Abstract
Background
Almost all patients with ovarian cancer will experience relapse and eventually develop platinum-resistant. The poor prognosis and limited treatment options have prompted the search for novel approaches in managing platinum-resistant ovarian cancer (PROC). Therefore, a meta-analysis was conducted to evaluate the efficacy and safety of combination therapy with vascular endothelial growth factor (VEGF) /VEGF receptor (VEGFR) inhibitors for PROC.
Methods
A comprehensive search of online databases was conducted to identify randomized clinical trials published until December 31, 2022. Pooled hazard ratios (HR) was calculated for overall survival (OS) and progression-free survival (PFS), while pooled odds ratio (OR) was calculated for objective response rate (ORR) and treatment-related adverse events (TRAEs). Subgroup analysis was further performed to investigate the source of heterogeneity.
Results
In total, 1097 patients from eight randomized clinical trials were included in this meta-analysis. The pooled HRs of OS (HR = 0.72; 95% CI: 0.62–0.84, p < 0.0001) and PFS (HR = 0.52; 95% CI: 0.45–0.59, p < 0.0001) demonstrated a significant prolongation in the combination group compared to chemotherapy alone for PROC. In addition, combination therapy demonstrated a superior ORR compared to monotherapy (OR = 2.34; 95%CI: 1.27–4.32, p < 0.0001). Subgroup analysis indicated that the combination treatment of VEGF/VEGFR inhibitors and chemotherapy was significantly more effective than monochemotherapy in terms of OS (HR = 0.71; 95% CI: 0.61–0.84, p < 0.0001), PFS (HR = 0.49; 95% CI: 0.42–0.57, p < 0.0001), and ORR (OR = 2.97; 95% CI: 1.89–4.67, p < 0.0001). Although the combination therapy was associated with higher incidences of hypertension, mucositis, proteinuria, diarrhea, and hand-foot syndrome compared to monochemotherapy, these toxicities were manageable and well-tolerated.
Conclusions
The meta-analysis demonstrated that combination therapy with VEGF/VEGFR inhibitors yielded better clinical outcomes for patients with PROC compared to monochemotherapy, especially when combined with chemotherapy. This analysis provides more treatment options for patients with PROC.
Systematic review registration
[https://www.crd.york.ac.uk/PROSPERO], Prospective Register of Systematic Reviews (PROSPERO), identifier: CRD42023402050.
Similar content being viewed by others
Introduction
Ovarian cancer (OC) is the seventh most common cancer in women and the eighth leading cause of cancer-related death worldwide [1]. At the time of initial diagnosis, over 70% of patients present with advanced disease due to the presence of atypical early symptoms [2]. Currently, for patients with a new diagnosis, the standard first-liner treatment involves cytoreductive surgery combined with platinum-based systematic chemotherapy, with or without the addition of bevacizumab. However, at first relapse, approximately 25% of patients develop platinum-resistant ovarian cancer (PROC), and nearly all patients will experience relapse and eventually develop platinum-resistant [3]. PROC is associated with a poor prognosis and an overall survival (OS) of less than 12 months, presenting a significant therapeutic challenge [4]. In the platinum-resistant setting, monotherapy with docetaxel, paclitaxel, topotecan or pegylated liposomal doxorubicin (PLD) remains the primary therapeutic option, but it results in a remarkably short survival, highlighting the urgent need for better treatment options. Furthermore, several trials have demonstrated that combining chemotherapy agents leads to increased adverse events without improving clinical benefit for PROC [5,6,7].
