Abstract
Background
Needs-based, patient-oriented palliative care includes palliative day care clinics as a specialized semi-inpatient care offer. However, the establishment and development of these facilities has been unsystematic. Research is needed to strengthen their transparency and ensure their accessibility, quality, and structural adequacy. A national Delphi study was conducted to generate appropriate recommendations for the establishment and development of palliative day care clinics in Germany.
Methods
Recommendations were formulated from focus group data on the development and expansion of palliative day care clinics in Germany. Experts on in- and outpatient palliative care rated 28 recommendations for relevance and feasibility, respectively, using a 4-point Likert-type scale. Suggestions for improvement were captured via free text comments. Items were considered consented when more than 80% of the experts scored them 4 (strongly agree) or 3 (somewhat agree), regarding both relevance and feasibility.
Results
A total of 23 experts (32% response rate) completed three Delphi rounds. Following the first round, 10 of 28 recommendations were revised according to participants’ comments; 1 recommendation was rejected. After the second round, 3 of these 10 recommendations were revised, while 3 were rejected. Consensus was achieved after the third round for 22 of the initial recommendations.
Conclusions
The Delphi-consented recommendations provide a basis for the targeted evidence- and needs-based development of palliative day care clinics. The findings show a need for standards setting and the meaningful integration of these clinics into existing structures.
Trial registration
The present study was prospectively registered on April 20, 2020, with the German Clinical Trials Register (DRKS00021446).
Similar content being viewed by others
Background
Cross-sectoral in- and outpatient palliative care for patients with incurable, progressive diseases and a limited lifespan has developed significantly over the last two decades, in both general and specialized palliative care services in Germany. This development has been partly due to the socio-political relevance of palliative care, alongside demographic changes in the population. Thus, over recent years, an increasing number of palliative care units and specialized palliative home care teams have been established. In 2015, the Hospice and Palliative Care Act added a further focus on strengthening and expanding general palliative care in Germany [1]. This ongoing dynamic development aims at providing needs-based, comprehensive care in both metropolitan areas and structurally weak and rural regions, and creating equal access to palliative care for all German citizens. This overall concept of palliative care includes palliative day care clinics as specialized semi-inpatient care for outpatients [2, 3].
Internationally, the goal of palliative day care clinics is to promote autonomy and improve quality of life for patients in need of palliative care, through medical care (e.g., ascites punctures, wound management), symptom control, physiotherapy, occupational therapy, art and music therapy, complementary therapies (e.g., aromatherapy, massage), and family caregiver support [4,5,6,7,8,9,10,11,12,13,14,15]. The German guidelines for palliative care for cancer patients refer to palliative day care (clinics) as a primarily medical model of care [16, 17]. In Germany, palliative day care clinics are generally affiliated with hospitals [18, 19], and they provide medical, nursing, and psychosocial treatment to patients with complex symptoms. During a visit to a palliative day care clinic, patients can access all departments and diagnostic options of the respective hospital as needed, and they may also receive interventional therapy measures without inpatient hospital admission. Specialist (e.g., oncological) parallel treatment is also possible [20].
Patients cared for in palliative day care clinics generally require the multi-professional diagnostic and therapeutic capabilities of a hospital, but not 24-hour hospital care. Common admission criteria for such clinics include the patient’s health state allowing transport to the clinic and the patient’s need for psychological support, family caregiver relief, monitoring, and symptom control. While no positive effect of palliative day care clinics on quality of life or symptom control has been clearly demonstrated [21], qualitative studies have shown high patient satisfaction [16, 21].
In 2010, the European Association for Palliative Care estimated the need for palliative day care clinics at 1 facility per 150,000 residents [22]. A systematic study of current palliative day care clinics in Germany by the present study team in 2021 identified eight facilities, of which five offered care and three were under development or in the planning stage [18]. This number falls far short of the estimated demand.
To date, the establishment and development of palliative day care clinics in Germany has been unsystematic. Additionally, financing for these clinics has not been uniformly regulated, and thus existing palliative day care clinics are financed by different sources (i.e., statutory health insurance funds, donations, private supplementary payments, support associations) [23]. Accordingly, there is a risk of isolated solutions that are not coordinated—either with each other or with existing services—and therefore not adequately integrated into the overall care of patients at the end of life. To strengthen the transparency of palliative day care clinics in Germany over the long term and ensure their accessibility, quality, and structural adequacy, further research is needed.
Methods
Study aim
The present study aimed at systematically and empirically generating recommendations for the development and expansion of palliative day care clinics in Germany. Recommendations were formulated to optimize the care of terminally ill patients according to their needs and ensure the adequate integration of palliative day care clinics into the existing care landscape.
Study design
The project “Improving health care for patients with terminal, progressive illnesses: Status and demand analysis for palliative day care clinics and day hospices and recommendations for health care planning” (ABPATITE) [24] formulated practical recommendations on the basis of empirical data gathered within the project. An online Delphi survey with palliative care experts was conducted to achieve a national consensus on these recommendations.
