Abstract
Background
Post pregnancy family planning includes both postpartum and post-abortion periods. Post pregnancy women remain one of the most vulnerable groups with high unmet need for family planning. This review aimed to describe and assess the quality of the evidence on implementation strategies, facilitators, and barriers to scaling up and sustaining post pregnancy family planning.
Methods
Electronic bibliographic databases (MEDLINE, PubMed, Scopus, the Cochrane Library, and Global Index Medicus) were searched from inception to October 2022 for primary quantitative, qualitative, and mixed method reports on scaling up post pregnancy family planning. Abstracts, titles, and full-text papers were assessed according to the inclusion criteria to select studies regardless of country, language, publication status, or methodological limitations. Data were extracted and methodological quality assessed using the Mixed Methods Appraisal Tool. The convergent integrated approach and a deductive thematic synthesis were used to identify themes and sub-themes of strategies to scale up post pregnancy family planning. The health system building blocks were used to summarize barriers and facilitators. GRADE-CERQual was used to assess our confidence in the findings.
Results
Twenty-nine reports (published 2005–2022) were included: 19 quantitative, 7 qualitative, and 3 mixed methods. Seven were from high-income countries, and twenty-two from LMIC settings. Sixty percent of studies had an unclear risk of bias. The included reports used either separate or bundled strategies for scaling-up post pregnancy family planning. These included strategies for healthcare infrastructure, policy and regulation, financing, human resource, and people at the point of care. Strategies that target the point of care (women and / or their partners) contributed to 89.66% (26/29) of the reports either independently or as part of a bundle. Point of care strategies increase adoption and coverage of post pregnancy contraceptive methods.
Conclusion
Post pregnancy family planning scaling up strategies, representing a range of styles and settings, were associated with improved post pregnancy contraceptive use. Factors that influence the success of implementing these strategies include issues related to counselling, integration in postnatal or post-abortion care, and religious and social norms.
Trial registration
Center for Open Science, OSF.IO/EDAKM
Plain English Summary
Family planning could prevent one third of maternal deaths by allowing women to delay motherhood, avoid unintended pregnancies and subsequent abortions. Post pregnancy family planning includes both postpartum and post-abortion periods. Post pregnancy women remain one of the most vulnerable groups with high unmet need for family planning. Scaling up post pregnancy family planning is essential for achieving universal access to reproductive health-care services. Reports of strategies to scale up post pregnancy family planning were systematically reviewed and summarized. These included strategies for healthcare infrastructure, policy and regulation, financing, human resource, and people at the point of care. Strategies that target the point of care (women and/or their partners) contributed to 89.66% (26/29) of the reports either independently or as part of a bundle. Point of care strategies increase adoption and coverage of post pregnancy contraceptive methods. Certain factors influence the success of implementing these strategies, including issues related to counselling, integration in postnatal or post-abortion care, and religious and social norms.
Similar content being viewed by others
Background
Post pregnancy women have a high unmet need for family planning (FP). Post pregnancy family planning (PPFP) includes both postpartum and post-abortion periods. The World Health Organization (WHO) recommends spacing pregnancies by two years or more following the delivery of a newborn, and at least six months after receiving post-abortion care [1]. This recommendation is based on evidence that PPFP reduces the burden of maternal and perinatal adverse events [2].
Despite this, there are still major missed opportunities for FP among postpartum women in many low- and middle-income countries (LMIC) and many post-abortion clients still leave the facility without a contraceptive method [3, 4].
Therefore, scaling up PPFP is important to allow women to delay motherhood, avoid unintended pregnancies and subsequent abortions, and consequently preventing maternal morbidity and mortality [5, 6]. Investing in scaling up PPFP can accelerate achievement across Sustainable Development Goal [7].
Scaling up is defined as deliberate efforts to increase the impact of health service innovations successfully tested in pilot or experimental projects to benefit more people and to foster policy and program development on a lasting basis [8,9,10].
