Abstract
Background
Both contextual and cancer-related factors could be identified as causes of the interindividual variability observed for symptoms experienced during breast cancer treatment with chemotherapy. Understanding age differences and the predictors of latent class memberships for symptom heterogeneity could contribute to personalized interventions. This study aimed to identify the role of age differences on cancer-related symptoms in women undergoing chemotherapy for breast cancer in China.
Methods
A cross‑sectional survey was conducted among patients with breast cancer in three tertiary hospitals in central China between August 2020 to December 2021. The outcomes of this study included sociodemographic and clinical characteristics, Patient-Reported Outcomes Measurement Information System (PROMIS)-57 and PROMIS-cognitive function short form scores.
Results
A total of 761 patients were included, with a mean age of 48.5 (SD = 11.8). Similar scores were observed across age groups for all symptoms except for fatigue and sleep disturbance domains. The most central symptoms varied among each group, and were fatigue, depression, and pain interference for the young-aged, middle-aged, and elderly-aged groups, respectively. In the young-aged group, patients without health insurance (OR = 0.30, P = 0.048) and in the fourth round of chemotherapy or above (OR = 0.33, P = 0.005) were more likely to belong to low symptom classes. In the middle-aged group, patients in menopause (OR = 3.58, P = 0.001) were more likely to belong to high symptom classes. In the elderly-aged group, patients with complications (OR = 7.40, P = 0.003) tended to belong to the high anxiety, depression, and pain interference classes.
Conclusions
Findings from this study indicated that there is age-specific heterogeneity of symptoms present for Chinese women being treated for breast cancer with chemotherapy. Tailored intervention should consider the impact of age to reduce patients’ symptom burdens.
Similar content being viewed by others
Background
Patients on chemotherapy for breast cancer experience multiple concurrent and coexisting symptoms caused by the disease and treatment toxicity [1]. Symptoms can result in treatment delays and non-adherence, with negative impacts on survival [2]. Age differences in treatment-related symptom burden are not well-documented in patients with breast cancer. The best survival rates of breast cancer have been found in middle-aged women, with decreased survival at each end of the age spectrum [3]. Young women with breast cancer have aggressive features and worse prognosis compared to older patients [4]. Evidence has shown that young women with breast cancer have worse health outcomes in terms of physical and psychosocial aspects, and chemotherapy was a significant treatment factor associated with poorer health outcomes [3, 5]. Additionally, chemotherapy played a more critical role in comparison to surgery, with age having an influence on the effects [3]. Older women with breast cancer were less likely to be concerned about premature menopausal symptoms, infertility, sexual dysfunction, and had less psychological symptoms [6]. Identification of age differences and patients at highest risk is critical and would benefit these patients by allowing early intervention. The modifiable drivers of symptom burden inequities can be reduced by minimizing the present knowledge gap.
Interindividual variability exists in the symptom experience for patients with breast cancer receiving chemotherapy. Contextual and cancer-related factors could both play different roles in this variability [7]. No studies to date have examined the age difference on symptoms via a person-centered method. Latent class analysis (LCA) is a person-centered approach that has been extensively used for clinical purposes and contributes to distinguishing those patients at risk [8, 9]. Additionally, intervention on central symptoms in the networks can provide targeted strategies. Cancer-related symptoms, and contextual and illness-related factors in patients with breast cancer display complex reciprocal interactions, which add to heterogeneous presentations of symptoms. The network approach has been used to examine multiple, complex relationships between symptoms among patients with chronic diseases, and helps to identify the most relevant connections between symptoms [10, 11]. Therefore, a LCA method in addition to network analysis is ideal for identifying symptom heterogeneity and the most central symptoms for appropriate intervention. Using LCA and network analysis, this study aimed to extend previous findings by identifying age difference and unique associations between cancer-related symptoms in women undergoing chemotherapy for breast cancer.
Methods
Study design and participants
This cross-sectional study recruited patients from three tertiary grade A hospitals (Affiliated Cancer Hospital of Fudan University, Affiliated Zhongshan Hospital of Fudan University, The Second Affiliated Hospital of Guilin Medical University) from August 2020 to December 2021. We invited women aged 18 or older who had been diagnosed with breast cancer, currently undergoing chemotherapy, and had access to a mobile app to complete a web-based survey. Patients were excluded if they were unable to participate owing to psychiatric or intellectual disabilities.
