Abstract
Background
Although age specific stroke rates are higher in men, women have a higher lifetime risk and are more likely to die from a stroke. Despite this increased severity, most studies focus on male/female differences in stroke onset, patterns of care and stroke-related outcomes. Given that stroke presents differently in men and women, mixed sex studies fail to fully capture heterogeneity among women with stroke and the subsequent impact on their outcomes. This study examined the sociodemographic characteristics, factors related to stroke incidence and post-stroke functional status between young (< 60) and old (≥ 60) women with stroke.
Methods
Using 5 years of data from the National Health Interview Survey (NHIS), a nationally representative sample of US adults, cohorts of young and old women with stroke were identified. A set of demographic/lifestyle, health services utilization and health status characteristics were used evaluate within gender heterogeneity in three ways. First, disparities in population characteristics were assessed using Chi-Square and t tests. Second, young and old women with stroke were matched with women without stroke in their respective cohorts to determine differences in factors related to stroke incidence. Finally, the determinants of post-stroke functional limitation for the two cohorts were determined.
Results
Young women with stroke were more likely to be Black, smoke regularly and frequently consume alcohol than older women. Young women were also less likely to engage with their health provider regularly or receive preventative health screenings. Diabetes, high blood pressure, high cholesterol and high BMI were correlated with an increased relative likelihood of stroke among older women. In contrast, family size, smoking frequency, alcohol consumption and sleep were correlated with an increased prevalence of stroke among young women. Although factors correlated with stroke varied between young and old women, health status and receipt of healthcare were the most significant determinants of post-stroke functional status for both cohorts.
Conclusions
Health related characteristics were the primary correlates of stroke in older women, whereas post-stroke lifestyle and behaviors are the most significant correlates for younger stroke survivors. These findings suggest that while receipt of health services is essential for preventing stroke in both young and old women, providers should stress the importance of post-stoke lifestyle and behaviors to younger women at risk of stroke using approaches that may be different from older stroke women.
Similar content being viewed by others
Introduction
Stroke is the leading cause of long-term disability in the US with approximately 795,000 Americans newly diagnosed with a stroke annually [1]. There is a substantial literature indicating sex disparities in stroke and stroke-related outcomes [2]. Collective evidence indicates women are more likely to: (a) have a stroke over a lifetime due to longer lifespans [3, 4], (b) experience strokes at an older age [5], (c) have more severe strokes [6], (d) die of stroke [7], (e) have greater illness at the time of stroke [8] and (f) have greater long-term post-stroke disability [9] relative to men [10]. There are many reported reasons indicating why women are more likely to have a stroke including: women live longer than men, and older age increases stroke risk. Other important risk factors for stroke in women include hypertension, heart disease, diabetes mellitus [11,12,13,14], antiphospholipid antibodies [15], pregnancy, use of birth control containing estrogen [16] and migraine with aura [17,18,19]—conditions more common among women comparatively to men.
Since studies have also shown that women are typically 4 years older than men at the time of stroke onset, older age has been attributed to their reduced pre-stroke functional ability [20], greater overall chronic illness burden [21] and greater likelihood of more severe strokes [22,23,24]. Furthermore, because strokes typically occur later in life, other age-related processes are also occurring that result in greater biological aging in stroke survivors over and above their chronological age [25]. Consistently, age is cited as the primary determinant of outcome differentials. However, researchers have to date offered little evidence explaining differential outcomes among young stroke survivors, particularly women. This study supplements existing knowledge of women with stroke by examining differences in demographic/lifestyle characteristics, physical/mental health status and health services utilization between young (< 60) and old (≥ 60) women with stroke. This analysis provides a more accurate characterization of stroke in women than previous mixed gender studies by examining within sex heterogeneity. This framework explores differences female age cohorts to enhance understanding of the causal, characteristic and outcome disparities between young and old female stroke survivors.
Healthcare, demographic and health status characteristics used in this study were drawn from literature citing correlation with stroke. While the role of traditional risk factors in the pathogenesis of stroke in younger adults has been debated, several studies have demonstrated a high prevalence of traditional cardiovascular risk factors among young individuals with stroke, primarily high levels of alcohol consumption [26], smoking [11, 14, 18], physical inactivity [27], poor diet [28], and obesity [29, 30]. While recent studies have shown that ischemic stroke is increasing in younger adults, they have also demonstrated an increasing prevalence of those traditional stroke risk factors (hypertension, dyslipidemia, diabetes mellitus, tobacco use, and obesity) that were previously only common in older adults [31, 32]. It is believed that a higher prevalence of these traditional risk factors increases susceptibility to stroke from other causes in younger adults [33].
