controls: a cross-sectional study. BMC Women's Health 24, 117 (2024). https://doi.org/10.1186/s12905-024-02900-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-024-02900-y