The WHO has commissioned this systematic review of scaling up of post pregnancy family planning. The overall aim of the review is to describe and assess the quality of the evidence on implementation strategies, facilitators, and barriers to scaling up and sustaining post pregnancy family planning. The review has the following objectives:
-
to identify, appraise and synthesize research evidence regarding the approaches or strategies to scaling up PPFP for improving coverage and sustainability.
-
to identify, appraise and synthesize research evidence on the barriers to and facilitators of scaling up of PPFP.
Methods
This systematic review followed the JBI methodology for mixed methods systematic reviews (MMSR) [11] and methods suggested by the Cochrane Effective Practice and Organisation of Care (EPOC) Review Group [12]. The protocol, available as a preprint [13], was registered in the Center for Open Science platform (https://doi.org/10.17605/OSF.IO/EDAKM). The full review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [14].
Criteria for considering studies for this review
Types of studies
Reports of primary studies, either quantitative, qualitative, process evaluation, policy analysis, and case studies were considered eligible. Mixed method studies were considered if data from the quantitative or qualitative components can be clearly extracted. Editorials, commentaries, proposals, conference abstracts and systematic reviews were excluded. Reports that lacked a clear methodology section were also excluded if clarification could not be obtained from the authors. There were no restrictions on length of study follow-up, language of publication, or country of origin.
Types of participants
Study participants were the targets of strategies that would scale up PPFP, whether individuals (recipients of care, providers of care, other stakeholders), organizations, or systems.
Types of scaling up strategies
Approaches or strategies of scaling-up [9, 15,16,17] healthcare infrastructure-related (e.g., providing medical equipment or changing linkages within a health system), policy and regulation-related (e.g., revising policy to allow widespread community-based case management of a disease), financing-related (e.g., changing payment mechanisms), human resource-related (e.g., training and deployment of health care providers, changing roles of administrators), and patient-related (e.g., involving patients/public in recruitment or promotion).
Types of outcome measures
Implementation research outcomes mainly adoption (the intention, initial decision, or action to try to employ a new intervention; also known as Uptake, Utilization, Intention to try), coverage (the degree to which the population that is eligible to benefit from an intervention actually receives it.), and sustainability (the extent to which an intervention is maintained or institutionalized in a given setting; also known as maintenance, continuation) [18, 19].
Barriers to and facilitators (Factors that influence scaling up of PPFP)
The approach to the factors affecting scaling up was based on Supporting the Use of Research Evidence (SURE) framework [20], namely factors related to recipients of care, providers of care, other stakeholders (including other healthcare providers, community health committees, community leaders, program managers, donors, policymakers, and opinion leaders), health system constraints, and social and political constraints (Supplementary file 1).
Factors were grouped by the categories of health system building blocks (HSBB). HSBB is an analytical framework used by WHO to describe health systems, disaggregating them into 6 core components with the people in the center: (i) service delivery, (ii) health workforce, (iii) health information systems, (iv) Medical products, vaccines, and technologies (access to essential medicines), (v) financing, and (vi) leadership and governance [21].
Literature search
Sources
Bibliographic databases were searched for peer reviewed publications as well as grey literature. We performed the search strategy to identify published studies in the following electronic bibliographic databases (from inception to October 2022): MEDLINE, PubMed, Scopus, the Cochrane Library, and Global Index Medicus, World Health Organization (www.globalindexmedicus.net). Search also included gray literature using the search engines and websites of relevant organizations. The reference list of all included reports was screened for additional studies.
Search strategy
The search terms were developed a priori. We followed recommendations of a previous review about terms to use for scaling up [22]. The search strategy was first developed in Pubmed format and was adapted to the other databases. The full search strategies for various platforms are available in an open access repository [23]. For unpublished studies, the review authors contacted global experts in family planning to identify possible reports. The email was sent through 3 major mailing lists maintained by relevant international organizations in the field of family planning.
