Abstract
Background
The objective of this study, the first of its kind in Kosovo, is to determine the level of Kosovo women’s knowledge and awareness of HPV infection, HPV vaccination, and its relation to cervical cancer.
Methods
This cross-sectional study was conducted from July to October 2018 at the Clinic of Obstetrics and Gynecology at the Hospital and University Clinical Service of Kosovo.
Results
Out of 800 questionnaires distributed, 645 were completed and returned (80.6%). Only 0.5% of women were vaccinated against HPV. The majority of respondents (66.4%) had no previous knowledge of HPV (human papillomavirus). Only 27.6% of respondents were aware that HPV is responsible for cervical cancer. About two-thirds (70.1%) of respondents had never heard of the HPV vaccine, and only 24% knew that the HPV vaccine can prevent cervical cancer.
Conclusion
The level of vaccination against HPV and the level of knowledge and awareness of HPV infection is extremely low. Higher education, younger age, and living in an urban area were favorable factors and correlated with awareness of HPV infection, vaccination against it, and its relation to cervical cancer. Based on this study, there is an immediate need for developing an educational program on HPV infection and the importance of HPV vaccination as a preventative measure against developing cervical cancer.
Similar content being viewed by others

Background
Genital human papillomavirus (HPV) is one of the most frequent sexually transmitted infections. Although more than 200 genotypes of HPV have been identified, a group of 15 high-risk types are known as an essential factor for development of cervical cancer[1, 2] and also vulvar, vaginal, penile, and oropharyngeal cancers [3, 4].
The worldwide prevalence of HPV infection varies from 2 to 44% [5]. Several meta-analyses indicate that the most prevalent HPV types are HPV16, HPV 18, HPV 31, HPV 52, and HPV 58 [6, 7] and HPV 16 and 18 are considered an etiologically determinant agent in over 71% of cervical cancer cases [6,7,8]. The prevalence of specific HPV types varies geographically, taking into consideration other cofactors, mainly socio-epidemiological ones. Recently, results were also obtained for Kosovo, where the overall HPV prevalence is 13.1%, with HPV 16 as the most prevalent type [9].
In order to prevent HPV infection and thus reduce the risk of precancerous lesions and HPV-related malignancies, three types of vaccines are in use worldwide. The bivalent vaccine (Cervarix) targets HPV 16 and HPV 18. Quadrivalent Gerdasil covers HPV 16, HPV 18, HPV 6, and HPV 11, and the last vaccine to be licensed in US and Europe, mainly in high-income countries, is nonavalent Gerdasil 9, which offers protection against HPV 16, 18, 31, 33, 45, 52, 58, 6, and 11.
By 2017, 71 countries (37%) had introduced the HPV vaccine into their national immunization program for girls, and 11 countries (6%) had also done so for boys [10]. The WHO recommends vaccination of adolescents 9 to 13 years old prior to becoming sexually active and their potential exposure to HPV [11].
A study by Klug et al. showed that awareness of HPV across all populations is poor [12]. Many health-promotion programs have sought to raise awareness of HPV vaccination, but evidence for such awareness is lacking [13]. Neighboring North Macedonia introduced primary vaccination against HPV in 2009, with a 40.1% vaccination rate reported in 2013 [14].
As a small low-income country, Kosovo has not yet established any organized screening program for cervical cancer or vaccination against HPV. The prevalence of HPV among Kosovo women is approximately at the same level as in other countries in the region, and so the risk for acquiring HPV-related malignancies is very high. Therefore it is necessary to introduce application of the HPV vaccine as well as the development of related health-promotion programs.
Methods and material
This cross-sectional study was conducted from July to October 2018 at the Clinic of Obstetrics and Gynecology at the Hospital and University Clinical Service of Kosovo. The methodology was based on questionnaires containing relevant indicators for each attribute. On average, the clinic serves about 200 hospitalized patients and provides outpatient treatment or advice to approximately 50 patients on a daily basis. This is the only tertiary clinic in Kosovo, and it provides medical services to women from across the country.
