Abstract
Background
Cervical cancer is the second leading cause of cancer-related death and one of the top 20 causes of death among women in Ethiopia. Cervical cancer screening service has a vital value to reduce morbidity and mortality. Even though cervical cancer screening service utilization in Ethiopia is unacceptably low, its determinant factors were not well studied in the study area. Hence, this study was aimed at filling this information gap. This study aimed to identify determinants of cervical cancer screening service utilization among women attending healthcare services in Amhara region referral hospitals, Ethiopia.
Methods
Hospital-based case–control study was conducted among 441 women (147 cases and 294 controls) from May to July 2021. Cases were included consecutively and controls were selected using a systematic random sampling technique from the randomly selected hospitals. A pretested interviewer-administered questionnaire was used to collect the data from respondents. The data were entered into Epi data version 4.6 and exported to SPSS version 25 for analysis. Bivariable and multivariable logistic regression analysis was employed. Adjusted odds ratio with its 95% confidence interval and p value < 0.05 were used to estimate the strength and significance of the association.
Result
A total of 147 cases and 294 controls were enrolled in this study. Women with 30–39 years-old [AOR = 2.3; 95% CI 1.21, 4.68] and 40–49 years-old [AOR = 4.4 95% CI 1.97, 10.12], urban residence [AOR = 2.6; 95% CI 1.36, 5.21], secondary education [AOR = 4.4; 95% CI 2.18, 8.87] and diploma and above [AOR = 2.0; 95% CI: 1.05, 4.59], ever gave birth [AOR = 9.4; 95% CI 4.92, 18.26], having multiple sexual partners [AOR = 2.8; 95% CI 1.60, 5.03], good knowledge towards cervical cancer screening [AOR = 3.6; 95% CI 2.07, 6.43] and positive attitude on cervical cancer screening [AOR = 2.0, 95% CI 1.20, 3.70] were significant determinants of cervical cancer screening service utilization.
Conclusion
In this study, age (30–39 and 40–49), urban residence, secondary education, ever gave birth, good knowledge of cervical cancer screening, positive attitude towards cervical cancer screening, and having multiple sexual partners were significant determinants of cervical cancer screening service utilization. There is a need to strengthen the policy and health education on safe sexual practices and healthy lifestyles through information dissemination and communication to scale up screening service utilization.
Similar content being viewed by others
Introduction
Cervical cancer is a malignant neoplasm from cells originating in the cervix uteri, and sometimes it can be asymptomatic in the early stages of the disease’s progress [1]. It is caused by human papillomavirus (HPV) infection, which is transmitted through sexual intercourse and infects the areas around the cervix, anus, mouth, and throat [2]. At the early-stage cervical cancer may be manifested with watery, blood-tinged vaginal discharge. Intermittent vaginal bleeding that follows coitus or douching may also be noted. As the malignancy enlarges, bleeding typically intensifies and occasionally follows uncontrolled hemorrhage [1].
Cervical cancer is still the most common female cancer globally and the leading cause of cancer deaths among females in Africa. It commonly occurs in women aged ranged from 25 to 65 years [3]. Among female cancers, cervical cancer is a leading cause of morbidity and mortality throughout the world, especially among women in Africa [4]. Of all the cancers, cervical cancer is the only one that has both an effective vaccine and screening program that can prevent disease and death [5].
Cervical cancer screening service is aimed at early detection and treatment of the disease [6]. In developed countries, the establishment of national screening programs with a population-based invitation of eligible women and a recall system for screen positives resulted in the prevention of almost 80% of cervical cancer [7]. Cervical cancer screening service utilization is recommended for effective methods for the prevention and early detection of cervical cancer [8]. Thus, evidence support the possibility to use specific biomarkers to identify early-stage cervical cancer (precancerous cervical lesion) which offer a better prognosis to the patients [9,10,11]. However, global evidence shows that the utilization of screening for prevention is very poor in developing countries. Lack of knowledge about cervical screening behavior among lower socio-economic status was found to be the primary barrier to the utilization of cervical cancer screening services [12, 13].
The introduction of Pap smear screening in western states reduce the incidence and mortality of cervical cancer. However cervical cancer still remains the main cause of death from cervical cancer in less developed settings where screening service utilization is scant or non-existent screening programs [10]. Recent evidence also showed that high risk Human Papilloma Virus (HPV) negative high grade abnormal type within a tissue of cervix have more improved results than patients with documented high risk HPV infection [10, 14]. Primary conization before radical hysterectomy for early-stage cervical cancer has also a potential protective role for patients with International Federation of Gynecology and Obstetrics (IFGO) stage IB1 cervical cancer [15, 16].
