Abstract
Background
Non-institutional delivery is one of the major reasons that results in high mortality rates for a mother and her neonate. The World Health Organization estimates that only 43% of mothers have access to skilled delivery services. A recent Ethiopian Mini Demographic Survey indicated that more than half of Ethiopian women have given birth non-institutionally. This shows that maternal health remains a major public health challenge in Ethiopia, irrespective of the government’s measures for institutional delivery. So, the aim of this study was to assess the practice of non-institutional delivery and its associated factors among women who gave birth in the study area.
Methods
A community-based cross-sectional study was carried out on 260 study participants from June 1 to July 1, 2022, in Boloso Bombe Woreda. Data collection was done using a structured questionnaire, and systematic sampling techniques were used to select the study subjects. The data was entered into the EPI data version 3.1 and analyzed using SPSS version 25. The adjusted odds ratio, along with 95% confidence intervals, was used, and the level of statistical significance was declared at a P-value of 0.05.
Result
Out of 260 women interviewed, 252 (97%) pregnant women participated in the interview. The prevalence of non-institutional delivery among study participants was 68.7% (95% CI: 63.1–72.9). Mothers who were a daily laborer [AOR = 6.6;95%CI(3.6(1.2–11.2), last pregnancy planned [AOR = 0.4; 95%CI (0.4(0.2–0.8)), an absence of antenatal care contacting history [AOR = 3.3; 95%CI (1.3–8.6)], respondents’ knowledge on the labor complication [AOR = 3; (95%CI); 3.5(2.2–6.1)], and place of first delivery [AOR = 8.7 95%CI(3.2–23)] were factors that significantly associated with practice of non-institutional delivery.
Conclusion
This study indicated that the majority of study participants practiced non-institutional delivery in this study area. Thus, we strongly recommend that all responsible bodies take immediate action, such as community health education on pregnancy-related complications, encouraging ANC visits, and raising awareness of the advantages of preventing non-institutional delivery in order to reduce non-institutional pregnancy practices and improve the factors identified.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Globally, only 123 million women who give birth each year receive antenatal care, neonatal care, and delivery care. To promote maternal, neonatal, and children’s health, women need to access basic health care settings during delivery [1]. According to the World Health Organization (WHO), more than 90% of women in high-income countries give birth at health facilities, whereas in low-income countries, most women give birth outside a health center by untrained people [2]. Non-institutional delivery means just giving birth outside a health institution by an unskilled person [3].
Many women who give birth outside a health facility can face problems such as dizziness, a tender abdomen, blood loss, fetal death, and uterine rupture. These problems are often considered dangerous for women who give birth outside a health facility [4]. Most maternal mortality (MM) occurs during delivery and in the immediate postpartum period. All women should have access to basic maternity care during their pregnancy, such as clean and safe births. They should also have access to emergency obstetric care if necessary [5]. In 2017, as a result of non-institutional deliveries and other-related factors, 462/100,000 mothers and 11/100,000 newborns died in both developed and developing countries, respectively [6].
In addition, giving birth outside a health institution has a three-fold higher risk of developing complications and has a higher risk of death [7]. The rate of neurological dysfunction and seizure in non-institutional delivery is three times higher than in institutional delivery [8]. Increasing delivery in health institutions is a crucial approach to preventing the death of a mother and her baby. However, the practice of institutional delivery has not changed consistently to reduce maternal deaths in low and middle-income countries [9]. Although there have been some improvements in reducing maternal and infant mortality worldwide, countries in sub-Saharan Africa and South Asia accounted for 86 per cent of the global maternal mortality rate in 2017. Only Sub-Saharan African countries accounted for two-thirds of maternal mortality [4, 6].
The literature has identified several factors associated with the practice of non-institutional delivery. These include maternal educational experiences, occupation, previous antenatal care contacts, and knowledge of obstetric complications. However, the last pregnancy planned, and complications from previous deliveries were not assessed in previous studies. [4, 5, 7].
Ethiopia is one of the 15 countries that are in a very high alert or high alert and as being in a fragile state. The practice of institutional delivery is an essential approach to preventing 13–33% and 20–30% maternal and newborn mortality, respectively [10]. Although the Ethiopian Government and non-governmental organizations try to prevent women from giving birth outside health facilities, more than 50% of Ethiopian women give birth outside health care facilities [11]. This shows that our country is still facing challenges in non-institutional delivery [12]. In southern Ethiopia, few studies have been conducted on the scope and factors influencing the non-institutional delivery. The literature available focuses mainly on urban and institutional areas, with little information on updated rural areas. So, the aim of this community-based study is to assess the practice of non-institutional delivery among women delivered in southern Ethiopia.