Tumor angiogenesis has been established as a hallmark of tumor development, growth, and metastasis. This complex process involves multiple signaling pathways. Vascular endothelial growth factor (VEGF), an important driver of angiogenesis in solid tumors, binds to VEGF receptor-1 or -2 (VEGFR-1/VEGFR-2) on target cells [8], thereby activating intracellular tyrosine kinase signaling. VEGF promotes the recruitment of circulating endothelial progenitor cells from the bone marrow and facilitates endothelial cell survival, differentiation, and proliferation during angiogenesis. Angiogenesis also plays a crucial role in the pathogenesis of OC by promoting tumor proliferation and metastasis [9, 10]. The presence of extensive neovascularization is closely associated with a poor prognosis in OC. Anti-VEGF therapy has emerged as a promising therapeutic target with potential clinical benefits for patients with OC, including those with platinum-resistant disease [11,12,13,14]. Recently, various anti-VEGF therapies, such as anti-VEGF monoclonal antibodies (e.g., bevacizumab) and VEGF-R tyrosine kinase inhibitors (e.g., sorafenib, pazopanib, apatinib, cediranib, anlotinib), have been evaluated in OC patients [15].
The AURELIA trial, a randomized phase III trial, demonstrated a significant improvement in progression-free survival (PFS) in PROC patients when treated with a combination of bevacizumab and chemotherapy compared to monochemotherapy (hazard ratio (HR) = 0.48; 95% CI: 0.38–0.60). The median PFS was 6.7 months with the combined regimen versus 3.4 months with monochemotherapy. The objective response rate (ORR) also increased by 15.5% compared to chemotherapy alone. However, there was no statistically significant improvement in OS when bevacizumab was combined with chemotherapy (HR = 0.85; 95% CI: 0.66–1.08, p < 0.17) [16]. Bevacizumab has been approved by the Food and Drug Administration (FDA) for PROC. Other anti-VEGF agents, such as apatinib, have also shown preliminary evidence of efficacy when combined with chemotherapy for PROC. Wang et al. reported that treatment with apatinib plus PLD resulted in a clinically meaningful improvement in PFS (HR = 0.44; 95% CI: 0.28–0.71, p < 0.001). The median PFS was 5.8 months for apatinib plus PLD versus 3.3 months for PLD alone. The median OS was 23.0 months versus 14.4 months for apatinib plus PLD and PLD alone, respectively (HR = 0.66; 95% CI: 0.40–1.09) [17].
Previous meta-analyses have demonstrated that combination therapy offers improved survival benefits compared to chemotherapy alone in ovarian cancer patients [18,19,20,21]. However, there is a lack of specific meta-analysis focusing on platinum-resistant patients. Given the clinical uncertainty and inconsistent efficacy related to VEGF/VEGFR inhibitors in PROC, a systematic review and meta-analysis was conducted to overcome the limitations of individual studies and provide a more accurate estimation of the efficacy and safety of VEGF/VEGFR inhibitors in PROC.
Materials and methods
This systematic review and meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The study was registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD42023402050).
Data source and search strategy
Eligible studies were identified by searching databases including Cochrane Library, PubMed, Embase, and Web of Science. The search covered the period from inception to December 2022. The main search terms associated with therapy included (anti-angiogenic OR targeted therapy OR molecular targeted therapy OR bevacizumab OR nintedanib OR pazopanib OR cediranib OR sorafenib OR apatinib OR anlotinib OR lenvatinib OR ramolumab OR VEGF OR VEGFR OR vascular endothelial growth factor). The terms related to the disease included ovarian cancer OR ovarian neoplasm. Subsequently, the reference lists of all relevant articles were also browsed.
Study selection
The following criteria were used to screen potential trials: (1) prospective phase II and phase III randomized controlled trials (RCTs); (2) patients with OC, peritoneal cancer (PC), or fallopian tube cancers (FTC) that had progressed during platinum therapy (platinum-refractory) or within 6 months of platinum-containing therapy (platinum-resistant); (3) comparison with therapy combining VEGF/VEGFR inhibitors with other drugs (chemotherapy or Poly (ADP-ribose) polymerase (PARP) inhibitors) and chemotherapy alone; (4) the study’s clinical outcomes included at least one of OS, PFS, ORR, and treatment-related adverse events (TRAEs); (5) Only studies published in English were included. The following criteria were excluded: reviews, fundamental studies, editorials, animal studies, comments, and case reports.
