Abstract
Background
The aim of this retrospective study was to investigate whether oral antibiotics (doxycycline and metronidazole) combined with intrauterine perfusion (gentamicin and dexamethasone) are beneficial for patients with repeated implantation failure (RIF) and chronic endometritis (CE) to improve clinical pregnancy outcomes.
Methods
Patients with RIF and CE were diagnosed using hysteroscopy and histology together. A total of 42 patients were enrolled in the study. All patients received oral antibiotics (doxycycline combined with metronidazole) and 22 patients underwent intrauterine perfusion (gentamicin combined with dexamethasone) immediately after the end of oral antibiotic therapy. Pregnancy outcomes were evaluated during the first in vitro fertilization (IVF) and embryo transfer (ET) cycle.
Results
For the first D3 ET after treatment with oral antibiotics (doxycycline and metronidazole) combined with intrauterine perfusion (gentamicin and dexamethasone), higher embryo implantation rate (30.95% vs. 26.67%, P = 0.0308), clinical pregnancy rate (30% vs. 50%, P < 0.001), live birth rate (33.33% vs. 45.45%, P < 0.0001). No fetal malformations or ectopic pregnancies were observed.
Conclusion
We report oral antibiotics (doxycycline and metronidazole) combined with intrauterine perfusion (gentamicin and dexamethasone) as a novel treatment for CE to improve the outcomes of successful pregnancy compared with those of oral antibiotics alone.
Similar content being viewed by others
Background
Repeated implantation failure (RIF) is defined as the inability to conceive following 3 or more consecutive embryo transfer cycles and each cycle transfer 1 ~ 2 high-quality embryos [1,2,3] and affects 12%–46% of patients experiencing infertility [3], which have caused great psychological distress to women [4]. RIF can result from a variety of causes, such as anomalies in the uterine cavity, endometrial non-receptivity, immunological factors, and developmental origins [3, 5]. Over recent years, an expanding body of research has shown that less receptive endometrium caused by local immune dysregulation may be the main cause of RIF [6].
Chronic endometritis (CE), which cannot be diagnosed using ultrasound and hysterosalpingography (HSG), is a chronic inflammatory condition of the endometrium without clear clinical signs. Immunohistochemistry has revealed the presence of plasma cells in the endometrial stroma. In the endometrium, CE generates an aberrant immunological milieu that results in the generation of abnormal levels of inflammatory mediators [7]. This decreases the endometrial capacity to receive embryos, which prevents implantation.
Diagnosis of CE is complicated and difficult. Currently, there are no universal diagnostic methods for endometritis. On hysteroscopy (HSC) [8], local endometrial redness and local or diffuse endometrial congestion are seen as "strawberry signs” in addition to endometrial interstitial edema, a pale and convex surface, and multiple tiny polyps. The identification of CD138 + cells by histopathology after curettage is considered a simple and objective method [9]. Among the many methods, five plasma cells per high-power field (HPF) is the most reliable method [10]. Intrauterine microbial detection can also be used as an auxiliary method, which is more complex to operate and has many factors that affect the results. In our study, we referred to hysteroscopic and histopathological findings to diagnose CE [11].
CE treatment involves administration of various antibiotics [10], and doxycycline combined with metronidazole is considered effective [12]. Doxycycline is a broad-spectrum antibiotic that is effective against both Gram-positive and Gram-negative bacteria, while metronidazole is a broad-spectrum anti-anaerobic bacteria drug that shows good effects against most bacilli. While oral antibiotics are mainly used to treat CE, improvements in pregnancy outcomes are not evident [13,14,15]. In a previous study [16] of patients with RIF, one group received doxycycline combined with metronidazole orally and the other group received a ciprofloxacin intrauterine infusion based on oral medication. After subsequent in vitro fertilization and embryo transfer (IVF-ET), there were no differences in embryo implantation rates, clinical pregnancy rates, or live birth rates between the two groups.
