Abstract
Background
Pelvic floor muscle training (PFMT) is the first-line treatment for urinary incontinence, but adherence to PFMT is generally poor. Currently, a number of novel strategies exist to facilitate adherence of PFMT. We sought to determine effectiveness of mHealth app-based PFMT for treating stress urinary incontinence (SUI) or stress-predominant mixed urinary incontinence (MUI) in women. The primary objective was to assess the effects of mHealth app-based PFMT and usual treatment on severity of the symptom, the quality of life (QoL) of users and the patient’s global impression of improvement. The secondary objective was to assess how mHealth app use affects adherence of PFMT.
Methods
All randomized controlled trials and quasi-randomized controlled trials aimed at evaluating the effects of mHealth app-based PFMT in women with SUI or stress-predominant MUI were included. Twelve electronic databases, namely the Cochrane Library, PubMed, CINAHL, Embase, Web of science, OVID, SciELO, REHABDATA, PEDro database, Chinese CNKI and Wanfang and the Open Grey databases were used as search sources. The protocol was registered in PROSPERO (CRD 42020183515). This systematic review was developed following the PRISMA 2020 Checklist. The Cochrane Handbook for Systematic Reviews of Interventions for Randomized Controlled Trials was used to assess risk of bias in included studies. Two authors extracted the data into a standardized spreadsheet.
Results
Six studies that met the eligibility criteria were included. The full sample included 439 patients with treatment via mHealth app and 442 controls of usual treatment. ICIQ-UI SF, ICIQ-VS, and QUID scores decreased after follow-up in the mHealth app and control groups in six studies. ICIQ-LUTS QoL scores decreased after follow-up in the mHealth app and control groups in three studies. In only one study, ICIQ-VS QoL scores decreased after 1 month and 2 months of follow-up in the mHealth app group, but increased abruptly after 3 months of follow-up. EQ5D-VAS scores increased in both groups in one study. The percentage of PGI-I increased in the mHealth app group in three studies after follow-up. After follow-up in three studies, BPMSES scores and self-reported adherence scores increased in the mHealth app group relative to the initial time point, but in one study, at 6 months compared with 3 months of follow-up, adherence scores decreased slightly in the mHealth app group.
Conclusions
This systematic review determined that mHealth app-based PFMT showed promise from the perspective of improving both outcomes and exercise adherence.
Similar content being viewed by others
Introduction
SUI is defined by the International Continence Society as “complaint of involuntary loss of urine on effort or physical exertion (e.g., sporting activities), or on sneezing or coughing” [1], and it is common among women and often leads to a significant decline in their QoL [2]. Accumulating epidemiological evidence indicated that the prevalence of SUI across studies varied from 10 to 39% and increased with age [3,4,5]. Data released by the United States Census Bureau recently showed that the demand for care for pelvic floor disorders will increase by 35% between 2010 and 2030 [6].
Evidence-based incontinence treatment can be separated broadly into stress incontinence surgery, medications, behavior and lifestyle modification, with the PFMT most commonly undertaken [7]. PFMT is the first-line conservative management programme for SUI with no adverse reaction [8]. The ideal treatment requires patients to be instructed to perform the exercises properly and persistently commit to it [9,10,11]. There is evidence that women perform better with exercise regimes supervised by medical staff and supervised PFMT showed satisfactory results in alleviating SUI symptoms [12, 13]. However, supervised PFMT is time-consuming, costly, and requires frequent visits to relevant medical institutions, which may hinder long-term treatment adherence. Adherence is considered crucial to PFMT success [14]. Unfortunately, treatment adherence to PFMT is still poor [15].
Mobile health applications (mHealth app) are increasingly being used in health care and public health practice for patient communication, monitoring, education, and to promote adherence to chronic diseases management [16]. A cross-sectional study of 200 adult women in Pennsylvania showed high rates of overall mHealth app ownership, with smartphones accounting for 92%, and women with pelvic floor disorders have high capability of using mHealth app to communicate with their health care providers [17]. MHealth app for PFMT are personal care apps that assist users in training their pelvic floor muscles. A recent systematic review including three eligible studies showed that mHealth app-based PFMT can reduce urinary symptoms [18].