Data extraction and quality assessment
For each eligible study, we extracted the following information: (1) general study information (study name, publication year, first author, study design, trial phase, sample size); (2) basic patient information (region, age, Eastern Cooperative Oncology Group (ECOG) performance status, primary tumor site); (3) control and intervention group. The main outcomes assessed were OS, PFS, ORR, and TRAEs. The risk of bias and methodological quality assessment was performed using the Cochrane Collaboration’s tool in RevMan5.4.
Statistical analysis
Statistical analysis was conducted using Stata 14.0 and RevMan5.4. Pooled odds ratios (ORs) and 95% confidence interval CI were calculated for ORR and TRAEs, while pooled HRs and 95% (CI) were calculated for OS and PFS. With I2 > 50% and p < 0.05 indicating statistically significant heterogeneity [22], a random-effects model was utilized to calculate the HR and OR; otherwise, the fixed-effects model was employed.
Publication bias assessment, sensitivity analysis, and subgroup analysis were conducted to further explore the source of heterogeneity. Begg’s test was performed to evaluate publication bias, and the results indicated the absence of publication bias with p > 0.05 [23]. The symmetry of the funnel plot was also visually observed to assess publication bias. Additionally, a sensitivity analysis was carried out by excluding each study to observe any changes in the pooled HR and OR. Subgroup analysis took into account factors such as region, combination therapeutic agents, trial phase, ECOG performance status, publication year, and primary tumor site.
Results
Study selection and characteristics
A total of 2408 potentially relevant trials were collected through independent evaluation by two authors. After removing irrelevant and duplicate studies, the initial search yielded 1422 abstracts and articles. Finally, eight studies were included (Fig. 1) [16, 17, 24,25,26,27,28,29].
Table 1 recorded the general information of the studies, therapeutic regimens, and baseline characteristics of the patients. Seven studies were prospective phase II RCTs, and one was a prospective phase III RCT. The studies were published between 2014 and 2022, and a total of 1097 patients were available for the meta-analysis, with a mean age of approximately 61 years.
Risk of bias
Seven studies were deemed to have a high risk of bias in blinding participants and personnel, while five studies had an unclear risk of bias in blinding outcome assessment, and one study had a high risk. The remaining studies were rated as having a low risk of bias (Figure S1).
Meta-analysis of OS and PFS
The pooled effects of HR for OS and PFS were available for all eight trials. The results demonstrated that combination therapy with VEGF/VEGFR inhibitors had a significantly better OS than chemotherapy (HR = 0.72; 95% CI: 0.62–0.84, p < 0.0001) (Fig. 2A). Compared to chemotherapy, combination therapy with VEGF/VEGFR inhibitors resulted in a significant improvement in PFS (HR = 0.52; 95% CI: 0.45–0.59, p < 0.0001) (Fig. 2B). Additionally, there were no significant heterogeneities observed in OS and PFS results among the included studies (I2 = 0% and 22.2%, respectively).
Meta-analysis of ORR
All eight trials with PROC reported ORR. Interestingly, the group of combination therapy exhibited respectable ORRs compared to chemotherapy (OR = 2.34; 95%CI: 1.27–4.32, p < 0.0001). There was a high degree of heterogeneity among different studies for ORR (I2 = 69.3%, p = 0.002). Subgroup analyses were conducted to determine the source of heterogeneity. A pooled analysis of ORR in patients with PROC was presented in Fig. 3.
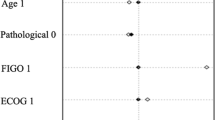
Subgroup analysis for OS
Subgroup analyses were conducted based on stratification factors including region, combination therapeutic agents, trial phase, ECOG performance status, publication year, and primary tumor site. The results were displayed in Table 2 and Figure S2. In the subgroup of combination therapeutic agents, a better OS benefit was revealed in combination treatment with chemotherapy (HR = 0.71; 95% CI: 0.61–0.84, p < 0.0001). Patients with an ECOG performance status of 0 to 2 showed greater OS benefit in the combination treatment group compared to monochemotherapy (HR = 0.72; 95% CI: 0.61–0.85, p < 0.0001). Furthermore, no significant heterogeneity was observed in any of the subgroups.
