Abstract
Introduction
Globally, in 2019, there are 1.9 billion women of reproductive age (15–49), of which 1.1 billion have a need for family planning. Of these, 842 million use contraceptives, and 270 million still have an unmet need for contraception. Ethiopia is a low-income country with inadequate access to family planning (FP), especially in the developing regions. The Ethiopian government was striving to increase the number of health facility in order to provide quality maternal care and services. Increasing the modern contraceptive prevalence rate is one of the goals of the government to reduce maternal and child mortality and morbidity.
Methods
Secondary data analysis was conducted using data from mini-EDHS of 2019 demographic and health Survey datasets. The study comprised a total of 8885 reproductive-age women. Spatial variations and multilevel mixed effect analysis on determinants factors of modern contraceptive use among reproductive age women in Ethiopia; evidenced by mini-EDHS 2019. Finally, the percentage and odd ratio, its 95% confidence intervals, and the result of spatial analysis were reported.
Result
This study includes a total weighted sample of 8885 reproductive-age women from the 2019 mini-Ethiopian demographic and health survey. The prevalence of modern contraceptive use was 25.5% in Ethiopia. living in urban area [AOR = 2.13; 95% CI = (1.75, 2.61); P = 0.000], being married [AOR = 1.42; 95% CI = (1.19, 1.70); P = 0.000] were found positively associated with contraceptive use. In contrast to this, attending primary education [AOR = 0.91; 95% CI = (0.74, 1.12); P = 0.000]., being Muslim [AOR = 0.25; 95% CI = (0.22, 0.29); P = 0.000], being poorest [AOR = 0.54; 95% CI = (0.45, 0.66); P = 0.000] were found negatively associated with contraceptive use.
Conclusion
In this study Individual and community level factors were associated with modern contraceptive use and also there were spatial variations in modern contraceptive use across the region among reproductive-age women. Empowering women to have better educational status, improving the wealth index, promoting marriage, creating awareness among rural residences women and promoting education about modern contraceptives through religiously acceptable persons, and promoting modern contraceptive use in developing regions were the key factors to improve modern contraceptive use among reproductive age women in Ethiopia.
Similar content being viewed by others
Introduction
The purposeful avoidance of pregnancy by the use of different techniques, sexual practices, drugs, medications, or surgical procedures is known as contraception [1]. Contraceptive methods are usually divided into modern and traditional categories. Traditional methods of contraception include the lactational amenorrhoea method, the rhythm method (periodic abstinence), withdrawal (coitus interruptus), and folk methods [2]. A modern contraceptive method is a drug or medical treatment that prevents sexual activity from leading to pregnancy [3]. modern contraceptive methods include barrier methods such as male and female condoms, diaphragm, cervical cap and sponge; hormonal contraceptives that include oral, injectable, transdermal, vaginal ring, and implants; intrauterine device (IUD) [4]. The majority of contraceptives used globally are modern methods. A modern method of family planning was used by 58% of married or in-union women of reproductive age worldwide in 2017, accounting for 92% of all contraceptive users [5]. According to the Ethiopian Mini Demographic and Health Survey of 2019 report, currently married women’s use of modern contraceptives has continuously risen from 2005, from 14 to 41% [6].
There are a variety of benefits to contraceptives, including those for women’s empowerment, maternal and child health, economic growth, and education [7]. Additionally, the modern methods of contraceptive are crucial for reducing unintended pregnancies, delaying births, and improving neonatal and child survival rates since there will be more time for good parenting and child care [8]. Several literature demonstrated that the use of modern contraceptives is influenced by a variety of factors, including age, education, communication between couples about FP, the number of living children, husband approval of FP, the intended number of children, place of residence, religion, knowledge, and attitudes [9,10,11].
A Bayesian hierarchical modeling study which was conducted by Vladimíra.etal in 2020, demonstrated that currently there are 1.9 billion women in the globe who are of reproductive age [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46], of whom 1.1 billion require family planning, and the number of women in this age group is predicted to rise. Of them, 842 million utilize contraceptives and 270 million still require contraceptives, which is still not being met [47]. To enhance women’s sexual and reproductive health, non-governmental organizations and the government are now working together in Ethiopia to provide outreach programs that provide contraceptives [48]. Since then, a health sector transformation plan (HSTP) has been formed by the Federal Ministry of Health (FMoH) to raise the contractive prevalence rate. But the demand for modern contraception was unsatisfied [49]. Due to the higher unmet demand and lower usage of modern contraceptives, women are likely experiencing unintended and untimely pregnancies. Unwanted pregnancy has a variety of negative effects on a woman’s health and economic development. For example, it increases maternal mortality, encourages prenatal depression, stunts children’s growth because of malnutrition caused by frequent births, compromises the bond between the mother and child, and lowers women’s participation in the workforce and politics [12,13,14,15].