Therefore, this systematic review extends the current literature providing meta-analysis of the most recent RCTs and quasi-randomized controlled trials evaluating mHealth app to deliver PFMT for SUI or stress-predominant MUI. The primary objective was to assess the effects of mHealth app-based PFMT and usual treatment on symptom severity, the QoL of users and the patient’s global impression of improvement. The secondary objective was to assess how mHealth app use affects adherence of PFMT.
Materials and methods
Protocol and registration
This systematic review was developed following the PRISMA 2020 Checklist [19]. The systematic review protocol was registered in the PROSPERO database under number CRD 42020183515.
Study design and eligibility criteria
This systematic review aimed to answer the following guiding question based on the PICO strategy: “Do women with SUI or stress-predominant MUI (P) who use mHealth app for PFMT (I) have better results (O) when compared with women using the usual treatment (C)?”. (1) Participants: participants were women who were diagnosed with SUI or stress-predominant MUI; (2) Intervention: in the intervention group, participants received mHealth app-based PFMT to help women treat or prevent SUI or stress-predominant MUI; (3) Comparison: traditional care (e.g., conventional home-based training without mHealth app) or no treatment in the control group; (4) Outcome: one or more of the following interesting outcomes have been reported (e.g., the severity of symptoms, QoL and the patient’s global impression of improvement were included as main outcome indicators; a secondary outcome measure was adherence to PFMT).
All RCTs and quasi-randomized controlled trials were included and there were no restrictions on year, language, publication status and type of setting.
The studies about qualitative studies, observational studies, review studies, case reports, case control studies, cohort studies, letters to the editor, conference abstracts, personal opinions, and books or book chapters were excluded.
Sources of information and search
We searched the Cochrane Library, PubMed, CINAHL, Embase, Web of science, OVID, SciELO, REHABDATA, PEDro database, Chinese CNKI, Chinese Wanfang, and the Open Grey databases, a total of twelve electronic databases, each from their date of inception to October 2021. Our search strategy involved a combination of the following MeSH and free word [PubMed for example, (“Urinary Incontinence” OR “Stress Urinary Incontinence”) AND (“Pelvic Floor” OR “Pelvic Floor Muscle” OR “Pelvic Floor Muscle Training”) AND (“Woman” OR “Women” OR “Girl” OR “Female”) AND (“Mobile” OR “Portable” OR “Electronic” OR “eHealth” OR “mHealth” OR “App” OR “Software” OR “Reminder Therapy” OR “Programme” OR “Program” OR “System” OR “phone” OR “smartphone” OR “application” OR “web-based”). A reviewer first drafted the search strategy and then defined it through discussions with team members. Two reviewers conducted an independent literature search and thoroughly checked the reference lists of included studies to avoid omitting relevant studies.
Study selection
During the literature screening process, search results from different electronic databases were imported into EndNote Version X9. These studies were selected at three distinct stages. In the first stage, two reviewers performed a methodical analysis of all study titles independently, and titles that did not meet the eligibility criteria were removed.
In the second stage, two reviewers read the abstracts independently for the initial application of the eligibility criteria. Studies containing titles that met the study objectives but did not have abstracts and full text available were removed.
In the last stage, the preliminary eligible studies were assessed in full text to verify whether they met the eligibility criteria. When reviewers disagreed about a particular study, a third reviewer was consulted to make a final decision. All stages were performed to reduce the literature search bias and literature screening bias.
Process of data collection and extraction
After the selection, we used structured forms to extract data from each study, such as authors, year, place of the study, sample characteristics including number of participants and age, SUI diagnosis, name of mHealth app used, control group, information contained in the mHealth app, timing of outcome measurement, reminder frequency and outcome measurement tools.
In the PROSPERO database, the systematic review protocol took adherence as the main outcome measure and incontinence severity as an additional measure. But when we read the relevant literature, we found that mHealth app-based PFMT should first be able to improve the severity of SUI symptoms, and then improve the patient's adherence on the basis of SUI symptom improvement, so that the research will make sense. If the study used adherence as the primary outcome measure, we do not know whether the SUI symptom severity improved if adherence improved. Therefore, after the formal start of the study, we included symptom severity as the primary outcome measure and adherence as the secondary outcome measure.
