Abstract
Background
Family caregivers may be at a higher risk for several chronic diseases, including cancer. Cervical cancer is one of the most common causes of cancer death among women. Despite family caregivers’ vulnerability, the status of their HPV awareness, knowledge, and preventive health behaviors, including cervical cancer screening, has been understudied. Thus, this study aimed to examine the sociodemographic factors associated with HPV awareness and knowledge and adherence to the cervical cancer screening guidelines among caregivers in the U.S.
Methods
Nationally representative cross-sectional survey data were obtained from the Health Information National Trends Survey (HINTS 5, 2017–2020). Female caregivers aged 21–65 were included (N = 1190). Weighted multivariable logistic regression was performed to identify factors associated with HPV awareness (heard of HPV), knowledge (HPV can cause cervical cancer), and adherence to the United States Preventive Service Task Force 2018 cervical cancer screening guidelines by sociodemographic factors (age, race/ethnicity, education, household income, marital status,) and the intensity of caregiving.
Results
An estimated 79% of female caregivers were aware of HPV and 84% adhered to the cervical cancer screening guidelines. Caregivers who were older than 50 (OR = 3.62, 1.91–6.85, adherence of aged 21–50 vs. 51–65), Hispanics of race/ethnicity compared with Black/African Americans (OR = 3.14, 1.31–7.52, adherence of Black/African Americans vs. Hispanics), with a high school education or less (OR = 2.34, 1.14–4.82, adherence of Some college or more vs. High school education or less), and with intense caregiving duty (spending 35 h/week or more on caregiving) compared with light-duty (OR = 2.34, 1.10–5.00, adherence of 5–14 h vs. 35 h or more, weekly) had poor adherence to the cervical cancer screening guidelines. Caregivers who were older, racial minorities (Asian, Native Hawaiian/Pacific Islander, American Indian/Alaska Native, Multiple races), and less educated showed lower HPV awareness (Heard of HPV) than their counterparts.
Conclusions
There are caregiving populations whose HPV awareness and cervical cancer screening adherence are low. To improve their awareness and knowledge of HPV and support their cervical cancer screening behaviors, we need to consider interventions that target those specific populations.
Similar content being viewed by others
Introduction
A family caregiver is defined as “any relative, partner, friend or neighbor who has a significant personal relationship with, and provides a broad range of assistance for, an older person or an adult with a chronic or disabling condition” [1]. Approximately 53 million individuals were family caregivers in the U.S. in 2020 [2]. More than one in five people (21%) provided unpaid healthcare or functional needs for their family members [2]. Caregivers are often described as hidden patients because caregiving is burdensome as it requires physical, emotional, and financial sacrifices and is usually a long-term commitment, spanning from several years to over a decade [3]. About a quarter of caregivers (26%) report spending over 20 h per week providing care [4]. Consequentially, this population is vulnerable to an unhealthy lifestyle, including insufficient sleep, and is at higher risk for chronic diseases, including depressive disorder and cancer [5,6,7,8,9].
The majority of caregivers are female (61%) [4], and the average age of female caregivers is 50.1 years [2]. Cervical cancer is the most common gynecological cancer and the average age at diagnosis is 50 [10]. It is also one of the most common causes of cancer death among U.S. women despite advances in cervical cancer prevention and treatment [10]. Over 90% of cervical cancer can be attributable to high-risk Human Papillomavirus infection. Papanicolaou cytology (Pap smear) detects cell changes caused by HPV and allows at-risk women to receive treatment before it becomes invasive carcinoma. As early detection can significantly reduce cervical cancer incidence and mortality, active cervical cancer screening is strongly recommended as an effective prevention strategy. The U.S. Preventive Services Task Force (USPSTF 2018) recommends cervical cytology every 3 years for women aged 21–29 years old and for women aged 30–65 years old, either cervical cytology every 3 years, high-risk Human papillomavirus (hrHPV) testing every 5 years, or hrHPV testing in combination with cytology (co-testing) every 5 years [11]. These guidelines, updated in 2018, highlight the importance of adhering to preventative cervical cancer screenings while providing more options for hrHPV testing in addition to Pap testing.