Little is known, about stroke among younger age cohorts and even less is known about stroke in young women. This study extends the current research regarding stroke in women by examining the differences in demographic/lifestyle, healthcare utilization, health status and post-stroke functional status among old and young women with stroke. A greater understanding of stroke in women and how various characteristics are related to the prevalence of stroke in women may help better identify high risk populations and target preventative strategies. Furthermore, analysis of differences among cohorts of women, rather than between men and women, may help clarify mechanisms of stroke in young and old women and potential differences in risk factors related to the incidence of early stroke.
Materials and methods
Database
Data from the 2014 through 2018 National Health Interview Survey (NHIS) was pooled to identify two cohorts of young (age less than 60) and old (age greater than 60) women. NHIS is a cross sectional household interview survey collected through geographically clustered sampling techniques. Information in the NHIS concerns the amount, distribution and effects of illness and disability in the United States and the services rendered for or because of such conditions in the noninstitutionalized civilian population. The main objective of the NHIS is to monitor the health of the US population through the collection and analysis of data on a broad range of health topics. The survey allows categorization of a variety of health characteristics by demographic and socioeconomic characteristics. Content in the NHIS is updated every 15–20 years, most recently in 2019 when it launched a redesigned content and structure that differs from its previous questionnaire design (1997–2018). Due to the redesigned 2019 sample, only data from 2014 through 2018 is included in this study due to comparability of survey items.
NHIS is a cross-sectional household interview survey targeting the civilian noninstitutionalized population residing within the 50 states and the District of Columbia at the time of the interview. The NHIS universe includes residents of households and noninstitutional group quarters. As the NHIS is conducted in a face-to-face interview format, a simple random sample of dwelling units would be too dispersed throughout the nation; as a result, the costs of interviewing a simple random sample of 35,000 dwelling units would be prohibitive. To achieve sampling efficiency and to keep survey operations manageable, cost-effective, and timely, the NHIS uses complex sampling techniques to select the sample of dwelling units for the NHIS. These methods partition the target universe into strata and clusters. Therefore, users of the public use NHIS files must utilize appropriately provided controls for clustering and stratification in addition to sampling weights to ensure that estimates are unbiased and standard errors are consistent. Additional information can be reviewed here: https://www.cdc.gov/nchs/nhis/methods.htm.
Sample
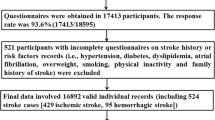
This investigation utilized a historical cohort study design. The study cohort was constructed by pooling women from the 2014 through 2018 NHIS ≥ 18 years who had responded either yes or no to the question “Have you ever been told by a doctor or other health professional that you had a stroke?” (n = 65,092). While NHIS does not include information on respondent age at stroke diagnosis, it does provide their age at the time of survey response. Women were divided into two cohorts based on age—young, less than 60, and old, greater than or equal to 60. Strokes were assumed to have occurred prior to the time of interview.
Since the average of stroke in women is 72.9, the young cohort was characterized by below average age at stroke [34]. This study cannot rule out that women in the older cohort suffered a stroke prior to age 60. However, estimates suggest only five to six women, 0.4%, in the older category would be misclassified [17]. Among the 65,092 women who responded to the survey item on stroke diagnosis, only 4%, (2,379 women unweighted) reported having experienced a stroke—slightly below the national average. Over 70% were over age 60 (n = 1,715), with less than 30% below age 60 (n = 664).
Variables of interest
Characteristics of interest were divided into four categories: (1) demographic/lifestyle, (2) health services utilization, (3) health status and (4) post-stroke functional status.
-
Demographic/Lifestyle characteristics include race, region of residence, marital status, household size, smoking regularity, frequency of alcohol consumption and hours of sleep. These characteristics, as referenced above, are correlated with stroke and/or primary health outcomes.
-
Health services utilization is characterized by receipt of health services within the last 12 months including blood pressure check, cholesterol screening, prescribed medications, total number of office visits, total number emergency room visits, total number of surgeries, having a regular place to go when sick and the most recent time respondents saw or talked to a health professional. These services were received post-stroke and NHIS does not provide an indicator capturing pre-stroke receipt of care. However, health services literature suggests that individuals establish patterns of health services utilization, particularly preventative care, relatively early in life [35,36,37,38]. As long as individuals maintain some form of health insurance (all women in the panel were insured), their patterns remain relatively consistent over the life course [36, 37]. Therefore, this study contends that previous receipt of health services in highly correlated with present receipt of health services apart from catastrophic accident or event and the preventative care and screening patterns remain consistent [36].
-
Health status describes both physical and emotional well-being. Indicators for diagnosis of diabetes, hypertension and high cholesterol and the frequency of feeling worthless, hopeless or depressed. These conditions were reported at the time of the survey rather than the time of stroke. However, given their chronic nature and duration of development, they likely existed for many years and developed prior to the stroke event.