Subgroup analysis for PFS
The subgroups of region, trial phase, ECOG performance status, publication year, and primary tumor site suggested that combination therapy exhibited better PFS than those receiving chemotherapy alone (Table 3 and Figure S3). Compared to the chemotherapy group, only the subgroup of combination treatment with PARP inhibitors exhibited no significant difference (HR = 0.76, 95% CI: 0.50–1.15, p = 0.192). The heterogeneity within each subgroup was no significant (p > 0.05).
Subgroup analysis for ORR
The results were presented in Table 4 and Figure S4. In the subgroup analysis of combination therapeutic agents, the combination therapy with chemotherapy showed a greater benefit in terms of ORR (OR = 2.97; 95% CI: 1.89–4.67, p < 0.0001). In the subgroup analysis of ECOG performance status, significant benefit of ORR was observed in patients with ECOG scores of 0 to 2 (OR = 3.14; 95% CI: 1.87–5.27, p < 0.0001). The heterogeneities of the two subgroups were reduced.
Meta-analysis of TRAEs
Six trials reported the incidences of any grade TRAEs and four trials reported grade 3–4 TRAEs. For both any grade TRAEs (OR = 2.06; 95% CI: 1.47–2.89, p < 0.0001) and grade 3–4 TRAEs (OR = 2.53; 95% CI: 1.64–3.90, p < 0.0001), the combination therapy with VEGF/VEGFR inhibitors was associated with significantly higher incidences compared to chemotherapy (Fig. 4).
The meta-analysis indicated that compared to chemotherapy, combination therapy had a higher incidence of any grade hypertension (OR = 4.38, 95%CI 1.28–14.93, p = 0.018), mucositis (OR = 3.20, 95%CI 1.25–8.16, p = 0.015), proteinuria (OR = 6.15, 95%CI 1.75–21.59, p = 0.005), diarrhea (OR = 3.14, 95%CI 1.36–7.25, p = 0.007), and hand-foot syndrome (OR = 6.52, 95%CI 1.02–41.70, p = 0.048). There was no statistical difference in the incidence of fatigue (OR = 1.64, 95%CI 0.87–3.10, p = 0.124), nausea (OR = 1.36, 95%CI 0.72–2.54, p = 0.341), and vomiting (OR = 1.74, 95%CI 0.76–4.02, p = 0.192) (Table 5 and Figure S5).
Sensitivity analysis and publication bias
Microvariation was observed in the sensitivity analysis when each trial was removed in turn (Figure S6). There was no publication biases according to Begg’s test (OS, p = 0.107; PFS, p = 0.998; ORR, p = 0.617), and the funnel plots were mostly symmetric (Figure S7).
Discussion
OC is often asymptomatic until it reaches an advanced stage, resulting in delayed diagnosis and poor prognosis. The current screening programs for OC diagnosis are inadequate [31]. PROC remains a significant challenge for clinical diagnosis and treatment due to the extreme cellular heterogeneity and the expression of various resistance and immune evasion mechanisms in this advanced stage of tumor complexity [25]. Combination therapy with VEGF/VEGFR inhibitors has shown a higher likelihood of being the most effective treatment compared to chemotherapy. Recent studies have reported encouraging results, particularly in terms of PFS, for several combination strategies involving VEGF/VEGFR inhibitors in PROC. However, the OS outcomes have been uncertain and inconsistent [16, 17]. To address this, a meta-analysis was conducted, which included eight randomized controlled trials in PROC, and demonstrated better OS, PFS, and ORR outcomes with VEGF/VEGFR inhibitors compared to monochemotherapy. Furthermore, heterogeneity was observed in terms of ORR among the included studies.