Other treatments have been investigated to achieve better results. Intrauterine administration is considered an effective method for the treatment of intrauterine diseases because of its rapid onset of action and high local drug concentrations. Antibiotic therapy in combination with platelet-rich plasma(PRP) is said to improve pregnancy outcomes in these patients, but the procedure has some limitations because it is a blood product and carries the risk of infection [17]. A recent study showed that intrauterine antibiotic infusions led to successful pregnancies in three patients with CE, for whom IVF had previously failed [15]. Oral doxycycline combined with the local administration of antibiotics can significantly improve implantation and pregnancy rates, and the effect is better than that of oral antibiotics alone [16, 18]. Another study showed that intrauterine administration of dexamethasone successfully improved endometrial receptivity. Gentamicin, the main drug used in the treatment of endometritis, is cheap and effective and has been widely used in obstetrics and gynecology [19]. Therefore, doxycycline combined with antibiotics and dexamethasone for the treatment of CE is feasible and worthy of further investigation.
In this study, we used doxycycline combined with intrauterine perfusion (gentamicin and dexamethasone) to further investigate whether this combination improves pregnancy outcomes, compared with oral administration of antibiotics alone, to find a new alternative method for the treatment of CE and to provide a new perspective for the treatment of RIF.
Methods
Inclusion population
We retrospectively analyzed patients who visited the reproductive centers of The First Affiliated Hospital of Guangxi Medical University between July 2019 and June 2021. All agreed and signed the informed consent form. Our screening included thyroid function and antibody testing as well as evaluation of the uterine cavity using ultrasound. During infertility evaluation, ultrasonography was performed to assess uterine anatomy and exclude those with abnormal uterine morphology.
We included women who underwent HSC and biopsy, were aged < 40 years, and had a body mass index (BMI) between 18 and 30 kg/m2. We excluded those with factors affecting pregnancy outcomes, such as parental chromosomal abnormalities, antiphospholipid syndrome, severe thyroid dysfunction, and autoimmune disease. All patients underwent at least three ETs with good-quality embryos (grade A), and none became pregnant. HSC was performed to clarify the cause, and a small amount of tissue was scraped for pathological examination.
Diagnosis and histological evaluation of CE
We used a cervical vaginal swab to rule out Chlamydia trachomatis and Neisseria gonorrhoeae infection before HSC. In the late follicular phase, we performed HSC and biopsy in the office without anesthetic. We photographed the uterine lumen and endometrium (Fig. 1A and B). After the intrauterine HSC inspection, we used a tiny scraping spoon to gently scrape the endometrium three times in the biopsy group. Endometrial tissue was stored in a 10% formaldehyde solution.
Hysteroscopy, HE staining, and immunohistochemical CD138 staining were used to compare images of patients with and without CE (× 200 magnification). Hysteroscopy (A. B), HE (C. D), and CD138 immunohistochemistry (E. F) were used to compare the normal endometrium (A. C. E) with that affected by chronic endometritis (B. D. F). CE, chronic endometritis; HE, hematoxylin–eosin; HSC, hysteroscopy
After paraffin embedding, serial sections with a heat treatment of 95 °C for 20 min on tissues with a thickness of 3 µm. After gradient deparaffinization and dehydration, the samples were stained with hematoxylin and eosin (HE) according to the routine protocol to distinguish the interstitial part. A dilution of 500 µL was incubated with antibodies against CD138 (Protech, Wuhan) for 1 h for simultaneous DAB coloration, and CD138 + appeared as yellow or brown-yellow particles in the interstitium. We used immunohistochemistry to diagnose CE as previously described and assessed ≥ 5 plasma cells per HPF at × 400 magnification [11] (Fig. 1 C-F).
Therapy for CE
Immunohistochemistry and HSC were used to diagnose CE in women. In cases of CE, patients received antibiotic treatment according to the French recommendations for pelvic inflammatory diseases [20, 12]. Oral antibiotics administered for CE treatment included doxycycline combined with metronidazole. Doxycycline (100 mg) was administered twice daily for 14 days. During the same period, metronidazole (400 mg) was also administered twice daily. Investigators were informed and agreed to the assigned treatment and the associated advantages and disadvantages. After oral doxycycline treatment, 22 patients were injected with a mixture of gentamicin (80 mg), dexamethasone (5 mg), and 0.9% normal saline (3 mL) into the intrauterine cavity using a sterile thin, soft tube(Fig. 2). All patients underwent re-endometrial biopsies at the end of treatment and were negative for CD138.
