Abstract
Background
Excess weight (BMI ≥25.0 kg/m2) and weight gain during adult life increase the risk of postmenopausal breast cancer in women who are already at increased risk of the disease. Reasons for weight gain in this population can inform strategies for weight gain prevention.
Methods
Baseline data from six weight loss studies for women at increased risk of breast cancer (age 31–74 years) were collated. Self-reported patterns of adult weight gain and attributed reasons for weight gain before joining the weight loss study were reported for the whole population and secondary analyses reported the different reasons given by women with/without children, pre−/peri- or postmenopausal, and moderate/high risk of breast cancer.
Results
Five hundred and one women with a mean age of 47.6 (SD 8.4) years and median BMI of 29.9 (IQR 27.0–34.7) kg/m2 were included in the analyses. The median weight gain since young adulthood (18–20 years) was 20.5 (IQR 14.0–29.7) kg or 33.7 (23.4–50.2) % and median annual weight gain was 0.73 (IQR 0.51–1.08) kg. Four hundred and one women were included in analysis of weight gain reasons. The main five self-reported reasons for weight gain were children / childcare / pregnancy (stated by 55.9% of participants), followed by inactivity (41.9%), comfort or boredom eating (38.2%), portion size (32.4%), and stress (27.4%). Reasons appeared broadly similar between the different groups in the secondary analyses.
Conclusions
We have highlighted common reasons for weight gain in women at increased risk of breast cancer. This will inform future interventions to support women to avoid weight gain in adulthood which would reduce the burden of breast cancer.
Trial registration
NIHR NRR N0226132725, ISRCTN52913838, ISRCTN77916487, ISRCTN91372184, ISRCTN10803394 and ISRCTN16431108.
Similar content being viewed by others
Background
Excess weight (BMI ≥25.0 kg/m2) [1] and weight gain during adult life increases the risk of postmenopausal breast cancer [2, 3]. Currently in England, 60% of adult women are overweight including 29% with obesity [4]. Breast cancer is the most common cancer in women worldwide [5], and the second highest cause of cancer death in UK women [6]. It is estimated that 8% of UK breast cancers are caused by overweight and obesity [7], equating to around 4500 cases per year [6]. Various groups have highlighted young adulthood (18–35 years) as the main time for weight gain in women (summarised in [8] and recent additional data from a large English cohort [9]). In addition to increasing risk of breast cancer, weight gain during adulthood increases risk of diabetes, cardiovascular disease and other cancers in females [10].
A significant proportion of breast cancer cases, around 40%, are reported to occur in the 20% of women who are at increased risk (lifetime risk of breast cancer ≥17% [11] or 1 in 6 as defined by the Tyrer Cuzick model [12]). Targeting higher risk women with health behaviour interventions will have the biggest impact on reducing breast cancer rates. Observational studies have reported that the relative risks of higher BMI and adult weight gain apply equally to women already at increased risk of the disease, i.e. with a family history or high polygenic risk score, compared to lower risk women [13,14,15]. An Australian cohort study found that being overweight and obese is associated with a greater absolute increase in breast cancer risk amongst women already at high familial risk compared with women from the general population. They concluded that “maintaining a healthy weight throughout adult life is of clinical significance for all women, and especially those with a family history of breast cancer” [16].
Many women known to be at increased risk of breast cancer attend Family History, Risk and Prevention Clinics (FHRPCs) of which there are around 90 in the UK, including our own based at The Nightingale Centre, Manchester University NHS Foundation Trust (MFT). Analysis of BMI and health behaviour data from a sample of high risk women in our Manchester FHRPC (n = 136) highlighted the prevalence of unhealthy behaviours which were comparable to the general population, i.e. almost 60% had overweight or obesity, 30% did not meet physical activity (PA) recommendations, and 45% exceeded alcohol recommendations [17].
Since 2002 we have performed a number of weight loss intervention studies for women at increased risk of breast cancer with BMI ≥24 kg/m2 or weight gain > 10 kg since young adulthood. Findings of these studies have been published separately (Table 1). As part of the studies, baseline data was collected on 1) self-reported weight gain since the age of 18 or 20 years, and 2) women’s perceived reasons for this weight gain.
