Abstract
Background
Over the past decade, Morocco has increasingly become the chosen destination for a growing number of migrants from neighbouring countries and especially from Sub-Saharan Africa. The aim of this study is to describe the sexual and reproductive health (SRH), as well as sexual and gender-based violence (SGBV) among female migrants in Morocco.
Methods
This is a descriptive cross-sectional study conducted between July and December 2021. Female migrants were recruited from one university maternity hospital and two primary healthcare centres in Rabat. Data were collected using a structured face-to-face questionnaire, which included information about sociodemographic characteristics, SRH, history of SGBV and its impact, as well as the utilization of preventive and supportive SGBV services.
Results
A total of 151 participants were included in this study. The majority of participants (60.9%) were aged 18 to 34 years old and 83.3% were single. Many participants (62.1%) did not use contraceptives. More than half (56%) of the participants who were pregnant at the time of the study were receiving pre-natal care. About 29.9% of interviewed participants reported experiencing female genital mutilation, and a significant majority (87.4%) experienced SGBV at least once during their lifetimes, while 76.2% experienced SGBV during migration. The most commonly reported form of violence was verbal abuse (75.8%). Among the victims of SGBV, a minority have visited a health facility (7%) or filed a complaint (9%) in the aftermath of violence.
Conclusion
Overall, our findings showed low contraception coverage, moderate access to prenatal care, high prevalence of SGBV, and low utilization of preventive and supportive SGBV services among migrant women in Morocco. Further studies are needed to understand the contextual barriers to access, and utilization of SRH care and additional efforts should be undertaken to strengthen SGBV prevention and support systems.
Similar content being viewed by others
Introduction
Migration has become a pervasive global phenomenon over the past decade [1]. According to the International Organization of Migrants (IOM), there were 281 million migrants in the world in 2020, which make up 3.6 per cent of the global population [1]. Migrants often come from countries where they experienced political instability, economic austerity, and structural violence [2]. Concurrently, migrants experience additional hardships during their migration pathway or in the host country, such as marginalization, discrimination, violence in all forms, abuse and exploitation [2]. Consequently, the migrant population often has poor social, economic, psychological and health outcomes, making migration a troubling global human rights and public health issue [3]. In fact, a robust body of evidence shows that migrants are disproportionately affected by mental health conditions, chronic diseases, antimicrobial resistance, occupational hazards, and oral diseases compared to the host population [4,5,6,7]. Additionally, migrants have been shown to have lower immunization rates compared to the host populations [8]. Furthermore, migrants, especially women and girls, – often experience poor sexual and reproductive health (SRH) outcomes such as low skilled-birth attendance [9], unintended pregnancies and abortion [10], inadequate pre-natal care [11] and low contraception coverage [12].
SGBV is a global phenomenon which affects an estimated 30% of ever-married or partnered women aged between 15 and 49 years old worldwide [13]. In the Eastern Mediterranean Region, 31% of ever partnered women experienced physical and/or sexual intimate partner violence during the course of their lives [14]. SGBV results in poor SRH and mental health outcomes among the victims [15]. In fact, according to the World Health Organization (WHO), women who have been physically or sexually abused are more likely to experience unintended pregnancies, gynecological morbidities, miscarriages, unsafe abortions, pregnancy complications and sexually-transmitted infections including HIV [15]. Consequently, the 70th World Health Assembly resolution stressed the importance of a multisectoral national response to interpersonal violence, particularly against women, girls and children, and endorsed a Global Plan of Action to strengthen the role of the health system in spearheading this endeavour [16]. Migrant women and girls are often more vulnerable to SGBV given the harsh migration journey and the difficult socio-economic conditions they experience in the host countries [2].