Subgroup analyses were performed for OS, PFS, and ORR, considering various stratification factors such as region, combination therapeutic agents, trial phase, ECOG performance status, publication year, and primary tumor site. Regardless of OS, PFS, or ORR, combination therapy with chemotherapy showed greater benefits in the subgroup analysis of combination therapeutic agents. Only one trial included combined PARP inhibitors therapy (cediranib plus olaparib), but it failed to demonstrate any superiority in efficacy compared to the standard treatment for patients with PROC [25]. Some studies have reported that cediranib induces the down-regulation of certain genes in the homologous recombination system, which synergistically enhances the effect of olaparib [32, 33]. Liu et al. demonstrated that the combination of cediranib and olaparib significantly prolonged PFS compared to olaparib alone in platinum-sensitive OC patients (HR = 0.50). Additionally, in the gBRCA/unknown-subset, the combination therapy showed significantly improved OS compared to olaparib alone (37.8 versus 23.0 months, p = 0.047) [34]. However, disappointing results were observed for both OS and PFS in the platinum resistance trials included in our analysis [25]. It should be noted that due to the limited number of trials, the accuracy of subgroup analysis may be insufficient. It is necessary to explore randomized controlled trials of new combinations of PARP inhibitors with various drugs, such as anti-angiogenesis agents, immune checkpoint inhibitors, or other inhibitors of DNA damage response pathways [35].
The analysis of TRAEs revealed that the combination therapy had significantly higher incidences of both any grade TRAEs and grade 3–4 TRAEs compared to monochemotherapy. These findings were consistent with the previously published safety profile of VEGF/VEGFR inhibitors in OC and other solid tumors [36,37,38,39,40,41], and no new safety concerns were identified. Most of the TRAEs reported were of grade 1–2, indicating that the adverse events were manageable. Only four trials reported the incidence of grade 3–4 TRAEs. Among them, paclitaxel plus pazopanib treatment had a higher incidence (OR = 3.33, 95% CI: 1.27–8.76), while bevacizumab plus chemotherapy had a lower incidence (OR = 1.68, 95% CI: 0.76–3.69). Combination therapy was associated with a higher incidence of any grade hypertension, mucositis, proteinuria, diarrhea, and hand-foot syndrome. Hypertension is a common adverse effect of VEGF inhibitors, with an incidence of approximately 30% in various clinical trials, and moderate hypertension occurring in 3–16% of cases. Mucositis is another common adverse effect of anti-VEGF therapy, characterized by symptoms such as pain, difficulty swallowing and pronunciation. Mucositis typically manifests 7–10 days after the initiation of treatment, and in the absence of concurrent bacterial, viral, or fungal infections, it is self-limiting and resolves spontaneously within 2–4 weeks. The mechanism underlying proteinuria production involves the regulation of glomerular vascular permeability by the VEGF signaling pathway. Inhibition of VEGF can result in the destruction of glomerular endothelial cells and epithelial cells (podocytes), leading to proteinuria. The use of VEGF-R tyrosine kinase inhibitors can induce hand-foot syndrome, characterized by red spots, swelling, and pain on the extremities, particularly the palms or soles of the feet. This syndrome typically emerges within the first 6 weeks of treatment.
A meta-analysis has demonstrated that combination therapy with VEGF/VEGFR inhibitors yields superior survival benefits compared to chemotherapy for patients with PROC [42]. However, the trials included in the analysis encompassed recurrent OC rather than exclusively focusing on platinum-resistant disease, and they encompassed a subset of patients with platinum-sensitive disease as well. Moreover, the most recent clinical trials were not incorporated. Therefore, our study serves as a supplement to previous meta-analyses, offering more comprehensive content and considering more stratification factors. It also addresses the limitations of previous meta-analyses and provides additional treatment options for patients with PROC. Several limitations were encountered in this meta-analysis. Firstly, the RCTs employed various therapeutic agents and had different baseline characteristics, resulting in a high degree of heterogeneity in the data analysis for ORR. In an attempt to stratify based on baseline characteristics to mitigate heterogeneity, subgroup analyses were conducted. In the future, network meta-analysis can be employed to further investigate the efficacy and safety of combination therapy. Secondly, this study only included eight RCTs comparing VEGF/VEGFR inhibitors in combination therapy with chemotherapy in patients with PROC, and the majority of these trials were phase II trials. Further more reliable data would be provided from phase III clinical trials for analysis, especially when combined with VEGF/VEGFR inhibitors and PARP inhibitors, which are expected to be included in future studies. Additionally, it is important to note that this meta-analysis lacks sufficient subgroup analyses, and the inclusion of more stratification factors would be crucial in demonstrating the efficacy of VEGF/VEGFR inhibitors for PROC.