The aim of this paper is to report findings on the above two elements.
Methods
Data source
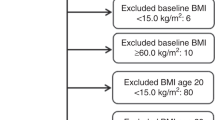
The analysis used anonymised baseline data from six weight loss studies conducted at the FHRPC between 2002 and 2019 (Fig. 1, n = 521) [18,19,20,21,22,23]. Inclusion criteria and details of ethics approvals and trial registry listings are given in Table 1.
Measures
Weight and height at study entry were measured as per standard protocols. Weight at age 18 or 20 was recalled by the participant. BMI at age 18 or 20 and entry was categorised as underweight (< 18.5 kg/m2), healthy weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2) [1]. Weight change since young adulthood (kg) is calculated as the difference between weight at joining the study, and young adulthood weight (18 or 20 years depending on study). Annual weight change was calculated as weight change since young adulthood (kg) / duration between young adulthood weight and study entry (years). Weight loss was defined as a loss of 5% or more between young adulthood and study entry [24], weight maintenance as maintaining between +/− 5% and the two weight gain categories were gaining 5–9.9%, or 10% or more. Participants reported their perceived opinions on reasons for weight gain using standard in-house questionnaires which included tick boxes for commonly occurring life events, psychological and physiological factors as well as actual diet and PA behaviours, with free text space for other reasons. Women could give more than one reason for weight gain. English Index of Multiple Deprivation was derived from postcodes [25].
Data inclusion
We included women at increased risk of breast cancer (i.e. ≥17% lifetime risk) and age ≥ 30 years as we were interested in weight gain from young adulthood. Duplicates were removed as women could enter more than one study. Data from the first study that they entered was included in the analyses. Analysis of weight gain reasons included women who had both gained ≥5% weight and given reasons for their weight gain. Two of the included studies also recruited women from outside of the FHRPC, but the majority of women recruited attended the Manchester FHRPC.
Statistical analysis
Descriptive statistics are presented with normally distributed data presented as mean (SD), otherwise median (IQR 25th–75th percentile) is used. Categorical data are presented as n (%). Reasons for weight gain are presented as a proportion of the included population stating each reason in descending order. Secondary analyses were run in sub-populations: those with / without children, pre / peri or postmenopausal at study entry, moderate risk of breast cancer (17–30% lifetime risk) / high risk of breast cancer (> 30% lifetime risk). Difference in reasons for weight gain between groups was compared using Pearson chi-square or Fisher’s exact tests. Bonferroni correction for multiple hypothesis testing was applied, by dividing the standard p-value by the number of comparisons made (0.05/30 = 0.0017). Analysis was performed using SPSS 25 (IBM, New York, USA).
Results
Included data are shown in Fig. 1. Women were excluded who were at low or average risk of breast cancer (i.e. < 17% lifetime risk, n = 104) aged and age < 30 years (n = 1). Duplicates were removed as n = 20 women had been in more than study. Uptake to and withdrawal from the included studies is described in the published papers [19,20,21, 26]. Upon joining the weight loss studies, the population had a mean age of 47.6 (SD 8.4) years and a median lifetime breast cancer risk of 29.0 (IQR 22.4–33.3) %. They were predominantly of white ethnicity (96%) and from the two least deprived quintiles (55%, Table 2).
In early adulthood (age 18–20 years), 74.6% had a healthy range BMI whilst only 7.4% were in the healthy BMI range at study entry (age 31–74 years, all ≥24 kg/m2 as per eligibility criteria for the weight loss studies, Table 1). Only 2.7% (12/469) of the population either lost weight or maintained within ±5% of their young adulthood weight while 95.3% gained ≥10% weight. The median annual weight gain was 0.73 (0.51–1.08) kg (Table 2).