In Ethiopia due to the lack of updated and reliable figures on spatial variation of modern contraceptive, it is difficult to establish policies and programs for the promotion of modern contraceptive use and to take an intervention to decrease unmet need of modern contraceptive use across the region. Therefore, the major goal of this study was to evaluate spatial variations in modern contraceptives use and the contributing factors among women of reproductive age Ethiopia. It is expected to have the following significance.
The document was used to access spatial variations of modern contraceptive use and determinants factors of modern contraceptive use. Therefore, it is important for the stakeholders to understand various factors that affects modern contraceptive use. Additionally, the findings of this study would provide better evidence for policymakers, ministry of health and other stakeholders, which in turn might enable designing and executing appropriate interventions at different levels to increase the rate of modern contraceptive usage, to reduce unmet need of modern contraceptive and to improve the health system as a whole.
Methods and data source
Study design, setting and period
The secondary data for this analysis were obtained from mini-Edhs of 2019 that was found at DHS portal of (https://dhsprogram.com/data/dataset/Ethiopia_Interim-DHS_2019.cfm?flag=1). The 2019 EMDHS sample was stratified and selected in two stages. Each region was stratified into urban and rural areas, yielding 21 sampling strata. Samples of EAs were selected independently in each stratum in two stages. To ensure that survey precision was comparable across regions, sample allocation was done through an equal allocation where in 25 EAs were selected from eight regions. However, 35 EAs were selected from each of the three larger regions: Amhara, Oromia, and the Southern Nations, Nationalities, and Peoples’ Region (SNNPR). In the first stage, a total of 305 EAs (93 in urban areas and 212 in rural areas) were selected with probability proportional to EA size (based on the 2019 EPHC frame) and with independent selection in each sampling stratum. A household listing operation was carried out in all selected EAs from January through April 2019. The resulting lists of households served as a sampling frame for the selection of households in the second stage. In the second stage of selection, a fixed number of 30 households per cluster were selected with an equal probability systematic selection from the newly created household listing. All women age 15-49 who were either permanent residents of the selected households or visitors who slept in the household the night before the survey were eligible to be interviewed. In all selected households, women age 15-49 were interviewed using the Woman’s Questionnaire. A total of 9150 households were selected for the sample, of which 8794 were occupied. Of the occupied households, 8663 were successfully interviewed, yielding a response rate of 99%. In the interviewed households, 9012 eligible women were identified for individual interviews; interviews were completed with 8885 women, yielding a response rate of 99%. Overall, there was little variation in response rates according to residence; however, rates were slightly higher in rural than in urban areas. From 8885 interviewed women,5934 were from rural area and the remaining 2951women were from urban area [6]. Since the outcome variable for this study was modern contraceptive utilization .so, the final sample size for this analysis was 8885.
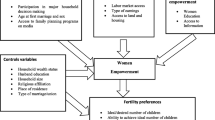
Study variables
The outcome variable for this study was the modern contraceptive use, which was coded as “0” if the women use modern contraceptive and “1” if the women not use modern contraceptive (No method, Folkloric method, Traditional method).
Individual-level variable: maternal age, educational status, religion, sex of household, wealth status, current marital status and number of children.
Community-level variable: Region and place of residence.
Inclusion and exclusion criteria
All women who were found within the range of reproductive age groups (15-49 years) included in this study. All women who were outside the range of the reproductive age group (15-49 years) excluded from this analysis.
Data management and analysis
In all the analyses, we adjusted for the complex nature of the survey design by accounting for clustering, stratification, and weighting. Due to the comparisons and combination (pooled data) of surveys from different regions, with different target population sizes, the weights were denormalized. This was done by dividing the women’s standard weights and their total number the country by the respective survey sampling fraction. Data Extraction, recoding, and both descriptive and analytical analysis were carried out using STATA version 14 software. The multilevel analysis was fitted due to the hierarchical nature of the demographic health survey data. In this study, the multilevel mixed-effects model was employed and the dependent variable was binary.
The Intraclass Correlation Coefficient (ICC) was employed to assess the variability across the region. Bi variable analysis was first done for maternal age, region, place of residence, educational status, religion, sex of household, wealth status, current marital status and number of children, to select variables for multivariable analysis and variables with p-value less than 0.05 were considered for multivariable analysis.
Spatial analysis
In Stata 14, the weighted frequency of modern contraceptives, cluster number, and geographic coordinate data were combined. Data was then exported to Excel and imported into ArcGIS 10.7 for spatial analysis.
Spatial autocorrelation analysis
The spatial autocorrelation (Global Moran’s I) statistic examines the distribution of modern contraceptives usage among Ethiopian women of reproductive age. Moran’s I is a spatial statistic that uses the entire data set to generate a single output value that varies from − 1 to + 1 in order to evaluate spatial autocorrelation. I, Moran’s Values around − 1 suggest scattered modern contraceptive usage, whereas values near + 1 indicate clustered modern contraceptive use, and values near 0 indicate random distribution of modern contraceptive use. A statistically significant Moran’s I (p < 0.05) lead to the failure to reject the alternative hypothesis and rejection of the null hypothesis (modern contraceptive use is randomly distributed) and indicates the presence of spatial autocorrelation.