The search strategies utilized the following terms (“Implementation Science” [MeSH Terms] OR scaling-up [Text Word] OR Scalability [Text Word] OR Scale-up [Text Word]) AND (“Family Planning Services” [MeSH Terms] OR contraception [MeSH Terms] OR contracept*[Text Word] OR “family planning” [Text Word]). The search aimed at sensitivity rather than precision since we opt to minimize false negative results.
Management of search results
All search results were imported into Jabref v5. Duplicate search results were identified by the software and were eliminated using a method that enables retaining unique citations without accidentally excluding false duplicates.
Data collection
Study selection
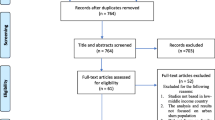
After removal of duplicates, two review authors (EI, NA) independently piloted the study selection form with a small random sample of studies to assess understanding of eligibility criteria and ease of use of the form. Two review authors (NW, NM) independently screened all titles/abstracts and full text to identify the relevant studies. Discrepancies between review authors regarding study eligibility was resolved by consensus or, when required, with a third party (AN). PRISMA flowchart was used to describe the process of study selection.
Data extraction
Two review authors (NW, NM) used a data extraction form (Supplementary file 2) adapted from JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach [11], to independently extract characteristics from the included studies: study title, first author, year of publication, country of study, the country’s economic status (low-, middle-, or high-income), funding source, study setting, facility type, study type (qualitative, quantitative and mixed methods studies). Data extraction included the components of scaling-up strategies mentioned in each study, the target of the scale up activity, the time frame of the scaling-up process, implementation outcome evaluated in each study, and barriers and facilitators. Any disagreement in the data collection process was resolved through discussion and consensus between the two reviewers and, if needed, with a third party (AN).
Quality assessment
For each included study, the methodological quality was described using the corresponding Mixed-Methods Appraisal Tool (MMAT) criteria (Supplementary file 3). [24, 25] Two independent reviewers (NW, NM) assessed the quality of included studies using MMAT, with a third independent reviewer (AN) to be used in case of any discrepancies. Studies were not excluded based on methodological limitations, but rather used to assess the confidence in the findings.
Data synthesis
A convergent integrated approach was used. This involved transformation into textual descriptions or narrative interpretation of the quantitative results in a way that answers the review questions. Articles were first grouped according to component(s) of scaling up, as defined above. A deductive thematic synthesis used the SURE framework and the health system building blocks to synthesize the factors affecting implementation (barriers and facilitators).
Appraisal of confidence in the review findings
GRADE‐CERQual was used to assess the confidence that can be placed in each review finding [26]. GRADE‐CERQual approach assesses confidence in the evidence based on four components: methodological limitations of included studies, coherence of the review findings, adequacy of the data contributing to a review finding, and relevance of the included studies to the review question.
After assessing each of the four components, a judgement about the overall confidence in the evidence supporting each review finding was made. The judgment of confidence was either high, moderate, low, or very low. The final assessment was based on consensus among the review authors. Summaries of the findings and the assessments of confidence in these findings were presented in Tables 3 and 4.
Researchers’ reflexivity
We maintained a reflexive stance throughout the stages of the review process, from study selection to data synthesis, as detailed in the review protocol [13].
Results
Study selection
The flow of identification, screening, and including 29 reports is depicted in Fig. 1
Findings of the review
Characteristics of included studies
The 29 included studies [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55] (Table 1) used quantitative (19/29; 65.52%), qualitative (7/29; 24.14%), and mixed methods (3/29; 10.34%). The studies were all published between 2005 and 2022. The studies werereported from 37 countries, from all regions, and from LMIC and High-income countries. Eight studies were reported from the USA [27,28,29,30,31,32,33,34]; four from Tanzania [35,36,37,38], two from Sri Lanka [39, 40], Nigeria [41, 42], Nepal [43, 44], Rwanda [45, 46], Bangladesh [38, 47], and one study from Benin [48], Bolivia [49], Burkina Faso [50], Chad [48], Côte d’Ivoire [48], Democratic Republic of Congo [50], Guatemala [51], India [52], Liberia [53], Mexico [49], Niger [48], Pakistan [54], Senegal [48], Togo [48], and Turkey [55].