To assess the impact of mHealth app-based PFMT on SUI symptoms (primary outcomes), the following data were extracted: the assessment of SUI symptoms based on the ICIQ-UI SF, ICIQ-VS and QUID. The ICIQ-UI SF is developed for assessing the prevalence, severity and impact on quality of life. It includes three scored items and one non-scored item, the sum-scores for the ICIQ-UI SF with (total score 0–21). Higher scores indicate more severe symptoms [20]. The ICIQ-VS is a questionnaire for assessing a range of pelvic floor dysfunction symptoms such as bowel, vaginal, and sexual matters. It consists of 14 questions, including 3 separate domains: the vaginal symptom (score from 0 to 53), sexual question (score from 0 to 58) and quality of life (score from 0 to 10). The higher the scores are, the worse the severity of the symptoms is [21]. The QUID consists of two subscales to identify SUI and/or urge urinary incontinence. Each subscale consists of three items to measure the symptom severity of the respective type of UI. Each item includes 6 frequency-based response options, ranging from “none of the time” to “all of the time,” which are scored from 0 to 5 points. The higher the scores are, the worse the severity of the symptoms is [22]. To assess how mHealth app use affects the QoL of users (primary outcomes), the following data were extracted: assessment of QoL specific to the condition based on the ICIQ-LUTS QoL and ICIQ-VS QoL. The ICIQ-LUTS QoL is a condition-specific quality of life questionnaire consisting of 19 items covering different aspects of everyday life that may be affected by leakage or other bladder conditions. These scores add up to a total of 19 to 76 points. A higher score indicates worser QoL [23]. The ICIQ-VS QoL is a questionnaire for assessing a range of pelvic floor dysfunction symptoms such as bowel, vaginal and sexual matters. It is composed of 14 questions, divided into 3 independent domains: the domain of the vaginal symptom, sexual question, and quality of life. The higher the scores are, the worse the severity of the symptoms is [21]. And the assessment of health specific QoL based on the EQ5D-VAS, a vertical VAS with the endpoints 0 (worst imaginable health state) and 100 (best imaginable health state). The higher scores indicate better QoL [24]. To assess the impact of mHealth app use on the patient's global impression of improvement (primary outcomes) through the PGI-I. PGI-I is a validated questionnaire asking the participants to rate their current condition compared to pre-treatment status. There are seven response options, including very much better, much better, a little better, no change, a little worse, much worse, very much worse [25].
Assessing how mHealth app use affects adherence to PFMT (secondary outcome), the following data were extracted: the assessment of the adherence based on the BPMSES and self-reported adherence (from 0 to 10, regarding their commitment to exercises where 0 means “no exercise at all” and 10 means “maximal adherence”).
We resolved any differences by discussions and when both reviewers disagreed, a third one was consulted to make a final decision. Where trial data were possibly collected but not reported, we sought further clarification from the trialists. We processed all included trial data as described in the Cochrane Handbook for Systematic Reviews of Interventions.
Risk of individual bias of the studies
The “Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0” [26] was used to assess risk of bias for selected studies. Two authors assessed independently each domain regarding the potential risk of bias.
We considered random sequence generation, allocation concealment, blinding of participants and intervention implementers, blinding of outcome evaluator, incomplete outcome data, reporting bias and other bias and deemed each category at low, high or unclear risk of bias. Where there was insufficient information to make a clear decision, trials were rated at “unclear risk of bias”. If the research fully meets these criteria, the possibility of various biases is low, and the quality level is A grade; If the research partially meets these standards, the probability of bias is moderate, and the quality level is B grade; If these criteria are not met at all, the possibility of bias is high, and the quality level is C grade. Any disagreements were resolved by discussion.
Summary measures and syntheses of results
The mean scores of the ICIQ-UI SF, ICIQ-VS, and QUID were described to assess the improvement of SUI symptoms. The impact of SUI on the QoL of the individuals was described from the mean scores of the ICIQ-LUTS QoL, ICIQ-VS QoL and EQ5D-VAS. The improvement based on PGI-I results were described by frequency (percentage). The impact of mHealth app-based PFMT on the adherence was described from the mean scores of the BPMSES and the self-reported adherence.
The mean scores of symptoms severity, QoL and adherence were compared between studies by calculating the standardized mean difference (SMD) using the method of Yange and Dalton [18]. The standardized difference was obtained by subtracting the mean post-intervention scores from the mean scores in the initial period of the study, which was weighted by the standard deviation of the between-group differences. Since the post-intervention period varied among eligible studies, the SMD was also weighted according to the number of months between the pre-intervention and post-intervention periods.