The number of migrants has been growing over the past decade in Morocco, the chosen country of destination for migrants from neighbouring countries, especially Sub-Saharan Africa [17]. The International Organization for Migration estimates that Morocco was home to 102 thousand migrants as of 2021, of which half were female [1]. Based on a national survey of 3000 migrants and refugees in Morocco, conducted by the High Commission of Planning (HCP) in 2021, the Democratic Republic of the Congo (DRC) (19.1%), Ivory coast (16.7%), Senegal (15.9%) and Guinea (13.2%) were the main countries of origin of migrants in Morocco [17]. Two consecutive mass regularization campaigns in 2014 and 2017 resulted in the regularization of almost 50,000 migrants including unaccompanied minors and more than 10,000 women [17]. Several efforts geared towards improving the living conditions of migrants and their access to public services have been undertaken by the Moroccan government, such as the adoption of the Global Compact for Safe, Orderly and Regular Migration in 2018[18] and the implementation of the National Strategy for Immigration and Asylum [19]. Moreover, the Moroccan Ministry of Health and Social Protection has been engaged, in collaboration with civil society and non-governmental organizations (CSOs/NGOs), in a participatory process aimed at improving access to healthcare services by the migrant population. In 2017, a circular was signed by the Minister Delegate to the Minister of the Interior, the Minister in charge of Moroccans residing abroad, the Minister in charge of Economy and Finance, and the Minister of Health, that provides documented migrants and refugees with access to multiple healthcare services under the Moroccan Health Insurance Scheme for the Economically Deprived (RAMED) [20]. With support from the IOM, the Ministry of Health also developed the National Strategic Plan for Health and Immigration (PSNSI) which covers the period 2021–2025 with the aim of improving access to health among migrants through an integrated and comprehensive approach [20]. The PSNSI identified the following areas of focus: strengthening monitoring, evaluation and research; building the capacity of different actors involved in promoting the health of migrants; the promotion of health and preventive care; provision of adequate care and good governance [20]. Regular migrants in Morocco have the right to access free of charge emergency care and could benefit from healthcare services in a wide network of primary healthcare facilities across the country. In addition, migrants are included in national vertical programs put in place by the Ministry of Health such as Family Planning, Maternal and Child Health and Reproductive health care programs [21]. The 2018, the Ministry of Health with help from NGOs, organized a national two-month TB screening campaign with Morocco’s migration organization partners. During this campaign, 5,553 migrants were tested for HIV, and 12,013 migrants received information on HIV prevention [22]. In addition, a winter school on Sexual and Reproductive Health Rights (SRHR) was organized by the Ministry of Health in collaboration with IOM in order to improve knowledge of SRH among migrants in Morocco. Moreover, several interventions aimed at improving the cultural competency of healthcare professionals have been implemented and a toolkit was developed to increase healthcare professionals’ sensitivity to migrant health issues [23]. Nevertheless, the utilization of healthcare services by migrants in Morocco remains insufficient due to several contextual and structural barriers such as language and cultural barriers, the lack of culturally-competent healthcare professionals and the lack of information on healthcare services [21]. In Morocco, data on the SRH outcomes of migrant women remains scarce, and very few studies have explored migrant women’s exposure to SGBV. In 2021, around 11.7% of migrant women in Morocco experienced physical or psychological violence, 17.7% have been victims of forced sexual intercourse or sexual harassment and 4.3% were pregnant or gave birth during their travel [17]. NGOs and CSOs in Morocco undertake tremendous efforts to provide psychological support to victims of SGBV including migrants. However, the utilization of SGBV prevention and support services psychosocial by migrants has not been the subject of previous research. The aim of this study is to describe the SRH as well as the experiences of SGBV among female migrant population in Morocco. The findings of this study will be useful to identify areas for improvement with regards to access and utilization of SRH and SGBV prevention and support services by the migrant population in Morocco.
Materials and methods
Study design
This is a descriptive cross-sectional study conducted between July and December 2021 in Rabat, Morocco.