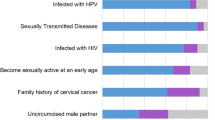
In 2022, 14,100 new cervical cancer cases and 4280 cervical cancer death were reported despite effective prevention and treatment options [12]. In the latest report, the disparities in cervical cancer incidence and mortality by socioeconomic status among U.S. women were still observed [12]. Despite the threat of cervical cancer, knowledge regarding the causes of cervical cancer and the linkage to HPV infection (referred to as HPV knowledge) has been low to moderate among Americans [13,14,15]. Furthermore, HPV knowledge level differs by sociodemographic characteristics (e.g., race/ethnicity, age, income, educational attainment, insurance status, rurality of residence) [15,16,17,18,19,20,21,22]. HPV knowledge level was lower in racial/ethnic minorities (particularly among Hmong and Korean Asian Americans and Hispanics), older populations, and rural residents [15,16,17,18,19,20,21,22]. Adherence to the cervical cancer screening guidelines (e.g., pap smear within the past 3 years) has been moderate to high [23, 24]. Previous analysis of HINTS data (2013–2014) revealed that 81.3% of 21–65 years reported that they had a Pap smear in the past 3 years [25]. However, stark disparities in sociodemographic factors were observed in cervical cancer screening behavior [3,4,5, 23, 26,27,28,29,30,31,32]. For example, pap test was less utilized among women who are older, racial/ethnic minorities (African American, Asians, Hispanics) [4, 26, 32], and women with low socioeconomic status (SES). Low SES includes women with low income, low educational attainment, no health insurance, and women who lack a usual source of healthcare [3, 5, 27,28,29,30,31].
While multiple studies have shown disparities in HPV knowledge and cervical cancer screening behavior in women in the U.S., studies focused on family caregivers’ negative health behaviors due to the caregiving burden and the receipt of preventive clinical services, including cancer screenings, are still scant with inconsistent results [33,34,35,36,37,38,39,40,41,42]. Studies have reported that caregivers’ were less likely to receive cervical cancer screening because of caregiving duties [33,34,35,36], caregivers were more aware of the preventive health services and hence actively participating in them [39,40,41,42], and or have reported no association [34, 37, 38].
Despite the inconsistent findings, there has been a longstanding concern that caregivers are less likely to receive cancer screenings because the burden of caregiving may hinder them from obtaining care for themselves. This is alarming as their health status is already vulnerable [5,6,7,8, 33,34,35,36]. While we can reasonably assume that subgroups of caregivers may have disproportionately low cervical cancer screening rates and low HPV awareness and knowledge, little is known in this area. Knowing which caregiver subgroups are not up to date with their cervical cancer screening and which subgroups lack HPV knowledge could contribute to developing targeted interventions to mitigate existing inequities [43]. Therefore, this study aimed to identify sociodemographic factors associated with disparities in HPV awareness and knowledge and cervical cancer screening behaviors among female caregivers in the U.S.
Methods
Data source
This study used publicly available cross-sectional data from the Health Information National Trends Survey (HINTS) [44]. HINTS is a self-administered nationally representative survey conducted by the National Cancer Institute. The present study used HINTS 5 Cycles 1–4 in 2017–2020. HINTS 5 is a single-mode mailed survey using a two-stage sample design except for Cycle 3, as Cycle 3 employed a push-to web pilot method in addition to the mailed survey. HINTS 5 included data on the caregiver population, their health-related behavior, perception, and knowledge of the disease. Geographic addresses were stratified by areas with a high or low concentration of minority populations in HINTS 5 Cycles 2–4. HINTS 5 Cycle 1 included one more stratification in geographic address, counties of Central Appalachia. The present study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline [45]. HINTS 5 included 16,092 respondents; 3285 in cycle 1 (2017, response rate: 32.4%), 3504 in cycle 2 (2018, response rate: 32.4%), 5,438 in cycle 3 (2019, response rate: 30.3%), and 3865 in cycle 4 (2020, response rate: 36.7%). The response rate was estimated based on the Response Rate 2 formula from the American Association of Public Opinion Research [46]. In our analysis, we included female caregivers aged 21–65 (n = 1190) because that is the population recommended to obtain a regular cervical cancer screening every 3 years by the USPSTF 2018.
Caregiver status
Caregiving status was identified by one question; “Are you currently caring for or making health care decisions for someone with a medical, behavioral, disability, or other condition?” Those who affirmatively responded ‘yes’ were defined as caregivers.
Outcome variables
HPV awareness (Heard of HPV) and HPV knowledge (HPV can cause cervical cancer)
The following question was used to investigate caregivers’ awareness of Human Papillomavirus (HPV): “Have you ever heard of HPV? HPV stands for Human Papilloma Virus. It is not HCV, HIV, or Herpes.” Among respondents who answered, ‘yes’ to HPV awareness, HPV knowledge was assessed with the question, “Do you think HPV can cause cervical cancer?” In this study, HPV knowledge was defined as having knowledge of the causal effect of HPV on cervical cancer.