-
Post-stroke functional status is described by presence of a functional limitation, suffering from a chronic condition or feeling as though stroke-related problems cause difficulty with activities. These items are derived directly from survey items regarding functional status.
Statistical analysis
All three phases of analysis were performed using the SAS statistical package (SAS System for Windows, Version 9.4, Cary NC, USA). First, Pearson Chi-Square Statistics and independent sample t-tests investigated disparities in demographic/lifestyle characteristics, healthcare utilization, health status and post-stroke functional status between young and old women with stroke. Second, the correlation between healthcare utilization, demographic/lifestyle traits and health status and prevalence of stroke was calculated for the young and old cohorts of women using Cox proportional hazards regression on a match cohort of young and old women with and without stroke. Matching was performed using propensity scores derived from age, race, region of residence, education, household size, and marital status with replacement. Finally, the impact of health status, healthcare utilization and demographics/lifestyle on post-stroke functional status was assessed with multiple logistic regression for young and old stroke sufferers.
Results
Mean prevalence values for all demographic, health status, healthcare utilization and functional status characteristics are listed in Table 1 for the young and old cohorts. Comparative sample statistics indicating significant differences between the cohorts are provided in Table 1.
Cross-cohort comparisons of key outcome variables
Demographic/lifestyle
Young women with stroke are 24% Black, compared to only 17% in the older cohort—a statistically significant difference (χ2 = 16.77, p < 0.001). They are also more likely to live in the South (χ2 = 4.14, p = 0.0373), be married (χ2 = 13.62, p = 0.001) and smoke cigarettes (χ2 = 9.53, p = 0.0019). They also live in larger houses, 2.26, than their older counterparts (1.67) (t-statistic = 11.18, p < 0.001) and sleep less per night (6.72, 7.50) (t statistic = 8.09, p < 0.001).
Healthcare utilization
The number of office visits, emergency department visits and surgeries in the past year was assessed between young and old women as well as routine screening for blood pressure, cholesterol and blood sugar. Surprisingly, older women visit the physician’s office (4.06 for older vs 4.29 for younger) and the emergency room (0.77 for older vs 1.13 for younger) less frequently than younger women with stroke (office visits, t statistic = 2.05, p = 0.0407; emergency room, t statistic = 6.38, p < 0.001). Older women have higher prevalence of blood pressure checks, cholesterol screenings, prescribed medication and speaking with their provider in the past 12 months.
Health status
While older women have a higher prevalence of physical health problems including of hypertension (0.92 vs 0.91) (χ2 = 0.11, p = 0.7216) diabetes (0.29 vs 0.26) (χ2 = 2.89, p = 0.0999) and high cholesterol (0.66 vs 0.47) (χ2 = 70.06, p < 0.001), younger women are more likely to have symptoms of poor mental health including feelings of hopelessness (0.05 vs 0.11) (χ2 = 24.52, p < 0.001), worthlessness (0.06 vs 0.09) (χ2 = 12.04, p = 0.002) and sadness (0.07 vs 0.13) (χ2 = 23.04, p < 0.001).
Post-stroke functional status
Younger women are more likely to report that stroke-related difficulties cause problems with activity (30% of younger vs 27% of older, t statistic = 3.72, p = 0.0493), while older women more frequently report overall functional limitations (78% for younger vs 89% for older, t statistic = 42.27, p < 0.001). However, there is no statistically significant difference in reporting of difficulties related to chronic conditions (t statistic = 0.51, p = 0.4804).
Contribution of key outcome variables to stroke prevalence
To determine the relationship between demographics/lifestyle, health status and healthcare utilization on prevalence of stroke for old and young women, individuals with stroke in each cohort were matched with women without stroke based on age, race, region, and chronic conditions. Results from cohort specific models are provided in Table 2. Those estimates significantly correlated with stroke differ between you and old women.
Among older women, more frequent utilization of health services such as office visits (β = 0.04, p value = 0.0466, HR = 1.04), prescription medications (β = 0.61, p value = 0.0311, HR = 1.84) and emergency room (β = 0.24, p value < 0.001, HR = 1.27) visits was highly correlated with stroke compared to those with lower frequencies of utilization in their age cohort. Additionally, older women with confounding comorbid conditions like hypertension (β = 0.17, p value = 0.0179, HR = 1.19), diabetes (β = 0.21, p value = 0.0127, HR = 1.12), high cholesterol (β = 0.42, p value < 0.001, HR = 1.53) and higher BMI (β = 0.03, p value < 0.001, HR = 1.03) showed substantially larger relative prevalence of stroke.
