Abstract
Background
Cervical cancer represents a high burden of disease. Many women in low- and middle-income countries face opposition from their partners and families to undergo cervical cancer screening. Identifying the social, cultural, and psychological factors that underly the opposition to screening by male partners is an important step towards reducing barriers for men to support their wives’ participation in cervical screening. This study explored the role of structural and psychological factors deriving from theoretical models as determinants of Indian men’s opposition to their partners being screened for cervical cancer.
Methods
A survey among 500 sexually active males was conducted between April 2020 and August 2020 to measure knowledge of cervical cancer and screening, awareness of screening possibilities, attitude towards screening, perceived barriers to screening, and health literacy. Regression analysis was performed to assess which of the potential factors contributed to the intention to support their wives’ screening.
Results
The majority of participants had very poor knowledge and awareness about cervical cancer and screening procedures, tended towards a negative attitude towards screening, and perceived several structural barriers. Attitude towards the screening procedure and routine participation in general screening significantly predicted their intention to support their wives’ screening for cervical cancer. Education moderated the association between knowledge and awareness and the intention to support their wives’ screening.
Conclusion
As women often rely on their spouses’ financial and emotional support of cervical screening, there is a need for men to be encouraged to support their wives’ screening participation. Programs to encourage men to support their wives’ cervical screening should focus on their attitude towards screening, educate about cervical cancer and screening procedures, and reduce perceived barriers.
Similar content being viewed by others
Introduction
Cervical cancer is the fourth most common cancer among women and represents one of the largest global burdens of disease [1]. The mortality due to cervical cancer remains very high worldwide, especially in Low- and Middle-Income countries (LMICs), due to the ageing and growth of the population and the variations in the occurrence and distribution of risk factors linked to socio-economic development [2, 3]. In the year 2020, there were 0.6 million new cases of cervical cancer in the world, most of them occurring in the Asian region [4], with the majority of the deaths taking place in LMICs [1]. India alone contributes to up to one-third of the burden of cervical cancer in Asia, with 0.9 million cases and 60, 000 deaths in 2020 [5].
Whereas most cancers are difficult to prevent as they are associated with multiple causal agents [6], cervical cancer can be prevented to some extent by the appropriate and consistent use of condoms which prevent the transmission of the Human Papilloma Virus (HPV) [7]. In addition, the discovery of a vaccine against cervical cancer in 2006 has increased the possibility to prevent the disease. Besides these two forms of primary prevention, the infection can also be detected at an early stage before it progresses to cancer. In its Global strategy to accelerate the elimination of cervical cancer, the World Health Organisation therefore proposes three main strategies to reduce the burden of cervical cancer, with targets to be reached by 2030: (i) Vaccination of 90% of girls against HPV by the age of 15; (ii) Screening of 70% of women with a high-performance testing method by the age of 35, and again by the age of 45; and (iii) Treatment of 90% of women with pre-cancer, and management of 90% of women with invasive cancer [8].
Vaccination against HPV has been initiated in most developed countries, but is more difficult to implement in LMICs due to the high vaccine cost [9]. Although vaccination is approved in India, only the affluent can choose to be vaccinated as each dose of the vaccine costs about 25–37 USD. Those living in poverty do not have the choice to get vaccinated as it is not yet included in the country’s immunization programs due to various reasons [10]. Factors like low social acceptance of the vaccine, lack of protection against certain strains of the virus, and uncertainty about the duration of the protection provided by the vaccine are additional barriers to large-scale vaccine implementation against cervical cancer in India [11]. As a consequence, screening remains the main prevention strategy against cervical cancer in the country.
Screening for cervical cancer using methods recommended by WHO has been tested and found feasible for implementation in India but has not yet been rolled out in the form of systematic screening. The National Program for Prevention and Control of Cancer, Diabetes, Cardio-vascular disease and Stroke (NPCDCS) includes screening women for cervical cancer at community health centres, has been initiated in a few districts and is expected to be expanded throughout the country. Yet despite the availability of opportunistic screening and the initiation of the NPCDCS, CCS uptake remains low [12, 13]. Apart from certain characteristics of the health system that pose structural barriers to the implementation of the program [14], this low participation in screening by women is likely due to psychological and social factors [15], including inadequate knowledge and awareness of the disease and of screening possibilities, or negative attitudes towards screening [12]. Besides these, the social environment including the family and community can also have an impact on the decision to be screened [15]. In this regard, stigma, community traditions, religious beliefs, and lack of support from a partner have been mentioned as important influencers in decision-making [16].
Men play a significant role in the transmission of the HPV that causes cervical cancer. However, in education about the disease little attention is given to the men’s role, despite the WHO’s recommendation to involve males in CCS education [17]. Several studies have also shown that women’s decision to get screened relies on the opinion of their husbands or partners [18, 19]. This is probably even more the case in LMICs like India [15, 20], where decision-making regarding a woman’s health mostly lies with her husband. Yet while the few studies that have investigated this issue show poor knowledge among men about cervical cancer in LMIC [21,22,23,24] in LMIC, not many studies have been conducted on these countries to assess the opinion and knowledge of males on cervical cancer prevention.
Considering the importance of the male partner’s role in the promotion of cervical cancer screening, it is important to identify the factors that determine the partners’ support for screening. Among the various factors that could be considered in this regard are knowledge about cervical cancer and screening, health literacy, attitude, perceived norms, perceived barriers, and habits.