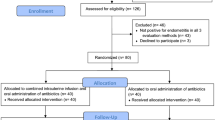
Flow of the treatment plan. Outline of the duration of treatment for each study group. During the first 14 days of treatment, all patients received oral therapy twice daily. After the oral course, the patients in the combination group received intrauterine fluid only once. All patients underwent D3 cleavage stage transplantation during the next menstrual cycle
Fertility treatment
Pregnancy outcomes were evaluated only for the first ET after the treatment. Embryos were usually transferred within 3 months following the end of treatment. An IVF procedure identical to the previous procedure was used. Agonist or antagonist regimens were used throughout the IVF treatment cycles, which were either natural or conventional gonadotropin-stimulated. We followed the usual protocol for endometrial preparation. In view of the fact that frozen embryo transplantation does not increase the incidence of neonatal complications and even has a better cognitive function on the nervous system [21], all patients were treated with frozen embryo transplantation after CE treatment. The cleavage stage was used to transfer all of the embryos (D3). After ET, progesterone was routinely supplemented until 12 weeks of gestation.
The following outcome indicators were observed: embryo implantation rate, clinical pregnancy rate, early abortion rate, live birth rate, and occurrence of fetal malformations.
Statistical analysis
Comparing categorical variables, such as specific clinical traits, implantation rates, clinical pregnancy rates, live birth rates, and clinical attrition rates, was performed using chi-square testing. A t-test was used to evaluate continuous variables. SPSS 17.0 (International Business Machines Corporation, USA) was used to perform statistical analyses. At P < 0.05, any bidirectional P-value was deemed statistically significant.
Results
Diagnosis and treatment of patients with CE
A flowchart of the study is shown in Fig. 3. After excluding those who were not associated with pregnancy and those who did not undergo HSC examination or had pathological evidence of CD138 in fewer than five cells per HPF, 88 patients with a diagnosis of RIF/CE were screened between July 2019 and June 2021. All patients underwent hysteroscopy and pathology twice, qualified for inclusion and turned negative for CD138 after treatment. After the simple screening, six cases were complicated with autoimmune diseases, such as systemic lupus erythematosus, Sjogren's syndrome, and antiphospholipid syndrome, while nine were excluded due to adenomyosis, intrauterine adhesions, and uterine malformations. Additionally, 12 patients were aged either > 40 years or < 18 years. We excluded those who had not had an embryo transplant within 3 months or had no transferable dominant embryos or other treatment. A final total of 42 patients participated in this study. These patients met the following criteria: history of three failed embryo implantations, suspected CE on HSC (strawberry appearance), endometrial edema, endometrial irregularity, hyperemic areas with marked white spots (Fig. 3), and pathological diagnosis of CD138 in five or more cells per HPF. All patients received doxycycline combined with metronidazole orally. Among these, 22 patients underwent uterine perfusion with gentamicin and dexamethasone immediately after the end of oral antibiotic administration. All patients underwent IVF-ET within 3 months following the end of treatment.
Population characteristics
The main clinical characteristics of the patients included in our study are shown in Table 1. Ovarian stimulation and ET were successfully performed in all cases using IVF-ET cycles within 3 months of treatment. We only collected results of the first ET after treatment. There were no significant differences in levels of anti-mullerian hormone (AMH), follicle-stimulating hormone (FSH), and estrogen (E2) levels or age, BMI, and infertility years between the two groups (P > 0.05).
Embryo implantation rate
The embryo implantation rate, which represents the transfer of gestational sacs/embryos, is an important indicator for evaluating patients with RIF. One of the main reasons for RIF is the change in endometrial receptivity, and an increase in implantation rate indicates a change in endometrial receptivity. In our study, the incidence of implantation was significantly greater in individuals who received oral antibiotics combined with intrauterine infusion than those who received oral antibiotics alone (30.95% vs. 26.67%, P = 0.0308, Table 2).