Among younger women, frequent visits to physicians’ offices (β = 0.01, p value = 0.004, HR = 1.11) and the emergency room (β = 0.024, p value < 0.001, HR = 1.27) were significantly related to incidence of stroke. The largest correlates of stroke among younger women were household, demographic, and lifestyle characteristics. The magnitude of the hazard ratio was small compared to other characteristics. Women in the younger cohort living in the South (β = 0.41, p value = 0.0014, HR = 1.51) with larger families (β = 0.17, p value = 0.006, HR = 1.18) have higher prevalence. However, lifestyle characteristics appear to have the largest impact on stroke incidence. Smoking (β = 0.24, p value = 0.0486, HR = 1.27) and consuming alcohol (β = 0.00, p value = 0.0505, HR = 1.00) were positively correlated with incidence of stroke, while increasing health habits like sleep (β = − 0.10, p value = 0.0052, HR = 0.90) were negatively correlated with stroke. Interestingly, being married (β = − 0.46, p value = 0.002, HR = 0.63) was negatively correlated with stroke while feeling sad or depressed (β = 0.46, p value = 0.0103, HR = 1.58) was positively correlated with stroke incidence.
Contribution of key variables to post-stroke functional status
To evaluate the determinants of post-stroke functionality among old and young women, three measures of functionality were assessed: overall functional limitations, stroke problems impeding activity and chronic conditions limiting behavior. Results are listed in Tables 3, 4 and 5. To observe associations with post-stroke functional limitations, regressions included a subset of characteristics to allow comparison of the determinants between cohorts. Interestingly, older and younger women experience similar determinants of post-stroke functionality. Interestingly, family size and being married is associated with a higher relative probability of having limited function or difficulty with activity. Indicating that individuals with limitations often live with other household members or that individuals in larger household rely on others to perform tasks that require mobility.
Discussion
This study focused on within age-related sex heterogeneity in demographic/lifestyle characteristics, health status and healthcare utilization. Disparities in cohort characteristics, prevalence of stroke event and determinants of post-stroke limitation were compared between the two groups. Of the 42,038 women under 60 identified form NHIS data, 1.58% (n = 664) had been diagnosed with stroke compared to 7.44% (n = 1715) of the 23,054 women over 60. While stroke is more common in older women, the National Stroke Association, strokes has reported a rise in stroke incidence among younger adults. Over the past decade, the US has seen a 44% increase in the number of young adults hospitalized due to stroke. Age inclusive studies to date have been primarily mixed gender. This analysis, however, examines within gender differences comparing characteristics, prevalence of stroke and determinants of post-stroke functional limitation between women above and below the age of 60.
Understanding risk factor profiles are critically important to understanding strategies to reduce stroke risk in women. For example, a recent study showed that stroke risk factors are more strongly associated with risk of stroke in women compared to men regardless of the stroke subtype and with men having higher incidence than women [39].
These findings highlight the complexity of the relationship between stroke risk factors and stroke onset particularly among women in general, women of different ages and women of different races. They also suggest more detailed analyses should be completed to examine variability among women as well as differences between men and women. More importantly, comparison of these age cohorts indicates two distinctly different populations of women experiencing stroke. While older women had a higher prevalence of healthcare utilization including blood pressure checks, cholesterol screening, speaking with healthcare providers and taking prescription medications, the young cohort was significantly more likely to visit the emergency or engage in an appointment with a physician. Younger women with stroke were more likely to be Black, reside in the south and be married. However, they were also more likely to smoke and slept significantly fewer hours per night than their older counterparts. These results compare with similar mixed gender and age inclusive assessment of stroke in women and minority populations [40,41,42]. These findings also highlight previously reported age-related differences in disease prevention practices [43]. Magwood et al. [43] found that although many young stroke survivors exhibit comorbid disease conditions that are similar to older stroke survivors, they are less like to follow-up with physicians than older stroke survivors.
Additional comparisons showed that older women had a significantly higher prevalence of those physical health conditions traditionally related to stroke—diabetes, hypertension and high cholesterol—while the younger cohort reported substantially higher mental health concerns—frequently feeling depressed, worthless or sad. These findings provide a sensible explanation for stroke in the older cohort—increased age coupled with confounding comorbidities and poor health results in stroke among women over 60. Magwood et al. [43] suggest that the higher rate of known risk conditions among young women and women of color could account for these observations. While the patterns of office and ER visits among women under 60 would suggest poor health status, the lower proportion reporting physical health issues could suggest that these issues are present but remain undiagnosed likely due to lack of preventative health services or regular health screening. Interestingly, while this comprises only one plausible explanation, women in poor health have shown to be reluctant to utilize health services for a variety of reasons [44].