Hot spot analysis (Getis-OrdGi* statistic)
The GI* statistics for each area were computed to determine how spatial autocorrelation varies in Ethiopia using Getis-OrdGi* statistics. The p-value is estimated for significance using Z-score in order to determine the statistical significance of clustering. High GI* statistical output suggests a “cold area,” whereas low GI* statistical output indicates a “hot spot.”
Spatial interpolation
To determine the impact of a particular event throughout the country, it is highly expensive and time-consuming to gather trustworthy data. As a result, using the observed data, interpolation was utilized to estimate a portion of a certain area. Based on sampled EAs from DHS, the spatial interpolation approach forecasts modern contraceptive usage in the un-studied portions of the country. In this work, modern contraceptive use in unobserved regions of Ethiopia was predicted using the standard Kriging spatial interpolation approach. The burden of modern contraceptive usage in unsampled regions was estimated for this study using the standard Kriging approach.
Ethical consideration
The measure DHS program used secondary publically accessible survey data, thus ethical review and participant permission were not required for this particular study. We asked DHS Program for permission to obtain and use the data for this study from their website, and they approved. The National Research Ethics Review Committee (NRERC) of the Ministry of Science and Technology as well as the Ethiopian Health Nutrition and Research Institute (EHNRI) Review Board granted clearance for the EMDHS data collection.
Result
Sociodemographic characteristics and bivariate analysis
This study includes a total weighted sample of 8885 reproductive age women from the 2019 mini-Ethiopian demographic and health survey. 2210 (24.9%) of the total study participants were between the age range of 15-19 years, 6024(67.8%) were from rural areas, 3701 (41.7%) were not attending formal education, 3685(41.5%) were orthodox, 7050 (79.3%) were male headed household, 268 (11.9%) were poorest 5743 (64.6%) participants. Were married and 2262(25.5%) use modern contraceptive. Bivariable logistic regression was employed for age, place of residence, religion, educational status, sex of household, wealth index current marital status, among reproductive age women. The result of the bivariable analysis demonstrated that contraceptive use had significant relationships with age, place of residence, religion, educational status, sex of household, wealth index, current marital status among reproductive age women. Variables having a p-value less than 0.05 were considered in multivariate analysis. (Table 1).
Spatial analysis results
Spatial distribution of modern contraceptive use
In Ethiopia, modern contraception use was analyzed geographically using 305 clusters. The number of current contraceptive usage instances in each cluster corresponds to one enumeration area at each spot on the map. This study’s analysis of the spatial distribution of modern contraception use showed that a higher proportion was used in Ethiopia’s northern region. The southern region of Ethiopia had a low rate of modern contraception usage Fig. 1.
Spatial autocorrelation modern contraceptive use
The spatial autocorrelation result reveals whether modern contraception use in Ethiopia is randomly distributed across the region, clustered, or dispersed. The results of the spatial autocorrelation study showed a clustering effect in the use of modern contraceptives across the country. The clustered patterns (on the right’s red box side) demonstrated a clustering effect on the usage of modern contraceptives in Ethiopia. The outputs have automatically generated keys on the right and left sides of each panel. The probability that this clustered pattern is the result of random chance is less than 1%, according to the z-score of 31.07 (p-value = 0.001). The bright red and blue colors to the end tails indicate an increased level of significances Fig. 2.
The hotspot analysis result
The hotspot analysis result shows the low proportion (hotspot) and high proportion (cold spot) areas of modern contraceptives use in Ethiopia. The blue colors were seen in the Tigray, Afar, Amhara, and northern part of Oromia regional states, which are cold spot areas (high proportion of modern contraception use). The red-colored hotspots (areas with a low percentage of women using modern contraceptives) were found in Gambella, SNNPRS. A region of Oromia, Diredawa, and Harari Fig. 3.
Spatial interpolation or prediction
Based on the sampled region, the spatial interpolation approach predicts the proportion of modern contraceptive use for unsampled areas. The area map was described using the standard Kriging method. The red color represents the projected low use of modern contraceptives. If the area’s color shifted from red to blue, it indicates that more people in the area are using modern contraceptives than was previously expected. The country is predicted to utilize modern contraceptives at a high rate, as shown by the blue color. According to the prediction’s results, Tigray, Afar, Amhara, and several areas of Oromia have high rates of modern contraception utilization. The red color prediction showed that the regions of Gambella, Benishangul, SNNPR, Oromia, Somalia, Harari, and Diredawa had the lowest rates of modern contraception usage nationwide Fig. 4.
