Abstract
Background
Relugolix is a once-daily, oral, nonpeptide, gonadotropin-releasing hormone receptor antagonist. The aim of this study was to evaluate safety of relugolix over 24 weeks in women with endometriosis-associated pain.
Methods
This phase 2, randomized, open-label, parallel-group extension study was conducted in 101 clinics in Japan. Patients (premenopausal females ≥ 20 years) who completed the preceding 12-week relugolix phase 2 study continued to receive relugolix (10 mg, 20 mg, or 40 mg), placebo, or leuprorelin (3.75 mg) for an additional 12 weeks. Relugolix was administered orally once daily, and leuprorelin subcutaneously once every 4 weeks. The primary outcome was safety, including bone mineral density (BMD) and treatment-emergent adverse events (TEAEs). Secondary endpoints included visual analog scale (VAS) scores for endometriosis-associated pain. Analysis sets were defined as all patients who were administered the study drug.
Results
Of 487 randomized patients in the preceding study, 397 enrolled in this extension study and continued to receive placebo (n = 77), relugolix 10 mg (n = 84), relugolix 20 mg (n = 78), relugolix 40 mg (n = 89), or leuprorelin (n = 69). Baseline characteristics were similar between extension study patients and patients in the preceding study. Frequency of TEAEs including metrorrhagia, menorrhagia, and hot flush was similar in the relugolix 40-mg and leuprorelin groups. Mean (SD) change in BMD from baseline at Week 24 was − 0.2 (1.99)% for placebo; − 1.6 (2.34)%, − 2.6 (2.94)%, and − 4.9 (2.91)% for the relugolix 10-mg, 20-mg, and 40-mg groups, respectively; and − 4.4 (2.16)% for leuprorelin. Mean ± SD change from baseline in mean VAS score (mm) for pelvic pain at end of treatment was − 3.2 ± 12.16 for placebo; − 6.8 ± 10.56, − 9.0 ± 11.84, and − 11.9 ± 11.26 for the relugolix 10-mg, 20-mg, and 40-mg groups, respectively; and − 12.7 ± 12.57 for leuprorelin. Estradiol levels decreased with increasing relugolix dose and remained below postmenopausal levels throughout the 24-week relugolix 40-mg treatment period.
Conclusions
Treatment with relugolix for 24 weeks was generally well tolerated and demonstrated similar pain reduction to leuprorelin in women with endometriosis. The dose-dependent loss in BMD observed with relugolix treatment was expected due to an induced hypoestrogenic state. Relugolix demonstrated a similar benefit/risk profile to injectable therapy in this phase 2 study.
Trial registration NCT01452685 (ClinicalTrials.gov, registered 17/10/2011).
Similar content being viewed by others
Background
Women with endometriosis experience various clinical symptoms including pelvic pain, dysmenorrhea, dyspareunia, and infertility [1, 2]. Such symptoms substantially affect quality of life (QOL) in patients with endometriosis. The European Society of Human Reproduction and Embryology guideline recommends prescription of hormonal contraceptives, progestins, or gonadotropin-releasing hormone (GnRH) agonists as options for reducing endometriosis-associated pain [3]. However, oral contraceptive pills are associated with increased risk of thrombosis and hepatic dysfunction [4, 5], and there is limited evidence of their efficacy for endometriosis-associated pain [3, 6]. Progestins may induce abnormal bleeding [7, 8], and implant and depot injectable forms are associated with weight gain, nausea, and breast tenderness [8] and a decrease in bone mineral content [9]. Although GnRH agonists such as leuprorelin are highly effective in relieving endometriosis-associated symptoms, they decrease bone mineral content (due to an estrogen-lowering effect), which limits their use to less than 6 months without an add-back therapy [4]. In addition, GnRH agonists induce a transient increase in the secretion of gonadotropins (flare), which results in a temporary worsening of symptoms, and they cannot be orally administered [4].