Health literacy refers to a person’s knowledge, motivation, and competencies in accessing, understanding, appraising, and applying health-related information with a view to making decisions related to health [25]. Poor health literacy is associated with lower participation in screening programs, suboptimal use of preventive services, and lower engagement in health promoting behaviours [26]. There are also potential links between health literacy and cervical cancer screening [27].
Attitude, perceived norms, and perceived barriers are social cognitive concepts that are central to behaviour theories that have been specifically developed to explain peoples’ health-related behaviour or intentions, such as the Health belief model (HBM) [28], the Protection Motivation Theory (PMT) [29], or the Theory of Planned Behaviour (TPB) [30]. These models can predict behaviours like colon or breast cancer screening [31, 32]. A recent systematic review confirmed that the HBM is the most widely used model to inform interventions to promote CCS behaviour, whereas the TPB is the most effective to predict CCS intention [33]. The TPB identifies three constructs - attitudes, subjective norm, and perceived behavioural control - as the main determinants of (the intention to) performing a health behaviour. Attitudes are defined as evaluative statements about an object, for example, an individual’s evaluative statements about CCS, based on outcome beliefs. Subjective normative beliefs refer to a person’s belief that a behaviour is (or is not) acceptable to others (e.g., partner, parents, peers, society) [34]. While such beliefs are subjective, the perception regarding the acceptability of a behaviour by others is more important than their objective influence. Perceived behavioural control refers to a person’s perception of the ease or difficulty of performing the behaviour of interest [34]. Studies have shown that adding additional constructs such as habit (i.e., one’s usual care-seeking behaviour, such as routinely participating in general screening) and ‘affect’ adds to the prediction of the behaviour [35]. A recent study that we conducted among females in India confirmed that although TPB is a better predictor of the intention to be screened, additional constructs like ‘structural barriers’ and ‘habit’ could enhance the prediction of screening intentions [36]. A model that includes the two most predictive TPB constructs (‘attitude’ and ‘subjective norm’) in combination with ‘structural barriers’ and ‘habits’ provided the best prediction of Indian women’s intentions to be screened for cervical cancer.
Drawing on those findings, the present study intended to test whether this model (henceforth referred to as the modified TPB model) could also predict the intention of male partners to support their wives’ participation in CCS. In addition, we also wanted to assess if the effects of the model on the men’s intention to support screening are moderated by their knowledge and health literacy level. This, study specifically aimed to (a) explore the factors that influence male partners’ intention to support their wives’ participation in cervical cancer screening using the modified TPB; (b) assess the variance explained by each of the model’s components on the male partners’ intention to support their wives’ participation in screening; and (c) assess the moderating role of health literacy and education on the attitude and subjective norm towards screening.
Materials and methods
Study design and setting
A cross-sectional survey was conducted among male partners of sexually active women in Karnataka, a southern state of India. All methods were carried out in accordance with relevant guidelines and regulations. The state has a population of 61.09 million with nearly 50% of the females aged between 15 and 44 years. Nearly 62% of the population lives in rural areas. The literacy rate of males dwelling in rural areas is about 78% and of those dwelling in urban areas 90%. Cervical cancer contributes to 13% of cancers [37], but only 0.5% of women in the state have undergone cervical cancer screening [38] and the average cervical cancer examination rate is very low [39].
Sample size and method
The study collected responses from a representative sample of sexually active males aged between 20 and 60 years. Individuals available at the time of data collection and able to read Kannada or English were included in the study. A sample size of 385 was calculated using Cochran’s formula considering a 50% response rate: Sample size = Z2 (p*q)/d2, with the estimated population proportion (p) of 50%, q=(1-p), the margin of error (d) as 5% and Z value 1.96 for 95%confidence level. The predicted variance of 50% was based on the population proportion (i.e., p = 0.5 yields an adequate sample to represent the population), since no similar studies existed for the given population.
As a first step, health facilities (public hospitals or tertiary screening centres) that conduct opportunistic screening for cervical cancer for less or no cost (hereafter referred to as screening centres) were identified in each district with the help of District health authorities, who provided a list of such centres. This was done to reduce the influence of barriers related to the availability of and affordability to screening. In a second step, two regions were identified, one accessible and one inaccessible to the screening centre, based on judgemental sampling to assess accessibility barriers. In the final step, individuals from both regions were approached using a consecutive approach.
Data collection was done by community health workers (ASHAs or Accredited Social Health Activists) who were trained in the data collection procedure and provided with a set of written instructions. The data collection took place under the supervision of the researcher who could be contacted whenever required.
Participants
The study included 500 sexually active men who were willing to participate in the survey and familiar with the Kannada or English language. The participants from rural and urban communities were approached by the health workers using a consecutive sampling approach. The participant characteristics are presented in Table 2. The mean age of the participants was 41 years (SD 8.5). Most participants were employed (98.8%) and had at least completed secondary education (73%). Only a few (0.4%) had been trained in a health care profession. Although three out of four participants (76%) did not have a health insurance (76%), 53% of them claimed to undergo routine health check-ups (blood pressure, blood sugar, serum cholesterol, etc.) irrespective of symptoms, and 64.2% reported to have no difficulties to pay for these check-ups. The majority of participants (87%) declared that the decision related to health care expenditure for women in their families was taken by them (male partner) or by another family members (in-laws or parents).
Conceptual model
The modified version of the TPB that was used for this study [33, 36] holds that the men’s intention to support their female partner’s cervical cancer screening (ISP) is influenced by attitude, subjective norms, and habitual screening behaviour, with attitudes and subjective norm in turn being influenced by knowledge, awareness of cervical cancer and routine screening participation (Fig. 1).