Pregnancy outcomes
The ultimate goals of all treatments are to improve pregnancy outcomes, increase live birth rates, and reduce abortion rates. We observed a higher clinical pregnancy rate (30% vs. 50%, P < 0.001), continuous pregnancy rate (33.33% vs. 45.45%, P < 0.0001), and live birth rate (33.33% vs. 45.45%, P < 0.0001) (Table 3). We also observed a statistically significant decrease in the rate of early pregnancy loss (6.667% vs. 4.545%, P = 0.0068) in the combination group compared with the oral administration group (Table 3). As for the statistics of early pregnancy loss, since there is only one case in each group, strictly speaking, the data cannot represent the difference in statistical rates, so it is necessary to expand the sample size and continue the statistics. We did not observe any ectopic pregnancies, fetal malformations, or preterm births with either treatment.
Discussion
RIF, which directly affects the pregnancy rate, is a difficult problem for reproductive doctors. In recent years, researchers have made significant efforts to study the pathogenesis and treatment of RIF with little success. Recent studies suggest that endometrial immune disorders may lead to immune cell abnormalities, involving natural killer (NK) cells, macrophages, regulatory T cells (Tregs), and other functional abnormalities, leading to maternal–fetal immune disorders and embryo implantation disorders [22]. The use of immunosuppressants, including intravenous immunoglobulin [23], intrauterine infusion of peripheral blood mononuclear cells [24], tacrolimus [25], subcutaneous administration of granulocyte colony-stimulating factor [26], and prednisone [27], have also been shown to improvement RIF and enhance the receptivity of the endometrium and improve the success rate of pregnancy. Scientists are even combining knowledge with computer science through machine learning algorithms, using artificial intelligence (AI) tools to analyze information about RIF patients and embryos to predict pregnancy outcomes [28]. In the near future, it may even be possible to use Artificial Womb Technology (AWT) to solve pregnancy problems in such patients [29].
Endometritis is an unsolved problem today. It is a significant contributor to repeated implant failures and other fertility problems. The clinical symptoms of endometritis are often mild and easily ignored. Endometritis is a complicated disease. First of all, the diagnostic methods and diagnostic criteria of endometritis are not uniform. Secondly, the treatment of endometritis is mainly empirical, the therapeutic effect is not ideal and easy to produce drug resistance. Finally, it is difficult to have a non-invasive way to check the effect of treatment after treatment.
Dexamethasone, a glucocorticoid, has powerful immunomodulatory effects. Zhang [18] administered an intrauterine infusion of dexamethasone to eight patients with RIF and found that the proportion of NK cells was downregulated in samples taken by endometrial biopsy. Seven patients successfully became pregnant after cryopreserved ET. Three patients delivered healthy babies at term without any pregnancy complications, suggesting that prednisone can downregulate the proportion of NK cells, improve endometrial receptivity, and promote embryo implantation. Huang [30] treated patients with RIF using prednisone and found that the proportion of Tregs and IL-10, which are indicators of immune tolerance, was significantly increased, whereas IL-17A, IL-23, and other proinflammatory factors were significantly decreased. After treatment, five patients with RIF successfully became pregnant and four had live births (n = 19). It has been suggested that prednisone can improve local immunity and place the endometrium in a sensitive phase, which is beneficial for embryo implantation.
In a study of patients with RIF, Kotaro [31] found that 33.7% of women with RIF infertility were diagnosed with CE. In a 10-year study of patients with RIF, Kotaro [32] also found that 31.4% of the women concurrently had CE and 7.8% of women with RIF had multi-drug-resistant CE, with a steady increase in multi-drug resistance (odds ratio [OR], 8.27; 95% confidence interval [CI], 2.58–26.43; P < 0.001). Therefore, a more effective method may be required to treat CE. Intrauterine perfusion can enable the drug to directly act more locally, quickly, and with a high concentration to reduce systemic adverse reactions. Intrauterine perfusion is a commonly used treatment in obstetrics and gynecology, and it is the first-line treatment for endometritis during labor [32], with high levels of safety and effectiveness. In animal experiments, intrauterine infusion of gentamicin and dexamethasone in buffaloes with endometritis was shown to significantly increase the number of pregnancies [32]. Zhang [18] treated patients with RIF/CE using an intrauterine infusion of dexamethasone combined with gentamicin/clindamycin, with a 60% cure rate of CE, indicating that gentamicin has good therapeutic effect on CE. The clinical pregnancy and live birth rates of patients with treated RIF/CE were increased after cryo-ET, not only because of the therapeutic effect of gentamicin on CE but also because dexamethasone treatment can increase endometrial embryo acceptance and improve pregnancy outcomes. Therefore, we believe that oral doxycycline and metronidazole combined with an intrauterine infusion of gentamicin and dexamethasone may achieve an improved therapeutic effect.