Adherence to the cervical cancer screening guidelines (Had a pap test within 3 years)
To distinguish the caregivers who were compliant with the USPSTF 2018 cervical cancer screening guidelines, the question, “How long ago did you have your most recent Pap test to check for cervical cancer?” was used. Those who answered, “I have never had a Pap test,” were re-coded to “Never.” Caregivers with all other answers were divided into “within guidelines” if they had a pap test within the past 3 years or “outside guidelines” if they had a pap test more than 3 years ago. As only 18 women reported never receiving a Pap test, we only included ‘within guidelines’ and ‘outside guidelines’ in our analysis, and ‘Never’ was excluded.
Covariates
The social determinants of health framework from the Healthy People 2030 was used to determine the sociodemographic predictors for this study [47]: Age (21–50, 51–65), race/ethnicity (White, Hispanic, African American/Black, Others including Asian, Native Hawaiian/Pacific Islander, American Indian/Alaska Native, Multiple races), household income (less than $20,000, $20,000 to less than $35,000, $35,000 to less than $50,000, $50,000 or more), educational attainment (high school graduate or less, some college or more), marital status (married or living with a romantic partner as married vs. not married including divorced, widowed, separated, single/never been married), employment status (employed vs. unemployed including homemaker, student, retired, disabled), health insurance type (insured by employment or private insurance, Tricare/VA/Indian Health Services, Medicare, Medicaid). Besides the sociodemographic factors, weekly time spent on caregiving (less than 5 h, 5–14 h, 15–20 h, 21–34 h, 35 h or more) was included.
Statistical analysis
The prevalence of HPV awareness, HPV knowledge, and adherence to cervical cancer screening guidelines were reported [frequency, weighted percentage, and 95% confidence interval (95% CI)]. To examine the association between characteristics and the three outcomes of interest (1) HPV awareness (heard of HPV), (2) HPV knowledge (HPV can cause cervical cancer), and (3) adherence to the cervical cancer screening guidelines (a Pap smear within 3 years), weighted multivariable logistic regression was performed to obtain odds ratios (ORs) and 95% CIs. Models for HPV awareness and knowledge were adjusted by sociodemographic factors, and the model for screening uptake was additionally adjusted for time spent on caregiving. The statistical significance was determined at a p value less than 0.05. A complete case analysis approach was used to manage missing data. All estimates accounted for the sampling strategy using full sample weights and survey procedures in SAS (SAS Studio, version 9.4, Cary, NC).
Results
Among female caregivers aged 21–65, 39% were aged 51–65, 63% were non-Hispanic White, 46% reported less than $50,000 annual household income, 24% had a high school education or less, 60% were employed, 64% were married, 67% were insured by an employment-based or private plan while 33% were insured by a government health plan (Medicare, Medicaid, Tricare, VA, Indian Health Services), and approximately 98% were urban residents. An estimated 33% spent 35 h or more on caregiving activities weekly (Table 1).
HPV awareness (Heard of HPV) and HPV knowledge (HPV can cause cervical cancer)
Approximately 79% of female caregivers (aged 21–65) heard of HPV, and the majority of participants thought that HPV could cause cervical cancer (99%) (Table 2). However, disparities in HPV awareness were found by sociodemographic characteristics (Table 3). Younger female caregivers (21–50) were nearly 2.5 times as likely to have heard of HPV compared with older caregivers [50,51,52,53,54,55,56,57,58,59,60,61,62,63,64] (OR = 2.47, 95% CI = 1.49, 4.08). Hispanic caregivers had 3.5 times the odds of having heard of HPV compared to other race/ethnic groups (OR = 0.29, 95% CI = 0.12, 0.70). Female caregivers with some college or more education had 3 times the odds of having heard of HPV compared with their less-educated counterparts (OR = 2.92, 95% CI = 1.72, 4.94).
Adherence to the cervical cancer screening guidelines (Had a pap test within 3 years)
Among female caregivers who had ever had a pap test, 84% had a pap test in the past 3 years (Table 2). As shown in Table 4, younger caregivers (21–50 years) were 3.5 times as likely to follow the cervical cancer screening guidelines compared with older caregivers (51–65 years) (OR = 3.62, 95% CI = 1.91, 6.85). Black/African American caregivers were 3 times as likely to adhere to the cervical cancer screening guidelines compared with Hispanics (OR = 3.14, 95% CI = 1.31, 7.52). More educated caregivers (some college or more) were almost 2.5 times as likely to obtain cervical cancer screening compared with their less-educated counterparts (high school or less) (OR = 2.34, 95% CI = 1.14, 4.82). Caregivers who spent fewer hours on caregiving (5–14 h weekly) were almost 2.5 times as likely to adhere to the screening guidelines as those who spent most hours (35 h or more) (OR = 2.34, 95% CI = 1.10, 5.00).