Methodological quality
Most of the included reports (17/29; 58.62%) had unclear risk of bias, with 9/29 (31.03%) were judged to be at high risk if bias.
Strategies of scaling-up post pregnancy family planning
The included 29 reports [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55] described unique yet interrelated strategies of scaling-up post pregnancy family planning including healthcare infrastructure, policy and regulation, financing, human resource, and recipient of care. Most reports (19/29; 65.52%) utilized a combination of these strategies, Table 2.
Effect of strategies for scaling up post pregnancy family planning
Strategies that target the point of care (women and / or their partners) contributed to 89.66% (26/29) of the reports either independently (Table 3) or as part of a bundle (Table 4) to scale up post pregnancy FP. Point of care, financial, and health resources strategies improved adoption and coverage of post pregnancy contraceptive methods (moderate certainty evidence).
Factors influencing scaling up of PPFP
The health system building blocks framework was used to allow synthesis of factors that influence the scaling up of PPFP, Table 5. The most notable barriers to scaling up PPFP included failure to provide effective counselling, lack of integration of PPFP in postnatal or post-abortion care, and negative religious and traditional norms.
Discussion
Summary of the evidence
The review identified unique yet interrelated strategies of scaling-up post pregnancy family planning including healthcare infrastructure, policy and regulation, financing, human resource, and recipient of care. Most reports (19/29; 65.52%) utilized a combination of these strategies. Results show that point of care strategies, financing strategies, human resource strategies increase the use of post pregnancy contraceptive methods.
The review highlighted core components of strategies for scaling up post pregnancy family planning. The results agree with and update previously published reviews [56]. These components include training or continuing education and ongoing technical assistance at the health care provider level; provision of low- or no-cost contraception, grants for contraceptive equipment or supplies, and quality improvement and monitoring at the health facility level; public awareness campaigns and stakeholder engagement at the community level; and legislation or other policy changes at the public policy level. Implementation of these intervention components is interrelated and represents a theory-based, systems change approach wherein multiple interventions are implemented across levels to maximize effects across diverse and often fragmented systems of care in different countries.
The results of the current review agree with a previous review [57] that suggested that offering modern contraception services as part of care provided during childbirth or abortion increases post pregnancy contraceptive use and is likely to reduce both unintended pregnancies and pregnancies that are too closely spaced. Evidence for sustainability is insufficient and this remains an important issue to maintain a reduction in unmet needs for postpartum or post abortion periods. The need for integration with health system is critical for family planning to be institutionalized and therefore sustainable [58].
Improving the effectiveness of family planning programs is critical for empowering women and adolescent girls, improving human capital, reducing dependency ratios, reducing maternal and child mortality, and achieving demographic dividends particularly in low- and middle-income countries [59].
The current review critically summarized the factors that affect the success of scaling up of PPFP. The most apparent factors influencing the success of implementing these strategies include factors related to effective counselling and challenges in the integration of PPFP in postnatal or post-abortion care. These factors should be carefully considered by policymakers and family planning service planners in the development of guidance document and programmatic tools for planning and implementing strategies to scale up PPFP.
Limitations
First, although a comprehensive literature search was conducted and a meticulous screening process was performed, yet the possibility of unpublished work always exists. Second, the adoption of clear criteria for what constitutes a standalone scaling up strategy was a major challenge. Each theme of scaling up PPFP contains a diversity of possible processes, content, and operational environments. Because these variables are often not controlled across studies, it is difficult to rigorously determine the situations in which specific strategies work best. Finally, information regarding the processes of scaling up strategies were not described in sufficiently informative details.