A second explanation may be related to a greater presence of vascular risk factors among older stroke women. The role of vascular risk factors has not been widely studied among young women stroke survivors. Cigarette smoking, alcohol consumption and drug use were also associated higher stroke rates particularly among those with confounding chronic or cardiovascular conditions [32, 45, 46]. Age inclusive studies have shown higher rate of stroke among those who have less than high school education and live below poverty level. Numerous studies have shown a correlation between socio economic status (SES) and stroke/stroke mortality—results were robust to the SES indicator used [42, 47]. While not widely studied in adults of any age, being overweight or obese and having inadequate levels physical activity were also more common among individuals with stroke [48, 49].
Young and old women exhibited different predictors of stroke or suspected lifestyle, demographic or environmental characteristic highly correlated with the likelihood of experiencing a stroke According to Carandang et al. [50], risk factors are relevant if they are strong and dose-related, predictive in a variety of samples, pathogenically plausible and supported by other investigations. While relatively few investigations have focused on age specific heterogeneity in women, factors shown to be highly correlated with stroke in this study largely align with those vascular and lifestyle characteristics cited elsewhere [51].
While relevant predictors of stroke were generally consistent in previous research, this cohorts displayed largely different subsets of predictors. For example, risk of stroke increased with the presence of hypertension, diabetes, high cholesterol and high BMI in older women by 19, 23, 53 and 3% respectively. For young women with stroke, both marital status and sleep lower the risk of stroke by 27 and 10% respectively. In contrast, while smoking and alcohol consumption increase the risk for stroke by two and 27%. The older cohort showed increased risk of stroke from primarily health related comorbidities, while the younger cohort shows risk to be more closely related to lifestyle and behavioral characteristics. Overall, demographic/lifestyle predictors of stroke were consistent with previous studies of men and women which have shown that blood pressure, smoking, physical activity and healthy diet reduce the risk of stroke [52, 53]. In fact, longitudinal assessment has demonstrated that modest changes in modifiable lifestyle risk factors can have a substantial effect on risk as all ages.
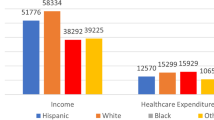
Black race also emerged as a primary correlate of stroke in younger women and has been previously reported as a risk factor in other studies. Evidence suggests significant racial disparities in stroke and stroke mortality among women with the highest disparities among women aged 50–< 60 [54]. Previous research has shown that hypertension, coronary artery disease, hyperlipidemia and diabetes more common in older Black compared to White adults [55,56,57]. While the root causes of these disparities is not fully understood, studies suggests a younger age of stroke onset among Black adults [58,59,60], potentially because of a heavier burden of stroke risk factors among Black adults at younger ages, as early as adolescence [61]. For example, elevated systolic blood pressure (SBP) may confer a greater risk of stroke among Black adults compared with White adults [62]. Importantly, socioeconomic factors have demonstrated only a minimal role in explaining racial disparities in stroke compared with the contribution of traditional stroke risk factors [58, 60]. Although higher socioeconomic status may attenuate racial disparities in stroke, Jiménez, et al. [54] suggests that the elevated stroke incidence among younger Black women and those without a family history of stroke, could reflect persistent racial differences in the distribution of deleterious exposures at the individual, neighborhood and institutional levels across the life course. Unequal access to material and social resources and psychological stress among Black women may result in accelerated cardiovascular aging. While cursory assessment of these disparities may suggest that they could be driven by income or other socioeconomic differences, studies have shown that lower income does not increase risk of ischemic stroke [63]. We do note that previous that showed higher level of income was associated with higher risk of ischemic stroke, the study focused only on individuals over age 65 indicating a reversal of the social gradient. Ultimately, the results could be explained by selective survival, yet no evidence of higher stroke risk among lower socioeconomic groups was found.
A second issue that should be considered in analyses of stroke relates to genetic contribution to stroke risk. To date, studies including genetic disposition have been limited, but family history is suggested to be a risk factor for ischemic stroke [64, 65]. While strokes occurring in very old age tending to be less familial, those occurring at younger ages are believed to be at least partially heritable [66,67,68,69,70]. However, evidence of heritability is not sufficient to assert it comprises the primary cause of stroke in younger adults. However, alternative theories fail to explain the fact that nearly one fourth of strokes occur in people under the age of 65.
Finally, measures of post-stroke function were completed to examine potential differences between older and younger women. Binary indicators for overall functional limitations, stroke problems impeding activity and chronic conditions limiting behaviors used to assess limitations were highly related with physical health determinants in both cohorts. Hypertension, diabetes and high BMI indicate lower levels of general health, reduced functionality and limited activity. All three indicators show a negative relationship to age suggesting that limitations increase over time. Not surprisingly, women taking prescription medication, experiencing surgeries and visiting the emergency show an increased likelihood of limitations and obstructed activity suggesting higher levels of impairment and greater post-stroke limitations.