Results
Study selection
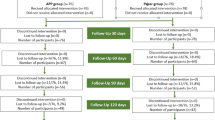
We found five studies in English and one study in Chinese, all six studies in women with SUI. We ultimately included six studies that have important implications for current clinical practice and constructed summary tables of that evidence for SUI. Figure 1 illustrated the detailed process of search, identification, inclusion, and exclusion of studies.
Characteristics of eligible studies
The summary of the main features of the studies can be found in Table 1. The studies were published between 2013 and 2021 and conducted in Sweden [27,28,29,30], Brazil [31], China [32, 33] and Netherlands [34, 35]. The full sample included 439 patients with treatment via mHealth app and 442 controls of usual treatment. Age ranged from 18 to 86 years and all studies informed the ethical criteria involved, including the use of a consent agreement. One study used the URinControl [34, 35], one study used the Tät.nu [27, 28], while another study used the Tät [29, 30]. And one study used the Diário Saúde [31], one study used the Hospital-Community-Family home care [32] and lastly, one study used the Pen Yi Kang [33]. All studies reported that mHealth app provided information about SUI and instructions about PFMT. The follow-up periods consisted in 1 month [31], 6 weeks [33], 2 months [31], 3 months [29, 31, 33], 4 months [27, 34], 6 months [32, 33], 1 year [28, 35] and 2 years [28, 30]. The reminders were sent three times per day [27,28,29,30, 32], twice per day [31], reminders frequency set by the participant [34, 35] and regularly audio reminders during the training [33].
Risk of individual bias of the studies
The risk of bias graph and the risk of bias summary were shown in Figs. 2 and 3. For random sequence generation, six studies were assessed as low risk because the method of random sequence generation was described in detail in the original study [27,28,29,30,31,32,33,34,35]. Six studies reported adequate allocation concealment, three of which were assessed as low risk [29, 31, 33] and the other three as high risk [27, 32, 34]. For blinding of participants and intervention implementers, six studies were considered “not applicable” because intervention group participants cannot be blinded for mHealth app use. For the blinding of outcome evaluator, three studies were assessed as low risk [31, 33, 34], and the other three studies were considered unclear risk due to insufficient descriptions [27, 29, 32]. With regard to the assessment of incomplete outcome data, six studies were rated as low risk. Six studies were judged to be at low risk for reporting bias, and a low risk of other bias was given to six studies.
Primary results of the eligible studies
This systematic review included six original studies, we extracted the data about the severity of symptoms, QoL and adherence, as showed in Tables 2, 3 and 4. Table 2 for example, at the same time point of follow-up, data from up to three studies used the same assessment tool. There were few data at the same time point, so this systematic review provided a narrative synthesis about symptoms severity, QoL and adherence.
Table 2 provides the overall results of symptoms severity assessments based on the ICIQ-UI SF, ICIQ-VS and QUID. Loohuis et al. reported that the change in ICIQ-UI SF symptom score with mHealth app-based treatment (− 2.16 points) was noninferior to that with usual care (− 2.56 points), with a mean difference of 0.06 points between groups after 4 months of follow-up [34], and the ICIQ-UI SF score reduced from 9.5 to 7.0 in the mHealth app group and from 10.3 to 7.1 in the control group after 12 months of follow-up [35]. Wang et al. [33] reported that the ICIQ-UI SF score reduced from 5.7 to 0.3 in the mHealth app group and from 6.1 to 0.4 in the control group after 6 months of follow-up. Araujo et al. [31] showed that after 3 months of follow-up, the ICIQ-UI SF score decreased from 16.3 to 9.1 in the mHealth app group and from 15.9 to 9.7 in the control group, and the ICIQ-VS score reduced from 11.8 to 6.8 in the mHealth app group and from 13.7 to 6.0 in the control group, and finally the QUID score reduced from 14.4 to 7.5 in the mHealth app group and from 15.6 to 3.9 in the control group. Jia et al. [32] verified a reduction of the ICIQ-UI SF score from 8.5 to 4.4 in the mHealth app group and from 8.5 to 8.0 in the control group after 6 months of follow-up. Asklund et al. [29] verified that after 3 months of follow-up, the ICIQ-UI SF score decreased from 11.1 to 7.0 in the mHealth app group and from 11.0 to 10.2 in the control group, and Hoffman et al. [30] found that the ICIQ-UI SF score decreased from 11.1 to 8.1 in the mHealth app group after 2 years of follow-up [30]. Sjöstrom et al. showed that after 4 months of follow-up, the ICIQ-UI SF score decreased from 10.4 to 6.9 in the mHealth app group and from 10.3 to 7.3 in the control group [27], and after 2 years of follow-up, the ICIQ-UI SF score decreased from 10.4 to 6.5 in the mHealth app group and from 10.3 to 6.4 in the control group [28].