An alternative therapeutic approach is the use of GnRH receptor antagonists, which do not induce an initial clinical flare and typically have fewer side effects than GnRH agonists [4]. Relugolix is an oral, nonpeptide GnRH receptor antagonist that reduces blood concentrations of hormones including estradiol (E2) and progesterone (P) via suppression of the hypothalamic–pituitary–gonadal (HPG) axis [10, 11], and induces endometrial atrophy. Therefore, relugolix is expected to improve the clinical symptoms of endometriosis, cause no flare, and have a faster onset of action than GnRH agonists. In Japanese premenopausal women with endometriosis, a phase 2 study (NCT01458301) evaluated ascending doses (10, 20, and 40 mg) of relugolix compared with placebo and demonstrated that doses up to 40 mg were well tolerated and effective in treating endometriosis-associated pain [12].
The present extension study (NCT01452685, registered 17/10/2011) evaluated the safety and efficacy of 12 additional weeks of therapy with relugolix (24 weeks in total) in patients who participated in the preceding phase 2 study.
Methods
Study design
This phase 2, multicenter, long-term extension study was conducted between March 2012 and February 2014 at 101 study sites in Japan. The study was designed as open-label, but study drug randomization information was only broken after testing and observation at Week 24 for the last patient in this study. The study was conducted in accordance with the principles of the Declaration of Helsinki, the International Council for Harmonisation Guideline for Good Clinical Practice, and all applicable laws and regulations. The protocol was reviewed and approved by the Institutional Review Boards at all participating study sites. All patients provided written informed consent before enrollment in this extension study.
The preceding study consisted of a pretreatment period of 4–12 weeks and a treatment period of 12 weeks; patients were randomized as previously described [12]. The present extension study consisted of an additional treatment period of 12 weeks and a follow-up period of 4 weeks (total period of study participation was 16 weeks). Overall treatment duration was 24 weeks, including the preceding study. Patients continued to receive the same treatment they were assigned at randomization in the preceding randomized controlled double-blind study (i.e., relugolix 10 mg, 20 mg, or 40 mg; placebo; or leuprorelin). To maintain blinding during the double-blind and extension phases, test results were concealed by the laboratory that conducted the drug concentration and pharmacodynamic analyses until the randomization schedule was broken.
Relugolix and its placebo were administered orally once daily 30 min before breakfast, and leuprorelin (3.75 mg) and its placebo were injected subcutaneously once every 4 weeks. Sex hormone preparations were prohibited during the study. A prescription analgesic (loxoprofen) was permitted when the investigator decided that an analgesic was required to alleviate severe endometriosis-associated pain. Analgesic use was recorded daily by the patients in their diaries.
Patients continuously recorded symptoms from the time of informed consent until after final study drug administration. Patients visited the investigational site every 4 weeks to undergo designated examinations and evaluations. During the follow-up period, if the first posttreatment menstruation was not observed by the final visit, the patient underwent further follow-up by telephone interview until the first posttreatment menstruation was observed.
Patients
Eligible patients were premenopausal Japanese females who had completed treatment with the study drug in the preceding phase 2 study. Patients were excluded from the extension study if they met any of the following criteria: those who had treatment-emergent adverse events (TEAEs) in the preceding phase 2 study that made study drug continuation not in the best interest of the patient; those unable to comply with the study protocol requirements due to the development of a new disease or symptom, or aggravation of clinical laboratory findings; those for whom treatment showed no efficacy during the preceding phase 2 study; and those who had problems with continuing the study because of the occurrence of symptoms of hypoestrogenism.
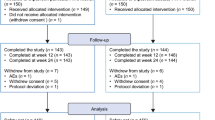
In the preceding phase 2 study, 487 patients were randomized to treatment groups and 484 patients were administered the study drug. Of these patients, 402 (83.1%) signed the informed consent form to participate in this extension study. Of the 402 patients, five did not participate in the extension study for the following reasons: pretreatment event/adverse event in four patients and voluntary withdrawal in one patient (Fig. 1). Therefore, 397 patients were enrolled in the extension study and administered the study drug: 77 patients in the placebo group, 84 in the relugolix 10-mg group, 78 in the relugolix 20-mg group, 89 in the relugolix 40-mg group, and 69 in the leuprorelin group. The FAS/SAS for the 24 weeks of study drug administration included 483 patients (Fig. 1) because three patients were not administered the study drug and one patient had a major violation of Good Clinical Practice (loss of source documents).