The construct of perceived behavioural control, which is normally part of the TPB, was not included in the model, since screening participation is a behaviour that is performed by the women, and as such not under the male partner’s control. Instead, perceived structural barriers to screening (e.g., financial cost, time, accessibility, or health system characteristics that could hinder the wives’ screening) were added to the model. Health literacy and education were added as moderating variables, as they significantly influence screening behaviour and knowledge.
Questionnaire
For the data collection a structured questionnaire was developed, based on the adapted version of the TPB informed by a systematic review, a qualitative study, and a validation study conducted at earlier stages of the research project [15, 33, 40]. In addition to socio-demographic characteristics, knowledge about cervical cancer and screening, and CCS intention, it measured knowledge and awareness about cervical cancer and screening, attitude towards the wife’s participation, subjective norm, habits, health literacy, and structural barriers preventing the wife’s participation in cervical screening. The questionnaire items were in the form of close-ended questions. They were developed in English and translated into Kannada with the help of language experts, and pretested for cultural relevance, comprehension, and clarity, with adaptations made when necessary.
The resulting questionnaire consisted of five sections as shown in Table 1. The first section asked for the participants’ demographic and background characteristics. The second section measured knowledge about cervical cancer and screening through eight questions (5 on cancer, 3 on screening) with multiple answers from which the participant had to choose the right one, yielding a score between 0 and 16. The reliability (KR-20) for the knowledge scale was 0.88, which can be considered as good [41]. The third section measured the theoretical constructs of the modified TPB model, i.e., attitude towards CCS (7 items), subjective norms related to cervical cancer and screening (6 items) and perceived structural barriers to screening (5 items). Items for in the form of statements to be scored on a 5-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’, with higher scores representing a higher level of the variable. Habit of participating in health screening was assessed by dichotomous scales (yes/no) asking participants if they engaged in regular check-ups of blood pressure, blood sugar, etc. even if they did not have any symptoms. Cronbach’s α for the attitude, subjective norms and structural barriers scales were 0.70, 0.72, and 0.83, respectively. The fourth section of the questionnaire measured health literacy using the HLS-IND-KAN-Q16 and HLS-IND-ENG-Q16 (25), which is a 16-item validated questionnaire for a Kannada and English-speaking population based on the HLS-EU questionnaire [42]. It contains questions about the ease or difficulty to perform various activities related to health care, disease prevention and health promotion, to be scored on a 5-point Likert scale (very difficult, difficult, don’t know, easy, and very easy). A standardized Health Literacy index score out of 50 for each participant is calculated using the formula HL = (Average − 1) x (50/3), with an index score greater than 33 considered as adequate [43]. Finally, the participant’s intention to support his wife’s participation in cervical cancer screening was measured on a dichotomous scale (yes/no), as a dependent variable for the analysis.
Data analysis
Data analysis was done in SPSS version 25.0. Frequencies with percentages and mean scores with standard deviations were provided as descriptive statistical measures. Bivariate analysis was performed using chi-square to test the association between categorical independent variables and intention to support the wife’s CCS as a dichotomous outcome, and independent t-tests to measure the differences on the continuous variables between men with and without the intention to support screening. Next, a series of logistic regression analyses were performed to assess the relative contribution of different factors to the male partners’ intention to support screening and the variance explained by the models, with the proportion of explained variance given by Nagelkerke’s pseudo R square. In a first regression model, knowledge and awareness were regressed on the intention to support the wife’s screening as a (dichotomous) dependent variable. In a second model, attitude, subjective norms, habit and perceived structural barriers were added as predictor variables, and both models were compared to assess the added variance. In a third step, the potential moderating effect of health literacy and education on the association between attitude and subjective norms on the one hand and intention on the other hand was tested using PROCESS macro in SPSS 25.0 bootstrapping analyses with 5000 bootstrapped samples to obtain reliable 95% confidence intervals.
Results
Knowledge and experience with cervical cancer
The majority of the men (68%) had a positive intention to support their partner’s participation in cervical cancer screening. Additionally, 12.8% of individuals claimed that their women had had one or more warning signs of cervical cancer, and 3.8% claimed their partners had suffered pain or itchiness in the vaginal region, foul smelly vaginal discharge (3.6%), post-menopausal bleeding (3.4%), bleeding between menstrual cycle (2.6%), or post-coital hemorrhage (1.4%). Men who completed secondary education had a significantly more positive intention to support their wife’s participation in screening than those who only had primary education. A small proportion of the participants (0.4%) who had been trained in a health care profession had a positive intention, but the difference was not significant compared to the untrained individuals (Table 2).
Knowledge about cervical cancer among men was poor. Most participants (66%) had never heard of cervical cancer, and only 12% had known someone with cervical cancer. Only 7.8% of the participants believed that cervical cancer is caused by a virus that is transmitted through sexual contact, and 21% were not aware of any of the risk factors of cervical cancer. More than half of the respondents (61%) did not know about the warning signs of cervical cancer, while about 40% identified chronic foul or blood-filled vaginal discharge as a sign of cervical cancer. The majority of respondents (95.4%) were unaware of the screening procedure, and 82% did not know that regular screening irrespective of warning signs was necessary.
The mean health literacy score of the participants in the study was 29.05, which is below the cut off score of 33 signifying a sufficient level of health literacy. Nearly 80% of the participants had limited health literacy. Those with a positive intention to support their wives’ participation in screening (ISP) had a significantly higher score for health literacy (30.6) than those without this intention (25.6), yet their average health literacy score remained in the ‘limited’ level.