Conclusions
Post pregnancy family planning can be scaled up using different strategies across a range of settings. This scale up appears to improve the uptake and utilization of post pregnancy contraceptive use. Programs striving to achieve a high impact need to overcome the most critical identified barriers namely those related to counselling and those related to integrating PPFP with postpartum or post-abortion care.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- CERQual:
-
Confidence in the Evidence from Reviews of Qualitative research
- EPOC:
-
Effective Practice and Organization of Care
- FP:
-
Family Planning
- GRADE:
-
Grading of Recommendations Assessment, Development, and Evaluation
- HSBB:
-
Health System Building Blocks
- JBI:
-
Joanna Briggs Institute
- LMIC:
-
Low- and middle-income countries
- MMAT:
-
Mixed Methods Appraisal Tool
- MMSR:
-
Mixed methods systematic reviews
- PPFP:
-
Post Pregnancy Family Planning
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SURE:
-
Supporting the Use of Research Evidence
- WHO:
-
World Health Organization
References
World Health Organization. Report of a WHO technical consultation on birth spacing: Geneva, Switzerland 13–15 June 2005. Geneva: World Health Organization; 2007. Available from: https://apps.who.int/iris/handle/10665/69855.
Makins A, Cameron S. Post pregnancy contraception. Best Pract Res Clin Obstet Gynaecol. 2020;66:41–54.
Moore Z, Pfitzer A, Gubin R, Charurat E, Elliott L, Croft T. Missed opportunities for family planning: an analysis of pregnancy risk and contraceptive method use among postpartum women in 21 low- and middle-income countries. Contraception. 2015;92:31–9.
Shah IH, Santhya KG, Cleland J. Postpartum and post-abortion contraception: From research to programs. Stud Fam Plann. 2015;46:343–53.
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJL, Group CRAC. Selected major risk factors and global and regional burden of disease. Lancet (London, England). 2002;360:1347–60.
Chola L, McGee S, Tugendhaft A, Buchmann E, Hofman K. Scaling up family planning to reduce maternal and child mortality: the potential costs and benefits of modern contraceptive use in South Africa. PLoS One. 2015;10:e0130077.
Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Global Health Sci Pract. 2016;4:191–210.
Simmons R, Fajans P, Ghiron L. Scaling up health service delivery: From pilot innovations to policies and programmes. 2008.
World Health Organization. Practical guidance for scaling up health service innovations. World Health Organization; 2009. Available from: https://apps.who.int/iris/handle/10665/44180.
World Health Organization and ExpandNet. Nine steps for developing a scaling-up strategy. World Health Organization; 2010. p. vi, 35 p. Available from: https://apps.who.int/iris/handle/10665/44432.
Lizarondo L, Stern C, Carrier J, Godfrey C, Rieger K, Salmond S, Apostolo J, Kirkpatrick P, Loveday H. Chapter 8: Mixed methods systematic reviews. In: Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis. JBI, 2020. Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-09.
Glenton C, Bohren MA, Downe S, Paulsen EJ, Lewin S, on behalf of Effective Practice and Organisation of Care (EPOC). EPOC Qualitative Evidence Syntheses: Protocol and review template v1.3. EPOC Resources for review authors. 2022. Available from: https://doi.org/10.5281/zenodo.5973704.
Nabhan A, Kabra R, Kiarie J. Implementation strategies, facilitators, and barriers to scaling up and sustaining post pregnancy family planning, a mixed-methods systematic review protocol. 2022. https://doi.org/10.21203/rs.3.rs-2388545/v2.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Barker PM, Reid A, Schall MW. A framework for scaling up health interventions: Lessons from large-scale improvement initiatives in africa. Implement Sci. 2015;11(1):12.
Milat A, Newson R, King L, Rissel C, Wolfenden L, Bauman A, et al. A guide to scaling up population health interventions. Public Health Res Pract. 2016;26(1, 1):e2611604.
Ben Charif A, Zomahoun HTV, LeBlanc A, Langlois L, Wolfenden L, Yoong SL, et al. Effective strategies for scaling up evidence-based practices in primary care: A systematic review. Vol. 12, Implementation science: IS. Health; Social Services Systems, Knowledge Translation; Implementation component of the Quebec SPOR-SUPPORT Unit, Université Laval, Quebec, QC, Canada.; 2017. p. 139. Available from: https://europepmc.org/articles/PMC5700621?pdf=render.