Study variables
The primary endpoints in this study were assessments of safety, including bone mineral density (BMD) assessed by dual energy X-ray absorptiometry, TEAEs, vital signs, weight, 12-lead electrocardiogram (ECG), and clinical laboratory tests. Secondary endpoints included visual analog scale (VAS) scores for pelvic pain, dysmenorrhea, and dyspareunia during the treatment period. Additional endpoints included endometriosis-associated pain symptoms assessed by modified Biberoglu and Behrman (M-B&B) and B&B scales during the treatment period [13]; use of analgesics during the treatment period; decrease in menstrual blood loss (based on self-reported amount of bleeding scores); achievement of amenorrheic state; QOL assessed by Endometriosis Health Profile-30 (EHP-30) [14, 15]; and blood concentration of E2, P, luteinizing hormone (LH), and follicle-stimulating hormone (FSH).
Statistical analyses
Data from the preceding phase 2 study were combined with data from the present extension study to analyze safety, efficacy, and pharmacodynamics across 24 weeks of relugolix administration. For this reason and consistent with the preceding study, the number of evaluable patients was set at 450.
In the present extension study, the full analysis set (FAS) and safety analysis set (SAS) were the same, defined as all patients who received at least one dose of the study drug in the preceding phase 2 study. TEAEs were coded using the Medical Dictionary for Regulatory Activities Version 16.1. For continuous variables (including BMD, vital signs, weight, clinical laboratory tests, and ECG), baseline values, observed values, and changes from baseline were summarized for each measurement time point. For the secondary efficacy endpoints, summary statistics and 95% confidence intervals were calculated for each treatment group.
Results
The mean VAS score (mm) for pelvic pain, dysmenorrhea, and dyspareunia at baseline for patients who entered the extension study ranged from 14.6 to 16.0, 26.6 to 31.57, and 8.1 to 12.6, respectively. Overall, there were no apparent differences in demographic and baseline characteristics among the treatment groups (Additional file 1). There were no clinically important differences in demographic and baseline characteristics between patients randomized in the preceding phase 2 study [12] and the subgroup who entered the extension study.
Safety assessment
The incidences of TEAEs over 24 weeks were 81.4% in the placebo group, 86.4% in the relugolix 10-mg group, 96.0% in the relugolix 20-mg group, 95.1% in the relugolix 40-mg group, and 97.5% in the leuprorelin group (Table 1). The incidences of TEAEs in the relugolix 20-mg and 40-mg groups were higher compared with the placebo group, and similar to that in the leuprorelin group. TEAEs with an incidence of ≥ 10% in any relugolix group were nasopharyngitis, headache, metrorrhagia, menstruation irregular, menorrhagia, oligomenorrhea, hyperhidrosis, and hot flush (Table 1). All TEAEs were mild or moderate in intensity except for two severe events (blood creatine phosphokinase increased and ovarian cyst ruptured) in the placebo group.
There were no deaths, and seven serious TEAEs were reported throughout the preceding and extension studies, including Langerhans’ cell histiocytosis, narcolepsy, ovarian cyst ruptured (two patients), and hemorrhagic ovarian cyst in the placebo group, and pseudocyst and liver function test abnormal in the relugolix 20-mg group. Of these, three serious TEAEs (hemorrhagic ovarian cyst and ovarian cyst ruptured in the placebo group, and pseudocyst in the relugolix 20-mg group) were observed during the extension study. An abnormal liver function test was reported in one patient in the relugolix 20-mg group in the preceding study; this was considered related to the study drug and resolved after study drug discontinuation. The incidences of TEAEs leading to discontinuation of the study drug were 6.2% in the placebo group, 1.0% in the relugolix 10-mg group, 7.0% in the relugolix 20-mg group, 1.9% in the relugolix 40-mg group, and 11.3% in the leuprorelin group. No clinically significant changes were found in clinical laboratory test results, vital signs, or ECG findings in the extension study.