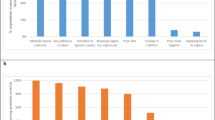
With regard to the socio-cognitive factors measured in the theoretical model, most men had a negative attitude towards screening, with 8.2% of them even considering screening to be non-beneficial. Most participants (46%) were anxious about the procedure while others felt uncomfortable (30.4%) or were afraid of the outcome (35.8%). In terms of subjective norms, about 17% of the participants did not know anyone who had been screened for cervical cancer, 11% of them thought that it was socially unacceptable, and 8% thought that the families would not approve of screening. Norms were not significantly associated with intention. The most common perceived barriers to cervical cancer screening were health system-related (63%) followed by lack of time (27%), low accessibility to screening centers (20.6%), and cost (15.6%).
Bivariate analysis
Analysis of the intercorrelations between the variables (Table 3) revealed that participants with better knowledge of cervical cancer were more aware of screening and more health literate. They also had a more positive attitude and scored higher for subjective norms (p < 0.05). Those who were more aware of the screening procedure were more knowledgeable and had higher scores on positive attitude and structural barriers, but lower on subjective norms (p < 0.05). Higher scores on subjective norms correlated positively with knowledge but negatively with positive attitudes and structural barriers, and a higher score on health literacy correlated positively with all variables except subjective norms.
Independent samples t-tests of the differences between participants with a positive or no intention to support their wife’s participation in screening revealed that the former were significantly more aware of the screening procedure, had a more positive attitude towards screening, perceived fewer structural barriers, and had significantly higher levels of health literacy. In contrast, the intention to support one’s wife’s participation in screening was not related to perceived norms.
Multivariate analysis
Logistic regressions assessing the relative contribution of different factors to the male partners’ intention to support screening revealed, in the first step (Model 1, Table 4) that knowledge of cervical cancer and awareness of screening explained only 3.9% of the variance of the men’s intention (Adjusted R square = 0.035). The addition of attitude, subjective norms, habits, and perceived structural barriers (Model 2) increased the explained variance of the intention to 19% (adjusted R square = 0.179), with the socio-cognitive variables alone explaining up to 15% of the variance. Inspection of the odds ratios showed that a positive attitude (OR = 1.18) and especially the habit of regular health screening (OR = 3.04) are the main predictors of the man’s intention to support their wives’ participation in cervical screening, whereas knowledge of cervical cancer and awareness of screening procedures are only marginally significant, and subjective norms and perceived structural barriers do not contribute to the intention. It is noted, however, that the model does not have a good fit (Hosmer-Lemeshow χ²= 24.5, df = 8, p < 0.05), which is probably due to the high correlation between attitudes and perceived structural barriers (r = 0.748). When the latter variable is left out, as well as the subjective norm (which does not contribute significantly), the remaining model with awareness, attitudes and habits has a good fit (Hosmer-Lemeshow χ²=11.65, df = 8, p = 0.17) and explains 16% variance in the intention to support the partner’s participation in screening.
The moderation analyses using Hayes’ Process Macro to test if health literacy and education moderate the relationships between the variables impacting the men’s intention to support CCS revealed a significant moderator effect of education on the association between knowledge and awareness (dependent variables) and attitude (independent variable). The interaction between knowledge and the moderator (education) was statistically significant for attitude (β = 0.43, SE = 0.17, p = 0.0128, LLCI = 0.09; ULCI = 0.73). Similarly, the interaction between awareness and the moderator education was statistically significant for attitude (β= -1.77, SE = 0.47, p < 0.001, LLCI= -2.71; ULCI= -0.83). This suggests that a higher education level increases the effect of knowledge of the disease and of awareness of the screening procedure on having a positive attitude towards screening. Health literacy was not a significant moderator.
Discussion
Screening is the main prevention strategy against cervical cancer in India, but despite the availability of opportunistic screening and the initiation of systematic screening within the National Program for Prevention and Control of Cancer, Diabetes, Cardio-vascular disease, and Stroke (NPCDCS), the uptake of screening remains low. One of the various factors that may influence screening uptake by women in the target group is the lack of support from their partners. While previous research has shown that women’s willingness to be screened for cervical cancer depends on their husbands’ opinion or approval [18, 44], a lack of such approval has been identified as a social barrier to participating in screening for many women in India [15, 19, 20, 45] and in other LMICs [46]. Therefore, the WHO recommends education of males to increase their willingness to encourage and support their partners [17]. Yet apart from knowledge and education, other factors may hamper men’s support for their wives’ participation in screening. As for women, the factors that influence the men’s decision-making regarding screening are manifold, and can best be understood by using conceptual models that acknowledge the role of both socio-economic factors such as age, income and education, and socio-cognitive factors like knowledge, attitudes, perceived norms, habits, or health literacy.
In accordance with these views, the present study aimed to identify the perceptions and beliefs of Indian men that could act as barriers to encouraging their partners to uptake cervical screening. To that effect, we relied on a modified version of the TPB that had been successful in predicting screening intention among Indian women in a previous study [34], and which included attitudes towards screening, perceived social norms, perceived barriers and regular screening practices for other health issues, while also considering knowledge of cervical cancer and screening and health literacy as potential moderators.
A first finding was that about 84% of the participants in the study claimed that decisions on healthcare for their wives were taken by themselves or other family members, confirming findings from previous research regarding male domination of health related decisions of women for financial [47] or emotional reasons [48]. Furthermore, participants who had completed secondary education were more likely to have a positive intention to support their wife’s screening, which is in line with other studies showing an association between education level and cancer screening in women [13].