Patients were classified into three age groups: young-aged group (18–39 years), middle-aged group (40–59 years), elderly-aged group (older than 60 years). The study was approved by the institutional review boards of Fudan University and all corresponding hospitals (no.: 1810192–22). All participants were informed of the study aims and procedures, and signed written informed consent before the study. A web-based survey was performed and collected from the participants. The research assistant clarified each question raised by participants and checked medical records for completeness and consistency.
Measures
Demographic and clinical characteristics of the patients were recorded in this study. The Patient-Reported Outcomes Measurement Information System (PROMIS) instruments, PROMIS-57 and PROMIS-cognitive function short form were included, with permission from the PROMIS National Center, China. The surveys took approximately 20–30 min to complete.
Demographic and clinical characteristics
Demographic characteristics included age, marital status, number of children, menstrual status, educational attainment, occupation, annual family income, and medical insurance. Clinical information, retrieved from the medical records, included complication status, therapeutic regimen, and chemotherapy cycles.
PROMIS-57
The PROMIS-57 was used to assess symptoms in this study. The scale consists of 57 items clustered into seven domains: anxiety, depression, fatigue, sleep disturbance, pain interference and intensity, physical function, and ability to participate in social roles and activities [12]. Each item was scored on a five-point Likert scale, except for pain intensity with one item, which was scored between 0 and 10 (least to most severe) [13]. Raw scores varied from 8 to 40 in each domain and were derived as per the PROMIS scoring manual into T-scores with a mean of 50 and a standard deviation (SD) of 10. Higher scores indicated a higher level of functioning or greater symptom severity. An acceptable internal consistency for the scale was found in this sample (α ranged from 0.87 to 0.97).
PROMIS-cognitive function short form
The 4-item PROMIS-cognitive function short form was used to identify perceived cognitive difficulties in the previous 7 days [14]. Items were scored on a 5-point Likert scale ranging from 1 (“very often”) to 5 (“never”) [15]. Total scores varied from 4 to 20 and were subsequently converted into T-scores (mean = 50, SD = 10). A higher score indicated better perceived cognitive function [15]. The Cronbach's α was 0.96 in this study.
Statistical analyses
Statistical analyses were performed by using SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA), R version 4.1.0 and Mplus version 8.0. Descriptive analysis was used for the distribution of sociodemographic, clinical, symptoms, and function characteristics. Categorical variables were presented as frequencies and percentages, and continuous variables as means and SDs. A symptom network analysis was used to identify the most central symptom in the entire sample and in each age group. In the symptom networks, a node indicates an independent symptom, an edge indicates the conditional relationships between two symptoms, and the edge thickness shows the strength of the relationship between them [16]. Thus, two centrality indices (strength and closeness) were output to quantify the relationship. The strength value represents the probability of one symptom and other symptoms occurring together, and the closeness value represents the path from one symptom to all other symptoms [16].
The questionnaires were scored according to the PROMIS Scoring Manual, and were dichotomized as 0 or 1 according to the cutoff scores for clinical differences (https://www.healthmeasures.net/). After data processing, LCA was performed to identify clusters of individuals displaying similar patterns of symptoms by age groups (15–39, 40–59, and over 60 years). Models with an increasing number of latent classes were assessed until the best fitting model was determined. To select the optimal LCA model, the following indices were included: the Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted BIC (aBIC) were used to assess information criteria; and the Lo-Mendell-Rubin (LMR) test and bootstrapped likelihood ratio test (BLRT) were used to improve the model fit, with significant values indicating a better fit for the k-class model than the k-1-class model. Entropy values that exceed 0.80 indicate a satisfactory classification accuracy [17]. Among the LCA models with different numbers of latent classes, a lower AIC, BIC, aBIC, larger entropy, and significant LMR-LRT and BLRT p values were indicative of good model fit [18]. Clinical interpretability was also considered to decide the best option. After the optimal model was determined, between-group difference was examined using Chi-square tests, Fisher’s exact tests or analysis of variance (ANOVA) where appropriate. Only statistically significant variables were entered into the stepwise logistic regression model. The regression was conducted separately by age groups to determine the contributing factors of symptoms for each group. P < 0.05 was considered statistically significant.