The mean percent changes in BMD from baseline at the lumbar spine (L1–L5) at Week 12 and 24 (SD) were − 0.1 (1.73)% and − 0.2 (1.99)%, respectively, for placebo, − 1.0 (1.88)% and − 1.6 (2.34)% for relugolix 10 mg, − 1.3 (2.09)% and − 2.6 (2.94)% for relugolix 20 mg, − 2.1 (2.22)% and − 4.9 (2.91)% for relugolix 40 mg, and − 2.2 (1.67)% and − 4.4 (2.16)% for leuprorelin. The decrease in BMD was time- and dose-dependent in the relugolix groups. The percent change from baseline in BMD in the relugolix 40-mg group was similar to that in the leuprorelin group. As for TEAEs related to BMD, 14 patients with BMD decreases at Week 24 [placebo (n = 1), relugolix 10 mg (n = 1), relugolix 20 mg (n = 2), relugolix 40 mg (n = 6), and leuprorelin (n = 4)] and two patients at Week 12 [relugolix 20 mg (n = 1) and 40 mg (n = 1)] were reported. All these TEAEs were considered related to the study drug and, except for one moderate event in the leuprorelin group, all the TEAEs related to BMD were considered mild in intensity by the investigator.
In the follow-up period, the return of menstrual cycles was not confirmed in 24 out of 483 patients for the following reasons: start of treatment with hormone preparations prior to the return of menstrual cycle (n = 19); surgical operation (n = 2); pregnancy (n = 1); lost to follow-up (n = 1); and the decision by the investigator that follow-up was not necessary (n = 1). The mean duration from the last dose of study drug to the return of menstrual cycles (SD) was 17.3 (8.49) days for placebo, 21.0 (12.32) days for relugolix 10 mg, 26.0 (12.97) days for relugolix 20 mg, 36.9 (9.49) days for relugolix 40 mg, and 73.3 (21.11) days for leuprorelin.
Efficacy assessments
The VAS scores for pelvic pain and dysmenorrhea in the relugolix and leuprorelin groups decreased in a time- and dose-dependent manner throughout the treatment period (Fig. 2a, b). No clear trend was observed in mean VAS score from baseline for dyspareunia among the treatment groups (Fig. 2c). The mean changes from baseline to end of the treatment period in mean VAS score (mm) for pelvic pain, dysmenorrhea, and dyspareunia (SD) were − 3.2 (12.16), − 5.8 (17.13), and − 1.1 (12.66), respectively, for placebo; − 6.8 (10.56), − 15.4 (18.05), and − 3.5 (10.85), respectively, for relugolix 10 mg; − 9.0 (11.84), − 19.8 (20.43), and − 3.6 (11.55), respectively, for relugolix 20 mg; − 11.9 (11.26), − 29.5 (17.54), and − 0.9 (12.04), respectively, for relugolix 40 mg; and − 12.7 (12.57), − 27.2 (19.86), and − 4.6 (15.09), respectively, for leuprorelin. The changes in mean VAS score from baseline for pelvic pain and dysmenorrhea in the relugolix 40-mg group were similar to those in the leuprorelin group. Overall, similar results were obtained in mean M-B&B (Additional file 2) and B&B (Additional file 3) scores for pelvic pain, dysmenorrhea, and dyspareunia.
VAS score (mm) by visit. a Pelvic pain (end-of-treatment group sizes: placebo n = 97, relugolix 10 mg n = 103, relugolix 20 mg n = 100, relugolix 40 mg n = 103, leuprorelin n = 80). b Dysmenorrhea (end-of-treatment group sizes: placebo n = 97, relugolix 10 mg n = 103, relugolix 20 mg n = 100, relugolix 40 mg n = 103, leuprorelin n = 80). c Dyspareunia (end-of-treatment group sizes: placebo n = 36, relugolix 10 mg n = 50, relugolix 20 mg n = 40, relugolix 40 mg n = 39, leuprorelin n = 23). Data are mean ± SD. SD standard deviation; VAS visual analog scale
The change from baseline in proportion of days with analgesic use showed a time- and dose-dependent decrease in the relugolix groups compared with placebo (Additional file 4). Dose-dependent improvements in QOL at Weeks 12 and 24 were demonstrated by changes in the EHP-30 scores in the “pain” (reflecting on daily activities and functioning) and “control and powerlessness” domains (Additional file 4). Patients receiving relugolix and leuprorelin had greater improvements in these QOL domains than patients receiving placebo.