Knowledge and awareness of cervical cancer and cancer screening
With regard to socio-cognitive factors, our findings confirmed those of previous studies [49], including those that had been performed in Low-middle income countries [46, 50] that knowledge about the disease and awareness of the possibility to be screened are significant predictors of screening intention. This is similar to what has been found among females in this context [36]. In that regard, it is important to note that the overall knowledge about cervical cancer, its aetiology, risk factors, and early warning signs, was very low amongst the male participants in our study, which is consistent with the results of similar studies conducted earlier [15, 18, 22,23,24, 44, 51] and among women. We found that although most of the men who participated in the study had heard about cervical cancer, more than 90% did not know that cervical cancer is caused by the HPV virus transmitted through sexual contact, and that many were lacking in concrete knowledge about the disease and screening. Similar findings have been reported for other developing countries. For instance, in a study conducted in Uganda, it was reported that most men had heard of HPV but were unaware that it was transmitted through sexual intercourse [51]. While most men in this study identified having multiple sexual partners as a risk factor for cervical cancer, only 4.8% knew that condom use can reduce the risk for the disease. This could be due to the belief that the disease is a result of punishment for promiscuity and lack of fidelity towards one’s partner, which has been reported in other studies in India [16]. Thus, having heard of cervical cancer does not necessarily imply having an adequate knowledge about the disease. Not surprisingly, the National Family Health Survey of India shows that only 4.1% of the couples in the state of Karnataka use a condom as a contraceptive method [38], implying that there remains a great need to promote awareness about the ways to prevent HPV transmission among males. Moreover, a very low percentage of the men in our study (4.6%) were aware of the screening procedure, and more than half of them (56.5%) did not know that screening had to be done at regular intervals. This concurs with findings from other studies indicating that women who would benefit from cervical cancer screening are also often unaware of the need for regular screening and of the availability of opportunistic screening services [15]. This lack of awareness of screening procedures and the availability of screening facilities can be a significant barrier for males to support their wives to participate in screening [52,53,54].
Psychological determinants of men’s willingness to support cervical cancer screening
Whereas knowledge and awareness remain important determinants of the willingness of men to support their wives’ screening for cervical cancer, they are not the only ones. Whereas the Theory of Planned Behaviour has been shown to be one of the better models to predict screening uptake for cervical cancer [33], previous research among Indian women suggested that intention to participate in cervical cancer can be improved by using a modified version of the model containing perceived structural barriers and habits (i.e., regular health checks) in addition to attitudes and subjective norms. Our findings revealed that these factors, combined with knowledge of cervical cancer and awareness of screening, explained up to 18% of the variance in the men’s intention to support their wives’ screening. Among these variables, attitude towards screening and the habit of having regular health checks were significant determinants of intention. These same factors were found to be the main socio-cognitive predictors of women’s intention to participate in screening [55, 56]. A reduced model with only attitude and habits along with awareness of screening procedures gave a better fit and explained a total of 16% variance in the men’s intention to support their wives’ cervical screening.
The significant role of attitude as a predictor of screening intention (in women) has been consistently found in other studies. In contrast, habit (defined here as regularly participating in routine health check-ups) has not often been included in studies on screening uptake, and a clear relationship between habit and behavioural intention has not been reported consistently for other health behaviours either [57, 58]. In this study, however, men who regularly underwent routine health check-ups themselves were twice as likely to have a positive intention to support their wives’ screening than those who did not undergo routine screening, suggesting that habit is a significant predictor of the men’s intention to support their wives’ screening. Subjective norm, on the other hand, was not found to be a significant predictor. This is comparable to the findings of a study of determinants of cervical screening uptake among Indian women [34], although other studies did show an effect of subjective norms on screening intention [56]. This difference in findings is not surprising given the variation in the conceptualization and operationalization of the constructs, the different context in which studies are carried out, and the nature and background of participants [33].
The moderating role of health literacy and education
Besides the structural and socio-cognitive determinants of the male partners’ intention to support their wives’ screening, this study also investigated the moderating role of education and health literacy. Health literacy is an important quality that enables an individual to acquire, understand, evaluate, and apply health-related information, thus allowing them to make well-informed decisions regarding their health and that of their families. Similar to previous research [59], our study revealed a significant positive correlation between health literacy and knowledge of cervical cancer and awareness of screening procedures. Men with higher levels of health literacy tend to have a more positive attitude towards cervical cancer screening, which is similar to the direct relationship between health literacy and screening uptake among women [59, 60]. Moreover, the low level of health literacy that was found among the men who participated in this study is comparable to that of other studies among Indian males [61] and among women in a similar context. However, we did not find a confirmation of the hypothesized moderating role of health literacy on the relationships between knowledge and awareness on the one hand, and attitudes, subjective norms, habit, and perceived barriers on the other hand. In contrast, a significant moderator effect was found of education on the association between knowledge and awareness (dependent variables) and attitude (independent variable), suggesting that a higher education level increases the effect of knowledge of the disease and of awareness of the screening procedure on having a positive attitude towards screening.