Methodology
Study area, period and design
A community-based cross-sectional study carried out in Boloso Bombe Woreda from June 1 to July 1 2022. The district is located about 57 km from Wolaita, southern Ethiopia, and 435 km from Addis Abeba, the capital of Ethiopia. Boloso Bombe’s geographical location is 70 1’ 32’’- 70 11’ 30” N latitude and 370 26’ 18’’-370 39’’ 38’’ E longitudinal. According to the Boloso Bombe Woreda Basic Plan Report 2013Woreda has a total population of 114,342. Of these, 57,400 were women, 56,942 were men, and 26,642 were reproductive-age women. The district has 21Kebeles, one primary hospital, four health centers, and eight health posts.
Population and eligibility criteria
Source populations are defined as all women who had given birth during the preceding six months and had resided in the district for at least a year. The study participants included of women who had given birth during the six months prior to the study and had resided for at least a year in the chosen region. Study participants were women who were selected and participated in the study during the data collecting period. The study did not include mothers who had any mental health issues, were deaf or difficulty of hearing, or both.
Sample size determination and its procedures
A total of 260 sample sizes were determined using a single population proportion. 5% margin of error, 95% confidence interval, 19% non-institutional delivery from the previous study, and 10% non-response were considered to calculate the final sample size [13].
According to the World Health Organization recommendation, 30% of the seven Kebeles (small villages) were selected from the total Kebeles using lottery methods. The total number of mothers who delivered in selected kebeles between 2021 and 2022 was determined using immunization registers and health post family folders. The sample size of each kebeles was proportionally allocated to the total number of deliveries of each kebeles for the selected kebeles. The respondents were then recruited using a systematic sampling method. Every other respondent to each kebeles were interviewed.
Study variables
The practice of non-institutional delivery was a dependent variable. Socio-demographic characteristics (age, educational status, occupational status), obstetric (parity, gravidity, ANC follow-up), and health care provider-related factors (privacy, respecting women, friendly behavior of service providers) were independent variables of the study.
Operational definition
Non-utilization of institutional delivery
Deals with women who deliver the last baby outside a health facility by non-skilled or traditional attendants [14].
Knowledge on labor complications
Knowledge level on labor complications measured using six major labor complications, such as failure to labor progress, fetal distress, malposition, fetal distress, excessive bleeding, and cephalopelvic disproportion. Those who mentioned greater than or equal to 3 labor complications were classified as having good knowledge [15]. And those who mention < 3 complications were assumed to have poor knowledge [15].
Data collection and analysis
A structured questionnaire, including four parts, was used to collect data. These include socio-demographic information, factors related to women’s obstetrics, factors related to health providers, and knowledge of labour complications. The last component contains a question that contains a list of the six most important labor complications adapted from the previous study [15].
The data were collected through face-to-face interviews. 10%of the questionnaires were pre-tested in unselected kebeles before the actual data collection began. The data were collected by seven B.Sc. nurses and supervised by three health officers. One day training was provided to data collectors and supervisors on data collection procedures. Firstly, the questionnaire was written in English, translated by experts into the local language, and again translated into English to increase consistency. In order to maintain data quality, the data collectors were closely supervised by the supervisor before and during the data collection process. The principal investigator (PI) supervised the correct implementation of the procedure and checks the completeness and logical coherence of the data collection after collecting the data.
The completeness and coherence of the data have been checked, encoded and entered into EPI Data Version 3.1. To analyze it, it was exported to SPSS version 25. In order to present descriptive statistics, frequencies, percentages, mean, standard deviations, and tables were used. The crude odd ratio (COR) of 95% of the confidence interval was calculated using a bivariate logistic regression test to test correlation between the dependent and the independent and select a the candidate variables. Then the variables that were found to be P < 0.25 in the bivariate analysis are taken as candidates for the multivariable logistic regression. Finally, multivariable logistic regression with AOR was used to control possible errors and to identify associated factors of the prevalence of non-institutional services. A P value < 0.05 was considered statistically significant.
Result
Socio-demographic features
Of a total of 260 women interviewed, 252 (97%) fully responded to the interview. The average age of the study participants was 28.07 years, and the standard deviationwas5.3 years. The age range of the participants was between 15 and 29 years old.122 (48.4%) participants were housewives. 86% of them were married and 205(81.3%) completed secondary school (Table 1).