Results
Characteristics of the sample
Among the 803 participants investigated, 42 of them were not involved in the final analysis due to too many missing items. A final sample of 761 patients was included, with a mean age of 48.5 (SD = 11.8). Most of the patients were married, had children, were premenopausal, had a secondary education, were unemployed, had an annual family income of less than ¥60,000, had employment health insurance, were without complications, and had received chemotherapy combined with surgery. Among the 761 included patients, 217 (28.5%) belonged to the young-aged group (mean = 34.3, SD = 3.6), 397 (52.2%) belonged to the middle-aged group (mean = 50.0, SD = 5.6), and 147 (19.3%) belonged to the elderly-aged group (mean = 65.5, SD = 4.9). The detailed demographic and clinical characteristics of the participants are reported in Table 1.
Symptoms among different age groups
As shown in Table 2, the average T scores of symptoms were all beyond the normal range according to the PROMIS score manual (mean = 50, SD = 10 for normal range). Significant differences were noted for the fatigue and sleep disturbance domains across the age groups (P < 0.05). Additionally, post hoc multiple comparisons demonstrated that the fatigue levels of the young and middle-aged groups were higher than those of the elderly-aged group, and the sleep disturbance scores of the middle-aged and elderly-aged groups were higher than those of the young-aged group.
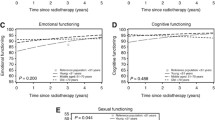
Network analysis of symptoms across different age groups
Networks are depicted in Fig. 1 a-d, with each group across the entire sample represented. Between-group differences were identified in terms of symptom networks of varied populations. Among the entire sample, depression (rs = 2.74, rc = 0.10) was identified as the most central symptom according to two centrality indices, followed by fatigue (rs = 2.65, rc = 0.10). In the young-aged group, the most central symptom was fatigue (rs = 2.55, rc = 0.99), followed by depression (rs = 2.52, rc = 0.10). The most central symptom was depression (rs = 2.92, rc = 0.11), followed by fatigue (rs = 2.80, rc = 0.11) in the middle-aged group. In the elderly-age group, the most central symptom was pain interference (rs = 2.72, rc = 0.11), followed by depression (rs = 2.70, rc = 0.10).
Latent class analysis among different age groups
The model fit statistics of LCA for each age group are reported in Table 3. The two-class model, the three-class model and the other two-class model were respectively selected by the young-aged group, the middle-aged group and the elderly-aged group, which was based on the model selection criteria for relatively low AIC, BIC, and aBIC values, high entropy, significant P values for LMR and BLRT, in addition to clinical interpretability. Detailed item probabilities of latent classes in different age groups were shown in Fig. 2, Fig. 3, and Fig. 4.
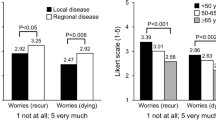
In terms of the latent classes in the young-aged group, Class 1 (n = 112, 51.6%) was characterized by high anxiety, depression, and pain intensity, as well as moderate fatigue and sleep disturbance, while Class 2 (n = 105, 48.4%) was characterized by low symptom probabilities. Similar patterns were found in the elderly-aged group (Class 1: n = 68, 46.3%; Class 2: n = 79, 53.7%). In the middle-aged group, an additional class with high symptom probabilities was identified: Class 1 (n = 74, 18.6%) was characterized by high symptom probabilities; Class 2 (n = 138, 34.8%) was characterized by high anxiety, depression and pain intensity but low fatigue and sleep disturbance, while Class 3 (n = 185, 46.6%) was characterized by low symptom probabilities.
Predictors of the latent classes among different age groups
Univariate analysis was performed to identify between-group differences in the latent classes. The number of children, educational attainment, medical insurance, and chemotherapy cycles were identified as significant variables in the young-aged group, and menstrual status was identified in the middle-aged group. Additionally, the number of children and complication status were found to be statistically significant in the elderly-aged group.
Based on the significant variables by univariate analysis, logistic regression analysis was performed to identify potential predictors for higher risk classes, with the low symptom latent class of each age group set as the reference. The results are reported in Table 4. In the young-aged group, patients without health insurance (OR = 0.30, P = 0.048) and in the fourth chemotherapy or above (OR = 0.33, P = 0.005) were more likely to belong to low symptom classes. In the middle-aged group, menopausal patients (OR = 3.58, P = 0.001) were more likely to belong to high symptom classes. As for patients in the elderly-aged group, those with complications (OR = 7.40, P = 0.003) were more likely to report high anxiety, depression, and pain interference.