Study population
Female migrants were recruited from one maternity university hospital (Les Orangers Maternity Hospital) and two primary healthcare centres in Rabat. The healthcare facilities in Rabat were selected due to the high influx of migrants. The inclusion criteria were being a migrant woman, regardless of legal status, aged 18 years old and over and having benefited from a medical consultation regarding SRH in one of the selected healthcare facilities. Participants were recruited through convenient sampling. The sample size was calculated using the OpenEpi, version 3 software (www.OpenEpi.com).
N is Population size (for finite population correction factor or fpc) = 51,200; p is the hypothesized (%) frequency of outcome factor in the population (10% +/−5; Confidence limits as % of 100) (absolute +/−%)(d) = 5%; DEFF (design effect = 1); Z is a constant = 1.96 for 95% Confidence interval. Based on the above parameters the minimum required sample size (n) was 138 participants.
Data collection
Data were collected through face-to-face interviews by three health care professionals, working at the selected healthcare facilities. The three interviewers were trained by the research team prior to the study. Structured questionnaires were administered before the consultations. Participants were given a unique identifier in order to avoid duplication. Once a participant was interviewed, the trained interviewers were instructed to cross their identifier off the list.
The questionnaire was developed based on existing literature and previous experience[24,25,26] (Additional File). The questionnaire comprised of three sections. The first section included general information (age, marital status, country of origin, duration of stay in Morocco, language, level of education, occupation, reasons for leaving country of origin, transit in Morocco, migration status, monthly income, social security, place of residence, household size). The second section included information about the SRH of the study participants (history of pregnancy, experience giving birth in a health facility, current use of contraceptives, history of unintended pregnancies, current pregnancy status, receiving pre-natal care, current diagnosis with obstetric morbidities). The third section included questions about SGBV (history of female genital mutilation, history of SGBV during lifetime and during migration, relationship with the aggressors, forms of SGBV, approaches used to commit SGBV). The fourth section included questions about the impact of SGBV (avoiding going out alone, change of residence, change in daily habits, experiencing psychological repercussions, experiencing repercussions on sexual health), and the utilization of prevention and support services (consulting a lawyer, reaching out to a CSO/NGO, visiting a health facility, filing a complaint). The questionnaire was administered in French for the majority of participants. One participant spoke English, therefore the questionnaire was translated into English and validated by the research team. Another participant spoke a foreign dialect but could understand French.
Operational definitions
SGBV was defined as “any harmful acts directed against a person because of his or her sex or gender. It includes sexual, physical, mental and economic harm inflicted in public or in private. It also includes threats of violence, coercion and manipulation [27].
Physical violence was defined as “the intentional use of physical force with the potential to cause death, disability, injury or harm” [28].
Sexual violence was defined “any sexual act, attempt to obtain a sexual act, or other act directed against a person’s sexuality using coercion, by any person regardless of their relationship to the victim, in any setting. It includes rape, defined as the physically forced or otherwise coerced penetration of the vulva or anus with a penis, other body part or object, attempted rape, unwanted sexual touching and other non-contact forms“[29].
Verbal abuse was defined “an act that undermines a person’s sense of self-worth through constant criticism; belittling one’s abilities; name-calling or other forms of insults”[30].
Blackmail was defined as “the act of threatening to harm someone or someone’s reputation unless the person does as you say, or a payment made to someone who has threatened to harm another person or another person’s reputation if they fail to pay them” [31]. Intimidation was defined as “the action of frightening or threatening someone, usually in order to persuade them to do something that you want them to do”[32].
Sexual dysfunction was defined as “any difficulty moving through the stages of sexual desire, arousal, and orgasm, as well as subjective satisfaction with the frequency and outcome of individual and partnered sexual behavior”[33]. Obstetric morbidities were defined as “any condition that is attributed to or aggravated by pregnancy and childbirth which has a negative impact on the woman’s wellbeing and/or functioning” [34].
Ethical considerations
This study was approved by the Ethics Committee. All study participants were given an information sheet about the aim and objectives of the study. Participants were also made aware of their right to withdraw from the study at any moment. Complete anonymity was maintained to guarantee confidentiality of data and protect the identity of the study participants.