Obstetric and provider-related factors among the respondents
This study showed that majority of the study participants (93.7%) had an abortion history of 0–3 times. Approximately 196 (77.8%) of the participants visited the ANC during their last pregnancy. Before birth, 198 women (76.6%) planned to have a pregnancy, with 42.9% having one–three children. 73 (21%) of the participants reported that they had not received care for respect during the previous delivery and 85 (34.5%) reported that their privacy has not been maintained during the previous delivery. The main reasons for non-institutional delivery were poor belief in health facilities, sudden onset of labor, and a lack of respect from health care providers (Table 2).
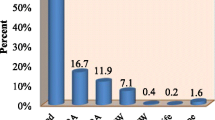
Knowledge of the respondent on labor complications
From the 252 participants, around 60% of women had poor knowledge of labor complications and 40% of them had good knowledge (Fig. 1).
Prevalence of non-institutional delivery
Among the total study participants, 68.7% practiced non-institutional delivery, and 31.3% practiced institutional delivery (Fig. 2).
Factors affecting the practice of non-institutional delivery
Bivariate logistic regression indicated that all variables, except place of first delivery, were significantly associated with dependent variables. Regarding multiple logistic regression, all variables selected for bivariate logistic regression were statistically associated with outcome variables. Mothers who were daily laborers were 6.6 times more likely to practice non-institutional delivery compared to their contrast group [AOR = 6.6; 95%CI (1.2–11.2)]. Women planning their last pregnancy are 60% less likely to give birth outside health institutions compared to unplanned women [AOR = 0.4; 95%CI (0.4 (0.2–0.8))]. Women who had no history of ANC follow-up were 3.3 times more likely to practice non-institution delivery compared to those who had an ANC follow-up history [AOR = 3.3; 95% CI (1.3–8.6)]. Participants who had poor knowledge of the labor complication were 3.5 times more likely to practice non-institutional delivery compared to their opposite group [AOR = 3.5; 95% CI (2.2–6.1)]. Women who gave birth outside of health institutions were 8.7 times more likely to do so than women who gave birth within health institutions [AOR = 8.7, 95% CI (3.2–23)] (Table 3).
Discussion
The non-institutional delivery practice in this study was 68.7%. This study is higher than the study done in the South Wollo Zone, Delanta district [16], Nepal (41.9%) [17], and Brazil (11.7%) [18]. Findings from the study are in line with the study done in Afar (71%) [19]. However, the variation in both cases may be due to differences in socio-demographic status, sample size, study period, geographic location, and methodological variation.
In this study, respondents’ occupational status was significantly associated with non-institutional delivery. Mothers who were daily laborers were three times more likely to give birth in non-institutions than mothers who were civil servants in occupation status. This study is supported by a study done in Gambela [14] and Benshangul Gumuz [20]. This may be due to the fact that being a daily laborer can inhibit them from getting health-related information easily, such as an advantage of institutional delivery and/or a disadvantage of non-institutional delivery; they may be easily exposed to economic problems that might inhibit access to a health facility; they are more exposed to family pressure and cultural influences. In addition, daily laborers had less awareness regarding complications of pregnancy, delivery, and labor, as well as the postnatal period, since they spent most of their time at work. Thus, this could increase the utilization of non-institutional delivery among them.
The place of previous delivery was significantly associated with non-institutional delivery. Women who gave their last birth outside a health center were 8.7 times more likely to give birth outside a health center than their counterparts. This study was in line with studies done in Ethiopia [21, 22]. The reason for this could be that mothers who lack adequate information about the benefits of institutional delivery may believe they are at lower risk of complications. As a result, this could increase the likelihood of non-institutional delivery and require close monitoring.
ANC is the most favorable period of contact for pregnant women to get adequate information about the risks and problems they may face during pregnancy, labor, delivery, and the postpartum period. The World Health Organization recommends that women without complications should have at least eight ANC contacts [23]. The study found that who had not followed were 3.3 times more likely to give birth outside a health center than those who had ANC follow-up. Which is consistent with studies done in the Delanta district [16], Zala Woreda [24] and, Nigeria [19]. This could be related to the fact that women who had no ANC might be less aware of birth preparedness and complications, danger signs of a pregnancy readiness plan, when to visit a health facility, and the danger of giving birth at a non-institutional place, which increases the chance of a non-institutional delivery.