Discussion
This study assessed sociodemographic factors associated with HPV awareness (heard of HPV), HPV knowledge (HPV can cause cervical cancer), and adherence to the cervical cancer screening guidelines (had a pap test within 3 years) among female caregivers in the U.S. from 2017 to 2020, using nationally representative survey data (HINTS 5, Cycles 1–4). Female caregivers who were older, racial/ethnic minorities, and those with less education had lower HPV awareness and cervical cancer screening adherence. Intense caregiving duty (spending 35 h/week or more on caregiving) was also associated with low adherence to the cervical cancer screening guidelines. Compared to the general population in the U.S., there were some similarities and differences. Similar to women in the general population, women caregivers who were older, racial/ethnic minorities, and those who were less educated were less likely to be aware of HPV and less likely to adhere to the cervical cancer screening guidelines [48,49,50,51]. However, income was associated with HPV awareness in the general population, but not among caregivers, and age and education were not related to HPV knowledge among caregivers, unlike the general U.S. population [48].
Older age was associated with low HPV awareness and low uptake of cervical cancer screening among caregivers. Plausible explanations could include that HPV vaccination campaigns and recommendations target young girls and/or healthcare professionals may focus more on younger age groups (11–12 years rather than 21–26 years) to promote HPV vaccine uptake and series completion [52,53,54]. This could result in more chances of being exposed to the HPV awareness campaigns among young teenagers and their mothers, who are most likely in their 30 s or 40 s. Older caregivers were far behind (75%) the targeted adherence to the cervical cancer screening guidelines (84.3%) set by Healthy People 2030 among U.S. women [55] compared to their younger counterparts (91%). The association between age and adherence to the screening guidelines could be explained by the relationship that low HPV awareness and knowledge are closely related to low cervical cancer screening [56, 57]. Considering the average diagnosed age of cervical cancer in the U.S. is 50, efforts targeting this older age group are needed to improve and maintain their adherence to the USPSTF guidelines.
We found that HPV awareness was lower among caregivers who were racial/ethnic minorities. Specifically, Hispanic caregivers were less likely to obtain preventive cancer screening behaviors compared with their Black/African American counterparts. Low HPV awareness and knowledge and low cervical cancer screening uptake has been previously reported among Hmong, a growing Southeast Asian American population, and Korean Asian Americans, and Hispanic women [18, 19, 21, 22, 50, 51, 58, 59].
We also found that HPV awareness was lower among caregivers who had less educational achievement. Individuals with higher education and higher income are more likely to have higher health literacy and greater access to health resources, which can possibly increase their knowledge and awareness of HPV. However, HPV knowledge was not different by socioeconomic status in our study. A potential explanation could be that only those who were already aware of HPV were asked further HPV knowledge questions. Thus, it would have been challenging to identify sociodemographic disparities in HPV knowledge in our sample. Our findings support the need for tailored interventions that take into consideration the individual (e.g., lack of knowledge in cervical cancer etiology and screening services available) [59, 60], sociocultural (e.g., low levels of acculturation, gynecologic clinic attending is hindered by male partner) [61, 62], and systematic barriers (e.g., lack of access to the services) [63, 64] to cervical cancer screening services among Hispanic caregivers.
Long caregiving hours (35 h or more weekly) were associated with low adherence to cervical cancer screening guidelines among caregivers. Several studies that examined the associations between caregiving, the caregiving burden, and low engagement in preventative cancer services reported inconclusive results [36,37,38, 65]. Our findings provide evidence to strengthen the rationale for developing tailored strategies targeting individuals with intense caregiving duty to promote cancer screening behaviors. Further studies will be warranted to comprehensively assess the associations of caregiving burden with cancer screening uptake, using standardized measures (e.g., Zarit score) with larger sample sizes. Additionally, a qualitative approach would be warranted to examine the detailed barriers that hinder cervical cancer screening uptake for those with poor adherence.
A recent study reported that the most common reason for not receiving timely screening was lack of screening knowledge [66]. Addressing disparities in HPV awareness and knowledge and cervical cancer screening behaviors is important for caregivers because this population needs additional support to promote their optimal health given their at-risk health condition and crucial role in care recipients’ health [67, 68]. Determining which caregiver subgroups are overdue for cervical cancer screenings could inform relevant stakeholders, including clinicians, who have a primary role in recommending screening to eligible caregivers [66].