Model comparison
Four models were built for this multistage investigation. The first model was built. Without independent factors, it is possible to determine how community variation affects women’s usage of modern contraceptives. The second model included variables at the individual level. Community level characteristics were incorporated in the third model. Finally, the fourth model took into account factors at both the individual and community levels. The ICC in the null model showed that among women of reproductive age, there was a variance in contraceptive usage of 9.97% in the communities. The variance in contraceptive usage among women of reproductive age is described by variables at the individual level in 17.62% of occurrences. The difference in contraceptive usage among women of reproductive age is accounted by 12.35% community level variables. In the end, 19.47% of the variances among women in reproductive age were caused by variables at the individual and community levels. Deviance was used to evaluate model fitness for model comparison (AIC). As a result, it was determined that Model IV, which included factors at both the individual and community levels and had the lowest deviance (AIC) value, provided the best suit. Variables having a p < 0.05 significance level were considered to be significant predictors of current modern contraceptive usage among reproductive-age women. Table 2.
Pearson Chi-Square analysis of factors associated with modern contraceptive use
The Pearson Chi-square analysis was employed for age, place of residence, religion, educational status, sex of household head, wealth index current marital status, among reproductive age women. The result of the Pearson Chi-square analysis demonstrated that contraceptive use had significant association with place of residence, religion, educational status, sex of household, wealth index, current marital status among reproductive age women. Table 3.
Multivariable logistic regression
According to the result of the multivariable regression the key variables related with modern contraceptive use among reproductive age women were women’s age, place of residence, educational status, religion, sex of household head, wealth index, current breast feeding and current marital status. The odd of using modern contraceptive among reproductive age women who were live in urban area were two times more likely [AOR = 2.13; 95% CI = (1.75, 2.61); P = 0.000] relative to women who were live in the rural area. The odd of modern contraceptive use among reproductive age women who were attending primary education were 0.91 times less likely to use modern contraceptive [AOR = 0.91; 95% CI = (0.74, 1.12); P = 0.000] compared to women who were attending higher education. The odd of modern contraceptive use among reproductive age women who were Muslim were 0.25 times less likely to use modern contraceptive [AOR = 0.25; 95% CI = (0.22, 0.29); P = 0.000] relative to women who were orthodox. The odd of contraceptive use among male headed household were 1.49 times more likely to use modern contraceptive [AOR = 1.49; 95% CI = (1.29, 1.70); P = 0.000] compared to female headed household. The odd of modern contraceptive use among poorest were 0.54 times less likely to use contraceptive [AOR = 0.54; 95% CI = (0.45, 0.66); P = 0.000] relative to women who were richest. The odd of modern contraceptive among married were 1.42 time more likely to use contraceptive [AOR = 1.42; 95% CI = (1.19, 1.70); P = 0.000] relative to women who were single (Table 4).
Discussion
The study assessed the spatial distribution of modern contraceptive use and the factors that influence its use among women of reproductive age in Ethiopia, using the recent Ethiopian mini demographic health survey data conducted in 2019. In general, this study showed geographical variations in the usage of modern contraceptives among women of reproductive age. In Ethiopia, the northern region had a higher proportion of women using modern contraceptives, while the southern region had a lower proportion. Particularly, areas of southern Ethiopia including Gambella, Benishangul, SNNPR, Oromia, Somalia, Harari, and Diredawa had low rates of modern contraception use. Furthermore, the northern region of Ethiopia had the highest rate of modern contraceptive use. High rates of modern contraception use are found in Tigray, Afar, Amhara, and several regions of Oromia. This variations were existed, because of Ethiopia is a low-income country with limited access to family planning (FP), particularly in the developing regions [16]. The Ethiopian government has significantly increased the number of medical facilities and qualified personnel [17]. In turn, this led to a rise in the country’s contraceptive prevalence rate (CPR), which increased from 8% in 2000 to 41.4% in 2019 [18]. However, there was a significant regional variation in CPR among the developing regions [19]. Additionally, we hypothesize that this discrepancy may result from regional socioeconomic disparities.
The results of the bivariable analysis in this study showed that among women of reproductive age, the use of contraception was significantly correlated with maternal age, place of residence, religion, educational status, sex of household, wealth index, and current marital status. According to other similar studies that supported this finding, the use of modern contraceptives is influenced by a variety of factors, including age, education, communication between couples about FP, the number of living children, husband approval of FP, the intended number of children, place of residence, religion, knowledge, and attitudes [9,10,11].
This survey revealed that 25.5% of women of reproductive age used modern contraceptives. This finding was slightly higher than the studies which was conducted in Ethiopia [20] and in Ghana [21]. On the other hand the finding of this study was lower than the study which was conducted in north west Ethiopia [22] Kenya [23] and in Ethiopia [24]. These variations may have been caused by the study period, sample size, and study area’s locations.