Knowledge is an important factor that affects intentions, attitudes, and behavior. Lack of risk perception of delivery and labour could increase the use of non-institutional delivery [1, 22]. Study participants who had no previous knowledge of labor and delivery were 3.5 times more likely to give birth outside a health facility than their opposite group. The possible explanation might be that knowledge of labor and delivery complications is essential for early recognition of the problem and appropriate for timely utilization of institutional delivery services. Thus, women who do not have good knowledge of labor and delivery complications, tend to deliver at non-institutional places. Teaching mothers and the community about the complications of non-institutional delivery increases the need for a preference for place of delivery, which is likely to be more useful in contributing to decision-making.
Previous deliveries’ complications were identified as explanatory variables significantly associated with non-institutional delivery. Respondents who had complications were 2.5 times more likely to give birth outside of health facilities compared to their counterparts. The possible explanation might be the occurrence of complications that can contribute to stress and dissatisfaction and limit the utilization of institutional delivery. No previous literature indicated an association between complications occurring in previous health facilities and non-institutional deliveries [13,14,15,16,17,18,19,20,21,22]. Finally, the last pregnancy planned was negatively and significantly associated with the non-utilization of institutional delivery. Mothers who planned their last pregnancy were 60% less likely to practice non-institutional delivery compared to the opposite group. This may be because mothers who planned their last pregnancy may have an interest in seeking health care, following health care recommendations, and cooperating with their partners. No previous literature indicated an association between the last pregnancy plan and non-institutional delivery practice [13,14,15,16,17,18,19,20,21,22]. The main strength of the study was that, being community-based; it could reflect the experiences of the women during the study period. The limitation of the study was that it included mothers who gave birth one year prior to the survey, which might result in a recall bias.
Conclusion
In general, 68.7% of mothers have given birth outside a health care facility. The main reasons for this are poor belief in the health care provider and the sudden onset of labor. Respondents’ occupation, last pregnancy planned, place of previous delivery, ANC follow-up, and knowledge of labor and delivery complications were associated factors. So, we strongly recommend that all stakeholders, such as health extension workers, health care providers, the district health office, and the district city administration, take immediate strategic actions to reduce the prevalence of non-institutional delivery and work more on the main reasons and factors that increase the practice of non-institutional delivery. Furthermore, actions aimed at maternal health education, encouraging ANC visits for pregnancy planning, and raising awareness about labor and delivery complications were critical to address for women giving birth outside of health facilities.
Data Availability
The data collected and/or analyzed in the current study are not available to the public before publication to prevent any misuse by the public, but are available upon reasonable request from the corresponding author.
References
UNFPA, MATERNAL HEALTH IN AFRICA: fact sheet., 2013. https://www.unfpa.org/sites/default/files/resource-pdf/EN_Maternal%20Health%20in%20Africa_factsheet_web.pdf.
World health organization, maternal mortality, key fact., 2017. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
James Kicinski-McCoy, Motherhood: Home Birth Vs. Hospital Birth., 2016. https://www.mothermag.com/home-birth-vs-hospital-birth/.
Sato R. Advantages and disadvantages of Institutional Delivery and Home Delivery: a qualitative study in Northern Nigeria. Eur J Prev Med Vol. 2021;9(1):19–24. https://doi.org/10.11648/j.ejpm.20210901.14.
Anna Jallow (Able-Thomas), WHY, ARE THERE LOW INSTITUTIONAL DELIVERY RATES IN. THE GAMBIA? WOMEN’S OPINION, University of Oslo, 2007. https://core.ac.uk/download/pdf/30858827.pdf.
World health organization, maternal mortality, key fact sheets., 2019. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
American Associates., Ben-Gurion University of the Negev. Home births are three times more dangerous than hospital deliveries., Sci Dly, 4 March 2019. https://www.sciencedaily.com/releases/2019/03/190304095841.htm.
WebMD. What to know about home delivery, 2021. https://www.webmd.com/baby/what-to-know-about-home-birth.
By Anna D. In Low- And Middle-Income Countries, Is Delivery In High Quality Obstetric Facilities Geographically Feasible? HEALTH AFFAIRS 38, NO. 9 (2019): 1576–1584. https://doi.org/10.1377/hlthaff.2018.05397.
Moyer RM, Adanu, Cyril M. Engmann the relationship between facility-based delivery and maternal and neonatal mortality in Sub-Saharan Africa Chery, 2013. https://doi.org/10.1016/j.ijgo.2013.04.010.
Central statistical Agency; Ethiopian Demographic health survey., 2016. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf.