Statistical analysis
Statistical analysis was conducted using SPSS software (version 21). Quantitative variables were presented in means and standard deviations (means ± standard deviation) and qualitative variables were presented in numbers and percentages (%).
Results
Socio-demographic characteristics of the study population
Of 151 participants included in this study, many participants (60.9%) were between the ages of 18 and 34 years old and 83.3% were single. The countries of origin included the Ivory coast (28.5%), the Democratic Republic of Congo (DRC) (17.9%), Guinea Conakry (24.5%) and Cameroun (20.5%). Almost all participants spoke French (98.7%) and the majority either received primary or secondary education (51%) or higher education or vocational training (29.1%). However, approximately 19.9% of respondents had no prior education. The majority of migrants (72.2%) in this study have been in Morocco for less than four years. Approximately 82% of participants declared having no source of income, and the majority (96.4%) did not have social security. A significant share of respondents (80.1%) considered Morocco a country of transit (Table 1).
Sexual and reproductive health of migrant women in Morocco
In this study, approximately 76.7% of participants had history of pregnancy, of which 67.3% previously gave birth in a health facility. Among respondents, the majority (62.1%) did not use any contraceptive method and approximately 11.7% have previously experienced an unintended pregnancy. About 16.6% of women were pregnant at the time of the study among which 56% declared receiving pre-natal care. Finally, approximately 12.1% of women with a history of pregnancy had an obstetric morbidity at the time of the study (Table 2).
Sexual and gender-based violence against migrant women in Morocco
In this study, almost 30% of participants have experienced female genital mutilation. The majority of participants (87.4%) have experienced SGBV during their lifetime and 68.7% have been victims of SGBV more than once. Additionally, more than two-thirds of participants (76.2%) have experienced SGBV during migration. Among victims of SGBV during migration, 21.2% have been aggressed by a thief or a delinquent. A large share of SGBV victims (75.8%) have experienced verbal abuse and 21.2% have experienced physical violence. When asked about the approaches used by the aggressor, over half of the study participants (58.6%) declared having been threatened with arms and/or physical force and 24.2% have been subject to intimidation (Table 3).
Impact of SGBV and utilization of preventive and supportive SGBV services by migrant victims
Among victims of SGBV during migration, only a minority have consulted a lawyer (1%), or have or reached out to a CSO/NGO (2%), or visited a health facility (7%) or filed a complaint (9%). Among victims who filed a complaint, only 9.1% declared having received follow-up on their complaint. Among victims of SGBV during migration, the majority (87.9%) avoid going out alone, 14.1% changed their place of residence, and 73.7% changed their daily habits. When asked about psychological repercussions, only a minority of victims (10.1%) declared having experienced psychological repercussions that required professional help in the aftermath of the violent act. Finally, only a minority of victims (2%) reported having experienced disruptions in their sexuality in the aftermath of the violent act (Table 4).
Discussion
This study described the SRH outcomes of migrant women in Morocco as well as the prevalence of SGBV and utilization of support services. The main findings were that many migrant women (62.1%) in this study did not use any contraceptives. However, the majority of women who were pregnant at the time of the study were receiving pre-natal care. In addition, a high share of participants in this study reported being a victim of SGBV, especially verbal, physical and psychological violence, and have expressed the impact of the violence on their daily lives. Finally, the utilization of legal, healthcare and social support services was low among victims of SGBV.