Cervical cancer is the fourth most common cancer accounting for 6.6% among women worldwide [17]. About 85% of the global burden and 87% of mortalities occur in developing countries. Of these, East African region is the top bookkeeping with an age-standardized incidence of 42.7/100,000 population and a mortality rate of 27.6/100,000 deaths [8]. In Ethiopia, it is the second most common female cancer with an incidence rate of 18.9/100,000 in 2018 [18]. Based on this public health significance, Ethiopia designed a strategic goal to reduce the incidence of cervical cancer and mortality by 15% by increasing the vaccination coverage against HPV [19]. To achieve its ambitious goals, cervical cancer screening services were being provided free for all eligible women since 2016 [20]. Despite the availability of guidelines for cervical cancer prevention and control; screening service was not fully utilized in all healthcare facilities [21]. The problem arose from inadequate knowledge about cervical cancer screening, limited treatment facilities,and too few government, and other stakeholders’ interventions [22]. As a result, most of the women in the country visit health institutions with the advanced stage of cervical cancer. Cervical cancer is the leading cause of cancer mortality among Ethiopian women over the age of 30 [23].
Cervical cancer screening has been shown as the most effective way to decrease cancer mortality among all women [24]. In Ethiopia, only 0.6% of all women, 1.6% of urban, and 0.4% of rural women aged 18–69 years screened every three years [25, 26]. The major factors associated with low cervical cancer screening were inadequate knowledge about the disease process, available screening methods, and client’s negative attitudes toward the procedure [17, 27, 28]. In Ethiopia, screening is usually conducted only when a woman seeks medical care for other reasons [29]. Regardless of the evidence that universal screening is important, women without symptoms are not routinely screened in many areas of Ethiopia [30]. Despite low cervical cancer screening service utilization in the country, evidence about the determinants of cervical cancer screening service utilization in Ethiopia, particularly in the study setting were scarce. Therefore, this study identified the determinants of cervical cancer screening service utilization among women attending health care services in Amhara region referral hospitals, in northwest Ethiopia.
Method and materials
Study setting and period
The study was conducted in referral hospitals of Amhara regional state, Northeastern and North-central part of Ethiopia. Amhara region is the second most populous region in Ethiopia. It has 12 zones, 3 city administrations, and 180 woredas. According to the Ethiopian Central Statistics Agency population projection, the region has a total population of 21.5 million people with a fifty-fifty numerical split between the sexes. Currently, the region has 84 hospitals (6 referrals, 14 general, and 64 primaries), 847 health centers, and 3,342 health posts [31]. The referral hospitals are the University of Gondar comprehensive and specialized referral hospital, Felege Hiwot comprehensive and specialized referral hospital, Debre Markos comprehensive and specialized referral hospital, Debre Berhan comprehensive and specialized referral hospital, Tibebe Gion, and Dessie comprehensive and specialized referral hospital. These referral hospitals are providing a broad range of services to outpatient, hospitalized patients and emergency cases including cervical cancer prevention services, and treatments. Each hospital is assumed to be serving 5.2 million people, has 200–400 beds, and around 1488 precancerous cases annually [32]. A hospital-based unmatched case–control study was conducted from May 1 to July 30, 2021.
Source and study population
All women attending health care services in Amhara region referral hospitals were the source population. All women attending health care services in the selected referral hospitals of the Amhara region during the study period were the study population. (Cases: were women who were newly utilizing screening services for cervical cancer during the study period. Controls: were women who visited the gynecologic outpatient department during the study period for other health services (other than cervical cancer screening service).
Eligibility criteria
For cases; all women who visited the gynecologic OPD for cervical cancer screening in the selected Amhara region referral hospitals during the study period were included in this study. For controls; all women who visited the gynecologic OPD other than cervical cancer screening in the selected Amhara region referral hospitals during the study period were included in this study. Women who were unable to hear and unconscious at the time of the study and those who were linked by health care professionals for cervical cancer screened by indication were excluded from the study.