Relugolix, at higher doses (20 mg and 40 mg), was associated with lower median values of E2, LH, FSH, and P (Additional file 5). In the relugolix 40-mg group, the median serum E2 concentration decreased to < 10 pg/mL (less than the lower limit of quantification [LLQ]) at Week 2 and was maintained at this level until Week 24; in contrast, in the leuprorelin group, the median serum E2 concentration did not decrease to LLQ until Week 4.
Discussion
In this phase 2 extension study in Japanese women with endometriosis, pelvic pain and dysmenorrhea decreased in a time- and dose-dependent manner over 24 consecutive weeks of treatment with relugolix (up to 40 mg). The majority of the TEAEs experienced by patients treated with relugolix were mild, and TEAEs leading to study drug discontinuation were uncommon. These safety and efficacy results over 24 weeks were consistent with the findings from the first 12 weeks of the phase 2 study [12].
There were no unexpected safety issues during the extended administration period of 12 weeks. Of the TEAEs reported, most were reported during the first 12 weeks [12]. The overall incidence of TEAEs was higher in the relugolix 20-mg and 40-mg groups compared with the placebo group, but was similar to the leuprorelin group. The most common TEAEs in the relugolix group included nasopharyngitis, metrorrhagia, irregular menstruation, menorrhagia, oligomenorrhea, hyperhidrosis, headache, and hot flush. These TEAEs were observed at similar frequencies in the leuprorelin group and were consistent with the estrogen-lowering effects of both relugolix and leuprorelin. In addition, relugolix time- and dose-dependently decreased BMD, with the change in BMD in the relugolix 40-mg group being similar to that in the leuprorelin group. Again, this TEAE was considered to be secondary to the hypoestrogenic state induced by relugolix and leuprorelin. These hypoestrogenic side effects may potentially be mitigated through add-back therapy using low-dose hormones, an approach that has been used with GnRH agonists such as leuprorelin [16] and is under investigation in ongoing global phase 3 studies of relugolix (ClinicalTrials.gov: NCT03049735, NCT03103087, NCT03204318, NCT03204331, NCT03654274).
Following cessation of the study drug, the return of menstrual cycles was confirmed in the majority of patients. The number of days until recovery of menstruation in the relugolix 40-mg group was approximately half of that in the leuprorelin group. This was considered to be related to a difference in the timing of HPG axis recovery after removal of an oral GnRH antagonist (relugolix) versus an injectable depot formulation of an agonist (leuprorelin). This is supported by the pharmacodynamic data: after suppression of E2 in the relugolix 40-mg and leuprorelin groups throughout the study period, E2 levels recovered during the follow-up period in the relugolix 40-mg group but remained low in the leuprorelin group.
Overall, in patients with endometriosis, the effects of relugolix on endometriosis-related pain after administration for 12 weeks in the preceding phase 2 study [12] were maintained for an additional 12 weeks. VAS scores for pelvic pain and dysmenorrhea in the relugolix and leuprorelin groups time- and dose-dependently decreased throughout the treatment period and were lower than placebo. VAS scores in the relugolix 40-mg group were similar to those in the leuprorelin group. These efficacy results were supported by the results for other pain evaluation indexes, M-B&B and B&B score, and the time- and dose-dependent reduction in the proportion of patients using analgesics in the relugolix groups. Although direct comparisons of efficacy between studies can be difficult owing to differences in pain rating scales, the efficacy of relugolix for reducing endometriosis-related pain is consistent with the findings for elagolix, another oral GnRH antagonist [17]. Other endometriosis-related symptoms were also time- and dose-dependently improved by treatment with relugolix. The amount of menstrual bleeding decreased, the proportion of patients who achieved amenorrhea increased, and QOL was improved in the “pain” and “control and powerlessness” domains of the EHP-30. These results suggest that relugolix improves more clinical symptoms than just endometriosis-related pain.