Amongst participants who had gained ≥5% weight since young adulthood and provided reasons for weight gain (n = 401), the median number of reasons given per participant was 4 (IQR 2–6). Two thirds of women gave three or more reasons for their weight gain. The main reason given for weight gain was children / childcare / pregnancy (stated by 55.9% of participants), followed by inactivity (41.9%), comfort or boredom eating (38.2%), portion size (32.4%), and stress (27.4%, Table 3).
None of the comparisons between the subgroups reached statistical significance after adjustment for multiple hypothesis testing (results not shown). For the sub-cohort with no children (n = 72), the most common reason for weight gain was inactivity (stated by 56.9%). Comfort or boredom eating, portion size, stress, and work / study as reasons for weight gain were all given by a higher proportion of women with no children compared to women with children (54.2% vs. 34.9, 41.7% vs. 30.6, 36.1% vs. 25.7, 27.8% vs. 18.7% respectively) (Table 4).
For the sub-cohort who were peri/postmenopausal and who provided reasons for weight gain (n = 188), the proportion stating menopause / HRT as a reason for weight gain was 38.8% (Table 5). Peri/postmenopausal women were less likely to report children / childcare / pregnancy, work / study, and stress as reasons for their weight gain. For premenopausal women (n = 211), Menopause / HRT as a reason for weight gain had been replaced in the main ten reasons again by takeaways / ready meals.
Comparison of weight gain reasons between women with moderate (lifetime risk of breast cancer 17–30% and) versus high risk (> 30% lifetime risk) of breast cancer showed that the proportions of women at moderate risk stating many of the reasons were higher than amongst women at high risk of breast cancer (for example comfort or boredom eating 43.0 vs. 34.2%, portion size 37.0 vs. 29.0%) (Table 6). The main ten reasons for both groups differed only by the tenth reason which was depression for women at moderate risk, and takeaways / ready meals for women at high risk of breast cancer.
Discussion
In this analysis of women at increased risk of breast cancer who had joined weight loss studies in Manchester, most women gave multiple perceived reasons for their weight gain. The main causes of weight gain as perceived by the study participants were related to pregnancy and childcare, a lack of PA, and comfort and boredom eating. The predominant reasons for weight gain for sub-cohorts with/without children, pre/peri or postmenopausal and moderate/high risk of breast cancer were broadly similar.
Our recent review of weight gain in 18–35 year old women highlighted many of the reasons also reported in the current analysis [8]. Pregnancy and motherhood are amongst the life events associated with the largest amount of weight gain, with women in the UK weighing a mean of 3.5 (SD 6.2) kg heavier than their pre-pregnancy weight at 6 months postpartum (n = 12,583) [27]. Motherhood is associated with a decrease in levels of PA [28, 29], mainly due to lack of time [30,31,32], which could contribute to further weight gain after pregnancy. This aligns with the current findings as children / childcare / pregnancy was the major reason given by women for their weight gain in both the whole cohort (56%) and the sub-cohort with children (68%). Inactivity was the next most cited reason by 43% of the whole cohort. Figures for England state that 34% of adult females (age 19–84) do not meet government guidelines for physical activity [33] (> 150 min of moderate or 75 min of vigorous intensity activity per week, or a combination of both) and a summary of evidence by the World Cancer Research Fund showed that there was convincing evidence that walking protects against weight gain and probable evidence for aerobic PA [34].
Thirty-two percent of women gave portion size as a reason for their weight gain. The link between portion size and weight gain is complex due the effects of other factors such as energy density and frequency of consumption, but reviews of the literature suggest that there is enough evidence to implicate portion size as an important component in the development of overweight and obesity [35, 36].
Finding effective ways to support women avoid weight gain during adulthood is a priority for women identified at increased risk of breast cancer. Our recent review summarised previous research into behavioural weight gain prevention interventions but none are targeted to this population [8]. The present results indicate that weight gain prevention programmes for this population should cover the same issues as those targeting the general population. Interventions based around pregnancy and postpartum have the strongest evidence base and a number of interventions could progress to practice. Evidence for interventions targeting other life events or general weight gain in young women is weaker and hampered by poor quality studies [8]. In addition to a standard behavioural approach to prevent weight gain, other emerging weight management methods such as third-wave cognitive behaviour therapies [37] and pharmacotherapy, for example GLP-1 receptor agonists in reduced doses [38], may also be effective in the field of weight gain prevention.