Sample size determination
The sample size for the study was computed using Epi info version 7.2.3 software, by considering the following assumptions; 95% level of significance, 80% of power, the ratio of cases to controls 1:2, the proportion of exposure among controls 38.8%, Odds ratio 2.15, the proportion of cases with exposure 57.7% from a previous similar study conductedin Mekelle [33] and design effect of 1.5. Thus, the sample size for this study was 267, by considering a 10% non-response rate and design effect, the final sample size was 294*1.5 design effect = 441 individuals (147 cases and 294 controls).
Sampling procedure
From a total of six (6) referral hospitals in the Amhara region, three (3) of them were selected by simple random sampling technique (lottery method). The selected referral hospitals were Debre Birhan referral hospital, TibebeGion referral hospital, and Dessie referral hospital. The total sample size was allocated to each selected referral hospital by using probability proportionate to the average monthly client flow, reviewed from the registration book. Cases were selected consecutively, i.e. by including all women screened for cervical cancer during the data collection period until the required sample size is achieved and controls were selected using a systematic random sampling technique. The first respondent from the control was selected randomly from all women who visit the gynecologic outpatient department and the next participant was included after every fourth interval.
Study variables
Dependent Variable Cervical cancer screening utilization (Yes/No).
Independent Variables included socio-demographic, and economic characteristics (age, marital status, level of education, occupational status, family monthly income and place of residence), reproductive, sexual behavior, behavioral and obstetric related factors (contraceptive utilization, Parity, Smoking status, history of STI and Multiple sexual partners), Knowledge for cervical cancer screening and Attitudes for cervical cancer screening.
Operational definitions
Knowledge about Cervical cancer screening the study participants were asked 12 knowledge- assessing questions. These items comprise "Yes" or "No" and multiple response options. One point was given for all the correct answers, while zero points were for incorrect answers. Then, based on the summative score, women's knowledge was composed (of good knowledge which was coded as "1" and poor knowledge which was coded as "0"). Thus, participants with a score of mean and above were considered as good knowledge otherwise poor knowledge [34].
Positive attitude towards cervical cancer screening Women's attitude towards cervical cancer screening utilization was measured using 11 attitude assessing questions. Each question has five points Likert scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree). Women who scored mean and above value were considered to have a positive attitude and those who scored less than the mean value were considered a negative attitude [34].
Data collection tools and procedures
Data were collected by face-to-face interviews using structured, pretested questionnaires adapted from different kinds of literature [4, 33, 35, 36]. The questionnaire comprises questions on socio-demographic and economic status, attitude, knowledge, reproductive, behavioral, and sexual behavior characteristics of study participants. The questionnaire was first prepared in English and translated to the local language (i.e. Amharic) then back to English to keep its consistency. Data were collected by three trained BSc. degree midwives who are experienced in cervical cancer screening services and working at the Gynecologic clinic during the time of the data collection period. The data collection process was supervised by three BSc midwives who had research skills.
Data quality control
To make sure the quality of data, one-day training was provided for the data collectors and supervisors in each referral hospital about techniques of data collection. Close supervision was made during the whole period of data collection and checked each questionnaire for completeness and consistency on a daily basis. The questionnaire was pre-tested on 5% [22] of the study population at Felege Hiwot referral hospital (which was not included in the actual data collection) to check the understandability and reliability of the questionnaires.
Data processing and analysis
The collected data were checked for completeness and consistency and then each questionnaire was coded and entered into Epi Data version 4.6.0 software and exported to SPSS version 25.0 for analysis. The Hosmer–Lemeshow test was checked to evaluate whether the assumption for binary logistic regression was fulfilled or to evaluate model fitness. The test result revealed a P-value of 0.6, which indicates that the assumption is fulfilled and the model is fitted with data. Multicollinearity was checked using the variance inflation factor (VIF) and the output indicated that there was no multicollinearity. A bivariable logistic regression was done and variables with p-value < 0.2 in a bivariable analysis were entered into multivariable regression analysis to identify determinant factors. A variable with a P-value of < 0.05 in the multivariable analysis was considered a measure of statistically significant determinants. Adjusted odds ratio with its 95% confidence interval was used to measure the strength of association between variables. The results were described and presented by tables, graphs, and narrative descriptions.