The findings of this study indicated that women of reproductive age who resided in urban areas had higher odds of using modern contraceptives than did women who lived in rural areas. This finding was supported by the studies which was conducted in Nigeria [25] and in Senegal [26]. This discrepancy may have existed due to the great availability of family planning services and the rising number of health institutions in urban areas. However, most women face several barriers to obtaining and using modern contraceptives, particularly those who live in rural areas [27] such as, low educational attainment in rural area [28], Poverty rates in rural areas have been consistently higher than those in urban area [29], deep rooted cultural belief [30] especially, the husband’s role as primary decision-maker and the desire for a large family [31], fear of side-effects due to lack of knowledge [32], long distances to healthcare facilities, and inadequate stock of preferred types of modern contraceptives [33, 34].
According to this study, women of reproductive age who were attended in primary education were less likely to use modern contraceptives than those attended in higher education. This finding was consistent with the studies which was conducted in Ethiopia [35], in Kenya [36] in Zaire [37]. The first possible reason for these variation were women who receive more maternal education may be more informed about the variety of contraceptive methods available, which will enable them to use contraception more effectively and make informed decisions [38]. The second reason were, when education levels rise, wealth and prestige tend to rise as well, and the desire to limit family size by utilizing modern contraceptives would increase [39].
The results of this study showed that Muslim women in reproductive age used modern contraceptives at a lower rate than orthodox and protestant women. This was in line with the studies which was conducted in Ethiopia [40, 41], Zambia [42], Ghana [21] and Tanzania [43]. Religious acceptance of family planning methods might be one reason for this variation, although participants’ interpretations of their religion’s position on the topic varied. Most people who believed that family planning was incompatible with their beliefs declared that they had a duty to have as many children as God would allow them to have. Others thought family planning was appropriate given their moral obligation to raise and safeguard their children by reducing the number of children [43]. Additionally, there are misinterpretations of Islamic teachings on polygamy, which is still practiced and has a negative impact on FP adoption, as well as contraceptives, which is frequently prohibited [44].
This study demonstrated that male headed households were more likely than female headed households to utilize contraceptives. This study finding was concurrent with studies which was conducted in Ethiopia [45], in Tanzania [46]. Since, Interspousal communication is a key issue that affects the sustained use of family planning [50]. Men were viewed as the only ones who could provide the demands of their families. Women were not thought of as decision makers, but rather as implementers of what males had decided, without challenging those decisions [51].
According to this study, women who were poorer were less likely than women who were wealthy to utilize modern contraceptives. This finding was in line with the studies which was conducted in Nigeria [52], in Ethiopia [53] and in Amhara region of Ethiopia [54]. The contributing factors for these disparity were the usage of contraceptives has a financial cost associated with it, rich women might be able to avoid any financial barriers to using modern contraceptives, while poor women might not [55, 56], the level of household wealth has a significant impact on access to education, basic healthcare services, and health information [57].
This study demonstrated that married women were more likely than single women to utilize modern contraceptives. This finding were consistent with studies which were conducted in southern Ethiopia [58], north west Tanzania [59], and Kenya [60]. From the perspective of males as a potential factor that influences the usage of modern contraceptives for the purposes of fertility control, these differences may have arisen [61].
Conclusion
In this study Individual and community level factors were associated with modern contraceptive use and also there were spatial variations in modern contraceptive use across the region among reproductive-age women. Empowering women to have better educational status, improving the wealth index, promoting marriage, creating awareness among rural residences women and promoting education about modern contraceptives through religiously acceptable persons, and promoting modern contraceptive use in developing regions were the key factors to improve modern contraceptive use among reproductive age women in Ethiopia.
Strengths and limitations of this study
-
The DHS has a similar design, with identical variables in a different environment; the result may, therefore, be applicable to other similar locations.
-
The study used a sufficiently large sample size at the national level to ensure its representativeness.
-
Recall bias is one of the potential drawbacks, especially for retrospective data based on past experiences.
-
The magnitude of the bias is often unknown and correcting for the bias is difficult.
-
Since, this study was cross sectional study.it doesn’t showed temporal relationships between independent and dependent variable.
Availability of data and materials
The data were obtained from mini-Edhs of 2019 that was found at DHS portal of (https://dhsprogram.com/data/dataset/Ethiopia_Interim-DHS_2019.cfm?flag=1).
References
Rakhi J, Sumathi M. Contraceptive methods: needs, options and utilization. J Obstet Gynecol India. 2011;61(6):626–34.
Ricci SS. Susan_Scott_Ricci_Essentials_of_Maternity_Newborn_and_Women_s_Health ;fourth edition.
Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception. 2015;92(5):420–1. Available from:. https://doi.org/10.1016/j.contraception.2015.08.008.
Almalik M, Mosleh S, Almasarweh I. Are users of modern and traditional contraceptive methods in Jordan different? East Mediterr Heal J. 2018;24(4):377–84.
UNDESA. World Family Planning. Highlights. Econ Soc Aff. 2017;2017:1–43 Available from: https://www.un.org/en/development/desa/population/publications/pdf/family/WFP2017_Highlights.pdf.