Table 3 shows summary results of the assessment of condition-specific and health-specific QoL to the SUI based on the ICIQ-LUTS QoL, ICIQ-VS QoL and EQ5D-VAS. Loohuis et al. reported that after 4 months of follow-up, the change in ICIQ-LUTS QoL score with mHealth app group (− 4.3 points) and usual care group (− 3.8 points), with a mean difference of − 0.57 points between groups [35], and the ICIQ-LUTS QoL score reduced from 33.9 to 28.4 in the mHealth app group and from 33.4 to 29.1 in the control group after 12 months of follow-up [36]. Asklund et al. [30] verified that after 3 months of follow-up, the ICIQ-LUTS QoL score reduced from 34.1 to 28.8 in the mHealth app group and from 34.8 to 34.1 in the control group, and Hoffman et al. [31] found that the ICIQ-LUTS QoL score decreased from 34.1 to 30.2 in the mHealth app group after 2 years of follow-up. Sjöstrom et al. showed that after 4 months of follow-up, the ICIQ-LUTS QoL score reduced from 33.6 to 27.8 in the mHealth app group and from 33.6 to 28.8 in the control group [28], and the ICIQ-LUTS QoL score reduced from 33.6 to 26.5 in the mHealth app group and from 33.6 to 27.2 in the control group after 2 years of follow-up [29]. Health-specific QoL was evaluated with the EQ5D-VAS [37]. After 4 months of follow-up, the EQ5D-VAS score improved from 79.1 to 83.3 in the mHealth app group and improved from 79.2 to 81.8 in the control group, and after 2 years of follow-up, the EQ5D-VAS score increased from 79.1 to 83.3 in the mHealth app group and from 79.2 to 83.5 in the control group. Araujo et al. [32] revealed that the ICIQ-VS QoL score increased from 5.0 to 5.6 in the mHealth app group and reduced from 5.9 to 1.3 in the control group after 3 months of follow-up.
We provided a detailed overview of the patient global impression of improvement of incontinence. Loohuis et al. reported that the majority of women in both the mHealth app-based treatment group (65.7%) and the usual care group (66.6%) had improved overall impressions after a follow-up of 4 months [34]. Asklund et al. [29] provided that the follow-up showed that mHealth app group participants reported much improved or very much improved urinary incontinence more often than control group participants, with an outcome of 91.8% in the mHealth app group. In the analysis of Sjöström et al. [27], participants in the mHealth app group rated their leakage as much better or very much better after treatment (40.9%), compared with participants in the control group (26.5%) after 4 months of follow-up. After a two-year follow-up [28], more participants in the mHealth app group believed that their leakage improvement was very high (39.2%) compared to the control group participants (23.8%).
Secondary results of the eligible studies
Table 4 shows summary results for assessment of the adherence. Wang et al. [33] reported that the average efficacy score improved from 59.9 at 6 weeks to 62.0 at 3 months then declined slightly to 60.4 at 6 months in the mHealth app group, while in the control group, the average score declined continuously from 55.5 at 6 weeks to 51.5 at 6 months. Araujo et al. [31] reported that self-reported adherence rate (attribute a score, from 0 to 10) showed better results during the treatment, which increased from 9.5 to 9.9 in the mHealth app group after 3 months of follow-up. The study of Jia et al. [32] verified an increase in the BPMSES score from 53.8 (average) to 105.4 in the mHealth app group and from 56.5 to 72.9 in the control group after a follow-up of 6 months.