In our study, we retrospectively analyzed patients with RIF/CE between July 2019 and June 2021. After oral doxycycline and metronidazole administration, patients were administered an intrauterine infusion of gentamicin and dexamethasone, and pregnancy outcomes were observed after ET. Our findings support that oral antibiotics combined with an intrauterine infusion of antibiotics have a better effect on pregnancy outcomes than do oral antibiotics alone and can improve implantation rate, clinical pregnancy rate, and live birth rate (all P < 0.05).
Our inclusion requirements are quite tight, which is why we only have a tiny number of examples. Another important factor was that we did not include these patients who did not have their CD138 levels checked again or who did not have two standardized hysteroscopies. Because the patients we included were retransplanted after RIF, and some of the patients had no optimal embryo, we had no way to evaluate the effectiveness of the method. Further decreasing the number of instances we considered was the fact that some patients were also not included in other therapies.
To assess the effect of antibiotic treatment on CE and the integrity of the study, we initially planned to include women with RIF/CE and either placebo or no treatment in the control group. However, we would not find patients in the hospital who were diagnosed with RIF/CE and did not receive any treatment, it's not ethical. We also excluded patients who were treated with other regiments. Given the large number of reports on the efficacy of oral antibiotics (doxycycline and metronidazole) in the treatment of CE, we compared whether oral antibiotics combined with an intrauterine infusion of antibiotics were more effective than oral antibiotics alone.
Conclusion
In conclusion, our results show that the use of oral antibiotics (doxycycline and metronidazole) combined with intrauterine perfusion (gentamicin and dexamethasone) are beneficial for patients with RIF/CE. When D3 cleavage were transplanted, the combination group showed higher implantation, clinical pregnancy, and live birth rates. These drugs are widely used in the fields of obstetrics and gynecology and have no teratogenic effect. We plan to conduct further animal experiments to elucidate the specific molecular mechanisms.
Availability of data and materials
All the data and materials were obtained from the First Affiliated Hospital of Guangxi Medical University, and the data were real and reliable. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Coughlan C, Ledger W, Wang Q, Liu F, Demirol A, Gurgan T, et al. Recurrent implantation failure: definition and management. Reprod Biomed Online. 2014;28(1):14–38.
Polanski LT, Baumgarten MN, Quenby S, Brosens J, Campbell BK, Raine-Fenning NJ. What exactly do we mean by “recurrent implantation failure”? A systematic review and opinion. Reprod Biomed Online. 2014;28(4):409–23.
Somigliana E, Vigano P, Busnelli A, Paffoni A, Vegetti W, Vercellini P. Repeated implantation failure at the crossroad between statistics, clinics and over-diagnosis. Reprod Biomed Online. 2018;36(1):32–8.
Burgio S, Polizzi C, Buzzaccarini G, Laganà AS, Gullo G, Perricone G, et al. Psychological variables in medically assisted reproduction: a systematic review. Prz Menopauzalny. 2022;21(1):47–63.
Sheikhansari G, Pourmoghadam Z, Danaii S, Mehdizadeh A, Yousefi M. Etiology and management of recurrent implantation failure: a focus on intra-uterine PBMC-therapy for RIF. J Reprod Immunol. 2020;139:103121.
Saxtorph MH, Hallager T, Persson G, Petersen KB, Eriksen JO, Larsen LG, et al. Assessing endometrial receptivity after recurrent implantation failure: a prospective controlled cohort study. Reprod Biomed Online. 2020;41(6):998–1006.
Li Y, Yu S, Huang C, Lian R, Chen C, Liu S, et al. Evaluation of peripheral and uterine immune status of chronic endometritis in patients with recurrent reproductive failure. Fertil Steril. 2020;113(1):187-196.e1.