Ethiopian Public Health Institute (EPHI), ICF. Ethiopia Mini demographic and health survey 2019: final report. 2021. 1–207 p. Available from: https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf
America L, America N, Africa W. Maternal morbidity and mortality. Br Med J. 1935;2(3892):265–7.
UNFPA. Contraceptives save life. 2012;(December):1–5. Available from: www.unfpa.org
Lwelamira J, Mnyamagola G, Msaki MM. Knowledge, attitude and practice (KAP) towards modern contraceptives among married women of reproductive age in Mpwapwa District, Central Tanzania. Curr Res J Soc Sci. 2012;4(3):235–45.
Hagos G, Tura G, Kahsay G, Haile K, Grum T, Araya T. Family planning utilization and factors associated among women receiving abortion services in health facilities of central zone towns of Tigray, northern Ethiopia: a cross sectional study. BMC Womens Health. 2018 Jun;18(1):83.
Assefa Y, Hill PS, Gilks CF, Admassu M, Tesfaye D, Van Damme W. Primary health care contributions to universal health coverage. Ethiopia Bull World Health Organ. 2020;98(12):894–905A.
Bahk J, Yun S-C, Kim Y, Khang Y-H. Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the panel study on Korean children (PSKC). BMC Pregnancy Childbirth. 2015;15(1):1–12.
Herd P, Higgins J, Sicinski K, Merkurieva I. The implications of unintended pregnancies for mental health in later life. Am J Public Health. 2016;106(3):421–9.
Foster DG, Raifman SE, Gipson JD, Rocca CH, Biggs MA. Effects of carrying an unwanted pregnancy to term on women’s existing children. J Pediatr. 2019;205:183–9.
Bhusal CK, Bhattarai S. Factors affecting unmet need of family planning among married Tharu women of dang district, Nepal. Int J Reprod Med 2018;2018.
FMOH. Ethiopian Health Sector Transformation Plan.2015/16 - 2019/20. Fed Democr Repub Ethiop Minist Heal. 2015;20(May):50.
Donovan P, Wulf D. Family planning can reduce high infant mortality levels. Issues Brief (Alan Guttmacher Inst). 2002 Apr;2:1–4.
Ethiopian Public Health Institute Addis Ababa. Ethiopia Mini demographic and health survey. FEDERAL DEMOCRATIC REPUBLIC OF ETHIOPIA Ethiopia. 2019.
Bekele D, Surur F, Nigatu B, Teklu A, Getinet T, Kassa M, et al. Contraceptive prevalence rate and associated factors among reproductive age women in four emerging regions of Ethiopia: a mixed method study. Contracept Reprod Med. 2021;6(1):18. Available from:. https://doi.org/10.1186/s40834-021-00162-9.
Gebre MN, Edossa ZK. Modern contraceptive utilization and associated factors among reproductive-age women in Ethiopia: evidence from 2016 Ethiopia demographic and health survey. BMC Womens Health. 2020;20(1):61. Available from:. https://doi.org/10.1186/s12905-020-00923-9.
Beson P, Appiah R, Adomah-Afari A. Modern contraceptive use among reproductive-aged women in Ghana: prevalence, predictors, and policy implications. BMC Womens Health. 2018;18(1):157. Available from:. https://doi.org/10.1186/s12905-018-0649-2.
Oumer M, Manaye A, Mengistu Z. Modern contraceptive method utilization and associated factors among women of reproductive age in Gondar City. Northwest Ethiopia Open access J Contracept. 2020;11:53–67.
Akoth C, Oguta JO, Kyololo OM, Nyamu M, Ndirangu MN, Gatimu SM. Factors associated with the utilisation and unmet need for modern contraceptives among urban women in Kenya: a cross-sectional study. Front Glob Women’s Heal. 2021:2 Available from: https://www.frontiersin.org/article/10.3389/fgwh.2021.669760.
Oumer M, Manaye A, Mengistu Z. <p>modern contraceptive method utilization and associated factors among women of reproductive age in Gondar City, Northwest Ethiopia</p>. Open Access J Contracept. 2020;11:53–67.
Training P, Africa S, Statistics M, Training P, Africa S. Contraceptive use among Nigerian women with no fertility intention. interaction amid potential causative factors. 2013;2:127–39.
Zegeye B, Ahinkorah BO, Idriss-Wheeler D, Olorunsaiye CZ, Adjei NK, Yaya S. Modern contraceptive utilization and its associated factors among married women in Senegal: a multilevel analysis. BMC Public Health. 2021;21(1):231. Available from:. https://doi.org/10.1186/s12889-021-10252-7.
Osinowo K, Ekholuenetale M, Ojomo O, Hassan A, Ladipo OA. Patterns of triggers, ideation and motivational factors of contraceptive utilization among women and gate-keepers in Nigeria: a scoping study on the resilient and accelerated scale up of DMPA-SC in Nigeria (RASUDIN). Contracept Reprod Med. 2020;5(1):1–10.