Results
Socio-demographic characteristics of the participants
A total of 441 women (147 cases and 294 controls) participated in the study, giving a response rate of 100%. Nearly half (49.0%) of the controls and 44.2% of the cases were between the age categories of 21–29 and 30–39 years respectively. The mean and standard deviation of the age of the cases and controls was 28.7 ± 7.6 and 25.5 ± 5.9 years, respectively. One hundred fourteen (77.6%) of cases and two hundred fifty- five (86.7%) of controls were married. Concerning the occupational status of participants, 25 (17.0%) of cases and forty-two (14.3%) of controls were housewives. Regarding educational status of the participants, 65 (44.2%) of cases and 209 (71.1%) of controls had no formal education, whereas 33 (22.4%) of cases and 41 (13.9%) of controls had attained higher education. More than half (55.8%) of cases and the majority (89.1%) of controls were rural residents (Table 1).
Reproductive health-related characteristics of the participants
The majority of the study participants (88.4% of the cases and 89.4% of the controls) had their first sex at age of ≤ 18 years old. On the other hand, 128 (87.1%) of the cases and 127 (43.2%) of the controls had ever given birth. Sixty-four (43.5%) of the cases and 140 (47.6%) of the controls had ever used contraceptives. The Majority (83.0%) of the cases and (79.9%) of the controls had ever tested for HIV. Regarding the number of sexual partners, the majority (78.2%) of the cases and 135 (45.9%) of the controls had two or more sexual partners (Table 2).
Knowledge and attitude on cervical cancer and its screening
A majority (68.7%) of the cases and 112 (38.1%) of the controls had good knowledge about cervical cancer screening services. More than half (60.5%) of cases and 133 (45.2%) of controls had a positive attitude towards cervical cancer screening services (Table 3).
Determinants of cervical cancer screening service utilization
Bi-variable and multivariable logistic regression analysis was carried out to see the association between explanatory variables and the outcome of the interest. Variables with a p-value < 0.2 on bi-variable logistic regression were further run under Multivariable logistic regression. Accordingly, variables including age group (30–39, and 40–49 years), educational status (completed secondary, diploma and above), residing in urban residence, ever gave birth, having multiple sexual partners, good attitude and knowledge of cervical cancer were independent predictors of cervical cancer screening service utilization at a p-value of < 0.05 during multivariable analysis.
This study revealed that women being in the age group of 30–39 and 40–49 years were two times and four times more likely to utilize cervical cancer screening services than those who were in the age group of 21–29 years (AOR = 2.3; 95% CI 1.21, 4.68) and (AOR = 4.4; 95% CI 1.97, 10.12 respectively). Regarding educational status, women who completed secondary education and diploma and above were four times and two times more likely to utilize CCA screening services than those who had no formal education with (AOR = 4.4; 95% CI 2.18, 8.87) and (AOR = 2.0; 95% CI 1.05, 4.59 respectively). Participants who had ever given birth were nine times more likely to utilize cervical cancer screening services (AOR = 9.4, 95% CI 4.92, 18.26) than their counterparts. Women having multiple sexual partners were nearly three times more likely to utilize cervical cancer screening services (AOR = 2.8; 95% CI 1.60, 5.03) than their counterparts. On the other hand, participants with a positive attitude towards cervical cancer screening were two times more likely to utilize cervical cancer screening services than their counterparts (AOR = 2.0; 95% CI 1.20, 3.70). Women who live in urban areas were 2.6 times more likely to utilize cervical cancer screening services than their counterparts (AOR = 2.6; 95% CI 1.36, 5.21). Women who have good Knowledge were four times more likely to utilize cervical cancer screening services than their counterparts (AOR = 3.6; 95% CI 2.07, 6.43) (Table 4).
Discussion
Cervical cancer is one of the public health challenges, especially in developing countries. Primary prevention of cervical cancer is a far more feasible approach than secondary or tertiary management of cervical cancer. Identifying the determinants and designing and applying respective strategies are among such cost-effective approaches [37, 38]. In this regard, the current study revealed that the age group of 30–39 and 40–49 years, having multiple sexual partners, ever gave birth, urban residence, educational status and positive attitude towards cervical cancer screening services, and good knowledge towards cervical cancer were predictors of utilization of cervical cancer screening services.
In this study, in the age group of 30–39 and 40–49 years was significantly associated with utilization of cervical cancer screening services as compared to young women (21–29 years). This finding is consistent with the study conducted in Debre Markos, Mekelle, and Addis Ababa, Ethiopia [34, 38, 39]. It was also similar to the study findings in Debre Markos, Mekelle, age groups of 40–49 years had significantly higher odds of being screened [4, 33]. Besides, a study finding from Kenya, also indicated that women in the age groups of 40–49 years had significantly higher odds of being screened for cervical cancer [40]. Similarly, a study conducted in Addis Ababa, reported that willingness and acceptance of screening were higher among women in the age groups of 40–49, 50–59, and > 60 years as compared to those below 29 years[19]. This might be explained that women in higher age groups think themselves at risk of developing cervical cancer.