Peters D, Adam T, Alonge O, Agyepong IA, Tran N. Implementation research: what it is and how to do it. BMJ (Clin Research Ed). 2013;347:f6753.
Peters D, Tran N, Adam T. Implementation research in health: a practical guide. Geneva: World Health Organization; 2013. Available from: https://apps.who.int/iris/handle/10665/91758.
The SURE Collaboration. SURE Guides for Preparing and Using Evidence-Based Policy Briefs: 5. Identifying and addressing barriers to implementing policy options. Version 2.1 [updated November 2011]. The SURE Collaboration, 2011. Available from www.evipnet.org/sure.
Savigny D de, Adam T, Alliance for Health Policy and Systems Research & World Health Organization. Systems thinking for health systems strengthening. Edited by Don de Savigny and Taghreed Adam. World Health Organization; 2009. Available from: https://apps.who.int/iris/handle/10665/44204.
Milat AJ, Bauman A, Redman S. Narrative review of models and success factors for scaling up public health interventions. Implement Sci. 2015;10:113.
Nabhan A. Search strategy: Post pregnancy family planning. figshare. 2022; Available from: https://figshare.com/articles/journal_contribution/Search_strategy_post_pregnancy_family_planning/21746852.
Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. Int J Nurs Stud. 2009;46:529–46.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods appraisal tool (MMAT), version 2018. 2018;1148552(10):1–10.
Lewin CAMK Simon AND Glenton. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLOS Med. 2015;12(10):1–18. https://doi.org/10.1371/journal.pmed.1001895.
DeSisto CL, Kroelinger CD, Estrich C, Velonis A, Uesugi K, Goodman DA, et al. Application of an implementation science framework to policies on immediate postpartum long-acting reversible contraception. Public Health Rep (Washington, DC : 1974). 2019;134:189–96.
Koch SK, Paul R, Addante AN, Brubaker A, Kelly JC, Raghuraman N, et al. Medicaid reimbursement program for immediate postpartum long-acting reversible contraception improves uptake regardless of insurance status. Contraception. 2022;113:57–61.
Lacy MM, McMurtry Baird S, Scott TA, Barker B, Zite NB. Statewide quality improvement initiative to implement immediate postpartum long-acting reversible contraception. Am J Obstet Gynecol. 2020;222(S910):e1–8.
Palm HC, Degnan JH, Biefeld SD, Reese AL, Espey E, Hofler LG. An initiative to implement immediate postpartum long-acting reversible contraception in rural New Mexico. Am J Obstet Gynecol. 2020;222(S911):e1–7.
Simmons KB, Edelman AB, Li H, Yanit KE, Jensen JT. Personalized contraceptive assistance and uptake of long-acting, reversible contraceptives by postpartum women: a randomized, controlled trial. Contraception. 2013;88:45–51.
Tang JH, Dominik RC, Zerden ML, Verbiest SB, Brody SC, Stuart GS. Effect of an educational script on postpartum contraceptive use: a randomized controlled trial. Contraception. 2014;90:162–7.
Wilkinson B, Ascha M, Verbus E, Montague M, Morris J, Mercer B, et al. Medicaid and receipt of interval postpartum long-acting reversible contraception. Contraception. 2019;99(1):32–5. Available from: https://www.sciencedirect.com/science/article/pii/S0010782418304268.
Zerden ML, Tang JH, Stuart GS, Norton DR, Verbiest SB, Brody S. Barriers to receiving long-acting reversible contraception in the postpartum period. Women’s Health Issues. 2015;25:616–21.
Pearson E, Senderowicz L, Pradhan E, Francis J, Muganyizi P, Shah I, et al. Effect of a postpartum family planning intervention on postpartum intrauterine device counseling and choice: Evidence from a cluster-randomized trial in tanzania. BMC Women’s Health. 2020;20:102.