During the study, 800 structured questionnaires were distributed to women that were hospitalized or had consultations at the outpatient unit between July and October 2018. The pretested questionnaire had three parts. The first part elicited socio-epidemiological data including the age, place of living (urban or rural) level of education as well as sexual activity of the women. The second part tested women’s knowledge of HPV infection, the HPV vaccine, and its relation to cervical cancer. The third part of the questionnaire gathered information regarding women’s knowledge and the rate of cervical cancer screening (the Pap test), also in the end specifying the source of information regarding all the issues of interest in our study.
The questions were simple to answer, with only one correct response. The questionnaires were completed by respondents and then gathered at the collection point in nurses’ offices in the departments at the clinic. Out of 800 questionnaires, 645 were completed properly and returned. The remainder were not filled out correctly or were not returned for final analysis. The overall response rate was 80.6%.
For more details regarding the questions find the questionnaire attached to the manuscript.
Statistical analyses
Method description
Categorical variables were described by frequencies and percentages, and continuous variables by means and standard deviations. Multivariable logistic regression was used to study the association between demographic, social, and informative factors and awareness about the cause and prevention of cervical cancer, as well as the association between demographic, social, and informative factors and understanding the cause and prevention of cervical cancer. P values < 0.05 were considered statistically significant. Statistical analysis was performed using SPSS, v. 26.
Results
Out of 800 questionnaires distributed, 645 were completed correctly (80.6%). Out of this number, 295 respondents (45.7%) belong to the age group 18–25, followed by 187 (29%) in the age group 26–33. Only four (0.6%) respondents were older than 58. Regarding their place of residence, 345 (53.5%) of women lived in urban areas, and 300 (46.5%) lived in rural areas. According to level of education, the respondents were divided into four different groups: 268 (41.6%) had completed secondary school, 212 (32.9%) had a bachelor’s degree, 126 (19.5%) had finished elementary school (or less), and only 39 (6.0%) had a master’s degree or higher level of education (Table 1).
As seen from Table 2, out of 645 respondents only 0.5% (3) of the women were vaccinated against HPV, whereas 99.5% (642) were not vaccinated.
The majority of respondents, 66.4% (or 428 of them) stated that they had no previous knowledge of HPV. One-third of them (215) knew of HPV, and two women (0.3%) did not answer this question. When asked if HPV is a responsible factor for cervical cancer, only 27.6% (or 178) confirmed that they knew this; 7.6% responded “no,” and most of them (64.7% or 417) had no knowledge of this issue. Of the 645 women involved in our study, only 29.6% (or 191) had previously heard of the HPV vaccine, 70.1% had no prior information about the HPV vaccine, and only 0.3% did not answer the question (Table 3).
The association between several demographic, social, and informational factors and awareness of HPV or knowledge that HPV is related to cervical cancer was studied using multivariable logistic regression, and the results are summarized in Table 4. When controlling for other factors in the regression model, respondents with sexual experience are less likely to have heard about HPV (OR [95% CI] 0.57 [0.32; 0.99]). Women with a university education had more often heard about HPV than women with a elementary education or less (OR [95% CI] 8.33 [3.94; 17.63]), and women that were informed about HPV by nurses (OR [95% CI] 2.75 [1.25; 6.05]), by teachers (OR [95% CI] 2.46 [1.39; 4.34]), or via the internet (OR [95% CI] 1.86 [1.17; 2.94]). Women with a university education were more frequently informed about the relationship between HPV and cervical cancer (OR [95% CI] 6.89 [3.13; 15.18]) compared to those that were informed about the topic by nurses (OR [95% CI] 2.78 [1.28; 6.00]) or/and via the internet (OR [95% CI] 1.9 [1.20; 3.01]). Women that were informed about HPV by friends knew about this relationship less often (OR [95% CI] 0.39 [0.16; 0.97]).
The existence of a vaccination against HPV is better known to women with a university education compared to women with an elementary education or less (OR [95% CI] 3.27 [1.65; 6.45]) and compared to those that were informed about vaccination by doctors (OR [95% CI] 1.72 [1.02; 2.88]) or via the internet (OR [95% CI] 2.23 [1.46; 3.42]) (Table 5). That vaccination prevents cervical cancer is better known to women with a university education (OR [95% CI] 3.68 [1.67; 8.13]) and those that were educated about the topic by nurses (OR [95% CI] 3.19 [1.42; 7.17]) or via the internet (OR [95% CI] 2.37 [1.49; 3.78]). Women that received information from friends are less aware of this fact (OR [95% CI] 0.33 [0.12; 0.92]).