Gkrozou F, Tsonis O, Dimitriou E, Paschopoulos M. In women with chronic or subclinical endometritis is hysteroscopy suitable for setting the diagnosis? A systematic review. J Obstet Gynaecol Res. 2020;46(9):1639–50.
Herlihy NS, Klimczak AM, Titus S, Scott C, Hanson BM, Kim JK, et al. The role of endometrial staining for CD138 as a marker of chronic endometritis in predicting live birth. J Assist Reprod Genet. 2022;39(2):473–9.
Cheng X, Huang Z, Xiao Z, Bai Y. Does antibiotic therapy for chronic endometritis improve clinical outcomes of patients with recurrent implantation failure in subsequent IVF cycles? A systematic review and meta-analysis. J Assist Reprod Genet. 2022;39(8):1797–813.
Zargar M, Ghafourian M, Nikbakht R, Mir Hosseini V, MoradiChoghakabodi P. Evaluating Chronic Endometritis in Women with Recurrent Implantation Failure and Recurrent Pregnancy Loss by Hysteroscopy and Immunohistochemistry. J Minim Invasive Gynecol. 2020;27(1):116–21.
Gay C, Hamdaoui N, Pauly V, Rojat Habib MC, Djemli A, Carmassi M, et al. Impact of antibiotic treatment for chronic endometritis on unexplained recurrent pregnancy loss. J Gynecol Obstet Hum Reprod. 2021;50(5):102034.
Vitagliano A, Saccardi C, Noventa M, DispiezioSardo A, Saccone G, Cicinelli E, et al. Effects of chronic endometritis therapy on in vitro fertilization outcome in women with repeated implantation failure: a systematic review and meta-analysis. Fertil Steril. 2018;110(1):103–1121.
Xiong Y, Chen Q, Chen C, Tan J, Wang Z, Gu F, et al. Impact of oral antibiotic treatment for chronic endometritis on pregnancy outcomes in the following frozen-thawed embryo transfer cycles of infertile women: a cohort study of 640 embryo transfer cycles. Fertil Steril. 2021;116(2):413–21.
Cicinelli E, Cicinelli R, Vitagliano A. Antibiotic therapy for chronic endometritis and its reproductive implications: a step forward, with some uncertainties. Fertil Steril. 2021;115(6):1445–6.
Pantos K, Simopoulou M, Maziotis E, Rapani A, Grigoriadis S, Tsioulou P, et al. Introducing intrauterine antibiotic infusion as a novel approach in effectively treating chronic endometritis and restoring reproductive dynamics: a randomized pilot study. Sci Rep. 2021;11(1):15581.
Li J, Li X, Ding J, Zhao J, Chen J, Guan F, et al. Analysis of pregnancy outcomes in patients with recurrent implantation failure complicated with chronic endometritis. Front Cell Dev Biol. 2023;11:1088586.
Zhang Y, Xu H, Liu Y, Zheng S, Zhao W, Wu D, et al. Confirmation of chronic endometritis in repeated implantation failure and success outcome in IVF-ET after intrauterine delivery of the combined administration of antibiotic and dexamethasone. Am J Reprod Immunol. 2019;82(5):e13177.
Chen LY, Harnod T, Chang YH, Chen H, Ding DC. The Combination of Clindamycin and Gentamicin Is Adequate for Pelvic Inflammatory Disease: A Retrospective Cohort Study. J Clin Med. 2021;10(18):4145.
Charvériat A, Fritel X. Diagnosis of pelvic inflammatory disease: Clinical, paraclinical, imaging and laparoscopy criteria. CNGOF and SPILF Pelvic Inflammatory Diseases Guidelines. Gynecol Obstet Fertil Senol. 2019;47(5):404–8.
Gullo G, Scaglione M, Cucinella G, Chiantera V, Perino A, Greco ME, et al. Neonatal Outcomes and Long-Term Follow-Up of Children Born from Frozen Embryo, a Narrative Review of Latest Research Findings. Medicina (Kaunas). 2022;58(9):1218.
Zeng S, Liu X, Liu D, Song W. Research update for the immune microenvironment of chronic endometritis. J Reprod Immunol. 2022;152:103637.