Conclusions
The combination therapy of VEGF/VEGFR inhibitors for PROC has shown superior OS, PFS, and ORR compared to monochemotherapy, particularly when combined with VEGF/VEGFR inhibitors and chemotherapy. However, it is worth mentioning that combination therapy is associated with a higher incidence of certain adverse events, such as hypertension, mucositis, proteinuria, diarrhea, and hand-foot syndrome. Nevertheless, the safety profile of combination therapy remains manageable. The present study provides more treatment options for PROC patients.
Data availability
The original datasets for this study are included in the article/Supplementary Material.
Abbreviations
- OC:
-
ovarian cancer
- PROC:
-
platinum-resistant ovarian cancer
- PARP:
-
poly (ADP-ribose) polymerase
- PLD:
-
pegylated liposomal doxorubicin
- HR:
-
hazard ratio
- CI:
-
confidence intervals
- OS:
-
overall survival
- PFS:
-
progression-free survival
- OR:
-
odds ratio
- ORR:
-
objective response rate
- TRAEs:
-
treatment-related adverse events
- VEGF:
-
vascular endothelial growth factor
- ECOG:
-
Eastern Cooperative Oncology Group
- ASCO:
-
American Society of Clinical Oncology
- ESMO:
-
European society of medical oncology
- SGO:
-
Society of Gynecologic Oncology
- RCT:
-
randomized controlled trial
- RECIST 1.1:
-
Response Evaluation Criteria in Solid Tumors version 1.1
- GCIG CA125:
-
Gynecological Cancer Intergroup cancer antigen 125
References
Webb PM, Jordan SJ. Epidemiology of epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017;41:3–14.
Wang Z, Huang Y, Long L, Zhou L, Huang Y, Gan L, et al. Apatinib treatment efficiently delays biochemical-only recurrent ovarian cancer progression. J Ovarian Res. 2021;14(1):91.
Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014;384(9951):1376–88.
Ledermann JA, Raja FA, Fotopoulou C, Gonzalez-Martin A, Colombo N, Sessa C, et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl 4):iv259.
Buda A, Floriani I, Rossi R, Randomised controlled trial comparing single agent paclitaxel vs epidoxorubicin plus paclitaxel in patients with advanced ovarian cancer in early progression after platinum-based chemotherapy: An Italian collaborative study from the Mario Negri Institute, Milan GO et al. N.O. (Gruppo Oncologico Nord Ovest) group and I.O.R (Istituto Oncologico Romagnolo) group. Br J Cancer. 2004; 90(11):2112-7.
Sehouli J, Stengel D, Oskay-Oezcelik G, et al. Non platinum topotecan combinations versus topotecan alone for recurrent ovarian cancer: results of a phase III study of the North-Eastern German Society of Gynecological Oncology Ovarian Cancer Study Group. J Clin Oncol. 2008;26(19):3176–82.
Lortholary A, Largillier R, Weber B, et al. Weekly paclitaxel as a single agent or in combination with carboplatin or weekly topotecan in patients with resistant ovarian cancer: the CARTAXHY randomized phase II trial from grouped’ investigateurs nationaux pour l’ etude des cancers Ovariens (GINECO). Ann Oncol. 2012;23(2):346–52.
Ferrara N, Kerbel RS. Angiogenesis as a therapeutic target. Nature. 2005;438(7070):967–74.
Brown MR, Blanchette JO, Kohn EC. Angiogenesis in ovarian cancer. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14(6):901–18.
Ramakrishnan S, Subramanian IV, Yokoyama Y, et al. Angiogenesis in normal and neoplastic ovaries. Angiogenesis. 2005;8(2):169–82.
Aghajanian C, Blank SV, Goff BA, et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal or fallopian tube cancer. J Clin Oncol. 2012;30(17):2039–45.
Monk BJ, Poveda A, Vergote I, et al. Anti-angiopoietin therapy with trebananib for recurrent ovarian cancer (TRINOVA-1): a randomised, multicentre, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2014;15(8):799–808.