The main strength of this study is the extended period of treatment, which enabled further elucidation of the safety and efficacy of relugolix beyond the initial 12-week phase 2 study period. Limitations of this study included a relatively small number of patients entering the extension period and the inclusion of only Japanese patients, both of which may reduce the generalizability of the results. Furthermore, the number of patients who received the assessment for dyspareunia was small in the present study, so the efficacy of relugolix for dyspareunia remains to be confirmed in larger studies.
Conclusions
In conclusion, treatment with relugolix up to 40 mg for 24 weeks improved endometriosis-related pain and was generally well tolerated. Relugolix 40 mg demonstrated similar efficacy to leuprorelin in premenopausal women with endometriosis. Relugolix may be a new oral treatment option for endometriosis-associated pain that has a similar benefit/risk profile to injectable therapy, without the initial hormonal flare and a more rapid return of menses after treatment discontinuation. The 40-mg dose of relugolix is currently under evaluation in phase 3 studies of patients with endometriosis.
Availability of data and materials
The datasets, including the redacted study protocol, redacted statistical analysis plan, and individual participants data supporting the results reported in this article, will be made available within three months from initial request, to researchers who provide a methodologically sound proposal. The data will be provided after its de-identification, in compliance with applicable privacy laws, data protection and requirements for consent and anonymization. For details on submitting a request, see the instructions provided at https://clinicaltrials.takeda.com/.
Abbreviations
- B&B:
-
Biberoglu and Behrman (scale)
- BMD:
-
Bone mineral density
- E2 :
-
Estradiol
- ECG:
-
Electrocardiogram
- EHP-30:
-
Endometriosis Health Profile-30
- FAS:
-
Full analysis set
- FSH:
-
Follicle-stimulating hormone
- GnRH:
-
Gonadotropin-releasing hormone
- HPG:
-
Hypothalamic–pituitary–gonadal
- LH:
-
Luteinizing hormone
- LLQ:
-
Lower limit of quantification
- M-B&B:
-
Modified Biberoglu and Behrman (scale)
- P:
-
Progesterone
- QOL:
-
Quality of life
- SAS:
-
Safety analysis set
- TEAE:
-
Treatment-emergent adverse event
- VAS:
-
Visual analog scale
References
Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364(9447):1789–99.
Mounsey AL, Wilgus A, Slawson DC. Diagnosis and management of endometriosis. Am Fam Physician. 2006;74(4):594–600.
Dunselman GAJ, Vermeulen N, Becker C, Calhaz-Jorge C, D’Hooghe T, De Bie B, et al. ESHRE guideline: management of women with endometriosis †. Hum Reprod. 2014;29(3):400–12. († ESHRE pages content are not externally peer reviewed. This manuscript has been approved by the Executive Committee of ESHRE.)
Rafique S, Decherney AH. Medical management of endometriosis. Clin Obstet Gynecol. 2017;60(3):485–96.
National Institute of Diabetes and Digestive and Kidney Diseases. Estrogens and oral contraceptives. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012 [Updated 28 May 2020]. https://www.ncbi.nlm.nih.gov/books/NBK548539/. Accessed 3 Feb 2021.
Brown J, Crawford TJ, Datta S, Prentice A. Oral contraceptives for pain associated with endometriosis. Cochrane Database Syst Rev. 2018;5(5):CD001019.
Gezer A, Oral E. Progestin therapy in endometriosis. Womens Health (Lond). 2015;11(5):643–52.
Barra F, Scala C, Ferrero S. Current understanding on pharmacokinetics, clinical efficacy and safety of progestins for treating pain associated to endometriosis. Expert Opin Drug Metab Toxicol. 2018;14(4):399–415.
Committee Opinion No. 602: Depot medroxyprogesterone acetate and bone effects. Obstet Gynecol. 2014;123(6):1398–402.