Rasch V, Yambesi F, Kipingili R. Scaling up postabortion contraceptive service–results from a study conducted among women having unwanted pregnancies in urban and rural tanzania. Contraception. 2005;72:377–82.
Stephens B, Mwandalima IJ, Samma A, Lyatuu J, Mimno K, Komwihangiro J. Reducing barriers to postabortion contraception: the role of expanding coverage of postabortion care in Dar es Salaam, Tanzania. Global Health Sci Pract. 2019;7:S258–70.
Yahner M. Promising directions and missed opportunities for reaching first-time mothers with reproductive, maternal, newborn, and child health services: findings from formative assessments in two countries. Save the Children US. 2022; Available from: https://resourcecentre.savethechildren.net/document/promising-directions-and-missed-opportunities-for-reaching-first-time-mother-with-reproductive-maternal-newborn-and-children-health-services-findings-from-formative-in-two-countries/.
de Silva R, Huber-Krum S, Samarasekera A, Karra M, Pearson E, Senanayake H, et al. Provider perspectives in implementing the postpartum intrauterine device initiative in sri lanka: a qualitative study. BMJ Sex Reprod Health. 2021;47:193–9.
Karra M, Pearson E, Pradhan E, de Silva R, Samarasekera A, Canning D, et al. The effect of a postpartum IUD intervention on counseling and choice: Evidence from a cluster-randomized stepped-wedge trial in sri lanka. Trials. 2019;20:407.
Eluwa GI, Atamewalen R, Odogwu K, Ahonsi B. Success providing postpartum intrauterine devices in private-sector health care facilities in nigeria: factors associated with uptake. Global Health Sci Pract. 2016;4:276–83.
Sodje JDK, Enaruna NO, Ehigiegba AE, Aromeh CO, Atamewalen M. Feasibility, acceptability, and uptake of postpartum intrauterine contraceptive devices in southern nigeria. Int J Gynaecol Obstet. 2016;135:149–53.
Pradhan E, Canning D, Shah IH, Puri M, Pearson E, Thapa K, et al. Integrating postpartum contraceptive counseling and IUD insertion services into maternity care in nepal: Results from stepped-wedge randomized controlled trial. Reprod Health. 2019;16:69.
Wu WJ, Tiwari A, Choudhury N, Basnett I, Bhatt R, Citrin D, et al. Community-based postpartum contraceptive counselling in rural Nepal: a mixed-methods evaluation. Sex Reprod Health Matters. 2020;28(MEDLINE:32546070, 2):1765646.
Espey J, Ingabire R, Nyombayire J, Hoagland A, Da Costa V, Mazzei A, et al. Postpartum long-acting contraception uptake and service delivery outcomes after a multilevel intervention in Kigali, Rwanda. BMJ Sex Reprod Health. 2021;47:173–8.
Ingabire R, Nyombayire J, Hoagland A, Da Costa V, Mazzei A, Haddad L, et al. Evaluation of a multi-level intervention to improve postpartum intrauterine device services in Rwanda. Gates Open Res. 2018;2:38.
Cooper CM, Ahmed S, Winch PJ, Pfitzer A, McKaig C, Baqui AH. Findings from the use of a narrative story and leaflet to influence shifts along the behavior change continuum toward postpartum contraceptive uptake in sylhet district, bangladesh. Patient Educ Couns. 2014;97:376–82.
Pleah T, Hyjazi Y, Austin S, Diallo A, Dao B, Waxman R, et al. Increasing use of postpartum family planning and the postpartum IUD: early experiences in West and Central Africa. Global Health Sci Pract. 2016;4(Suppl 2):S140–52.
Billings DL, Crane BB, Benson J, Solo J, Fetters T. Scaling-up a public health innovation: a comparative study of post-abortion care in Bolivia and Mexico. Soc Sci Med (1982). 2007;64:2210–22.