Structural barriers to screening uptake
Various structural barriers can prevent the utilization of a screening offer. Structural barriers that prevent CCS utilization in LMICs have been well recorded [62, 63]. These barriers also exist in India, as has been reported elsewhere [64]. In our study, health system-related barriers were identified by most men, also those who had a positive intention to support their wife’s screening. This means that reducing structural barriers can be helpful. Among the barriers that are mentioned are the fact that most men do not like the approach of the health professionals or think that the process is time-consuming. These findings coincide with those of Binka et al., [52] and Basu et al. [65] who mentioned indifference by health professionals and poor quality of care received in public hospitals. In India, cervical cancer screening is available for minimum cost in district hospitals and selected health centres, which sometimes charge a fee for the procedure. This explains the role of geographical and financial inaccessibility of cervical screening for many women, as highlighted in previous studies in the same context [15, 46, 63, 66,67,68]. But in addition to these physical and structural barriers, it is also important to address social barriers, for which the engagement of family and community in CCS prevention is key [12]. Men can be supportive and help encourage women to disclose issues related to early warning signs of cervical cancer and support her to be screened, as most women fear to discuss these issues [15]. A study conducted in Kenya and sub-Saharan Africa showed that men were willing to support their partner to uptake screening and wanted to know more about screening and cervical cancer prevention [21, 24]. Beneficiaries of the program in India and their partners are mostly unaware of the existing services [54]. Hence, awareness on cervical screening must target men and families and must include information on how to support women in this regard, as seen in a study conducted in Ghana [44].
Study Limitations
This study is not without limitations. Firstly, as it concerns a questionnaire study it is likely that the data include a certain amount of bias. It is possible that the participants’ responses were biased by social desirability tendencies. Moreover, random bias may have been induced due to the fact that data were collected by health workers. Secondly, the study explored factors that influence men’s intentions to support their wives’ screening uptake, rather than their actual behaviour. Since intentions do not always translate into actual behaviour, it is not possible to infer to what extent the intentions would be put into practice. For that, it would be useful to measure the outcomes of the existing actions within the NPCDCS program via a cohort study, looking at actual behaviour. Finally, it should be noted that interactions exist between the different variables included in this study. While these interactions were accounted for in the statistical analyses that were performed, it would be interesting to also study their direct and indirect effects on the outcomes.
Conclusion
To improve the uptake of screening for cervical cancer most interventions aim to inform, encourage, and convince women to participate in screening programs, but engaging women alone might not be sufficient. To overcome social barriers to screening, the role of the male partners and families also needs to be acknowledged, especially in cultures where health-related decisions are mostly taken by men or heads of the family. While it is likely that the same kinds of social, cognitive, emotional, and cultural factors that influence women’s decisions to uptake screening can influence men to support their partners’ screening, research about these factors is scarce. This study is one of the first to examine socio-cognitive and structural determinants of males’ support of cervical cancer screening, using a behavioural model as a conceptual basis. The results of this study suggest that in addition to effective and active education to inform both women and men on cervical cancer, screening recommendation, the benefits of screening, and the services that are available, it is also important to promote a positive attitude towards screening among men. Interventions that are set up to that effect should take the overall low health literacy of men and families into account. Therefore, it would be wise to implement screening at community level and to strengthen the capacities of community health centres to provide their service.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due to ethical reasons but are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Omram AR. The epidemiologic transition: a theory of the epidemiology of population change. Bull World Health Organ. 2001;79:161–70.
Gersten O, Wilmoth JR. The cancer transition in Japan since 1951. Demographic Res. 2002;7:271–306.
Cervix. Uteri factsheet https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf.
India factsheet http://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf.
Curry SJ, Byers T, Hewitt M. Lifestyle Behaviors Contributing to the Burden of Cancer. Fulfilling the Potential of Cancer Prevention and Early Detection 2003.
Lam JUH, Rebolj M, Dugue P-A, Bonde J, von Euler-Chelpin M, Lynge E. Condom use in prevention of Human Papillomavirus infections and cervical neoplasia: systematic review of longitudinal studies. J Med Screen. 2014;21(1):38–50.
Organization WH. Accelerating the elimination of cervical cancer as a global public health problem. In.: World Health Organization. Regional Office for South-East Asia; 2019.
Graham JE, Mishra A. Global challenges of implementing human papillomavirus vaccines. Int J Equity Health. 2011;10(1):1–11.
Sankaranarayanan R, Basu P, Kaur P, Bhaskar R, Singh GB, Denzongpa P, Grover RK, Sebastian P, Saikia T, Oswal K. Current status of human papillomavirus vaccination in India’s cervical cancer prevention efforts. Lancet Oncol. 2019;20(11):e637–44.
Nigam A, Saxena P, Acharya AS, Mishra A, Batra S: HPV vaccination in India: critical appraisal. International Scholarly Research Notices 2014, 2014.
Thulaseedharan JV, Frie KG, Sankaranarayanan R. Challenges of health promotion and education strategies to prevent cervical cancer in India: A systematic review. Journal of Education and Health Promotion 2019, 8.
Van Dyne EA. Establishing baseline cervical cancer screening coverage—India, 2015–2016. MMWR Morbidity and mortality weekly report 2019, 68.
Dhillon PK, Hallowell BD, Agrawal S, Ghosh A, Yadav A, Van Dyne E, Senkomago V, Patel SA, Saraf D, Hariprasad R: Is India’s public health care system prepared for cervical cancer screening?: Evaluating facility readiness from the fourth round of the District Level Household and Facility Survey (DLHS-4). Preventive Medicine 2020, 138:106147.
Dsouza JP, Van den Broucke S, Pattanshetty S, Dhoore W. Exploring the Barriers to Cervical Cancer Screening through the Lens of Implementers and Beneficiaries of the National Screening Program: A Multi-Contextual Study. Asian Pac J Cancer Prev. 2020;21(8):2209–15.