Syntheses of results
Table 5 presented the SMD in ICIQ-UI SF, ICIQ-LUTS QoL and BPMSES scores for the control and mHealth app group in each eligible study. In the studies of Loohuis et al., Wang et al., Araujo et al., Asklund et al. and Sjöström et al. (both for the control group and the mHealth app group), the values of SMD/month for ICIQ-UI SF and ICIQ-LUTS QoL decreased as the follow-up time increased [27,28,29, 31, 33, 35]. Jia et al. showed that the SMD of BPMSES in the control and mHealth app group were 0.82 and 3.11, respectively, after 6 months follow-up [32].
Discussion
This systematic review aimed to summarize the evidence on the effectiveness of mHealth app-based PFMT on outcomes, including SUI symptom severity, QoL, and the patient's global impression of improvement. In addition, this systematic review summarized the evidence on the impact of mHealth app-based PFMT on adherence. We found that mHealth app-based PFMT showed positive effects on primary and secondary indicators. Compared with control group, the mHealth app group had significant improvement in severity of SUI symptoms, QoL and the global impression of patients. The mHealth app group also showed a significant improvement in adherence to PFMT.
PFMT is a first-line strategy for SUI [36]. One possible way to meet the future needs of the medical industry is to enhance patients' self-management capabilities through mHealth app [37, 38]. A number of studies show that mHealth app improve health outcomes [39]. MHealth app are potentially effective for delivering PFMT to women, which is convenient, flexible, and time-saving [40]. Use of mHealth app for PFMT expands access to care and aids the management of patients [27].
Effects of mHealth app-based PFMT on primary objectives
The severity of SUI symptoms
In this systematic review, all original studies that met the inclusion criteria used ICIQ-UI SF to analyze the severity of SUI symptoms. Based on this, when comparing participants in the mHealth app group with those in the control group, a significant decrease in ICIQ-UI SF scores was seen. The summary results of all RCTs and quasi-randomized controlled trials showed that mHealth app-based PFMT improved the severity of SUI symptoms, which is consistent with other studies [18, 41].
QoL
SUI can affect the QoL. This systematic review showed that mHealth app-based PFMT exercises are effective in treating SUI and will improve the QoL of patients. This was probably due to the fact that these women have less SUI symptoms than before and enhanced their self-confidence in daily activities [42].
The patient’s global impression of improvement
The PGI-I is an outcome measure that is readily understood by both the patient and the clinician, and it gives a direct reflection of the patient's overall opinion. The follow-up PGI-I results in our systematic review showed that mHealth app group participants reported much improved. This could be associated with improved urinary symptoms and QoL.
Effects of mHealth app-based PFMT on secondary objective
Adherence
MHealth app-based PFMT works better among people who are interested in it and have higher expectations [41], it has the potential to improve adherence of PFMT [42]. The eligible studies for adherence assessment used the BPMSES and self-reported adherence rate, verifying an increase in the self-efficacy scores of patients in the mHealth app group [32, 33]. This could be explained by the mHealth app group exhibited greater self-efficacy across the follow-up, indicating the efficacy of the mHealth app in improving and maintaining adherence to training. Evidence suggests that participants with higher self-efficacy are more likely to seek out and stick to PFMT protocols [42].
This systematic review assessed the SMD of the ICIQ-UI SF, ICIQ-LUTS QoL and BPMSES scores, comparing initial values with scores in the post-intervention period. In most studies, we found that the SMD was higher in mHealth app group for the ICIQ-UI SF, ICIQ-LUTS QoL and BPMSES than in the control group [27,28,29, 31,32,33]. But the values of SMD/month reduced as the follow-up time increased, it may be associated with the sample loss over time, which is consistent with previous study [18].
Strengths and limitations
Strengths of this systematic review are as follows. First, it offers a literature review on the impact of mHealth app-based PFMT on SUI or stress-predominant MUI. Currently, only two systematic reviews have evaluated the impact of mHealth app-based PFMT on urinary incontinence, but these were limited to qualitative analyses of the results and included an insufficient number of articles. Our systematic review included more studies to evaluate multiple outcomes of the impact of mHealth app-based PFMT on SUI or stress-predominant MUI, including the severity of SUI symptoms, QoL, the patient's global impression of improvement and adherence. Second, we searched a total of 12 databases and systematically reviewed articles using an integrated search strategy, ultimately including six studies.
However, this study also has some limitations. Six studies that meet the inclusion criteria, and three of these trials conducted follow-up studies of the same original population for several years [27,28,29,30, 34, 35], we completed a narrative analysis. Future research should aim to capture more high quality RCTs to allow for statistical analysis of effects on outcomes.