Tran NT, Yameogo WME, Langwana F, Gaffield ME, Seuc A, Cuzin-Kihl A, et al. Participatory action research to identify a package of interventions to promote postpartum family planning in Burkina Faso and the democratic republic of Congo. BMC Women’s Health. 2018;18(MEDLINE:29976182, 1):122.
Kestler E, Valencia L, Del Valle V, Silva A. Scaling up post-abortion care in guatemala: Initial successes at national level. Reprod Health Matters. 2006;14:138–47.
Sebastian MP, Khan ME, Kumari K, Idnani R. Increasing postpartum contraception in rural India: evaluation of a community-based behavior change communication intervention. Int Perspect Sex Reprod Health. 2012;38:68–77.
Nelson AR, Cooper CM, Kamara S, Taylor ND, Zikeh T, Kanneh-Kesselly C, et al. Operationalizing integrated immunization and family planning services in rural Liberia: lessons learned from evaluating service quality and utilization. Global Health Sci Pract. 2019;7:418–34.
Saeed GA, Fakhar S, Rahim F, Tabassum S. Change in trend of contraceptive uptake–effect of educational leaflets and counseling. Contraception. 2008;77:377–81.
Akman M, Tüzün S, Uzuner A, Başgul A, Kavak Z. The influence of prenatal counselling on postpartum contraceptive choice. J Int Med Res. 2010;38:1243–9.
Belaid L, Dumont A, Chaillet N, Zertal A, De Brouwere V, Hounton S, et al. Effectiveness of demand generation interventions on use of modern contraceptives in low- and middle-income countries. Trop Med Int Health. 2016;21:1240–54.
Bongaarts J. The impact of family planning programs on unmet need and demand for contraception. Stud Fam Plann. 2014;45:247–62.
SebertKuhlmann A, Gavin L, Galavotti C. The integration of family planning with other health services: a literature review. Int Perspect Sex Reprod Health. 2010;36(04):189–96. https://doi.org/10.1363/3618910.
Sferrazza C, editor. Family planning, women’s empowerment, and population and societal impacts. National Academies Press; 2021. Available from: https://doi.org/10.17226/26023.
Acknowledgements
Not applicable
Consortium Name: Family Planning Research Collaborators
Ashraf Nabhan1, Rita Kabra2, Nahed Allam3, Eman Ibrahim3, Norhan Abdelmonem4, Nouran Wagih5, Nourhan Mostafa5, James Kiarie2, Ahmed Zenhom1, Alyaa Ashraf5, Amal Alshabrawy1, Emry Atwa5, Fatma Elghamry5, Mai Abouelnaga5, Mariam Kodsy5, Marwa Elgendi1, Marwa Snosi 1, Menna Kamel5, Mohamed Salama1, Nada Makram5, Noha Sakna1, Salma Eltayeb5, Samhaa bahnasy5, Sara Galal5, Shorouk Taha5.
Funding
This work received funding from the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored program executed by the World Health Organization (WHO) (WHO-SRH/HRP-CFC grant number 2022/1240770–0).
Author information
Authors and Affiliations
Consortia
Contributions
AN, RK, JK conceived the idea for this review and designed the systematic review methods. AN, RK, NA, EI, NAE, NW, NM, JK collaborated in conducting the review. All authors (members of the Consortium “Family Planning Research Collaborators”) collaborated in screening of studies and data extraction and the evidence synthesis. AN, RK, JK collaborated in writing the first draft of this review. All authors provided critical input to the final manuscript. All authors read and approved the final manuscript. The authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policy, or views of the World Health Organization.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary File 1. The SURE Framework. Supplementary File 2. Data extraction form: Scaling up post pregnancy FP. Supplementary File 3. Mixed Methods Appraisal Tool (MMAT).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nabhan, A., Kabra, R., Allam, N. et al. Implementation strategies, facilitators, and barriers to scaling up and sustaining post pregnancy family planning, a mixed-methods systematic review. BMC Women's Health 23, 379 (2023). https://doi.org/10.1186/s12905-023-02518-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02518-6