This study revealed that women with multiple sexual partners were 2.8 times more likely to utilize cervical cancer screening services. This is consistent with a study conducted in Debre Markos; which reported that women with a history of multiple sexual partners were 1.64 times more likely to undergo screening as compared to those who have no history of multiple sexual partners [34]. Another study conducted in Kenya showed that women with more than one- sexual partner were found to be two times more likely to utilize cervical cancer screening services compared to those with single sexual partner [40]. A study conducted in Yirgalem General Hospital, Ethiopia showed that having multiple sexual partners is significantly associated with knowledge of cervical cancer [41]. This can be explained by the fact that women with many sexual partners may perceive themselves to be more at risk for cervical cancer than others. Evidence supplemented that there is a positive association between multiple sexual partners and the development of the precancerous cervical lesion; thus, due to the sexually transmitted nature of HPV, perhaps reflecting a greater likelihood of utilization of screening services.
A positive attitude towards cervical cancer screening was significantly associated with cervical cancer screening services utilization. This finding is supplemented with studies conducted in Debre Markos, and Mekelle, Ethiopia which indicate that the odds of getting screened for cervical cancer were 3.4 times higher among women who had positive attitudes than those who had negative attitudes [33, 34]. Respondents who had negative attitude had 63% lesser odds of being screened compared to those who had positive attitudes towards screening in Nigeria [42]. Those studies were consistent with this study's finding in wolaita positive attitude were 4.8 times more likely to utilize cervical cancer screening than the counterpart [4]. This could be explained that a positive attitude is a precondition to accomplishing a certain task.
Women who had a degree/diploma level of education were 2.0 times more likely to utilize cervical cancer screening services compared with those who did not attend formal education. This is consistent with studies conducted in Dessie referral hospital, Debre Markos, Amhara region, and Addis Ababa, Ethiopia [19, 34, 39]. This finding is also consistent with studies conducted in Kenya, and Swedish which indicated that women who have educated were more likely to utilize cervical cancer screening services than those who had no formal education [40, 43]. This study also supplemented with a study conducted in Yirgalem general hospital, Ethiopia showed that women in secondary education level and degree and above levels were five times and seven times more likely to utilize cervical cancer screening services respectively than those who had no formal education [41]. This might be explained that educated women may have more knowledge of cervical cancer and screening services, and also have more information about cervical cancer screening services. As result, they might develop favorable attitudes and interest to get screened for CCA.
Moreover, in this study women who ever gave birth was nine times more likely to utilize cervical cancer screening services. This is similar to a study conducted at BahirDar which showed that multiparous women were 3 times more likely to utilize the services as compared to those with zero parity [37]. A study from Thailand, and Tanzania revealed a significant relationship between the number of children and cervical cancer screening utilization [44, 45]. This is in line with a study conducted at Yirgalem general hospital, Ethiopia which showed that multipara women were 3.4 times more likely to utilize cervical cancer screening services than their counterparts [41]. This might be explained by the fact that previous pregnancies of a woman may expose her to receive health education and particularly on sexual and reproductive health compared to those with no previous pregnancies.
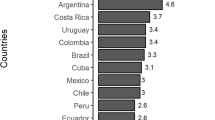
It is found that women living in urban residences were highly utilizing cervical cancer screening services with (AOR = 2.6, 95% CI 1.36, 5.21). This is consistent with a study conducted in Addis Ababa, Ethiopia which showed that women living in urban were 2 times more likely to utilize cervical cancer screening services than their counterparts [19]. This is in agreement with a study conducted in Kenya, and India which showed that women living in urban were 3.4 times more likely to utilize cervical cancer screening than those who were living in rural area [40, 46]. This might be due to the better availability of health facilities, closer to information, and accessibility of screening services in urban than rural areas.
Good knowledge of cervical cancer was significantly associated with CCA screening service utilization with (AOR = 3.6, 95% CI 2.07, 6.43). This is consistent with studies conducted at Debre Markos and Mekelle, Ethiopia which showed that women who had good knowledge of cervical cancer were 4 and 2.3 times more likely to utilize cervical cancer screening services than their counterparts [30, 41]. However, this finding is different from a study conducted in Tanzania which reported that women who had good knowledge were 3.3 times more likely to utilize cervical cancer screening services than those who had poor knowledge [45]. This might be due to having good knowledge about cervical cancer and its screening may interest in the utilization of cervical cancer screening services.