Limitation
The current study has several limitations. First, HINTS is a cross-sectional survey and cannot provide knowledge of temporality or causal associations. Second, as HINTS data is self-reported, we need to acknowledge the possibility of respondent biases. Respondents may have mis-reported the dates of their last Pap Smear test, especially if it happened 2–3 years ago (recall bias). Moreover, respondents might not always honestly report their knowledge and behaviors, which potentially could lead to either an increase or decrease in screening rates (reporting bias). Third, the small sample size may be related to some of the non-significant results. Fourth, there is a possibility of mislabeling the screening guideline-compliant individuals as non-compliant due to the potential confusion between hrHPV test and a Pap smear. As HINTS only asks about a Pap smear as a preventative screening service for cervical cancer, we might have underestimated the percent who were screening-compliant, as we did not include those who received hrHPV testing every 5 years. Since there is an increasing trend of using hrHPV test over a Pap smear due to convenience in recent years [69], we would suggest HINTS incorporate hrHPV testing into the Pap smear questionnaire to properly specify people with preventative cervical cancer screening behaviors. Fifth, potentially, the changes in cervical cancer screening guidelines that happened over the survey period might have affected women's cervical cancer screening knowledge and behaviors [66]. Last, this study did not include the rurality of residence as a sociodemographic factor despite the potential association with disparities in HPV awareness and knowledge as well as adherence to the guidelines of cervical cancer screening [67, 69, 70]. Because nearly 98% of caregivers were urban residents, we did not think we could have meaningful results out of this population distribution. However, further investigation is needed to better understand how rurality of residence is associated with caregivers' cervical cancer screening behaviors, including the caregiving burden among rural residents [70].
Conclusion
We found that sociodemographic factors, particularly age, race/ethnicity, educational attainment, and the intensity of caregiving, were associated with disparities in HPV awareness and adherence to the cervical cancer screening guidelines among female caregivers in the U.S. The value of this study is the suggestion that targeted interventions should focus on female caregivers who are aged 51–65, racial/ethnic minorities (Hispanics and other race/ethnic groups, including Asian, Native Hawaiian/Pacific Islander, American Indian/Alaska Native, Multiple races), have low educational attainment (high school graduate or less) and spend 35 h or more on caregiving weekly. Therefore, targeted interventions to improve HPV awareness and cervical cancer screening adherence are urgently required to mitigate existing inequities among these vulnerable subgroups of caregiving women in the U.S.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the Health Information National Trends Survey, https://hints.cancer.gov/data/default.aspx
Abbreviations
- HINTS:
-
Health Information National Trends Survey
- HPV:
-
Human papillomavirus
- BRFSS:
-
Behavioral Risk Factor Surveillance System
- Pap Smear:
-
Papanicolaou cytology
- USPSTF:
-
U.S. Preventive Services Task Force
References
Definitions - Family Caregiver Alliance. [cited 2022 Mar 15]. https://www.caregiver.org/resource/definitions-0/.
Caregiving in the US 2020 | The National Alliance for Caregiving. [cited 2021 Aug 21]. https://www.caregiving.org/caregiving-in-the-us-2020/.
Hewitt M, Devesa SS, Breen N. Cervical cancer screening among U..S women: analyses of the 2000 National Health Interview Survey. Prev Med (Baltim). 2004;39(2):270–8.
Taylor VM, Nguyen TT, Jackson JC, McPhee SJ. Cervical cancer control research in Vietnamese American communities. Cancer Epidemiol Biomark Prev. 2008;17(11):2924–30.
Martin LM, Calle EE, Wingo PA, Heath CW. Comparison of mammography and Pap test use from the 1987 and 1992 National Health Interview Surveys: are we closing the gaps? Am J Prev Med. 1996;12(2):82–90.
Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Philos Rhetor 1977;10(2). https://philpapers.org/rec/FISBAI.
Ajzen I. Understanding attitudes and predicting social behavior. ed. Journal of Personality and Social Psychology, 1992, 98–109. Englewood Cliffs: Prentice-Hall; 1980. p. 278.
Cohen SA, Kunicki ZJ, Nash CC, Drohan MM, Greaney ML. Rural-urban differences in caregiver burden due to the COVID-19 pandemic among a national sample of informal caregivers. Gerontol Geriatr Med. 2021;7:23337214211025124.