USAID, Ethiopia fact sheet maternal and child health. 2016. https://www.usaid.gov/ethiopia/fact-sheets.
Gultie T, Wasihun B, Kondale M, Balcha B. Home Delivery and Associated factors among Reproductive Age Women in Shashemene Town, Ethiopia. J Women’s Health Care. 2016;5:300.
Gora GA, Umer MF, Ojulu PO, Betaw ST, Cham AO, Gora OA, Qi X. Non-institutional childbirths and the Associated Socio-Demographic factors in Gambella Regional State, Ethiopia. Int J Environ Res Public Health. 2021;18:2859.
Asmelash Abera Mitiku, Abraham Lomboro Dimor. : Determinants of Home Delivery among mothers in Abobo District, Gambella Region, Ethiopia: a Case Control Study : International Journal of Reproductive Medicine volume 2020, Article ID 8856576, 7 pages.
Wodaynew T, Fekecha B, Abdisa B. Magnitude of Home Delivery and Associated Fac-tors among Antenatal Care Booked Mothers in Delanta District, South Wollo Zone, North East Ethiopia: a cross-sectional study, March 2018. Int J Womens Health Wellness. 2018.
Dhakal P, Shrestha M, Baral D, Morang, et al. Nepal Int J Community Based Nurs Midwifery. 2018;6(1):2.
Wachs LS, Nunes BP, Soares MU et al. Prevalence of home care and associated factors in the brazilian elderly population. Cadernos de Saude Publica. 2016;32(3).
Abdella M, Abraha A, Gebre A, et al. Magnitude and Associated factors for Home Delivery among Women who gave birth in last 12 months in Ayssaita, Afar, Ethiopia-2016. A Community Based Cross Sectional Study. Glob J Fertil Res. 2017;2(1):30–9.
Berhe and Nigusie. Magnitude of home delivery and associated factors among child bearing age mothers in Sherkole District, Benishangul Gumuz regional state-western-ethiopia. BMC Public Health. 2020;20:796.
Ibrahim SA, Handiso TB. Markos selamu Jifar, Eshetu Yoseph. Analyzing prevalence of Home Delivery and Associated factors in Anlemo District, Southern Ethiopia. Int Annals Med. 2017;1(5).
Fira Abamecha A, Tariku Tesfaye B. Delivery Site Preferences and Associated factors among Married Women of Child Bearing Age in Bench Maji Zone, Ethiopia Ethiop J Health Sci Vol. 26, No. 1 January 2016.
WHO recommendations on antenatal care for a positive pregnancy experience. (2016). Accessed by https://apps.who.int/iris/bitstream/handle/10665/259947/WHO-RHR-18.02-eng.pdf?sequence=1.
Kucho B, Mekonnen N. Delivery at home and associated factors among women in child bearing age, who gave birth in the preceding two years in Zala Woreda, southern Ethiopia. J Public Health Epidemiol. 2017;9(6):177–88.
Acknowledgements
We would like to express my appreciation to Wolaita Sodo University, College of Medicine and Health Sciences, and School of Nursing for continued support and follow-up.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
TG: Conceived data and designed the study, supervised the data collection, performed the analysis and interpretation of data, drafted the manuscript, and finally approved the revision for publication. TG had full access to all the data in the study and takes responsibility for the integrity of data and the accuracy of data analysis. FS and FA assisted in designing the study and data interpretation, and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare they have no competing interest. We declare that this paper is our original work and has never been presented in any university and we understand that plagiarism will not be tolerated and all directly quoted material has been appropriately referenced.
Ethical approval and consent to participate
Wolaita Sodo University, College of Health Science Institutional review board approved all experimental protocols and issued ethical clearance with reference to the number of WSU/IRB/1288/2022. Informed consent was obtained from all participants after the nature of the study was fully explained to them in their local languages. A thumbprint or signature was used on the consent form. Only those who signed the written consent took part in the study. Throughout the research process, the participants provided codes to maintain confidentiality. The entire study participants were informed that data was kept private and confidential and used only for research purposes. The participants were assured that they would have the right to withdraw if they would not like at any time. Personal privacy and cultural norms were respected. The method was carried out in line with the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Geta, T., Sugebo, F. & Anjulo, F. Practice of non-institutional delivery and its associated factors among women who gave birth in Southern Ethiopia, 2022. BMC Women's Health 23, 529 (2023). https://doi.org/10.1186/s12905-023-02683-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02683-8