Implication for practice
In this study findings, as the determinants for cervical cancer screening service utilization were knowledge and attitude of women towards cervical cancer and its screening, this calls the healthcare authority should create awareness through information, education and communication (IEC), and behavioral change communication (BCC) through health information communication on usage of cervical cancer screening. It is hoped that this will also improve the knowledge and attitude of women. Policymakers like the Ethiopian Ministry of Health (MoH) should ensure that continuing education programs on the use of cervical cancer screening for the prevention of invasive cancer.
Strengths and limitations of the study
The authors would like to recommend that readers shall interpret certain findings of this study with precautions as recall and social desirability biases might be committed. However, this multi-center study provides valuable information about women’s cervical cancer screening service utilization determinants.
Conclusion
In this study, women in the age group of 30–39 and 40–49 years, educational status (completed secondary, diploma and above), urban residence, having multiple sexual partners, and ever giving birth were determinant factors to utilize cervical cancer screening services. Good knowledge about cervical cancer screening and a positive attitude towards cervical cancer screening were significantly associated with the uptake of cervical cancer screening services. Results should be considered when developing and implementing strategies to improve CCA screening service utilization in the region.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CCA:
-
Cervical cancer
- CIN:
-
Cervical intraepithelial Neoplasia
- HPV:
-
Human papillomavirus
- SPSS:
-
Statistical package for social science
- STD:
-
Sexually transmitted disease
- STI:
-
Sexual transmitted infection
- VIA:
-
Visual inspection with acetic acid
- WHO:
-
World health organization
- AOR:
-
Adjusted odds ratio
- COR:
-
Crud odds ratio
- CI:
-
Confidence interval
- BSC:
-
Bachelor of Science
References
John O, Schorge M et al. Williams’ gynecology. 2008. p. 20–30.
WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention, 2nd edn. WHO; 2020.
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Heal. 2020;8(2):e191-203.
Tekle T, Wolka E, Nega B, Kumma WP, Koyira MM. Knowledge, attitude and practice towards cervical cancer screening among women and associated factors in hospitals of Wolaita zone, southern Ethiopia. Cancer Manag Res. 2020;12:993–1005.
Adewole IF, Abauleth YR, Adoubi I, Amorissani F, Anorlu RI, Awolude OA, et al. Consensus recommendations for the prevention of cervical cancer in sub-Saharan Africa. S Afr J Gynaecol Oncol. 2013;5(2):47–57.
Gebremariam T. Human papillomavirus related cervical cancer and anticipated vaccination challenges in Ethiopia. Int J Health Sci. 2016;10(1):137–43.
Bhatla N, Singhal S, Saraiya U, Srivastava S, Bhalerao S, Shamsunder S, et al. Screening and management of preinvasive lesions of the cervix: Good clinical practice recommendations from the Federation of Obstetrics and Gynaecologic Societies of India (FOGSI). J Obstet Gynaecol Res. 2020;46(2):201–14.
Sangam S, Naveed A, Athar M, Prathyusha P, Moulika S, Lakshmi S. Understanding the screening behavior in mothers and adolescent daughter’s human papillomavirus vaccine uptake—the transtheoretical model. Int J Health Sci Res. 2015;5(1):156–64.
Yaya S, Olarewaju O, Oladimeji KE, Bishwajit G. Determinants of prenatal care use and HIV testing during pregnancy: a population-based, cross-sectional study of 7080 women of reproductive age in Mozambique. BMC Pregnancy Childbirth. 2019;19(1):1–10. https://doi.org/10.1186/s12884-019-2540-z.
Valenti G, Vitale SG, Tropea A, Biondi A, Laganà AS. Tumor markers of uterine cervical cancer: a new scenario to guide surgical practice? Updates Surg. 2017;69(4):441–9.
Calagna G, Maranto M, Paola C, Capra G, Perino A, Chiantera V, et al. ‘Secondary prevention’ against female HPV infection: literature review of the role of carrageenan. Expert Rev Anti Infect Ther. 2020;18(9):865–74. https://doi.org/10.1080/14787210.2020.1770082.