Conclusion
This systematic review determined that mHealth app-based PFMT showed promise from the perspective of improving both outcomes and exercise adherence.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- PFMT:
-
Pelvic Floor Muscle Training
- SUI:
-
Stress Urinary Incontinence
- MUI:
-
Mixed Urinary Incontinence
- QoL:
-
Quality of Life
- RCTs:
-
Randomized Controlled Trials
- ICIQ‐UI SF:
-
International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form
- ICIQ‐VS:
-
International Consultation on Incontinence Questionnaire-Vaginal Symptoms
- QUID:
-
Questionnaire for Urinary Incontinence Diagnosis
- ICIQ-LUTS QoL:
-
International Consultation on Incontinence Questionnaire-Lower Urinary Tract Symptoms Quality of Life
- EQ5D-VAS:
-
The EuroQol 5D-Visual Analogue Scale
- BPMSES:
-
The Broome Pelvic Muscle Self-Efficacy Scale
- PGI-I:
-
Patient's Global Impression of Improvement
- SMD:
-
Standardized Mean Difference
- mHealth app:
-
Mobile Health Applications
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Rada MP, Jones S, Betschart C, Falconi G, Haddad JM, Doumouchtsis SK, et al. A meta-synthesis of qualitative studies on stress urinary incontinence in women for the development of a Core Outcome Set: a systematic review. Int J Gynaecol Obstet. 2021;158:3–12.
Abrams P, Andersson KE, Apostolidis A, Birder L, Bliss D, Brubaker L, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2.
Pathiraja R, Prathapan S, Goonawardena S. Urinary incontinence of women in a nationwide study in Sri Lanka: prevalence and risk factors. Urol J. 2017;14(3):3075–80.
Zhang RQ, Xia MC, Cui F, Chen JW, Bian XD, Xie HJ, et al. Epidemiological survey of adult female stress urinary incontinence. BMC Womens Health. 2021;21(1):172.
Kirby AC, Luber KM, Menefee SA. An update on the current and future demand for care of pelvic floor disorders in the United States. Am J Obstet Gynecol. 2013;209(6):584 e1-e5.
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318(16):1592–604.
Pelvic floor dysfunction: prevention and non-surgical management. National Institute for Health and Care Excellence: Guidelines. London;2021.
Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodyn. 2017;36(2):221–44.
Reed P, Osborne LA, Whittall CM, Emery S. Impact of patient motivation on compliance and outcomes for incontinence. Physiotherapy. 2021;113:100–6.
Bohorquez J, McKinney J, Keyser L, Sutherland R, Pulliam SJ. Development of a wireless accelerometer-based Intravaginal device to detect pelvic floor motion for evaluation of pelvic floor dysfunction. Biomed Microdevices. 2020;22(2):26.
Riemsma R, Hagen S, Kirschner-Hermanns R, Norton C, Wijk H, Andersson KE, et al. Can incontinence be cured? A systematic review of cure rates. BMC Med. 2017;15(1):63.
Price N, Dawood R, Jackson SR. Pelvic floor exercise for urinary incontinence: a systematic literature review. Maturitas. 2010;67(4):309–15.
McClurg D, Frawley H, Hay-Smith J, Dean S, Chen SY, Chiarelli P, et al. Scoping review of adherence promotion theories in pelvic floor muscle training—2011 ICS state-of-the-science seminar research paper I of IV. Neurourol Urodyn. 2015;34(7):606–14.
Latorre GFS, de Fraga R, Seleme MR, Mueller CV, Berghmans B. An ideal e-health system for pelvic floor muscle training adherence: Systematic review. Neurourol Urodyn. 2019;38(1):63–80.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2): e52.
Lee DD, Arya LA, Andy UU, Sammel MD, Harvie HS. Willingness of women with pelvic floor disorders to use mobile technology to communicate with their health care providers. Female Pelvic Med Reconstr Surg. 2019;25(2):134–8.
Leme Nagib AB, Riccetto C, Martinho NM, Camargos Pennisi PR, Blumenberg C, Paranhos LR, et al. Use of mobile apps for controlling of the urinary incontinence: a systematic review. Neurourol Urodyn. 2020;39(4):1036–48.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30.