In this study, over half of migrant women who were pregnant at the time of study declared receiving pre-natal care. However, over two thirds of migrant women were not using any contraceptive method. In the general population, according to recent data released by the United Nations Population Fund (UNFPA), the prevalence rate of contraception use is 43% among all women and 71% among married and in union women as of 2022,[35]. Furthermore, 87% of births were attended by skilled health personnel between 2004 and 2020 [35]. Family planning represents a major challenge to population health in Morocco due to its social, economic and health implications. Major strides have been made in contraception coverage, reducing maternal and child mortality, preventing unintended pregnancies and the provision of pre-natal care [36]. Local NGOs have launched several initiatives to promote the SRH of migrants in Morocco. In 2018, community-based health services launched by the Moroccan Association of Family Planning have raised awareness about family planning reaching 16,400 men and women, including migrants, refugees and asylum seekers [37]. In 2017, 329 women have benefited from pregnancy surveillance through the National Program for Pregnancy and Childbirth Surveillance, in three Moroccan regions [38]. Additionally, about 224 and 534 women benefited from family planning services and HIV-AIDS follow-up respectively in the same regions, and 57 migrant women were admitted to a maternity hospital [38]. Despite the abovementioned efforts to improve access to care, there remains an underutilization of healthcare services by the migrant population which spurs questions around the local barriers that prevent migrants from accessing services offered by Ministry of Health and its NGO and civil society partners. Migrant women and girls are subject to the interruption of the continuum of care during their migration or in the host country and are therefore at high risk of pregnancy complications and morbidities. Consequently, there would seem to be a definite need for further large-scale studies in order to identify institutional and structural barriers that impede access to care by the migrant population in Morocco. These barriers would be an appropriate target for interventions aimed at improving health outcomes of migrant women and facilitating their social and professional integration.
In this study, that most participants (76.2%) declared having been a victim of SGBV during migration. This number is lower compared to another study among sub-Saharan migrants in Morocco and along its borders (89.6%) [39]. Lower numbers were reported among migrants in Italy 46.5% [26], among female refugees and asylum seekers in the DRC, Somalia and Uganda (52.1%) [40], among immigrants in the United States (4.1%)[41] and among Moroccan migrants in Spain (12%) [7]. Verbal abuse followed by physical violence were the most common forms of SGBV in this study which match the results of a study among immigrants and refugees in Italy [26]. Psychological violence such as threats to use arms and/or physical force was also common among survivors of SGBV in this study. It is often difficult to determine the extent of violence among migrant populations; however, data from organizations such as Médecins Sans Frontières (MSF) showed that in 2012, care has been provided to approximately 700 survivors of sexual violence in Morocco, among which 94% were female [42]. In 7% of cases, there were more than two aggressors and the majority of victims were from the DRC (32%) and Nigeria (30%) [42]. Additionally, one qualitative study using a community-based research approach explored violence among sub-Saharan migrants in Morocco [39]. Results showed that much of the violence was of a sexual nature which is differs greatly from the findings in this study, where only 2% of SGBV victims reported a sexual form of abuse [39]. The forms of SGBV experienced by migrants often vary during migration phases and may lead to migrants experiencing several forms of SGBV and by different aggressors. Further understanding of how time and space affect the experience of SGBV should be the target of future research and would guide the design of appropriate interventions tailored to migration stages and forms of SGBV [43].
In this study only a minority of survivors of SGBV reported the incident. Underreporting largely affects the estimations of the magnitude of SGBV. Some studies exploring the determinants of reporting of SGBV have shown that reporting was less likely to occur among women with no education or with a low education level which make up a small but non-negligible percentage of migrant women in this study. However, some contradicting findings were reported by other studies where reporting of SGBV was lower among women with higher than primary school education. This was explained by the need of highly educated survivors to maintain their social standing in their communities [44]. Other factors such as shame, guilt and stigma particularly in the case of sexual violence, doubts about confidentiality and about being believed, act as barriers to the reporting of SGBV [45]. Furthermore, studies among survivors of SGBV showed that women who relied on financial support from their partners were also less likely to report SGBV. Many NGO-led initiatives in Morocco are geared towards capacity building and improving professional integration of migrants within their host communities [46]. These efforts need to be strengthened in order to promote autonomy among migrant women and empower them to report SGBV, as well as to seek and utilize support services, particularly in the case of intimate partner violence.