Carey MC, Grazia C, Mccarey C, Pirek D, Tebeu PM, Boulvain M, et al. Awareness of HPV and cervical cancer prevention among Cameroonian healthcare workers. 11.
Solomon D, Breen N, McNeel T. Cervical cancer screening rates in the United States and the potential impact of implementation of screening guidelines. CA Cancer J Clin. 2007;57(2):105–11.
Bogani G, Sopracordevole F, Di Donato V, Ciavattini A, Ghelardi A, Lopez S, et al. High-risk HPV-positive and -negative high-grade cervical dysplasia: analysis of 5-year outcomes. Gynecol Oncol. 2021;161(1):173–8.
Casarin J, Bogani G, Papadia A, Ditto A, Pinelli C, Garzon S, et al. Preoperative conization and risk of recurrence in patients undergoing laparoscopic radical hysterectomy for early stage cervical cancer: a multicenter study. J Minim Invasive Gynecol. 2021;28(1):117–23.
Bizzarri N, Pedone Anchora L, Cattani P, De Vincenzo R, Marchetti S, Conte C, et al. Peritoneal HPV-DNA test in cervical cancer (PIONEER study): a proof of concept. Int J Cancer. 2021;148(5):1197–207.
del González-Losa MR, Puerto-Solis M, Ruiz JT, Rosado-López AI, Hau-Aviles O, Ayora-Talavera G, et al. Analysis of E2 gene integrity in HPV16 and HPV58 viruses isolated from women with cervical pathology. Mem Inst Oswaldo Cruz. 2016;111(12):770–3.
Guvenc G, Akyuz A, Açikel CH. Health belief model scale for cervical cancer and pap smear test: psychometric testing. J Adv Nurs. 2011;67(2):428–37.
Ababa A, Fentie AM, Tadesse TB, Gebretekle GB. Factors affecting cervical cancer screening uptake, visual inspection with acetic acid positivity and its predictors among women attending cervical cancer screening service. 2020;1–10.
Gedefaw A, Astatkie A, Tessema GA. The prevalence of precancerous cervical cancer lesion among HIV-infected women in Southern Ethiopia: a cross-sectional study. PLoS ONE. 2013;8(12):1–8.
Tekalegn Y, Aman R, Woldeyohannes D, Sahiledengle B, Degno S. Determinants of VIA positivity among women screened for cervical precancerous lesion in public hospitals of Oromia region, Ethiopia: Unmatched Case-Control Study. 2020;587–96.
WHO. Comprehensive cervical cancer control. Geneva. 2014;366–78.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Chan CWH, Choi KC, Wong RS, Chow KM, So WKW, Leung DYP, et al. Examining the cervical screening behaviour of women aged 50 or above and its predicting factors: a population-based survey. Int J Environ Res Public Health. 2016;13(12):1195.
Ababa A. Knowledge, attitude, practice of cervical cancer screening and its associated factors among female students in Hawassa University College of Medicine and Health Science Hawassa Ethiopia, Addis Ababa, Ethiopia February, 2015;(July).
Wu LW, Lin LP, Chen SF, Hsu SW, Loh CH, Wu CL, et al. Knowledge and attitudes regarding cervical cancer screening among women with physical disabilities living in the community. Res Dev Disabil. 2012;33(2):376–81.
Eba B. Assessment of knowledge and attitude of cervical cancer and screening among primary health care workers of west Wollega Zone, Addis Ababa, Ethiopia. 2016;(May).
West S, Dirriba B, Rundasa DN. Research article cervical cancer screening and associated factors among women attending gynecology out -patient department and maternal and child health Atmettu. 2019;08(01):2934–44.
Gebrie MH. Knowledge, preventive practice and associated factors of female nurses? Towards cervical cancer in the selected government hospitals in Addis Ababa, Ethiopia. J Diabetes Metab. 2015;06:7.
Gurmu SE. Assessing survival time of women with cervical cancer using various parametric frailty models: a case study at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. Ann Data Sci. 2018;5(4):513–27.
HSFR/HFG Project. HSFR/HFG end of project achievement highlights—Amhara. Rockville, MD Heal Financ Gov Proj Abt Assoc. 2018;(June).
Adugna A. Demography and health. 2018.
Te H, Gebremariam L, Kahsay T, Berhe K, Gebreheat G, Gebremariam G. Factors affecting utilization of cervical cancer screening services among women attending public hospitals in Tigray region, Ethiopia, 2018; case control study. PLoS ONE. 2019;14(3):1–11.