Nyblade L, Stockton M, Travasso S, Krishnan S. A qualitative exploration of cervical and breast cancer stigma in Karnataka, India. BMC Womens Health. 2017;17(1):1–15.
Comprehensive cervical cancer control: a guide to essential practice. Geneva: World Health Organization; 2006.
Al-Naggar RA, Low W, Isa ZM. Knowledge and barriers towards cervical cancer screening among young women in Malaysia. Asian Pac J Cancer Prev. 2010;11(4):867–73.
Baskaran P, Subramanian P, Rahman RA, Ping WL, Taib NAM, Rosli R. Perceived susceptibility, and cervical cancer screening benefits and barriers in Malaysian women visiting outpatient clinics. Asian Pac J Cancer Prev. 2013;14(12):7693–9.
Basu P, Sarkar S, Mukherjee S, Ghoshal M, Mittal S, Biswas S, Mandal R, Sankaranarayanan R. Women’s perceptions and social barriers determine compliance to cervical screening: results from a population based study in India. Cancer Detect Prev. 2006;30(4):369–74.
Adegboyega A, Aleshire M, Dignan M, Hatcher J. Spousal support and knowledge related to cervical cancer screening: Are Sub-Saharan African immigrant men interested? Health Care Women Int. 2019;40(6):665–81.
Williams M, Amoateng P. Knowledge and beliefs about cervical cancer screening among men in Kumasi, Ghana. Ghana Med J. 2012;46(3):147.
Castellsagué X, Bosch FX, Muñoz N. The male role in cervical cancer. salud pública de méxico. 2003;45:345–53.
Rosser JI, Zakaras JM, Hamisi S, Huchko MJ. Men’s knowledge and attitudes about cervical cancer screening in Kenya. BMC Womens Health. 2014;14(1):1–7.
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):1–13.
White S, Chen J, Atchison R. Relationship of preventive health practices and health literacy: a national study. Am J Health Behav. 2008;32(3):227–42.
Kim K, Han HR. Potential links between health literacy and cervical cancer screening behaviors: a systematic review. Psycho-oncology. 2016;25(2):122–30.
Champion VL, Skinner CS. The health belief model. Health Behav health education: Theory Res Pract. 2008;4:45–65.
Rogers RW, Prentice-Dunn S: Protection motivation theory. 1997.
Ajzen I. The theory of planned behaviour: Reactions and reflections. In.: Taylor & Francis; 2011.
Macrae FA, Hill DJ, John DJBS, Ambikapathy A, Garner JF, Group BGPR. Predicting colon cancer screening behavior from health beliefs. Prev Med. 1984;13(1):115–26.
Ritchie D, Van den Broucke S, Van Hal G. The health belief model and theory of planned behavior applied to mammography screening: A systematic review and meta-analysis. Public Health Nursing 2020.
Dsouza JP, Van den Broucke S, Pattanshetty S, Dhoore W. The application of health behavior theories to promote cervical cancer screening uptake. Public Health Nursing (Boston, Mass) 2021.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Tommasetti A, Singer P, Troisi O, Maione G. Extended theory of planned behavior (ETPB): investigating customers’ perception of restaurants’ sustainability by testing a structural equation model. Sustainability. 2018;10(7):2580.
Dsouza JP, Broucke SVd, Pattanshetty S, Dhoore W. A comparison of behavioural models explaining cervical cancer screening uptake. BMC Womens Health. 2022;22(1):1–14.
Bobdey S, Sathwara J, Jain A, Balasubramaniam G. Burden of cervical cancer and role of screening in India. Indian J Med Pediatr oncology: official J Indian Soc Med Pediatr Oncol. 2016;37(4):278.
Ministry of Health and Family Welfare GoI. NFHS-5 Factsheet. Key Indicators. In. Mumbai: IIPS; 2020.
Mishra R. An epidemiological study of cervical and breast screening in India: district-level analysis. BMC Womens Health. 2020;20(1):1–15.
Dsouza JP, Van den Broucke S, Pattanshetty S. Validity and Reliability of the Indian Version of the HLS-EU-Q16 Questionnaire. Int J Environ Res Public Health. 2021;18(2):495.
Kuder GF, Richardson MW. The theory of the estimation of test reliability. Psychometrika. 1937;2(3):151–60.
Sørensen K, Van den Broucke S, Pelikan JM, Fullam J, Doyle G, Slonska Z, Kondilis B, Stoffels V, Osborne RH, Brand H. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health. 2013;13(1):1–10.
Pelikan JM, Röthlin F, Ganahl K: Measuring comprehensive health literacy in general populations: validation of instrument, indices and scales of the HLS-EU study. In: 6th annual health literacy research conference Bethesda: 2014; 2014.
Binka C, Doku DT, Nyarko SH, Awusabo-Asare K. Male support for cervical cancer screening and treatment in rural Ghana. PLoS ONE. 2019;14(11):e0224692.
Krishnan S, Madsen E, Porterfield D, Varghese B. Advancing cervical cancer prevention in India: implementation science priorities. Oncologist. 2013;18(12):1285.
Faradisa E, Ardiana H, Priyantini D, Fauziah A, Susanti I. A Systematic Review of the Factors Associated with Cervical Cancer Screening Uptake among Women in Low and Middle-Income Countries. Jurnal Ners. 2020;15(2):113–9.
Reichheld A, Mukherjee PK, Rahman SM, David KV, Pricilla RA. Prevalence of cervical cancer screening and awareness among women in an urban community in South India—a cross sectional study. Annals of global health 2020, 86(1).