CDC - BRFSS. [cited 2021 Aug 21] https://www.cdc.gov/brfss/index.html.
Fontham ETH, Wolf AMD, Church TR, Etzioni R, Flowers CR, Herzig A, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70(5):321–46.
Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Screening for cervical cancer us preventive services task force recommendation statement. JAMA J Am Med Assoc. 2018;320(7):674–86.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. https://doi.org/10.3322/caac.21708.
Bendik MK, Mayo RM, Parker VG. Knowledge, perceptions, and motivations related to HPV vaccination among college women. J Cancer Educ. 2011;26(3):459–64.
Boakye EA, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum Vaccin Immunother. 2017;13(11):2713.
Holcomb B, Bailey JM, Crawford K, Ruffin MT. Adults’ knowledge and behaviors related to human papillomavirus infection. J Am Board Fam Pract. 2004;17(1):26–31.
McBride KR, Singh S. Predictors of adults’ knowledge and awareness of HPV, HPV-associated cancers, and the HPV vaccine: implications for health education. Health Educ Behav. 2018;45(1):68–76.
Watkins KL, Reitzel LR, Wetter DW, McNeill LH. HPV awareness, knowledge and attitudes among older African-American women. Am J Health Behav. 2015;39(2):204–10.
Davlin SL, Berenson AB, Rahman M. Correlates of HPV knowledge among low-income minority mothers with a child 9–17 years of age. J Pediatr Adolesc Gynecol. 2015;28(1):19–23.
Strohl AE, Mendoza G, Ghant MS, Cameron KA, Simon MA, Schink JC, et al. Barriers to prevention: knowledge of HPV, cervical cancer, and HPV vaccinations among African American women. Am J Obstet Gynecol. 2015;212(1):65.e1-65.e5.
Mohammed KA, Subramaniam DS, Geneus CJ, Henderson ER, Dean CA, Subramaniam DP, et al. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med (Baltim). 2018;109:39–43.
Beltran R, Simms T, Lee HY, Kwon M. HPV literacy and associated factors among hmong american immigrants: implications for reducing cervical cancer disparity. J Community Health. 2016;41(3):603–11.
Lee HY, Choi YJ, Yoon YJ, Oh J. HPV literacy: the role of English proficiency in Korean American immigrant women. Clin J Oncol Nurs. 2018;22(3):E64–70.
Spadea T, Bellini S, Kunst A, Stirbu I, Costa G. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups: a review. Prev Med (Baltim). 2010;50(4):159–64.
Nelson W, Moser RP, Gaffey A, Waldron W. Adherence to cervical cancer screening guidelines for U.S. women aged 25–64: data from the 2005 Health Information National Trends Survey (HINTS). J Women’s Health. 2009;18(11):1759.
Luque JS, Tarasenko YN, Chen C. Correlates of cervical cancer screening adherence among women in the U.S.: findings from HINTS 2013–2014. J Prim Prev. 2018;39(4):329–44.
Fernández LE, Morales A. Language and use of cancer screening services among border and non-border Hispanic Texas women. Ethn Health. 2007;12(3):245–63. https://doi.org/10.1080/13557850701235150.
Hsia J, Kemper E, Kiefe C, Zapka J, Sofaer S, Pettinger M, et al. The importance of health insurance as a determinant of cancer screening: evidence from the Women’s Health Initiative. Prev Med (Baltim). 2000;31(3):261–70.
Akinlotan M, Bolin JN, Helduser J, Ojinnaka C, Lichorad A, McClellan D. Cervical cancer screening barriers and risk factor knowledge among uninsured women. J Community Health. 2017;42(4):770–8.
Limmer K, LoBiondo-Wood G, Dains J. Predictors of cervical cancer screening adherence in the United States: a systematic review. J Adv Pract Oncol. 2014;5(1):31.
Selvin E, Brett KM. Breast and cervical cancer screening: sociodemographic predictors among White, Black, and Hispanic women. Am J Public Health. 2003;93(4):618.
Somkin CP, McPhee SJ, Nguyen T, Stewart S, Shema SJ, Nguyen B, et al. The effect of access and satisfaction on regular mammogram and Papanicolaou test screening in a multiethnic population. Med Care. 2004;42(9):914–26.
American Cancer Society. Cancer Prevention & Early Detection Facts & Figures 2019–2020. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-prevention-and-early-detection-facts-and-figures/cancer-prevention-and-early-detection-facts-and-figures-2019-2020.pdf.
Bradley PJ. Family caregiver assessment. Essential for effective home health care. J Gerontol Nurs. 2003;29(2):29–36.