Osuga Y, Enya K, Kudou K, Hoshiai H. Relugolix, a novel oral gonadotropin-releasing hormone antagonist, in the treatment of pain symptoms associated with uterine fibroids: a randomized, placebo-controlled, phase 3 study in Japanese women. Fertil Steril. 2019;112(5):922–9.e2.
Nakata D, Masaki T, Tanaka A, Yoshimatsu M, Akinaga Y, Asada M, et al. Suppression of the hypothalamic–pituitary–gonadal axis by TAK-385 (relugolix), a novel, investigational, orally active, small molecule gonadotropin-releasing hormone (GnRH) antagonist: studies in human GnRH receptor knock-in mice. Eur J Pharmacol. 2014;723:167–74.
Osuga Y, Seki Y, Tanimoto M, Kusumoto T, Kudou K, Terakawa N. Relugolix, an oral gonadotropin-releasing hormone receptor antagonist, reduces endometriosis-associated pain in a dose-response manner: a randomized, double-blind, placebo-controlled study. Fertil Steril. 2020;115(2):397–405.
Biberoglu KO, Behrman SJ. Dosage aspects of danazol therapy in endometriosis: short-term and long-term effectiveness. Am J Obstet Gynecol. 1981;139(6):645–54.
Jones G, Kennedy S, Barnard A, Wong J, Jenkinson C. Development of an endometriosis quality-of-life instrument: the Endometriosis Health Profile-30. Obstet Gynecol. 2001;98(2):258–64.
Jones G, Jenkinson C, Taylor N, Mills A, Kennedy S. Measuring quality of life in women with endometriosis: tests of data quality, score reliability, response rate and scaling assumptions of the Endometriosis Health Profile Questionnaire. Hum Reprod. 2006;21(10):2686–93.
DiVasta AD, Feldman HA, Sadler Gallagher J, Stokes NA, Laufer MR, Hornstein MD, et al. Hormonal add-back therapy for females treated with gonadotropin-releasing hormone agonist for endometriosis: a randomized controlled trial. Obstet Gynecol. 2015;126(3):617–27.
Taylor HS, Giudice LC, Lessey BA, Abrao MS, Kotarski J, Archer DF, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377(1):28–40.
Acknowledgements
The authors would like to thank all study participants and the investigators and other staff members who participated in this study. Medical writing assistance and coordination of the manuscript’s development were provided by WysiWyg Co., Ltd. Additional medical writing assistance was provided by Koa Webster, Ph.D., and Tania Dickson, Ph.D., CMPP, of ProScribe—Envision Pharma Group. ProScribe’s services complied with international guidelines for Good Publication Practice (GPP3). Medical writing and editorial support for this article was funded by Takeda Pharmaceutical Company Limited.
Prior presentation The data in this article were previously presented at the 19th European Congress of Endocrinology, May 20–23, 2017, Lisbon, Portugal.
Funding
This study was sponsored by Takeda Pharmaceutical Company Limited (Osaka, Japan), manufacturer/licensee of relugolix. Takeda Pharmaceutical Company Limited was involved in the study design, protocol development, data collection, review, analysis of the data, and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YO, YS, MT, TK, KK, and NT participated in the study design and interpretation of the study results, and in the drafting, critical revision, and approval of the final version of the manuscript. YO and NT were investigators and KK performed the statistical analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the principles of the Declaration of Helsinki, the International Council for Harmonisation Guideline for Good Clinical Practice, and all applicable laws and regulations. All patients provided written informed consent before enrollment in this extension study. Ethics approval for the study, including the protocol and informed consent form, was obtained from the Institutional Review Board (IRB) for each study site: Chayamachi