Discussion
To the best of our knowledge, this is the first study of this kind conducted in Kosovo. The overall rate of women ever vaccinated against HPV is extremely low: 0.5%, or only three women out of 645 included in the study. To date, Kosovo has no national programs for HPV vaccination and it has not promoted HPV vaccination. The prevalence of high-risk HPV genotypes among Kosovo women [9] is similar to that in other countries in the region, and the lack of a national screening program for cervical cancer in Kosovo corresponds to the great risk women have of acquiring cervical cancer.
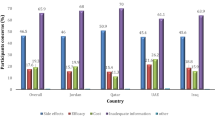
Our results show that women’s knowledge about HPV infection is poor because only 33.3% of women have any information about HPV, and the majority state that they have never heard of HPV. Some similar studies have been conducted worldwide, mainly assessing the knowledge of young adolescents and students, and they yielded different results. Much higher results were obtained in studies in many developed countries [13, 15,16,17]. In a study of 204 women 16–23 years old attending a public outpatient gynecology clinic in Brazil, Moreira et al. found that 66.7% of women were informed about HPV [18]. However, a study in China showed even lower results, at 19.3% [19].
Most of the women included in the study (72.3%) do not know or think it is not true that HPV is a factor responsible for the development of cervical cancer. Other studies have showed similar results, such as a study in Nigeria [20], whereas a survey in Australia revealed that 66% of men and women know about HPV and cervical cancer [21].
Two-thirds of Kosovo women stated that they had never heard about the HPV vaccine, and only 29.6% of them have some information about the HPV vaccine. The percentage of women that know that the HPV vaccine can prevent the development of cervical cancer is even lower (24%). These results are far lower than the rates reported in studies conducted in other countries [17, 18, 21, 22]. The results of this study also confirm previous findings by other authors that a higher education level and younger age have an impact on the level of knowledge and awareness of HPV infection, vaccination, and its relation to cervical cancer [22, 23].
Women with higher education and younger in age, have more access to the proper information, as a result of easier access to updated information from the media, internet or literature, increased awareness and regular consultations with doctors, therefore they are more keen to understand the importance of HPV infection and its relationship to cervical cancer, as well as HPV vaccination as the most important measure to prevent cervical cancer.
This study has some limitations. As a cross-sectional study, it may exclude causal relationships between various factors and results. Also, because the information was collected through questionnaires, there is a possibility of incorrect answers, which could lead to possible bias. Despite these possible limitations, the study had quite a high rate of response. Information was gathered from a large number of participants, making it a very representative sample.
Conclusion
Based on our results, the level of knowledge and awareness of HPV infection, the HPV vaccine, and its causal association with cervical cancer is generally very low among Kosovo women. Also, it can be concluded that the level of vaccination against HPV in Kosovo is extremely low. The results also indicate that having a higher level of education, living in urban areas, and being younger are favorable factors for having more information about HPV infection and the HPV vaccine.
Based on our study data, there is an immediate need for the development of a proper educational program about HPV infection and the importance of HPV vaccination as a preventative measure against the development of cervical cancer.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–9.
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370(9590):890–907.
Zur Hausen H. Papillomaviruses in the causation of human cancers - a brief historical account. Virology. 2009;384(2):260–5.
Gillison ML. Human papillomavirus-associated head and neck cancer is a distinct epidemiologic, clinical, and molecular entity. Semin Oncol. 2004;31(6):744–54.
Bosch FX, de Sanjosé S. Chapter 1: Human papillomavirus and cervical cancer--burden and assessment of causality. J Natl Cancer Inst Monogr. 2003;31:3–13.
Bruni L, Diaz M, Castellsagué X, et al. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202(12):1789–99.
Guan P, Howell-Jones R, Li N, et al. Human apillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer. 2012;131(10):2349–59.
Li N, Franceschi S, Howell-Jones R, Snijders PJ, Clifford GM. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: Variation by geographical region, histological type and year of publication. Int J Cancer. 2011;128(4):927–35.
Zejnullahu Raçi P, Hošnjak L, Poljak M, Lepej SŽ, Vince A. Pre-vaccination prevalence of high-risk human papillomaviruses (HPV) in women from Kosovo and their related sociodemographic characteristics. Ginekol Pol. 2018;89(9):485–94.