Bante SA, Getie SA, Getu AA, Mulatu K. Uptake of pre-cervical cancer screening and associated factors among reproductive age women in Debre Markos town, Northwest Ethiopia, 2017. 2019;1–9.
Nega AD, Woldetsadik MA, Gelagay AA. Low uptake of cervical cancer screening among HIV positive women in Gondar University referral hospital, Northwest Ethiopia: cross-sectional study design. 2018;1–7.
Mekuria R. Cervical cancer screening behavior and associated factors among women attending gynecology out—patient department and maternal and child health at Dilla University referral ho. 2018;(June).
Muluneh BA, Atnafu DD. Predictors of cervical cancer screening service utilization among commercial sex workers in Northwest Ethiopia: a case-control study. 2019;1–9.
Taye BT, Mihret MS, Muche HA. Risk factors of precancerous cervical lesions: the role of women’s socio-demographic, sexual behavior and body mass index in Amhara region referral hospitals; case-control study. PLoS ONE. 2021;16(3):e0249218. https://doi.org/10.1371/journal.pone.0249218.
Heyi WD, Bekabil TT, Ebo GG. Knowledge, attitude and practice of cervical cancer screening among women aged 15–49 years in Bishoftu Town, East Shewa Zone, Oromia Region. 2018;10(2):42–52.
Ng’Ang’A A, Nyangasi M, Nkonge NG, Gathitu E, Kibachio J, Gichangi P, et al. Predictors of cervical cancer screening among Kenyan women: results of a nested case-control study in a nationally representative survey. BMC Public Health. 2018;18(Suppl 3).
Hospital G, Hailemariam T, Yohannes B, Aschenaki H, Mamaye E, Orkaido G, et al. Cancer science & therapy prevalence of cervical cancer and associated risk factors among women attending cervical cancer screening and diagnosis center at Yirgalem. 2017;9(11):730–5.
Titiloye MA, Womitenren YT, Arulogun OS. Barriers to utilization of cervical cancer screening services among women of reproductive age in Ondo, Southwest Nigeria. Afr J Biomed Res. 2017;20(3):229–35.
Broberg G, Wang J. Socio-economic and demographic determinants affecting participation in the Swedish cervical screening program: A. 2018;1–14.
Visanuyothin S, Chompikul J. Determinants of cervical cancer screening adherence in urban areas of Nakhon Ratchasima Province, Thailand. J Infect Public Health. 2015;8(6):543–52.
Kahesa C, Kjaer S, Mwaiselage J, Ngoma T, Tersbol B, Dartell M, et al. Determinants of acceptance of cervical cancer screening in Dar es Salaam, Tanzania. BMC Public Health. 2012;12(1):1.
Nene B, Jayant K, Arrossi S, Shastri S, Budukh A, Hingmire S. Determinants of women’s participation in cervical cancer screening trial, Maharashtra, India. 2007;031195(July 2006).
Acknowledgements
We would like to acknowledge Wollo University for ethical clearance. Our compliment is also great to the study participants, data collectors, and supervisors for their kind cooperation. We also want to appreciate the Amhara region health bureau and administrator of each selected hospital for the permission letter.
Funding
This study was funded by Wollo University, Ethiopia.
Author information
Authors and Affiliations
Contributions
TDL designed the study, developed data collection tools, performed the analysis and interpretation, and drafted the paper. KT, ZTA, MSC, FDB, JCF, ATT, BTT, and MAA participated in the development of the study proposal, analysis, and interpretation, revised drafts of the paper, and revised the final version of the manuscript. All authors read and gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from Wollo University College of medicine and health science and research Ethics Committee, Institutional Review Board (IRB). A formal letter of cooperation was written to each referral hospital from the Amhara regional health bureau and permission conduct to the study was obtained from the hospital administrators. Written informed consent was obtained from each study participant independently before the data collection. the study participants’ anonymity, privacy, and confidentiality were kept throughout the study process. Moreover, all methods were carried out followingthe Declaration of Helsinki.
Consent for publication
Consent for publication is not applicable.
Competing interests
The authors declare that there is no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Legasu, T.D., Temesgen, K., Ayele, Z.T. et al. Determinants of cervical cancer screening service utilization among women attending healthcare services in Amhara region referral hospitals: a case–control study. BMC Women's Health 22, 484 (2022). https://doi.org/10.1186/s12905-022-02071-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-02071-8