Ladies Clinic IRB, Osaka Clinical Research Collaborative Network IRB, Jinsenkai Hanna Hospital IRB, Doujin Kinenkai Meiwa Hospital IRB, Shintokai Yokohama Minoru Clinic IRB, International University of Health and Welfare, Kouhoukai Group Kyushu District Clinical Trial IRB, Hakataeki-Higashi Clinic IRB, Chiba Kaihin Municipal Hospital IRB, Eiyukai Yasuda Hospital IRB, Jikeikai Shinsuma General Hospital IRB, Sapporo Medical Association IRB, Bokai Tenshi Hospital IRB, Suita Municipal Hospital IRB, Kansai Rosai Hospital IRB, Saiseikai Suita Hospital IRB, Yuwakai Kimura Hospital IRB, Yokohama Sakae Kyowai Hospital IRB, Nippon Koukan Hospital IRB, Koujinkai Sapporo Dermatology Clinic IRB, Tokushima Red Cross Hospital IRB, Yamate Dermatological Clinic IRB, Tokushukai Group IRB, Seiwakai Shouda Hospital IRB, Kumamoto City Hospital IRB, Toyama Prefectural Central Hospital IRB, Japanese Red Cross Nagoya Daiichi Hospital IRB, Higashiyama Shinagawa Clinic IRB, National Hospital Organization Central Review Board, Seikoukai Kusatsu General Hospital IRB, Japanese Red Cross Kyoto Daini Hospital IRB, Ehime Rosai Hospital IRB, NTT Medical Center Tokyo IRB, Chiba Rosai Hospital IRB, Nara Prefectural General Medical Center IRB, Fuyo Association Seirei Numazu Hospital IRB, Kagoshima City Hospital IRB, Iizuka Hospital IRB, Fukui General Hospital IRB, Osaka City University Hospital IRB, Oita Prefectural Hospital IRB, Chiyukai Fukuoka Shin Mizumaki Hospital IRB, Northern Kyushu Saiseikai Central IRB, Funabashi Municipal Medical Center IRB, Kagawa Rosai Hospital IRB, Japanese Red Cross Takayama Hospital IRB, Hamanomachi Hospital IRB, Tazuke Kofukai Medical Research Institute, Kitano Hospital IRB, Wakokai Kawasaki Rinko General Hospital IRB, Hiroshima Prefectural Hospital IRB, Fukui Prefectural Hospital IRB, Ogikubo Hospital IRB, Yuasa Houonkai Central IRB, Jizankai Tsuboi Hospital IRB, Tokyo Women's Medical University IRB, Kochi Medical School Hospital IRB, Okayama City Hospital IRB, Ikeda City Hospital IRB, Kawanishi City Hospital IRB, Hiratsuka Kyosai Hospital IRB, Japanese Red Cross Kumamoto Hospital IRB, Satokai Yuge Neuropsychiatric Hospital IRB, Kurashiki Medical Center IRB, Ekihigashi Hihuka Clinic IRB, Marunouchi Hospital IRB, Mizuo Clinic IRB, Ishikawa Prefectural Central Hospital IRB, Osaka Police Hospital IRB, Teine Keijinkai Hospital IRB, Shinagawa East One Medical Clinic IRB, Showa University Fujigaoka Hospital IRB, Yaizu City Hospital IRB, Osaka Central Hospital IRB, Enshu Hospital IRB, Nagano Prefectural Susaka Hospital IRB, Ogori Daiichi General Hospital IRB, Minami Sakai Hospital IRB, and Nagano Municipal Hospital Clinical Research (Clinical Trial) IRB.
Consent for publication
Not applicable.
Competing interests
KK, MT, and TK are employees, and YS was a past employee, of Takeda Pharmaceutical Company Limited. NT and YO have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Demographic and baseline characteristics.
Additional file 2.
Change from baseline in mean of M-B&B score for pelvic pain, dysmenorrhea, and dyspareunia by visit.
Additional file 3.
Change from baseline in mean of B&B score for pelvic pain, dysmenorrhea, and dyspareunia by visit.
Additional file 4.
Results of other endpoints.
Additional file 5.
Summary of pharmacodynamic parameters at each assessment point.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Osuga, Y., Seki, Y., Tanimoto, M. et al. Relugolix, an oral gonadotropin-releasing hormone (GnRH) receptor antagonist, in women with endometriosis-associated pain: phase 2 safety and efficacy 24-week results. BMC Women's Health 21, 250 (2021). https://doi.org/10.1186/s12905-021-01393-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-021-01393-3