Discussion
This study examined whether age difference existed in terms of cancer-related symptoms in women with breast cancer receiving chemotherapy. Except for fatigue and sleep disturbance, similar symptom patterns were observed across the three age groups. Despite similar mean scores across the age groups, heterogeneity of symptoms was observed via the network analysis and the LCA. The results of network analysis demonstrated that depression and fatigue were the central symptoms in the investigated population. Depression and fatigue were frequently reported symptoms in patients with breast cancer, and younger women consistently had more severe symptoms when compared with their older counterparts [19, 20] In our study, pain interference was more closely related to the occurrence of other symptoms in the elderly-aged group. Furthermore, the results of the LCA also indicated that middle-aged patients showed more symptoms than other groups, in line with results from a prior study by Pinto et al. [21] showing that younger age (< 65 years) had a negative impact on physical and mental symptom domains.
Occupation, annual family income, and medical insurance were associated with symptoms in the investigated population. Employment was shown to play a significant role in post-diagnostic health according to existing evidence in patients with breast cancer [22]. Health benefits from employment included an increased sense of purpose, high self-esteem, and a strong sense of social support, all of which were associated with improved quality of life [23]. As a result of cancer and its expensive treatment, a financial dilemma was triggered owing to lower income, insufficient health insurance, or unemployment [24]. These results were consistent with previous reports in the context of cancer. For example, perceived financial hardship had been reported to be directly correlated with symptom distress in patients with advanced cancer [25]. In a sample of patients with breast cancer, the financial strain showed a significant association with worse depression, anxiety, and physical symptoms [26]. Further, a systematic review indicated that there was a positive relationship between financial strain and psychological symptoms including anxiety, depression, and overall distress, but less evidence for physical symptoms [27].
Young patients in the fourth chemotherapy cycle or higher appeared to belong to low symptom classes. Undergoing more chemotherapy cycles would allow the patients to be better prepared, and the findings were in accord with a previous study reporting that patients with breast cancer have more intense symptoms in the initial stage of chemotherapy [28]. However, young patients in this study did not report a higher symptom burden when compared with other groups. According to a systematic review, younger patients with breast cancer were at particular risk for psychological symptoms, especially for altered body image and sexual concerns, and the younger life stage was often associated with more aggressive treatments [29]. This inconformity might be attributed to the fact that one-tenth of the young patients were single; whereas in other groups there was a very small proportion of single patients.
For middle-aged patients, menopausal patients were more likely to report high symptom burdens. Menopausal symptoms such as fatigue, sleep disturbance, and anxiety, were common in patients after their chemotherapy and might be more frequent and severe among women after natural menopause [30]. Middle-aged patients were the groups with the largest proportion of low-income and rural health insurance in this study. Young to middle-aged patients were reported to experience more psychological stress than older counterparts, in part due to the effect of treatment on fertility, raising young children, not expecting to get a diagnosis of cancer at a relatively young age, worse marital satisfaction, and employment worries [31, 32].
Most notably, the presence of complications including myelosuppression, peripheral neurotoxicity, dermal toxicity, and urinary system toxicity significantly increased patients’ likelihood of reporting high anxiety, depression, and pain interference, particularly in the elderly-aged group. These women were more likely to have complications due to pre-existing medical conditions, which might cause psychological symptoms. The results were consistent with previous studies, showing that comorbidities and functional limitations were significant risk factors for depressive symptoms in older patients with breast cancer [27, 33]. Cancer and comorbidities have been reported to interact synergistically to affect physical and psychological outcomes in older patients with cancer [27, 33]. Having two or more comorbidities and functional limitations were strongly related to an elevated risk of depression both in patients with cancer and non-cancer controls, which supported our findings.
Limitations
Several limitations must be noted in this study. First, the cross-sectional design might hinder our ability to explore the age differences in the symptom experiences over time. Second, the sample size was small, and the patients were recruited in tertiary grade A hospitals. The findings might not be generalizable to other care centers since results obtained by the network analysis and the LCA can be sample-specific. Finally, we did not specify the therapeutic regimen and chemotherapy drugs used in this study, which might have impacted the results. Further studies are needed to confirm the results in other populations.
Conclusions
Findings from this study demonstrated symptom heterogeneity in women undergoing chemotherapy for breast cancer. Middle-aged patients, especially menopausal women, were more likely to report high symptom burdens. Additionally, older patients with complications were more likely to belong to have high levels of anxiety, depression, and pain interference classes. Tailored intervention should consider the impact of age to reduce symptom burdens.