Lan CY, Wang Y, Xiong Y, Li JD, Shen JX, Li YF, et al. Apatinib combined with oral etoposide in patients with platinum-resistant or platinum-refractory ovarian cancer (AEROC): a phase 2, single-arm, prospective study. Lancet Oncol. 2018;19(9):1239–46.
Chase DM, Chaplin DJ, Monk BJ. The development and use of vascular targeted therapy in ovarian cancer. Gynecol Oncol. 2017;145(2):393–406.
Monk BJ, Minion LE, Coleman RL. Anti-angiogenic agents in ovarian cancer: past, present, and future. Ann Oncol. 2016;27(Suppl 1):i33–9.
Pujade-Lauraine E, Hilpert F, Weber B, Reuss A, Poveda A, Kristensen G, et al. Bevacizumab combined with chemotherapy for platinum-resistant recurrent ovarian cancer: the AURELIA open-label randomized phase III trial. J Clin Oncol. 2014;32(13):1302–8.
Wang T, Tang J, Yang H, Yin R, Zhang J, Zhou Q, et al. Effect of Apatinib Plus Pegylated liposomal doxorubicin vs pegylated liposomal doxorubicin alone on platinum-resistant recurrent ovarian Cancer: the APPROVE Randomized Clinical Trial. JAMA Oncol. 2022;8(8):1169–76.
Jiang Y, Sun X, Kong B, Jiang J. Antiangiogenesis therapy in ovarian cancer patients: an updated meta-analysis for 15 randomized controlled trials. Med (Baltim). 2018;97(34):e11920.
Wang Y, Zhang S, Song Z, Ouyang L, Li Y. Anti-angiogenesis maintenance therapy in newly diagnosed and relapsed ovarian Cancer: a Meta-analysis of phase III randomized controlled trials. Front Pharmacol. 2021;12:726278.
Zhang C, Zhao W. The efficacy and safety of angiogenesis inhibitors for recurrent ovarian cancer: a metaanalysis. J Ovarian Res. 2022;15(1):99.
Yi S, Zeng L, Kuang Y, Cao Z, Zheng C, Zhang Y, et al. Antiangiogenic drugs used with chemotherapy for patients with recurrent ovarian cancer: a meta-analysis. Onco Targets Ther. 2017;10:973–84.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Chekerov R, Hilpert F, Mahner S, El-Balat A, Harter P, De Gregorio N, et al. Sorafenib plus Topotecan versus placebo plus topotecan for platinum-resistant ovarian cancer (TRIAS): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2018;19(9):1247–58.
Colombo N, Tomao F, Benedetti Panici P, Nicoletto MO, Tognon G, Bologna A, et al. Randomized phase II trial of weekly paclitaxel vs. cediranib-olaparib (continuous or intermittent schedule) in platinum-resistant high-grade epithelial ovarian cancer. Gynecol Oncol. 2022;164(3):505–13.
Pignata S, Lorusso D, Scambia G, Sambataro D, Tamberi S, Cinieri S, et al. Pazopanib plus weekly paclitaxel versus weekly paclitaxel alone for platinum-resistant or platinum-refractory advanced ovarian cancer (MITO 11): a randomised, open-label, phase 2 trial. Lancet Oncol. 2015;16(5):561–8.
Roque DM, Siegel ER, Buza N, Bellone S, Silasi DA, Huang GS, et al. Randomised phase II trial of weekly ixabepilone ± biweekly bevacizumab for platinum-resistant or refractory ovarian/fallopian tube/primary peritoneal cancer. Br J Cancer. 2022;126(12):1695–703.
Sharma A, Singh M, Chauhan R, Malik PS, Khurana S, Mathur S, et al. Pazopanib based oral metronomic therapy for platinum resistant/refractory epithelial ovarian cancer: a phase II, open label, randomized, controlled trial. Gynecol Oncol. 2021;162(2):382–8.