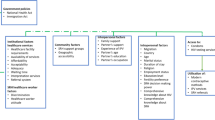
The precarious conditions under which migrants, especially undocumented migrants live, and their exposure to violence and abuse increases their vulnerability as well as their healthcare and psychological needs. While major progress has been made in Morocco with regards to recognizing the rights of migrants, and more specifically their right to adequate healthcare [20], more efforts should go towards understanding and addressing the contextual determinants of vulnerability [2]. In this study, only a minority of SGBV victims used one or more form of SGBV support services. Potential causes of the underutilization of these services are lack of adequate information systems and communication channels, previous unsatisfying experiences, stigma and discrimination and fear of deportation in the case of lack of legal documentation [47]. Further research is needed to investigate these barriers and identify facilitators that strengthen SGBV support systems. Nevertheless, the need to provide information about available SGBV support services to migrant women Morocco cannot be overemphasized. Lastly, improving coordination mechanisms and referral pathways between NGOs offering these services and healthcare facilities in Morocco, is critical in order to mitigate the negative SRH outcomes in victims of SGBV.
This is the first descriptive study to describe the SRH status of migrant women in Morocco and the first study to explore the impact of SGBV and the utilization of preventive and supportive SGBV services by the victims. Our study has some limitations. First, the study was only performed at three centres; therefore, the results should be generalized with caution to the total migrant population in Morocco. Second, the findings were based on self-reported responses which may have been subject to recollection bias. Third, the sensitive nature of the topic may lead to underreporting especially pertaining to sexual violence, which could potentially lead to the underestimation of the real prevalence of certain forms of SGBV. Fourth, this study was conducted in healthcare settings which may have affected the prevalence estimates.
Conclusion
Overall, our findings show a low contraception coverage, moderate access to prenatal care, high prevalence of SGBV, and low utilization of preventive and supportive SGBV services by migrant women in Morocco. Despite the efforts undertaken by the Moroccan government and the Ministry of Health, the SRH needs of the migrant population are yet to be realized. The complexity of the migration phenomenon and its spill-over consequences on health and social well-being call for comprehensive public policies that address the fundamental determinants of the vulnerability experienced by this population. Because of the intimate link between SGBV and SRH outcomes, it is also imperative that SGBV is included as a strategic area of focus and is integrated in the national 2021–2030 SRH Strategy in Morocco.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- SRH:
-
Sexual and reproductive health
- SGBV:
-
Sexual and gender-based violence
- IOM:
-
International Organization for Migration
- CSO:
-
Civil Society Organization
- NGO:
-
Non-Governmental Organization
- HCP:
-
High Commission of Planning
- WHO:
-
World Health Organization
- UNFPA:
-
United Nations Population Fund
References
Interactive World Migration Report. 2022. https://worldmigrationreport.iom.int/wmr-2022-interactive/. Accessed 13 Jul 2022.
International Organization for Migration (IOM). The Determinants of Migrant Vulnrrability. 2019.
Refugee and migrant health. https://www.who.int/news-room/fact-sheets/detail/refugee-and-migrant-health. Accessed 13 Jul 2022.
Lauritano D, Moreo G, Carinci F, Campanella V, Della Vella F, Petruzzi M. Oral Health Status among Migrants from Middle- and Low-Income Countries to Europe: A Systematic Review.Int J Environ Res Public Health. 2021;18.
Hargreaves S, Rustage K, Nellums LB, McAlpine A, Pocock N, Devakumar D, et al. Occupational health outcomes among international migrant workers: a systematic review and meta-analysis. Lancet Glob Health. 2019;7:e872–82.
Bedaso A, Duko B. Epidemiology of depression among displaced people: A systematic review and meta-analysis.Psychiatry Res. 2022;311.
Nellums LB, Thompson H, Holmes A, Castro-Sánchez E, Otter JA, Norredam M, et al. Antimicrobial resistance among migrants in Europe: a systematic review and meta-analysis. Lancet Infect Dis. 2018;18:796–811.
Rojas-Venegas M, Cano-Ibáñez N, Khan KS. Vaccination coverage among migrants: a systematic review and meta-analysis. Semergen. 2022;48:96–105.