Availability of data and materials
The dataset generated and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Abbreviations
- PROMIS:
-
Patient-reported outcomes measurement information system
- LCA:
-
Latent class analysis
- AIC:
-
Akaike information criterion
- BIC:
-
Bayesian information criterion
- aBIC:
-
Adjusted Bayesian information criterion
- LMR test:
-
Lo-Mendell-Rubin
- BLRT:
-
Bootstrapped likelihood ratio test
References
AlFayyad I, Al-Tannir M, AlShammari A. Clinically significant symptoms prevalence in breast and colon cancers and leukemia patients: a comparison analysis of patient-reported outcomes. Support Care Cancer. 2022;30(1):439–46.
Reilly CM, Bruner DW, Mitchell SA, Minasian LM, Basch E, Dueck AC, et al. A literature synthesis of symptom prevalence and severity in persons receiving active cancer treatment. Support Care Cancer. 2013;21(6):1525–50.
Sauder CAM, Li Q, Bold RJ, Ruddy KJ, Keegan THM. Secondary breast cancer sociodemographic characteristics and survival by age group. Ann Surg Oncol. 2021;28(13):8118–27.
Avci O, Tacar SY, Seber ES, Yetisyigit T. Breast cancer in young and very young women; is age related to outcome? J Cancer Res Ther. 2021;17(6):1322–7.
Choong WL, Andrew RE, Hogg FJ, Munnoch DA, Pitsinis V, Macaskill EJ. Age and cancer treatment factors influence patient-reported outcomes following therapeutic mammoplasty and contralateral symmetrisation for the treatment of breast cancer. J Plast Reconstr Aes. 2021;74(10):2557–64.
Vazquez D, Rosenberg S, Gelber S, Ruddy KJ, Morgan E, Recklitis C, et al. Posttraumatic stress in breast cancer survivors diagnosed at a young age. Psychooncology. 2020;29(8):1312–20.
Cai T, Qian J, Huang Q, Yuan C. Distinct dyadic coping profiles in Chinese couples with breast cancer. Support Care Cancer. 2021;29(11):1–10.
Cai T, Zhou T, Yuan C, Yu C, Ni F, Sheng Z. Heterogeneity of symptoms and functions among women receiving chemotherapy for breast cancer in China: A multicentre, cross-sectional study. Front Public Health. 2022;10:952710.
Cai T, Huang Q, Yuan C. Profiles of instrumental, emotional, and informational support in Chinese breast cancer patients undergoing chemotherapy: a latent class analysis. BMC Womens Health. 2021;21:183.
Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psych Psych Epid. 2017;52(1):1–10.
Robinaugh DJ, Hoekstra RHA, Toner ER, Borsboom D. The network approach to psychopathology: a review of the literature 2008–2018 and an agenda for future research. Psychol Med. 2020;50(3):353–66.
Cai T, Wu F, Huang Q, Yu C, Yang Y, Ni F, et al. Validity and reliability of the Chinese version of the patient-reported outcomes measurement information system adult profile-57 (PROMIS-57). Health Qual Life Out. 2022;20(1):1–12.
Rimehaug SA, Kaat AJ, Nordvik JE, Klokkerud M, Robinson HS. Psychometric properties of the PROMIS-57 questionnaire, Norwegian version. Qual Life Res. 2022;31(1):269–80.
Valentine TR, Weiss DM, Jones JA, Andersen BL. Construct validity of PROMIS® cognitive function in cancer patients and noncancer controls. Health Psychol. 2019;38(5):351–8.
Hartman SJ, Weiner LS, Nelson SH, Natarajan L, Patterson RE, Palmer BW, et al. Mediators of a physical activity intervention on cognition in breast cancer survivors: evidence from a randomized controlled trial. JMIR Cancer. 2019;5(2):e13150.
Zhu Z, Guo M, Dong T, Han S, Hu Y, Wu B. Assessing psychological symptom networks related to HIV-positive duration among people living with HIV: a network analysis. AIDS Care. 2022;34(6):725–33.
Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–69.
Watanabe M, Yamauchi K. Subtypes of overtime work and nurses’ fatigue, mental status, and work engagement: a latent class analysis of Japanese hospital nurses. J Adv Nurs. 2019;75(10):2122–32.
Ruiz-Casado A, Álvarez-Bustos A, de Pedro CG, Méndez-Otero M, Romero-Elías M. Cancer-related fatigue in breast cancer survivors: a review. Clin Breast Cancer. 2021;21(1):10–25.