Strengths
The strength of the current analysis is that combining data from a number of studies increased the sample size to over 500 women, with the majority (85%) providing reasons for weight gain. This is the first overview of reasons for weight gain specific to the population of women at increased risk of breast cancer.
Limitations
There is likely to be an overlap between many of the reasons provided, i.e. inactivity is often attributed to lack of time which is commonly associated with motherhood and childcare [30,31,32]. Lower PA is also associated with marriage and cohabiting in women [39, 40]. Comfort or boredom eating (mentioned by 38% of the cohort) is often associated with stress (27%) and depression (16%) [41].
The generalisability of the findings to high-risk populations is limited for a number of reasons. Women joined the included studies because they were interested in losing weight by joining dietitian-led weight loss programmes. The majority of participants were white and the population was skewed towards the least deprived quintile, as is a recognised problem in health research [42].
Weight at study entry was reliably measured as per study protocols on calibrated scales, however weight in young adulthood was recalled therefore could be inaccurate, although studies have shown recalled weights to be fairly accurate on a population level [43].
Providing tick box options could have been leading and altered results, for example attending university is often associated with weight gain in women [44, 45] but was not included in the tick boxes which may explain why it was not mentioned by any of the study participants. Other known mediators of weight gain which were not in the questionnaire include lack of knowledge and skills around food and cooking, anxiety, and neural responses [8]. Primacy bias, where respondents are more likely to choose the first few response options when presented with a list, could also have affected the present results. Women could select multiple reasons for weight gain with no weighting given therefore all reported reasons were given equal weight and analysis was performed on frequency. This may have resulted in a loss of detail regarding the relative importance of each reason but it may be unfeasible to ask women to retrospectively recall the amount of weight gain linked with the different reasons. Some of the sub-cohorts we analysed were small, for example there were only 76 women with no children.
We were unable to compare reasons between high risk and population risk women. Only two of the six trials also included population-risk women so as there was not a large enough pool of these women. A stronger study design would have included adequate numbers of women in both groups to allow statistical comparison but it is interesting that the current results show similar findings to the literature about the general female population.
Conclusions
Limiting weight gain that is frequently experienced by young women could reduce the burden of breast cancer and other diseases. Our analysis has highlighted common reasons women at increased risk of breast cancer attribute to their gain weight. This will help inform the design of future interventions to support women to avoid weight gain. Future research should focus on developing and testing such interventions thus reducing weight gain particularly in women identified at increased risk of breast cancer which will lead to a reduction in the burden of breast cancer.
Availability of data and materials
The datasets analysed for this article are available in the Figshare repository (https://doi.org/10.48420/19614531.v1), apart from the Lifestyle Study for which the dataset is not publicly available as participants on this study did not consent to anonymous data sharing.
References
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. 1995.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K, et al. Body fatness and cancer--viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794–8.
World Cancer Research Fund, American Institute for Cancer Research. Continuous Update Project Expert Report. Diet, nutrition, physical activity and breast cancer. 2018.
NHS Digital. Health survey for England 2019. 2020. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2019. Accessed 17 Aug 2022.
World Cancer Research Fund, American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective. A summary of the Third Expert Report. 2018.
Cancer Research UK. Cancer mortality statistics. 2021. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/mortality. Accessed 17 Aug 2022.
Brown KF, Rumgay H, Dunlop C, Ryan M, Quartly F, Cox A, et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer. 2018;118(8):1130–41.
Pegington M, French DP, Harvie MN. Why young women gain weight: a narrative review of influencing factors and possible solutions. Obes Rev. 2020;21(5):e13002.
Katsoulis M, Lai AG, Diaz-Ordaz K, Gomes M, Pasea L, Banerjee A, et al. Identifying adults at high-risk for change in weight and BMI in England: a longitudinal, large-scale, population-based cohort study using electronic health records. Lancet Diabetes Endocrinol. 2021;9(10):681–94.