Hasan-ul-Bari SM, Ahmed T. Ensuring sexual and reproductive health and rights of Rohingya women and girls. The Lancet. 2018;392:2439–40.
Zong Z, Sun X, Mao J, Shu X, Hearst N. Contraception and abortion among migrant women in Changzhou, China. Eur J Contracept Reprod Health Care. 2021;26:36–41.
Heaman M, Bayrampour H, Kingston D, Blondel B, Gissler M, Roth C, et al. Migrant women’s utilization of prenatal care: a systematic review. Matern Child Health J. 2013;17:816–36.
Khin YP, Nawa N, Fujiwara T, Surkan PJ. Access to contraceptive services among Myanmar women living in Japan: a qualitative study. Contraception. 2021;104:538–46.
Violence against women prevalence estimates., 2018 – Global fact sheet. https://www.who.int/publications/i/item/WHO-SRH-21.6. Accessed 28 Apr 2022.
El-Adawy M, Ronzoni AR, Sakr H. Addressing violence against women in the Eastern Mediterranean Region. East Mediterr Health J. 2021;27:431–2.
Violence against women. https://www.who.int/news-room/fact-sheets/detail/violence-against-women. Accessed 13 Jul 2022.
World Health Organization. Seventieth World Health Assembly: Promoting the health of refugees and migrants. 2017.
Haut-Commissariat au. Plan du Royaume du Maroc. Enquête Nationale sur la Migration. 2021.
Global Compact for Migration | IOM, UN Migration. https://www.iom.int/global-compact-migration. Accessed 15 Apr 2022.
Ministry of Foreign Affairs Morocco. Politique Nationale d’Immigration et d’Asile. 2018.
Ministère de la Santé. et de la Protection Sociale OI des M. Plan Stratégique National Santé et Immigration 2021–2025. 2021.
el Berri H. Ministère de la Santé. Journée Mondiale de la santé: Couverture Sanitaire des Migrants au Maroc. Rabat; 2018.
Health of refugees. and migrants Practices in addressing the health needs of refugees and migrants WHO Eastern Mediterranean Region 2018.
Ministry of Foreign Affairs Morocco. Politique Nationale d’Immigration et d’Asile. 2017.
McCloskey LA, Williams C, Larsen U. Gender inequality and intimate partner violence among women in Moshi, Tanzania. Int Fam Plan Perspect. 2005;31:124–30.
Oliveira C, Keygnaert I, Oliveira Martins M do, Dias R. S. Assessing reported cases of sexual and gender-based violence, causes and preventive strategies, in European asylum reception facilities. Global Health. 2018;14.
Napolitano F, Gualdieri L, Santagati G, Angelillo IF. Violence Experience among Immigrants and Refugees: A Cross-Sectional Study in Italy. Biomed Res Int. 2018;2018.
UNHCR - Gender-based Violence. https://www.unhcr.org/gender-based-violence.html. Accessed 1 Jan 2023.
World Health Organization. Integrating Poverty and Gender into Health Programmes. 2005. https://apps.who.int/iris/bitstream/handle/10665/207485/9290611944_eng.pdf?se. Accessed 1 Jan 2023.
Violence against women. https://www.who.int/news-room/fact-sheets/detail/violence-against-women. Accessed 6 Jan 2023.
Types of violence against women and girls | UN Women. – Headquarters. https://www.unwomen.org/en/what-we-do/ending-violence-against-women/faqs/types-of-violence. Accessed 6 Jan 2023.
BLACKMAIL | définition en anglais - Cambridge Dictionary. https://dictionary.cambridge.org/fr/dictionnaire/anglais/blackmail. Accessed 1 Jan 2023.
INTIMIDATION | English meaning - Cambridge Dictionary. https://dictionary.cambridge.org/dictionary/english/intimidation. Accessed 6 Jan 2023.