Habtu A. ScholarWorks at WMU Women ’ s Higher Education in Ethiopia Under Three Regimes, Women ’ s Higher Education in Ethiopia Under Three Regimes, 1950-1997; 2001.
Dorosh P, Schmidt E. The rural-urban transformation in Ethiopia; 2010.
Jan M, Akhtar S. An analysis of decision-making power among married and unmarried women. Stud Home Community Sci. 2008;2(1):43–50.
Muanda MF, Ndongo GP, Messina LJ, Bertrand JT. Barriers to modern contraceptive use in rural areas in DRC. Cult Health Sex. 2017;19(9):1011–23. Available from. https://doi.org/10.1080/13691058.2017.1286690.
Schrumpf LA, Stephens MJ, Nsarko NE, Akosah E, Baumgartner JN, Ohemeng-Dapaah S, et al. Side effect concerns and their impact on women’s uptake of modern family planning methods in rural Ghana: a mixed methods study. BMC Womens Health. 2020;20(1):57. Available from:. https://doi.org/10.1186/s12905-020-0885-0.
Mushy SE, Tarimo EAM, Fredrick Massae A, Horiuchi S. Barriers to the uptake of modern family planning methods among female youth of Temeke District in Dar Es Salaam, Tanzania: a qualitative study. Sex Reprod Healthc Off J Swedish Assoc Midwives. 2020;24:100499.
Ramírez GR, Bravo PE, Vivaldi MIM, Manríquez IP, Pérez TG. Adolescents’ access to contraception: perceptions of health workers in Huechuraba, Chile. Rev Panam Salud Publica. 2017;41:e77.
Adane AA, Bekele YA, Melese E, Worku GT, Netsere HB. Modern contraceptive utilization and associated factors among married Gumuz women in Metekel zone north West Ethiopia. Biomed Res Int. 2020.
Mukthar VK, Maranga AK, Kulei SJ, Chemoiwa RK. The uptake of modern contraceptives among women of reproductive age attending maternal child health and family planning (MCH/FP) clinics. East Afr Med J. 2014;91(12):457–66.
Shapiro D, Tambashe BO. The impact of women’s employment and education on contraceptive use and abortion in Kinshasa. Zaire Stud Fam Plann. 1994;25(2):96–110.
Pazol K, Zapata LB, Tregear SJ, Mautone-Smith N, Gavin LE. Impact of contraceptive education on contraceptive knowledge and decision making: a systematic review. Am J Prev Med. 2015;49(2 Suppl 1):S46–56.
Adebowale SA, Adedini SA, Ibisomi LD, Palamuleni ME. Differential effect of wealth quintile on modern contraceptive use and fertility: evidence from Malawian women. BMC Womens Health. 2014;14(1):40. Available from:. https://doi.org/10.1186/1472-6874-14-40.
Tigabu S, Demelew T, Seid A, Sime B, Manyazewal T. Socioeconomic and religious differentials in contraceptive uptake in western Ethiopia: a mixed-methods phenomenological study. BMC Womens Health. 2018;18(1):85. Available from:. https://doi.org/10.1186/s12905-018-0580-6.
Walelign D, Mekonen A, Netsere M, Tarekegn M. Modern contraceptive use among orthodox Christian and Muslim women of reproductive age Group in Bahir Dar City, north West Ethiopia: comparative cross sectional study. Open J Epidemiol. 2014;04(04):235–42.
Lasong J, Zhang Y, Gebremedhin SA, Opoku S, Abaidoo CS, Mkandawire T, et al. Determinants of modern contraceptive use among married women of reproductive age: a cross-sectional study in rural Zambia. BMJ Open. 2020;10(3):e030980 Available from: http://bmjopen.bmj.com/content/10/3/e030980.abstract.
Sundararajan R, Yoder LM, Kihunrwa A, Aristide C, Kalluvya SE, Downs DJ, et al. How gender and religion impact uptake of family planning: results from a qualitative study in northwestern Tanzania. BMC Womens Health. 2019;19(1):99. Available from:. https://doi.org/10.1186/s12905-019-0802-6.
Abdi B, Okal J, Serour G, Temmerman M. “Children are a blessing from god” – a qualitative study exploring the socio-cultural factors influencing contraceptive use in two Muslim communities in Kenya. Reprod Health. 2020;17(1):44. Available from:. https://doi.org/10.1186/s12978-020-0898-z.
Mulatu T, Sintayehu Y, Dessie Y, Deressa M. Modern family planning utilization and its associated factors among currently married women in rural eastern Ethiopia: a community-based study. Gigantesco a, editor. Biomed res Int. 2020;2020:6096280. Available from. https://doi.org/10.1155/2020/6096280.