Avis NE, Levine B, Naughton MJ, Case DL, Naftalis E, van Zee KJ. Explaining age-related differences in depression following breast cancer diagnosis and treatment. Breast Cancer Res Tr. 2012;136(2):581–91.
Pinto M, Gimigliano F, Tatangelo F, Megna M, Izzo F, Gimigliano R, et al. Upper limb function and quality of life in breast cancer related lymphedema: a cross-sectional study. Eur J Phys Rehab Med. 2013;49(5):665–73.
Mazanec SR, Park S, Connolly MC, Rosenzweig MQ. Factors associated with symptom distress in women with breast cancer prior to initiation of chemotherapy. Appl Nurs Res. 2021;62:151515.
Ekenga CC, Pérez M, Margenthaler JA, Jeffe DB. Early-stage breast cancer and employment participation after 2 years of follow-up: a comparison with age-matched controls. Cancer. 2018;124(9):2026–35.
Smith GL, Lopez-Olivo MA, Advani PG, Ning MS, Geng Y, Giordano SH, et al. Financial burdens of cancer treatment: a systematic review of risk factors and outcomes. J Natl Compr Cancer Ne. 2019;17(10):1184–92.
Gallups S, Copeland VC, Rosenzweig M. Perceived financial hardship among patients with advanced cancer. J Community Support Oncol. 2017;15(3):e163–9.
Perry LM, Hoerger M, Seibert K, Gerhart JI, O’Mahony S, Duberstein PR. Financial strain and physical and emotional quality of life in breast cancer. J Pain Symptom Manag. 2019;58(3):454–9.
Chan RJ, Gordon LG, Tan CJ, Chan A, Bradford NK, Yates P, et al. Relationships between financial toxicity and symptom burden in cancer survivors: a systematic review. J Pain Symptom Manag. 2019;57(3):646–60.
Plichta JK, Thomas SM, Vernon R, Fayanju OM, Rosenberger LH, Hyslop T, et al. Breast cancer tumor histopathology, stage at presentation, and treatment in the extremes of age. Breast Cancer Res Tr. 2020;180(1):227–35.
Paterson CL, Lengacher CA, Donovan KA, Kip KE, Tofthagen CS. Body image in younger breast cancer survivors: a systematic review. Cancer Nurs. 2016;39(1):e39–58.
Cohen PA, Brennan A, Marino JL, Saunders CM, Hickey M. Managing menopausal symptoms after breast cancer–A multidisciplinary approach. Maturitas. 2017;105:4–7.
Reyes-Gibby CC, Anderson KO, Morrow PK, Shete S, Hassan S. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health. 2012;21(3):311–8.
Champion VL, Wagner LI, Monahan PO, Daggy J, Smith L, Cohee A, et al. Comparison of younger and older breast cancer survivors and age-matched controls on specific and overall quality of life domains. Cancer. 2014;120(15):2237–46.
Deckx L, van Abbema DL, van den Akker M, van den Broeke C, van Driel M, Bulens P, et al. A cohort study on the evolution of psychosocial problems in older patients with breast or colorectal cancer: comparison with younger cancer patients and older primary care patients without cancer. BMC Geriatr. 2015;15(1):1–13.
Acknowledgements
The authors wish to extend sincere thanks to the data collectors for their contribution and the participants of the study for their co-operation.
Funding
This research was supported by the National Natural Science Foundation of China Youth Project (72104055). The funding agencies had no role in the design of the study, or collection, analysis, and interpretation of the data.
Author information
Authors and Affiliations
Contributions
TC, TZ, and FW were involved in the manuscript writing, design, analysis, and interpretation of the data. JC and QH were involved in the data collection, analysis, and interpretation of the data. TC, FW, and CY were involved in the conception, design, analysis, interpretation, and critical revision of manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethical Review Board of Fudan University (no.: 1810192–22). Permission letters were obtained from the three investigated hospitals. The study participants were asked for their full voluntary participation and written informed consent was obtained from those who agreed to participate upon provision of adequate explanation on the purpose and procedures of the study before enrollment into the study. This study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cai, T., Zhou, T., Chen, J. et al. Identification of age differences in cancer-related symptoms in women undergoing chemotherapy for breast cancer in China. BMC Women's Health 23, 100 (2023). https://doi.org/10.1186/s12905-023-02256-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02256-9