Price N, Jackson SR, Avery K, Brookes ST, Abrams P. Development and psychometric evaluation of the ICIQ Vaginal Symptoms Questionnaire: the ICIQ-VS. BJOG. 2006;113(6):700–12.
Bradley CS, Rovner ES, Morgan MA, Berlin M, Novi JM, Shea JA, et al. A new questionnaire for urinary incontinence diagnosis in women: development and testing. Am J Obstet Gynecol. 2005;192(1):66–73.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997;104(12):1374–9.
EuroQol G. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
Yalcin I, Bump RC. Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol. 2003;189(1):98–101.
Cumpston M, Li T, Pae MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142.
Sjostrom M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: a randomised controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112(3):362–72.
Sjostrom M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: 1- and 2-year results of a randomized controlled trial with a focus on pelvic floor muscle training. BJU Int. 2015;116(6):955–64.
Asklund I, Nystrom E, Sjostrom M, Umefjord G, Stenlund H, Samuelsson E. Mobile app for treatment of stress urinary incontinence: a randomized controlled trial. Neurourol Urodyn. 2017;36(5):1369–76.
Hoffman V, Soderstrom L, Samuelsson E. Self-management of stress urinary incontinence via a mobile app: two-year follow-up of a randomized controlled trial. Acta Obstet Gynecol Scand. 2017;96(10):1180–7.
Araujo CC, Marques AA, Juliato CRT. The adherence of home pelvic floor muscles training using a mobile device application for women with urinary incontinence: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020;26(11):697–703.
Jia J, Xu J, Qiu X. Application of hospital-community-family incontinence care platform in the management of patients with stress urinary incontinence. Chin J Nurs. 2018;53(05):533–6.
Wang X, Xu X, Luo J, Chen Z, Feng S. Effect of app-based audio guidance pelvic floor muscle training on treatment of stress urinary incontinence in primiparas: a randomized controlled trial. Int J Nurs Stud. 2020;104: 103527.
Loohuis AMM, Wessels NJ, Dekker JH, van Merode NAM, Slieker-Ten Hove MCP, Kollen BJ, et al. App-based treatment in primary care for urinary incontinence: a pragmatic. Randomized Controlled Trial Ann Fam Med. 2021;19(2):102–9.
Loohuis AMM, Van Der Worp H, Wessels NJ, Dekker JH, Slieker-Ten Hove MCP, Berger MY, et al. One year effectiveness of an app-based treatment for urinary incontinence in comparison to care as usual in Dutch general practice: a pragmatic randomised controlled trial over 12 months. BJOG. 2021;129:1474–80.
Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654.
Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA. 2013;310(22):2395–6.
Zhou X, Feng X, Lu S, Zhou Y. Research progress on the application of mobile medicine in the self-management of female patients with stress urinary incontinence. Chin Nurs Manag. 2019;19(04):598–602.
Doocy S, Paik KE, Lyles E, Hei Tam H, Fahed Z, Winkler E, et al. Guidelines and mHealth to improve quality of hypertension and type 2 diabetes care for vulnerable populations in lebanon: longitudinal cohort study. JMIR Mhealth Uhealth. 2017;5(10):e158.
Asklund I, Samuelsson E, Hamberg K, Umefjord G, Sjostrom M. User experience of an app-based treatment for stress urinary incontinence: qualitative interview study. J Med Internet Res. 2019;21(3):e11296.
Widdison R, Rashidi A, Whitehead L. Effectiveness of mobile apps to improve urinary incontinence: a systematic review of randomised controlled trials. BMC Nurs. 2022;21(1):32.
Pires TF, Pires PM, Costa R, Viana R. Effects of pelvic floor muscle training in pregnant women. Porto Biomed J. 2020;5(5):e077.
Acknowledgements
We are grateful to all authors for their support of this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
YH: Search literature, Manuscript writing, Manuscript editing. YJ: Construction of the systematic review protocol, PROSPERO registration, Search literature. SF: Study selection, Data collection and extraction, Risk of individual bias of the studies, Manuscript revision. BT: Study selection, Data collection and extraction, Risk of individual bias of the studies. SL: A third reviewer to make a final decision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hou, Y., Feng, S., Tong, B. et al. Effect of pelvic floor muscle training using mobile health applications for stress urinary incontinence in women: a systematic review. BMC Women's Health 22, 400 (2022). https://doi.org/10.1186/s12905-022-01985-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01985-7