Msovela J, Tengia–Kessy A, Rumisha SF, Simba DO, Urassa DP, Msamanga G. Male partner approval on the use of modern contraceptive methods: factors determining usage among couples in Kibaha district, Tanzania. Contracept Reprod Med. 2020;5(1):3. Available from: https://doi.org/10.1186/s40834-020-00107-8.
Kantorová V, Wheldon MC, Ueffing P, Dasgupta ANZ. Estimating progress towards meeting women’s contraceptive needs in 185 countries: a Bayesian hierarchical modelling study. PLOS Med. 2020;17(2):1–23. Available from:. https://doi.org/10.1371/journal.pmed.1003026.
Federal Democratic Republic of Ethiopia ministry of health October 2011. NATIONAL GUIDELINE FOR FAMILY PLANNING Federal Democratic Republic of Ethiopia. Fed Democr Repub Ethiop Minist heal Oct ,2011. 2011;1–69.
Weel C van, Kidd MR. Primary health care to contribute to universal health coverage. Prim Heal Care Around World. 2020;(September):123–7.
Adelekan A, Omoregie P, Edoni E. Male involvement in family planning: challenges and way forward. Kost K, editor. Int J Popul res. 2014;2014:416457. Available from. https://doi.org/10.1155/2014/416457.
Wambui T, Ek A, Alehagen S. Perceptions of family planning among low-income men in Western Kenya. Int Nurs Rev. 2009;56(3):340–5.
Fadeyibi O, Alade M, Adebayo S, Erinfolami T, Mustapha F, Yaradua S. Household Structure and Contraceptive Use in Nigeria. Frontiers in Global Women’s Health. 2022;3 Available from: https://www.frontiersin.org/article/10.3389/fgwh.2022.821178.
Tsehay CT. Factors associated with modern contraceptive demands satisfied among currently married/in-union women of reproductive age in Ethiopia: a multilevel analysis of the 2016 demographic and health survey. BMJ Open. 2022;12(2).
Asresie MB, Fekadu GA, Dagnew GW, Gelaw YM. Modern contraceptive use and influencing factors in Amhara regional state: further analysis of Ethiopian demographic health survey data 2016. Khubchandani J, Adv public heal. 2020;2020:5817383. Available from: https://doi.org/10.1155/2020/5817383.
Ahinkorah BO. Predictors of modern contraceptive use among adolescent girls and young women in sub-Saharan Africa: a mixed effects multilevel analysis of data from 29 demographic and health surveys. Contracept Reprod Med. 2020;5(1):1–12.
Ahinkorah BO, Seidu A-A, Appiah F, Budu E, Adu C, Aderoju YBG, et al. Individual and community-level factors associated with modern contraceptive use among adolescent girls and young women in Mali: a mixed effects multilevel analysis of the 2018 Mali demographic and health survey. Contracept Reprod Med. 2020;5(1):1–12.
Shagaro SS, Gebabo TF, Mulugeta BT. Four out of ten married women utilized modern contraceptive method in Ethiopia: A Multilevel analysis of the 2019 Ethiopia mini demographic and health survey. PLoS One. 2022;17(1):e0262431. Available from. https://doi.org/10.1371/journal.pone.0262431.
Bogale B, Wondafrash M, Tilahun T, Girma E. Married women’s decision making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11(1):342. Available from:. https://doi.org/10.1186/1471-2458-11-342.
Safari W, Urassa M, Mtenga B, Changalucha J, Beard J, Church K, et al. Contraceptive use and discontinuation among women in rural north-West Tanzania. Contracept Reprod Med. 2019;4(1):18. Available from:. https://doi.org/10.1186/s40834-019-0100-6.
Lunani LL, Abaasa A, Omosa-Manyonyi G. Prevalence and factors associated with contraceptive use among Kenyan women aged 15–49 years. AIDS Behav. 2018;22(1):125–30. Available from:. https://doi.org/10.1007/s10461-018-2203-5.
Asa SS, Titilayo A, Kupoluyi JA. Assessment of Contraceptive Use by Marriage Type Among Sexually Active Men in Nigeria. Int Q Community Health Educ. 2018;38(3):181–94. Available from. https://doi.org/10.1177/0272684X17749800.
Acknowledgments
The authors would like to thank measure DHS for their permission to access the DHS datasets.
Funding
For this study, the author did not receive any financial support.
Author information
Authors and Affiliations
Contributions
G.M. and B.K. worked on this study from start to finish, including design, data extraction, data cleaning and coding, data analysis and interpretation, and composing and revising the manuscript. G.M. then completed the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
In relation to the research, authorship, and publication of this work, the author (G.M.) disclosed no possible conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mankelkl, G., Kinfe, B. Spatial variations and multilevel mixed effect analysis on determinants factors of modern contraceptive utilization among reproductive age women in Ethiopia; proven by Ethiopian mini demographic health survey 2019. BMC Women's Health 23, 77 (2023). https://doi.org/10.1186/s12905-022-02030-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-02030-3