Shoji T, Enomoto T, Abe M, Okamoto A, Nagasawa T, Oishi T, et al. Efficacy and safety of standard of care with/without bevacizumab for platinum-resistant ovarian/fallopian tube/peritoneal cancer previously treated with bevacizumab: the Japanese Gynecologic Oncology Group study JGOG3023. Cancer Sci. 2022;113(1):240–50.
Stewart C, Ralyea C, Lockwood S. Ovarian cancer: an integrated review. Semin Oncol Nurs. 2019;35(2):151–6.
Tullio Golia D’Augè, Giannini A, Bogani G, et al. Prevention, Screening, Treatment and Follow-Up of gynecological cancers: state of art and future perspectives. Clin Exp Obstet Gynecol. 2023;50(8):160.
Kaplan AR, Gueble SE, Liu Y, Oeck S, Kim H, Yun Z, et al. Cediranib suppresses homology-directed DNA repair through down-regulation of BRCA1/2 and RAD51. Sci Transl Med. 2019;11(492):eaav4508.
Bizzaro F, Fuso Nerini I, Taylor MA, Anastasia A, Russo M, Damia G, et al. VEGF pathway inhibition potentiates PARP inhibitor efficacy in ovarian cancer independent of BRCA status. J Hematol Oncol. 2021;14(1):186.
Liu JF, Barry WT, Birrer M, Lee JM, Buckanovich RJ, Fleming GF, et al. Overall survival and updated progression-free survival outcomes in a randomized phase II study of combination cediranib and olaparib versus olaparib in relapsed platinum-sensitive ovarian cancer. Ann Oncol. 2019;30(4):551–7.
Giannini A, Di Dio C, Di Donato V, et al. PARP inhibitors in newly diagnosed and recurrent ovarian Cancer. Am J Clin Oncol. 2023;46(9):414–9.
Shah AA, Kamal MA, Akhtar S. Tumor angiogenesis and VEGFR-2: mechanism, pathways and current biological therapeutic interventions. Curr Drug Metab. 2021;22(1):50–9.
Chen D, Zhong X, Lin L, Xie J, Lian Y, Xu L. Comparative efficacy and adverse reactions of apatinib-chemotherapy combinations versus chemotherapy alone for treatment of advanced colorectal cancer: a meta-analysis of randomized controlled trials. Am J Transl Res. 2022;14(9):6703–11.
Itatani Y, Kawada K, Yamamoto T, Sakai Y. Resistance to anti-angiogenic therapy in Cancer-alterations to Anti-VEGF pathway. Int J Mol Sci. 2018;19(4):1232.
Iyer PG, Albini TA. Drug-related adverse effects of antivascular endothelial growth factor agents. Curr Opin Ophthalmol. 2021;32(3):191–7.
Jean GW, Mani RM, Jaffry A, Khan SA. Toxic effects of Sorafenib in patients with differentiated thyroid carcinoma compared with other cancers. JAMA Oncol. 2016;2(4):529–34.
Karczmarek-Borowska B, Sałek-Zań A. Hepatotoxicity of molecular targeted therapy. Contemp Oncol (Pozn). 2015;19(2):87–92.
Liu L, Xiong W. Effect of molecular targeted agents in chemotherapy for treating platinum-resistant recurrent ovarian cancer: a systematic review and meta-analysis. Med (Baltim). 2021;100(32):e26849.
Acknowledgements
We would like to thank all authors who provided published data for our meta-analysis.
Funding
This study was funded by Mass spectrometry project of Liaoning Cancer Hospital & Institute, Project number: ZP202019.
Author information
Authors and Affiliations
Contributions
HDX and SFL contributed the study concept and design. HDX and LS contributed to the data acquisition. HDX and KLY were responsible for data analysis and editing the manuscript. LS and CHX contributed to critical revision of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships, and they have no competing interests.
Disclosure
The authors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, D., Ke, L., Cui, H. et al. Efficacy and safety of VEGF/VEGFR inhibitors for platinum-resistant ovarian cancer: a systematic review and meta-analysis of randomized controlled trials. BMC Women's Health 24, 34 (2024). https://doi.org/10.1186/s12905-023-02879-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02879-y