Colditz G, Coakley E. Weight, weight gain, activity, and major illnesses: the Nurses’ Health Study. Int J Sports Med. 1997;18(S 3):S162–S70.
NICE. Clinical guideline CG164. Familial breast cancer classification, care and managing breast cancer and related risks in people with a family history of breast cancer. 2013.
Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23(7):1111–30.
Maas P, Barrdahl M, Joshi AD, Auer PL, Gaudet MM, Milne RL, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol. 2016;2(10):1295–302.
Arthur RS, Wang T, Xue X, Kamensky V, Rohan TE. Genetic factors, adherence to healthy lifestyle behavior, and risk of invasive breast cancer among women in the UK biobank. J Natl Cancer Inst. 2020;112(9):893–901.
Gramling R, Lash TL, Rothman KJ, Cabral HJ, Silliman R, Roberts M, et al. Family history of later-onset breast cancer, breast healthy behavior and invasive breast cancer among postmenopausal women: a cohort study. Breast Cancer Res. 2010;12(5):R82.
Hopper JL, Dite GS, MacInnis RJ, Liao Y, Zeinomar N, Knight JA, et al. Age-specific breast cancer risk by body mass index and familial risk: prospective family study cohort (ProF-SC). Breast Cancer Res. 2018;20(1):132.
Pegington M, Evans DG, Howell A, Donnelly LS, Wiseman J, Cuzick JM, et al. Lifestyle behaviours and health measures of women at increased risk of breast cancer taking chemoprevention. Eur J Cancer Prev. 2019;28(6):500–6.
Ong KR, Sims AH, Harvie M, Chapman M, Dunn WB, Broadhurst D, et al. Biomarkers of dietary energy restriction in women at increased risk of breast cancer. Cancer Prev Res. 2009;2(8):720–31.
Harvie MN, Sims AH, Pegington M, Spence K, Mitchell A, Vaughan AA, et al. Intermittent energy restriction induces changes in breast gene expression and systemic metabolism. Breast Cancer Res. 2016;18(1):57.
Harvie M, Pegington M, French D, Cooper G, McDiarmid S, Howell A, et al. Breast cancer risk status influences uptake, retention and efficacy of a weight loss programme amongst breast cancer screening attendees: two randomised controlled feasibility trials. BMC Cancer. 2019;19(1):1089.
Harvie M, Renehan AG, Frystyk J, Flyvbjerg A, Mercer T, Malik R, et al. Increase in serum total IGF-I and maintenance of free IGF-I following intentional weight loss in pre-menopausal women at increased risk of breast cancer. Open Obes J. 2010;2:63–70.
Harvie MN. ISRCTN record: BRRIDE 2 - Breast Risk Reduction Intermittent Diet Evaluation. ISRCTN10803394. 2015. Available from: https://www.isrctn.com/ISRCTN10803394.
Harvie MN. ISRCTN record: family history lifestyle study. ISRCTN16431108. 2017. Available from: https://www.isrctn.com/ISRCTN16431108.
Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Executive summary: guidelines (2013) for the management of overweight and obesity in adults. Obesity. 2014;22(S2):S5–S39.
Office for National Statistics. Postcode directories: UK data service census support. 2021. Available from: https://geoconvert.ukdataservice.ac.uk/. Accessed 17 Aug 2022.
Harvie M, Wright C, Pegington M, McMullan D, Mitchell E, Martin B, et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br J Nutr. 2013;110(8):1534–47.
Hollis JL, Crozier SR, Inskip HM, Cooper C, Godfrey KM, Harvey NC, et al. Modifiable risk factors of maternal postpartum weight retention: an analysis of their combined impact and potential opportunities for prevention. Int J Obes. 2017;41(7):1091–8.
Brown WJ, Trost SG. Life transitions and changing physical activity patterns in young women. Am J Prev Med. 2003;25(2):140–3.
Perales F, del Pozo-Cruz J, del Pozo-Cruz B. Long-term dynamics in physical activity behaviour across the transition to parenthood. Int J Public Health. 2015;60(3):301–8.