Limitations
Although interesting findings, the study does have a number of imitations. First, NHIS did not include respondent age at stroke. Without this information, individuals were classified into age cohorts by their age at the time of the interview rather their age at the event. Therefore, it is possible that older women who experienced a stroke below the age of 60 were misclassified. Second, NHIS does not include an indicator for the totally number of stroke events, the type of stroke suffered, months post-stroke, stroke severity, or the receipt of post-stroke rehabilitative care. These factors were unavailable in the NHIS data but have the potential to confound estimations of functional limitations and other post-stroke outcomes. While data from 5 years of the NHIS data were pooled for this analysis, NHIS is a cross sectional data set precluding longitudinal assessment of individuals over time as they recover from each stroke event. Third, all women in the sample were insured; therefore, results are not generalizable to an uninsured population which could have different outcome correlates. Fourth, all NHIS data included functional status and stroke events are self-reported and, therefore, subject to recall and selectivity bias. Finally, type, quality and the relationship to the primary care has been shown to impact post-stroke outcomes, disability status and quality of life. Unfortunately, caregiver information and type are not included in the NHIS survey. Finally, the NHIS is based on respondent interviews. Survey data is subject to recall, telescoping and social desirability bias.
Conclusion
Stroke is a major cause of death and disability in the United States impacting 23–29% of the population. While a variety of studies have examined stroke, stroke-related mortality, and post-stroke disability, most current research involves mixed-gender panels. This study exploits the within gender heterogeneity among women with stroke by examining factors related to stroke in young and old women. Results suggest that those factors related to stroke differ between young and old women with behavioral characteristics including smoking frequency, alcohol consumption, and sleep being significant in young women and diabetes, high blood pressure, high cholesterol and high BMI being correlated in older women. However, health status and receipt of healthcare were the most significant determinants of post-stroke functional status for both cohorts. Since those factors correlated with stroke in women vary significantly by age, studies examining women in different age cohorts are needed to address age and gender specific factors and have the best opportunity to reduce or postpone the devastating impact of stroke in women.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the National Health Interview Survey repository, https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm
References
Cassella CR, Jagoda A. Ischemic stroke: advances in diagnosis and management. Emerg Med Clin N Am. 2017;35:911–30.
Dehlendorff C, Andersen KK, Olsen TS. Sex disparities in stroke: Women have more severe strokes but better survival than men. J Am Heart Assoc. 2015. https://doi.org/10.1161/JAHA.115.001967.
Stuart-Shor EM, Wellenius GA, DelloIacono DM, Mittleman MA. Gender differences in presenting and prodromal stroke symptoms. Stroke. 2009;40:1121–6.
Reeves MJ, Bushnell CD, Howard G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–26.
Haast RA, Gustafson DR, Kiliaan AJ. Sex differences in stroke. J Cereb Blood Flow Metab. 2012;32:2100–7.
Lang C, Seyfang L, Ferrari J, Gattringer T, Greisenegger S, Willeit K, Toell T, Krebs S, Brainin M, Kiechl S, Willeit J. Do women with atrial fibrillation experience more severe strokes? Results from the Austrian stroke unit registry. Stroke. 2017;48(3):778–80.
Carcel C, Woodward M, Wang X, Bushnell C, Sandset EC. Sex matters in stroke: a review of recent evidence on the differences between women and men. Front Neuroendrocrinol. 2020. https://doi.org/10.1016/j.yfrne.2020.100870.
Andrade KV, Souza ICD, Balsells MMD, Lima ACS, Moura ERF, Aquino PDS. Factors associated with performing activities of daily living in women after suffering a stroke. Rev Esc Enferm USP. 2020;54:e03560. https://doi.org/10.1590/s1980-220x2018041503560.
Arba F, Quinn T, Hankey GJ, et al. Determinants of post-stroke cognitive impairment: analysis from VISTA. Acta Neurol Scand. 2017;135:603–7.
Buie JN, Zhao Y, Burns S, et al. Racial disparities in stroke recovery persistence in the post-acute stroke recovery phase: evidence from the health and retirement study. Ethn Dis. 2020;30:339–48.
Lidegaard Ø, Kreiner S. Cerebral thrombosis and oral contraceptives: a case-control study. Contraception. 1998;57:303–14.
Heinemann LAJ, Lewis MA, Spitzer WO, et al. Thromboembolic stroke in young women: a European case-control study on oral contraceptives. Contraception. 1998;57:29–37.
Petitti DB, Sidney S, Bernstein A, Wolf S, Quesenberry C, Ziel HK. Stroke in users of low-dose oral contraceptives. N Engl J Med. 1996;335(1):8–15.
You RX, McNeil JJ, O’Malley HM, Davis SM, Thrift AG, Donnan GA. Risk factors for stroke due to cerebral infarction in young adults. Stroke. 1997;28:1913–8.