Nene B, Jayant K, Arrossi S, Shastri S, Budukh A, Hingmire S, Muwonge R, Malvi S, Dinshaw K, Sankaranarayanan R. Determinants of women’s participation in cervical cancer screening trial, Maharashtra, India. Bull World Health Organ. 2007;85:264–72.
Ijezie AE, Johnson OE. Knowledge of cervical cancer and the uptake of the Papanicolaou smear test among public secondary school teachers in Akwa Ibom State, Nigeria. Nigerian Med journal: J Nigeria Med Association. 2019;60(5):245.
Abamecha F, Tena A, Kiros G. Psychographic predictors of intention to use cervical cancer screening services among women attending maternal and child health services in Southern Ethiopia: the theory of planned behavior (TPB) perspective. BMC Public Health. 2019;19(1):1–9.
Moses E, Pedersen HN, Wagner EC, Sekikubo M, Money DM, Ogilvie GS, Mitchell-Foster SM. Understanding Men’s Perceptions of Human Papillomavirus and Cervical Cancer Screening in Kampala, Uganda. J global Oncol. 2018;4:1–9.
Binka C, Nyarko SH, Awusabo-Asare K, Doku DT. Barriers to the uptake of cervical cancer screening and treatment among rural women in Ghana. BioMed research international 2019, 2019.
Siddharthar J, Rajkumar B, Deivasigamani K. Knowledge, awareness and prevention of cervical cancer among women attending a tertiary care hospital in Puducherry, India. J Clin Diagn research: JCDR. 2014;8(6):OC01.
Aswathy S, Quereshi MA, Kurian B, Leelamoni K. Cervical cancer screening: Current knowledge & practice among women in a rural population of Kerala, India. Indian J Med Res. 2012;136(2):205.
Jennings-Dozier K. Predicting intentions to obtain a Pap smear among African American and Latina women: testing the theory of planned behavior. Nurs Res. 1999;48(4):198–205.
Duffett-Leger LA, Letourneau NL, Croll JC. Cervical cancer screening practices among university women. J Obstetric Gynecologic Neonatal Nurs. 2008;37(5):572–81.
Gardner B, de Bruijn GJ, Lally P. Habit, identity, and repetitive action: A prospective study of binge-drinking in UK students. Br J Health Psychol. 2012;17(3):565–81.
Gardner B, Lally P, Rebar AL. Does habit weaken the relationship between intention and behaviour? Revisiting the habit-intention interaction hypothesis. Soc Pers Psychol Compass. 2020;14(8):e12553.
Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol. 2002;186(5):938–43.
Heberer MA, Komenaka IK, Nodora JN, Hsu C-H, Gandhi SG, Welch LE, Bouton ME, Aristizabal P, Weiss BD, Martinez ME. Factors associated with cervical cancer screening in a safety net population. World J Clin Oncol. 2016;7(5):406.
D’Cruz AM, Aradhya MS. Health literacy among Indian adults seeking dental care. Dent Res J. 2013;10(1):20.
Paz-Soldán VA, Bayer AM, Nussbaum L, Cabrera L. Structural barriers to screening for and treatment of cervical cancer in Peru. Reprod Health Matters. 2012;20(40):49–58.
Gossa W, Fetters MD. How should cervical cancer prevention be improved in LMICs? AMA J ethics. 2020;22(2):126–34.
Dsouza JP, Van den Broucke S, Pattanshetty S, Dhoore W. Cervical cancer screening status and implementation challenges: Report from selected states of India. The International Journal of Health Planning and Management 2021.
Baru R, Acharya A, Acharya S, Kumar AS, Nagaraj K. Inequities in access to health services in India: caste, class and region. Economic and political Weekly 2010:49–58.
Dabash R, Vajpayee J, Jacob M, Dzuba I, Lal N, Bradley J, Prasad L. A strategic assessment of cervical cancer prevention and treatment services in 3 districts of Uttar Pradesh, India. Reproductive health. 2005;2(1):1–8.
Montgomery MP, Dune T, Shetty PK, Shetty AK. Knowledge and acceptability of human papillomavirus vaccination and cervical cancer screening among women in Karnataka, India. J Cancer Educ. 2015;30(1):130–7.
Devarapalli P, Labani S, Nagarjuna N, Panchal P, Asthana S. Barriers affecting uptake of cervical cancer screening in low and middle income countries: A systematic review. Indian J Cancer. 2018;55(4):318.
Acknowledgements
The authors are grateful to the Director of Health and Family Welfare of Government of Karnataka for support and permission to conduct the study and disseminate the findings.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JPD, SVDB, WD and SP formulated the study plan and design; JPD acquired permissions with SVDB and SP, JPD did the data collection, interpreted the data and drafted the manuscript. SVDB, WD and SP reviewed the results, provided feedback, read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The ethical approval for the study was obtained from The Institutional Ethics Committee of Manipal Academy of Higher education, KMC Manipal. Community health workers (ASHAs or Accredited Social Health Activists) approached participants and provided the questionnaire, after obtaining informed consent for the study.
Consent for publication
Not applicable.
Competing interests and consent
The authors do not declare any competing interests. All the authors provide their consent for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dsouza, J.P., Van den Broucke, S., Pattanshetty, S. et al. Factors explaining men’s intentions to support their partner’s participation in cervical cancer screening. BMC Women's Health 22, 443 (2022). https://doi.org/10.1186/s12905-022-02019-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-02019-y