Ho YK, Chen HH, Huang CC, Lee CI, Lin PY, Lee MS, et al. Peripheral CD56(+)CD16(+) NK Cell Populations in the Early Follicular Phase Are Associated With Successful Clinical Outcomes of Intravenous Immunoglobulin Treatment in Women With Repeated Implantation Failure. Front Endocrinol (Lausanne). 2019;10:937.
Pourmoghadam Z, Soltani-Zangbar MS, Sheikhansari G, Azizi R, Eghbal-Fard S, Mohammadi H, et al. Intrauterine administration of autologous hCG- activated peripheral blood mononuclear cells improves pregnancy outcomes in patients with recurrent implantation failure; a double-blind, randomized control trial study. J Reprod Immunol. 2020;142:103182.
Nakagawa K, Kwak-Kim J, Kuroda K, Sugiyama R and Yamaguchi K. Immunosuppressive treatment using tacrolimus promotes pregnancy outcome in infertile women with repeated implantation failures. Am J Reprod Immunol. 2017;78(3). https://doi.org/10.1111/aji.12682.
Kamath MS, Kirubakaran R, Sunkara SK. Granulocyte-colony stimulating factor administration for subfertile women undergoing assisted reproduction. Cochrane Database Syst Rev. 2020;1(1):Cd013226.
Sung N, Khan SA, Yiu ME, Jubiz G, Salazar MD, Skariah A, et al. Reproductive outcomes of women with recurrent pregnancy losses and repeated implantation failures are significantly improved with immunomodulatory treatment. J Reprod Immunol. 2021;148:103369.
Medenica S, Zivanovic D, Batkoska L, Marinelli S, Basile G, Perino A, et al. The future is coming: artificial intelligence in the treatment of infertility could improve assisted reproduction outcomes-the value of regulatory frameworks. Diagnostics (Basel). 2022;12(12):2979.
Zaami S, Gullo G, Varone MC, UmaniRonchi F, Montanari Vergallo G. From the maternal uterus to the “uterus device”? Ethical and scientific considerations on partial ectogenesis. Eur Rev Med Pharmacol Sci. 2021;25(23):7354–62.
Huang Q, Wu H, Li M, Yang Y, Fu X. Prednisone improves pregnancy outcome in repeated implantation failure by enhance regulatory T cells bias. J Reprod Immunol. 2021;143:103245.
Kitaya K, Matsubayashi H, Takaya Y, Nishiyama R, Yamaguchi K, Takeuchi T, et al., Live birth rate following oral antibiotic treatment for chronic endometritis in infertile women with repeated implantation failure. Am J Reprod Immunol. 2017;78(5). https://doi.org/10.1111/aji.12719.
Kitaya K, Tanaka SE, Sakuraba Y, Ishikawa T. Multi-drug-resistant chronic endometritis in infertile women with repeated implantation failure: trend over the decade and pilot study for third-line oral antibiotic treatment. J Assist Reprod Genet. 2022;39(8):1839–48.
Acknowledgements
We would like to thank the staff of the Department of Pathology at the First Affiliated Hospital of Guangxi Medical University for their help with this project.
Funding
This work was supported by grants from the National Natural Science Foundation of China (NO. 81960280) and Guangxi Health Commission Research Project (Grand No.Z2013046).
Author information
Authors and Affiliations
Contributions
A.Q., F. H. designed the study. N. M., J. L. drafted the first version of the manuscript. J.W. and Y.J. collect all clinical informed consent forms and pictures. J. Z., W. Q. contributed to data analysis and interpretation. All authors revised the manuscript and approved the final submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Our research was carried out in accordance with the Declaration of Helsinki. The Ethical approval for the study was received by the Institutional review board of The First Affiliated Hospital of Guangxi Medical University( reference number 2022-E327-01).
All patients provided written informed consent.
Consent for publication
Not applicable.
Competing of interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, N., Li, J., Zhang, J. et al. Combined oral antibiotics and intrauterine perfusion can improve in vitro fertilization and embryo transfer pregnancy outcomes in patients with chronic endometritis and repeated embryo implantation failure. BMC Women's Health 23, 344 (2023). https://doi.org/10.1186/s12905-023-02443-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02443-8