Brey RL, Stallworth CL, McGlasson DL, et al. Antiphospholipid antibodies and stroke in young women. Stroke. 2002;33:2396–9.
Kemmeren JM, Tanis BC, van den Bosch MA, et al. Risk of arterial thrombosis in relation to oral contraceptives (RATIO) study: oral contraceptives and the risk of ischemic stroke. Stroke. 2002;33:1202–8.
Nightingale AL, Farmer RD. Ischemic stroke in young women: a nested case–control study using the UK general practice research database. Stroke. 2004;35:1574–8.
Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ. 1999;318:13–8.
Tzourio C, Tehindrazanarivelo A, Iglesias S, et al. Case-control study of migraine and risk of ischaemic stroke in young women. BMJ. 1995;310:830–3.
Renoux C, Coulombe J, Li L, Ganesh A, Silver L, Rothwell PM. Confounding by pre-morbid functional status in studies of apparent sex differences in severity and outcome of stroke. Stroke. 2017;48:2731–8.
Gall S, Phan H, Madsen TE, et al. Focused update of sex differences in patient reported outcome measures after stroke. Stroke. 2018;49:531–5.
Andersen MN, Andersen KK, Kammersgaard LP, Olsen TS. Sex differences in stroke survival: 10-year follow-up of the Copenhagen stroke study cohort. J Stroke Cerebrovasc Dis. 2005;14:215–20.
Berglund A, Schenck-Gustafsson K, von Euler M. Sex differences in the presentation of stroke. Maturitas. 2017;99:47–50.
Willers C, Lekander I, Ekstrand E, et al. Sex as predictor for achieved health outcomes and received care in ischemic stroke and intracerebral hemorrhage: a register-based study. Biol Sex Differ. 2018;9:11.
Soriano-Tárraga C, Giralt-Steinhauer E, Mola-Caminal M, et al. Ischemic stroke patients are biologically older than their chronological age. Aging (Albany NY). 2016;8:2655.
Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:401–11.
Lundberg GP, Volgman AS. Burden of stroke in women. Trends Cardiovasc Med. 2016;26:81–8.
Chomistek AK, Chiuve S, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol. 2015;65:43–51.
Towfighi A, Zheng L, Ovbiagele B. Weight of the obesity epidemic: rising stroke rates among middle-aged women in the United States. Stroke. 2010;41:1371–5.
Kernan WN, Dearborn JL. Obesity increases stroke risk in young adults: opportunity for prevention. Stroke. 2015;46:1435–6.
Renna R, Pilato F, Profice P, et al. Risk factor and etiology analysis of ischemic stroke in young adult patients. J Stroke Cerebrovasc Dis. 2014;23:e221–7.
Rohr J, Kittner S, Feeser B, et al. Traditional risk factors and ischemic stroke in young adults: the Baltimore-Washington cooperative young stroke study. Arch Neurol. 1996;53:603–7.
Ji R, Schwamm LH, Pervez MA, Singhal AB. Ischemic stroke and transient ischemic attack in young adults: risk factors, diagnostic yield, neuroimaging, and thrombolysis. JAMA Neurol. 2013;70:51–7.
Persky RW, Turtzo LC, McCullough LD. Stroke in women: disparities and outcomes. Curr Cardiol Rep. 2010;12:6–13.
Hall A, Wood D, Hou T, Zhang J. Patterns in primary health care utilization among individuals with intellectual and developmental disabilities in Florida. Intellect Dev Disabil. 2007;45:310–22.
DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–91.
Tao G. Utilization pattern of other preventive services during the US Medicare annual wellness visit. Prev Med Rep. 2018;10:210–1.
Allen SM, Wieland S, Griffin J, Gozalo P. Continuity in provider and site of care and preventive services receipt in an adult Medicaid population with physical disabilities. Disabil Health J. 2009;2:180–7.
Peters SAE, Carcel C, Millett ERC, Woodward M. Sex differences in the association between major risk factors and the risk of stroke in the UK Biobank cohort study. Neurology. 2020;95(20):e2715–26. https://doi.org/10.1212/WNL.0000000000010982.
Howard TD, Giles WH, Xu J, et al. Promoter polymorphisms in the nitric oxide synthase 3 gene are associated with ischemic stroke susceptibility in young Black women. Stroke. 2005;36:1848–51.
Qureshi AI, Safdar K, Patel M, Janssen RS, Frankel MR. Stroke in young Black patients: risk factors, subtypes, and prognosis. Stroke. 1995;26:1995–8.
Jacobs BS, Boden-Albala B, Lin IF, Sacco RL. Stroke in the young in the northern Manhattan stroke study. Stroke. 2002;33:2789–93.
Magwood GS, White BM, Ellis C. Stroke-related disease comorbidity and secondary stroke prevention practices among young stroke survivors. J Neurosci Nurs. 2017;49:296–301.