Kim C, Kabeto MU, Wallace RB, Langa KM. Quality of preventive clinical services among caregivers in the health and retirement study. J Gen Intern Med. 2004;19(8):875–8.
McGuire LC, Bouldin EL, Andresen EM, Anderson LA. Examining modifiable health behaviors, body weight, and use of preventive health services among caregivers and non-caregivers aged 65 years and older in Hawaii, Kansas, and Washington using 2007 BRFSS. J Nutr Health Aging. 2010;14(5):373–9.
Son KY, Park SM, Lee CH, Choi GJ, Lee D, Jo S, et al. Behavioral risk factors and use of preventive screening services among spousal caregivers of cancer patients. Support Care Cancer. 2011;19(7):919–27.
Sarna L, Chang BL. Colon cancer screening among older women caregivers. Cancer Nurs. 2000;23(2):109–16.
Reeves KW, Bacon K, Fredman L. Caregiving associated with selected cancer risk behaviors and screening utilization among women: cross-sectional results of the 2009 BRFSS. BMC Public Health. 2012;12(1):1–8. https://doi.org/10.1186/1471-2458-12-685.
McCaffery K, Forrest S, Waller J, Desai M, Szarewski A, Wardle J. Attitudes towards HPV testing: a qualitative study of beliefs among Indian, Pakistani, African-Caribbean and white British women in the UK. Br J Cancer. 2003;88(1):42–6.
Chua MS, Mok TS, Kwan WH, Yeo W, Zee B. Knowledge, perceptions, and attitudes of Hong Kong Chinese women on screening mammography and early breast cancer management. Breast J. 2005;11(1):52–6.
Juon HS, Kim M, Shankar S, Han W. Predictors of adherence to screening mammography among Korean American women. Prev Med (Baltim). 2004;39(3):474–81.
Yavan T, Akyüz A, Tosun N, İyigÜn E. Women’s breast cancer risk perception and attitudes toward screening tests. J Psychosoc Oncol. 2010;28(2):189–201.
Islami F, Fedewa SA, Jemal A. Trends in cervical cancer incidence rates by age, race/ethnicity, histological subtype, and stage at diagnosis in the United States. Prev Med (Baltim). 2019;1(123):316–23.
Survey Instruments | HINTS. [cited 2021 Aug 23]. https://hints.cancer.gov/data/survey-instruments.aspx.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
Standard Definitions Final Dispositions of Case Codes and Outcome Rates for Surveys Revised 2016 RDD Telephone Surveys In-Person Household Surveys Mail Surveys of Specifically Named Persons Mail Surveys of Unnamed Persons Internet Surveys of Specifically Named Persons 2 0 1 6 T H E A M E R I C A N A S S O C I A T I O N F O R P U B L I C O P I N I O N R E S E A R C H.
Social Determinants of Health—Healthy People 2030 | health.gov. [cited 2021 Aug 23]. https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
Blake KD, Ottenbacher AJ, Finney Rutten LJ, Grady MA, Kobrin SC, Jacobson RM, et al. Predictors of Human Papillomavirus Awareness and Knowledge in 2013: gaps and opportunities for targeted communication strategies. Am J Prev Med. 2015;48(4):402–10.
Watson M, Benard V, King J, Crawford A, Saraiya M. National assessment of HPV and Pap tests: changes in cervical cancer screening, National Health Interview Survey. Prev Med (Baltim). 2017;100:243–7.
Johnson NL, Head KJ, Scott SF, Zimet GD. Persistent disparities in cervical cancer screening uptake: knowledge and sociodemographic determinants of Papanicolaou and Human papillomavirus testing among women in the United States. Public Health Rep. 2020;135(4):483–91.
Bazargan M, Bazargan SH, Farooq M, Baker RS. Correlates of cervical cancer screening among underserved Hispanic and African-American women. Prev Med (Baltim). 2004;39(3):465–73.
Rubin RF, Kuttab HM, Rihani RS, Reutzel TJ. Patient adherence to three dose completion of the quadrivalent Human papillomavirus (HPV) vaccine in a private practice. J Community Health. 2012;37(6):1145–50. https://doi.org/10.1007/s10900-012-9581-9.
Price RA, Tiro JA, Saraiya M, Meissner H, Breen N. Use of human papillomavirus vaccines among young adult women in the United States: an analysis of the 2008 National Health Interview Survey. Wiley Online Libr. 2011;117(24):5560–8. https://doi.org/10.1002/cncr.26244.