Fielder R. Sexual Functioning.Encyclopedia of Behavioral Medicine. 2013;:1774–7.
van den Broek NR. Maternal and Newborn Health. Hunter’s Tropical Medicine and Emerging Infectious Diseases. 2020;:133–40.
UNFPA Morocco. https://www.unfpa.org/fr/data/MA. Accessed 14 Jul 2022.
Morocco (MAR). - Demographics, Health & Infant Mortality - UNICEF DATA. https://data.unicef.org/country/mar/. Accessed 14 Jul 2022.
HIV/AIDS - Association Marocaine de Planification Familiale. https://www.ampf.org.ma/language/en/vhs-aids/. Accessed 8 May 2022.
Ministère de la Santé et de la Protection Sociale. Célébration de la Journée Internationale du Migrant. https://www.sante.gov.ma/Pages/Communiques.aspx?IDCom=189. Accessed 8 Apr 2022.
Keygnaert I, Dialmy A, Manço A, Keygnaert J, Vettenburg N, Roelens K, et al. Sexual violence and sub-saharan migrants in Morocco: a community-based participatory assessment using respondent driven sampling. Global Health. 2014;10:1–16.
Morof DF, Sami S, Mangeni M, Blanton C, Cardozo BL, Tomczyk B. A cross-sectional survey on gender-based violence and mental health among female urban refugees and asylum seekers in Kampala, Uganda. Int J Gynaecol Obstet. 2014;127:138–43.
Wheeler K, Zhao W, Kelleher K, Stallones L, Xiang H. Immigrants as crime victims: experiences of personal nonfatal victimization. Am J Ind Med. 2010;53:435–42.
Médecins Sans Frontières (MSF), Violences. Vulnérabilité et Migration:Bloqués aux Portes de l’Europe. 2013.
Tan SE, Kuschminder K. Migrant experiences of sexual and gender based violence: a critical interpretative synthesis. Globalization and Health 2022 18:1. 2022;18:1–15.
Ssanyu JN, Namuhani N, Nalwadda CK. Reporting of sexual and gender-based violence and associated factors among survivors in Mayuge, Uganda. Afr Health Sci. 2022;22:62–8.
Sable MR, Danis F, Mauzy DL, Gallagher SK. Barriers to reporting sexual assault for women and men: perspectives of college students. J Am Coll Health. 2006;55:157–62.
BILAN OIM MAROC. 2021. https://morocco.iom.int/sites/g/files/tmzbdl936/files/documents/bilan_oim-2021.pdf. Accessed 12 May 2022.
Ivanova O, Rai M, Kemigisha E. A Systematic Review of Sexual and Reproductive Health Knowledge, Experiences and Access to Services among Refugee, Migrant and Displaced Girls and Young Women in Africa.Int J Environ Res Public Health. 2018;15.
Acknowledgements
The authors would like to acknowledge deeply the technical support and guidance of the WHO and UNFPA Morocco. The authors would also like to thank all key interviewees, health professionals and other participants for their support during this study.
Funding
This study was initiated and fully-funded by the WHO.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.K., L.A. and B.A., methodology, M.K. and B.A., validation, M.K., L.A. and A.Y.; formal analysis, O.B. and L.A. data curation, L.A., A.Y. and S.E. writing—original draft preparation, L.A. and O.B.; writing—review and editing, L.A., M.K., O.B., B.A, S.E., A.Y. and G.K.; supervision, M.K.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Ethics Committee for Biomedical Research of Mohammed V University of Rabat authorization number 36/21. Participation in this study was voluntary and was not compensated. Written informed consent was obtained from all participants prior to the study. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional File
: Sexual and reproductive health and gender-based violence among female migrants in Morocco: a cross sectional survey
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Acharai, L., Khalis, M., Bouaddi, O. et al. Sexual and reproductive health and gender-based violence among female migrants in Morocco: a cross sectional survey. BMC Women's Health 23, 174 (2023). https://doi.org/10.1186/s12905-023-02307-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02307-1