Evenson KR, Aytur SA, Borodulin K. Physical activity beliefs, barriers, and enablers among postpartum women. J Womens Health. 2009;18(12):1925–34.
Larouche R, Laurencelle L, Shephard RJ, Trudeau F. Life transitions in the waning of physical activity from childhood to adult life in the Trois-Rivieres study. J Phys Act Health. 2012;9(4):516–24.
Owen N, Bauman A. The descriptive epidemiology of a sedentary lifestyle in adult Australians. Int J Epidemiol. 1992;21(2):305–10.
NHS Digital. Statistics on obesity, physical activity and diet, England, 2020. 2020.
World Cancer Research Fund, American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Diet, nutrition and physical activity: energy balance and body fatness. 2018.
Livingstone MBE, Pourshahidi LK. Portion size and obesity. Adv Nutr. 2014;5(6):829–34.
Ello-Martin JA, Ledikwe JH, Rolls BJ. The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr. 2005;82:236S–41S.
Lawlor ER, Islam N, Bates S, Griffin SJ, Hill AJ, Hughes CA, et al. Third-wave cognitive behaviour therapies for weight management: a systematic review and network meta-analysis. Obes Rev. 2020;21(7):e13013.
Shi Q, Wang Y, Hao Q, Vandvik PO, Guyatt G, Li J, et al. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. Lancet. 2022;399(10321):259–69.
Bell S, Lee C. Emerging adulthood and patterns of physical activity among young Australian women. Int J Behav Med. 2005;12(4):227–35.
Dowda M, Ainsworth BE, Addy CL, Saunders R, Riner W. Correlates of physical activity among US young adults, 18 to 30 years of age, from NHANES III. Ann Behav Med. 2003;26(1):15–23.
Laitinen J, Ek E, Sovio U. Stress-related eating and drinking behavior and body mass index and predictors of this behavior. Prev Med. 2002;34(1):29–39.
Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. 2014;14(1):42.
Dahl AK, Reynolds CA. Accuracy of recalled body weight-a study with 20-years of follow-up. Obesity. 2013;21(6):1293–8.
Vadeboncoeur C, Townsend N, Foster C. A meta-analysis of weight gain in first year university students: is freshman 15 a myth? BMC Obes. 2015;2:22.
Meisel SF, Beeken RJ, van Jaarsveld CH, Wardle J. The association of FTO SNP rs9939609 with weight gain at university. Obes Facts. 2015;8(4):243–51.
Acknowledgements
We thank the women who participated in, and the research staff who worked on the included studies.
Funding
Funding for the included studies is detailed in Table 1. None of the funding bodies played a role in the design of the study and collection, analysis, and interpretation of data or in writing this manuscript. MP and DGE are supported by the National Institute for Health Research (NIHR) Manchester Biomedical Research Centre (BRC1215–20007). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
Conception of the studies (MP, MH, DGE, AH), design of the work (MP, MH, EH), acquisition of data (MP, MH), analysis of data (MP), interpretation of data (MP, MH, EH), drafting the work (MP). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All studies were performed in accordance with the Declaration of Helsinki and relevant guidelines and regulations. All participants in the included studies provided informed consent. NHS Research Ethics Committee approvals for each study were as follows: Lifestyle: South Manchester REC (ref: 01/426), IER vs CER diets: Bolton (Lancashire) Local REC (ref: 05/Q1409/42), BRRIDE: North West 10 REC, Greater Manchester North (ref: 09/H1006/33), PROCAS-Lifestyle: NRES Committee West Midlands–Solihull (ref: 14/WM/1088), BRRIDE 2: NRES Committee South Central - Oxford B (ref: 14/SC/1097), Family History Lifestyle: North West - Preston Research Ethics Committee (ref: 17/NW/0440).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pegington, M., Harkness, E.F., Howell, A. et al. Magnitude and attributed reasons for adult weight gain amongst women at increased risk of breast cancer. BMC Women's Health 22, 447 (2022). https://doi.org/10.1186/s12905-022-02037-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-02037-w