WHO/ Immunization,Vaccines and Biologicals database, as of 31 March 2017. Available at http://www.who.int/entity/immunization/monitoring_surveillance/VaccineIntroStatus.pptx, accessed February 2017
Human papillomavirus vaccines: WHO position paper, May 2017, No 19, 2017, 92, 241–268 http://www.who.int/wer
Klug SJ, Hukelmann M, Blettner M. Knowledge about infection with human papillomavirus: a systematic review. Prev Med. 2008;46:87–98.
Hendry M, Lewis R, Clements A, Damery S, Wilkinson C. “HPV? Never heard of it!”: a systematic review of girls’ and parents’ information needs, views and preferences about human papillomavirus vaccination. Vaccine. 2013;31:5152–67.
Vaccination in Republic of Macedonia: Standards and Actual Trends. 2013. Available at http://www.medical-chambers.org/documents/Prof.DrKocoCakalaroski_Vaccination_Macedonia.pdf
Waller J, Marlow LA, Wardle J. The association between knowledge of HPV and feelings of stigma, shame and anxiety. Sex Transm Infect. 2007;83(2):155–9.
Dodd RH, McCaffery KJ, Marlow LA, Ostini R, Zimet GD, Waller J. Knowledge of human papillomavirus (HPV) testing in the USA, the UK and Australia: an international survey. Sex Transm Infect. 2014;90(3):201–7.
Bowyer HL, Marlow LA, Hibbitts S, Pollock KG, Waller J. Knowledge and awareness of HPV and the HPV vaccine among young women in the first routinely vaccinated cohort in England. Vaccine. 2013;31(7):1051–6.
Moreira ED Jr, de Oliveira BG, Neves RC, et al. Assessment of knowledge and attitudes of young uninsured women toward human papillomavirus vaccination and clinical trials. J Pediatr Adolesc Gynecol. 2006;19(2):81–7.
Yu Y, Xu M, Sun J, et al. Human papillomavirus infection and vaccination: awareness and knowledge of HPV and acceptability of HPV vaccine among mothers of teenage daughters in Weihai, Shandong China. PLoS ONE. 2016;11(1):e0146741.
Makwe CC, Anorlu RI, Odeyemi KA. Human papillomavirus (HPV) infection and vaccines: knowledge, attitude and perception among female students at the University of Lagos, Lagos. Nigeria J Epidemiol Glob Health. 2012;2(4):199–206.
Pitts MK, Heywood W, Ryall R, et al. Knowledge of human papillomavirus (HPV) and the HPV vaccine in a national sample of Australian men and women. Sex Health. 2010;7(3):299–303.
Marlow LA, Zimet GD, McCaffery KJ, Ostini R, Waller J. Knowledge of human papillomavirus (HPV) and HPV vaccination: an international comparison. Vaccine. 2013;31(5):763–9.
Tiro JA, Meissner HI, Kobrin S, Chollette V. What do women in the U.S. Know about HumanPapillomavirus and Cervical Cancer? Cancer Epidemiol Biomark Prev. 2007;16(2):288.
Acknowledgements
The authors would like to thank the staff of Department of Gynaecology and Obstetrics in the Hospital and University Clinical Service of Kosovo for their technical assistance.
Author information
Authors and Affiliations
Contributions
Author PZR, FR and TH have given substantial contribution to design and conception of the manuscript, authors PZR and FR participated in acquisition, analysis and interpretation of the data. All authors have participated on drafting and revising the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in compliance with the Declaration of Helsinki and was approved by the Ethics and Professional Board of the Hospital and University Clinical Service of Kosovo (HUCSK), number 905 (dt. 06.08.2018). As in this study, no personal data of the subjects have been taken (anonymous questionnaire used), the Ethics and Professional Board of the Hospital and University Clinical Service of Kosovo (HUCSK) has waived the requirement of formal informed consent from the participants.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Questionnaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Raçi, P.Z., Raçi, F. & Hadri, T. Kosovo women’s knowledge and awareness of human papillomavirus (HPV) infection, HPV vaccination, and its relation to cervical cancer. BMC Women's Health 21, 354 (2021). https://doi.org/10.1186/s12905-021-01496-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-021-01496-x