Hirth JM, Tan A, Wilkinson GS, Berenson AB. Completion of the Human papillomavirus (HPV) vaccine series among insured females, 2006–2009. Cancer. 2012;118(22):5623.
Increase the proportion of females who get screened for cervical cancer—C‑09—Healthy People 2030 | health.gov [Internet]. [cited 2021 Sep 15]. https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-females-who-get-screened-cervical-cancer-c-09.
Crawford A, Benard V, King J, Thomas CC. Understanding barriers to cervical cancer screening in women with access to care, behavioral risk factor surveillance system, 2014. Prev Chronic Dis. 2016;13(11):1–8.
Heintzman J, Hatch B, Coronado G, Ezekiel D, Cowburn S, Escamilla-Sanchez O, et al. Role of race/ethnicity, language, and insurance in use of cervical cancer prevention services among low-income Hispanic women, 2009–2013. Prev Chronic Dis. 2018;15(2):E25.
Lee HY, Luo Y, Daniel C, Wang K, Ikenberg C. Is HPV vaccine awareness associated with HPV knowledge level? Findings from HINTS data across racial/ethnic groups in the US. 2020. https://doi.org/10.1080/13557858.2020.1850648.
Otero-Sabogal R, Stewart S, Sabogal F, Brown BA, Pérez-Stable EJ. Access and attitudinal factors related to breast and cervical cancer rescreening: why are Latinas still underscreened? Health Educ Behav. 2003;30(3):337–59.
Ford JL. Racial and ethnic disparities in human papillomavirus awareness and vaccination among young adult women. Public Health Nurs. 2011;28(6):485–93.
Gregg J, Centurion T, Aguillon R, Maldonado J, Celaya-Alston R. Beliefs about the pap smear among Mexican immigrants. J Immigr Minor Health. 2011;13(5):899–905.
Shah M, Zhu K, Wu H, Potter J. Hispanic acculturation and utilization of cervical cancer screening in the US. Prev Med (Baltim). 2006;42(2):146–9.
Scarinci IC, Beech BM, Kovach KW, Bailey TL. An examination of sociocultural factors associated with cervical cancer screening among low-income Latina immigrants of reproductive age. J Immigr Health. 2003;5(3):119–28.
Flores K, Bencomo C. Preventing cervical cancer in the Latina population. J Womens Health (Larchmt). 2009;18(12):1935–43.
Rha SY, Park Y, Song SK, Lee CE, Lee J. Caregiving burden and health-promoting behaviors among the family caregivers of cancer patients. Eur J Oncol Nurs. 2015;19(2):174–81.
Suk R, Hong YR, Rajan SS, Xie Z, Zhu Y, Spencer JC. Assessment of US preventive services task force guideline-concordant cervical cancer screening rates and reasons for underscreening by age, race and ethnicity, sexual orientation, rurality, and insurance, 2005 to 2019. JAMA Netw Open. 2022;5(1):e2143582–e2143582.
Thompson EL, Wheldon CW, Vamos CA, Griner SB, Daley EM. How is health literacy related to pap testing among US women? J Cancer Educ. 2019;34(4):789–95.
Ackerson K, Gretebeck K. Factors influencing cancer screening practices of underserved women. J Am Acad Nurse Pract. 2007;19(11):591–601.
Qin J, Shahangian S, Saraiya M, Holt H, Gagnon M, Sawaya GF. Trends in the use of cervical cancer screening tests in a large medical claims database, United States, 2013–2019. Gynecol Oncol. 2021;163(2):378–84.
Coughlin SS, Thompson TD, Hall HI, Logan P, Uhler RJ. Breast and cervical carcinoma screening practices among women in rural and nonrural areas of the United States, 1998–1999. Cancer. 2002;94(11):2801–12. https://doi.org/10.1002/cncr.10577.
Acknowledgements
Not applicable.
Funding
Melanie Dove was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant No. UL1 TR001860 and linked award KL2 TR001859. However, those fundings had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
JK conceived the study. JK designed the study protocol and conducted literature search under the supervision of JHTD. JK and MD analyzed and interpreted the data. JK wrote the manuscript and JHTD and MD substantially contributed to the manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and participant consent was not necessary as this study involved the use of a previously-published de-identified database. The data used in the study were publicly available.
All the methods performed in the study followed the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
We declare no competing interests regarding the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, J., Dove, M.S. & Dang, J.H.T. Sociodemographic factors associated with HPV awareness/knowledge and cervical cancer screening behaviors among caregivers in the U.S. BMC Women's Health 22, 335 (2022). https://doi.org/10.1186/s12905-022-01918-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01918-4