Wilkinson RG. Socioeconomic determinants of health: health inequalities: relative or absolute material standards? BMJ. 1997;314:591.
Bland SD, Bolen JC, Holtzman D, Powell-Griner E, Rhodes L. State-specific prevalence of selected health behaviors, by race and ethnicity—behavioral risk factor surveillance system, 1997. MMWR 2000; i-iii, 1–60.
McGruder HF, Malarcher AM, Antoine TL, Greenlund KJ, Croft JB. Racial and ethnic disparities in cardiovascular risk factors among stroke survivors: United States 1999 to 2001. Stroke. 2004;35:1557–61.
Kapral MK, Wang H, Mamdani M, Tu JV. Effect of socioeconomic status on treatment and mortality after stroke. Stroke. 2002;33:268–73.
Cox AM, McKevitt C, Rudd AG, Wolfe CD. Socioeconomic status and stroke. Lancet Neurol. 2006;5:181–8.
Addo J, Ayerbe L, Mohan KM, et al. Socioeconomic status and stroke: an updated review. Stroke. 2012;43:1186–91.
Carandang R, Seshadri S, Beiser A, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296:2939–46.
Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: The American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37:577–617.
D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care. Circulation. 2008;117:743–53.
Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham study. Stroke. 1991;22:312–8.
Jiménez MC, Manson JE, Cook NR, et al. Racial variation in stroke risk among women by stroke risk factors. Stroke. 2019;50:797–804.
Hajat C, Dundas R, Stewart JA, et al. Cerebrovascular risk factors and stroke subtypes: differences between ethnic groups. Stroke. 2001;32:37–42.
Sacco RL, Boden-Albala B, Abel G, et al. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke. 2001;32:1725–31.
Lee TH, Hsu WC, Chen CJ, Chen ST. Etiologic study of young ischemic stroke in Taiwan. Stroke. 2002;33:1950–5.
Howard VJ, Kleindorfer DO, Judd SE, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–27.
Sacco RL, Boden-Albala B, Gan R, et al. Stroke incidence among White, Black, and Hispanic residents of an urban community: the northern Manhattan stroke study. Am J Epidemiol. 1998;147:259–68.
Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the atherosclerosis risk in communities (ARIC) cohort. Stroke. 1999;30:736–43.
Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127:1369–76.
Howard G, Lackland DT, Kleindorfer DO, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173:46–51.
Grimaud O, Dufouil C, Alpérovitch A, et al. Incidence of ischaemic stroke according to income level among older people: the 3C study. Age Ageing. 2011;40:116–21.
Casas JP, Hingorani AD, Bautista LE, Sharma P. Meta-analysis of genetic studies in ischemic stroke: thirty-two genes involving approximately 18000 cases and 58000 controls. Arch Neurol. 2004;61:1652–61.
Floßmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke. 2004;35:212–27.
Carrieri PB, Orefice G, Maiorino A, Provitera V, Balzano G, Lucariello A. Age-related risk factors for ischemic stroke in Italian men. Neuroepidemiology. 1994;13:28–33.
Jerrard-Dunne P, Cloud G, Hassan A, Markus HS. Evaluating the genetic component of ischemic stroke subtypes: a family history study. Stroke. 2003;34:1364–9.
Kim H, Friedlander Y, Longstreth WT Jr, Edwards KL, Schwartz SM, Siscovick DS. Family history as a risk factor for stroke in young women. Am J Prev Med. 2004;27:391–6.
Liao D, Myers R, Hunt S, et al. Familial history of stroke and stroke risk: the family heart study. Stroke. 1997;28:1908–12.
Schulz UGR, Flossmann E, Rothwell PM. Heritability of ischemic stroke in relation to age, vascular risk factors, and subtypes of incident stroke in population-based studies. Stroke. 2004;35:819–24.
Acknowledgements
N/A.
Human Subjects
This study utilizes publicly available data from the National Health Interview Survey (NHIS). Published NHIS data is de-identified to protect confidentiality of participants and combined with responses from other subjects to prevent disclosure of protected information. Each year the Research Ethics Review Board (ERB) of the National Center for Health Statistics reviews NHIS procedure and data to ensure that it complies with all ethical and scientific standards.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
MJ completed all statistical and data analysis. MJ and CE contributed to the writing and editing of this manuscript. All authors contributed to the design and implementation of the research and to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate.
N/A.
Consent for publication
The authors provide their consent for the publication of the contents of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jacobs, M.M., Ellis, C. Heterogeneity among women with stroke: health, demographic and healthcare utilization differentials. BMC Women's Health 21, 160 (2021). https://doi.org/10.1186/s12905-021-01305-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-021-01305-5