Previous research steps in ABPATITE
ABPATITE was divided into three study phases [24]: Phase 1 involved a systematic survey of operating and developing palliative day care clinics and day hospices in Germany. Phase 2 consisted of three work packages aimed at determining the significance of palliative day care clinics: (a) a qualitative study of day hospices and palliative day care clinic management staff, to explore insider views of these facilities; (b) focus groups with local representatives from hospice work and palliative care, to seek the external perspectives of local care networks on the cooperating palliative care services; and (c) a quantitative survey administered to patients and their relatives on care preferences at the end of life. In phase 3, a consensus workshop (i.e., focus groups) was held to reflect on the synthesized evidence from phases 1 and 2 and to derive recommendations for the development and expansion of palliative day care clinics in Germany. The key results of the consensus workshop served as the basis for the present Delphi survey. Recommendations for day hospices were derived separately and are not addressed in this article.
Delphi survey
Participants
Heterogeneous experts who were currently working with or had experience with in- and outpatient palliative and/or hospice care, including experts employed in palliative day care clinics in Germany, were invited to participate in the national Delphi survey. The group of invited experts was meant to be as heterogeneous as possible, to promote diverse perspectives on the presented recommendations. Existing contacts of the study team and the Institute for General Practice and Palliative Care at Hannover Medical School were used to recruit potential participants. In addition, relevant stakeholders were researched online and participants from previous project phases were invited (e.g., from the German Association for Palliative Medicine, the German Hospice and Palliative Care Association, home care and nursing societies, the National Association of Statutory Health Insurance Physicians, the German Medical Association, the National Association of Statutory Health Insurance Funds, the Association of Private Health Insurance Companies, and municipal branches involved in social and health policy). The experts participated voluntarily and without compensation; however, they were invited to participate in a random draw for five 50€ and ten 5€ vouchers for online stores.
Delphi method
The Delphi technique was employed because it enables consensus to be achieved among a wide range of knowledgeable experts when face-to-face discussion is not feasible. In total, 28 recommendations were administered anonymously online, using the software SoSci Survey V3.4 (SoSci Survey GmbH, München, Germany). The Delphi survey was developed for this study (see Supplementary 1 for Delphi survey of round 1). Participants were asked to rate each recommendation on a 4-point verbal scale (i.e., strongly agree, somewhat agree, rather disagree, disagree), according to its: (a) relevance and (b) feasibility for the development and expansion of palliative day care clinics in Germany. Experts also had the option to abstain from rating individual items by selecting a “no answer” option. Each recommendation was considered consented when at least 80% of all participants who rated the item attributed it a score of 4 (i.e., strongly agree) or 3 (i.e., somewhat agree), for both relevance and feasibility. Recommendations that did not achieve consensus in a Delphi round were revised for content and/or language, according to participants’ free text comments. These recommendations were presented in the next Delphi round to all those who participated in the previous round and entered full data.
After each Delphi round was distributed, participants were reminded of their participation a maximum of two times prior to the round closure. The first two Delphi rounds were closed after 4 weeks, while the third round was closed after 2 weeks.
Study material
In the first Delphi round, 28 recommendations were presented in relation to the following topics: (1) the establishment of palliative day care clinics, (2) care provision (i.e., access to palliative day care clinics, integration of family caregivers, opening hours, appointment allocation, public relations), (3) professions and cooperation (i.e., occupational groups, cooperation, volunteer work), and (4) financing. In addition, sociodemographic data were gathered for participants.
Data analysis
Participants in each Delphi survey round confirmed their consent to participate online prior to starting the survey. The results of all Delphi survey rounds, including the sociodemographic data collected, were exported to the software packages IBM SPSS Statistics 28 (SPSS Inc., Chicago, IL, USA) and Microsoft Excel 2016 (Microsoft Corporation, Redmond, WA; USA), and analyzed descriptively. The Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care checklist [25] was used to ensure comprehensive reporting.
Results
Study participants
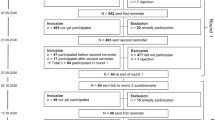
For the first Delphi round, 72 experts were invited to participate. After two reminders were sent, the survey was closed, with 36 responses. Four cases were excluded from the analysis (i.e., two due to a lack of consent to participate and data protection, two due to the submission of an incomplete survey). Thus, 32 data sets (representing 44.4% of the invited responses) were finally included.
All 32 experts from the first round were asked to participate again in the second round. Of these, 27 experts agreed. One expert was later excluded due to a lack of consent to participate. Hence, a final response rate of 26 experts (81.3%) was achieved.
The 27 participating experts from the second Delphi round were invited to participate in the third round. Of these, 23 (85.2%) ultimately completed the survey. Thus, the final response rate was 31.9% (n = 23/72) (see Table 1 for participants’ sociodemographic characteristics).
Results of each Delphi round
First Delphi round
In the first Delphi round, 17 out of the 28 presented recommendations achieved consensus with respect to both assessment criteria (see Table 2). For the first core theme, “establishment of palliative day care clinics,” 2 of the 4 recommendations achieved consensus. For the second core theme, “care provision,” 5 of the 9 recommendations were consented. For the third core theme, “professions and cooperation,” 9 of the 12 recommendations achieved consensus. Finally, 1 of the 3 recommendations for the fourth core theme, “financing,” was consented.
Participants disagreed on 11 items. While 9 of these 11 recommendations reached consensus in terms of relevance, participants disagreed on 10 recommendations because they assessed them as unfeasible. Inability to implement the recommendations due to a lack of funding and qualified staff emerged as the main reasons for their disagreement, in the free text fields. Experts claimed that it is unfeasible to adjust clinic opening hours according to perceived demand and to arrange appointments individually and on short notice, as there is a lack of qualified staff. Also, low awareness of palliative day care clinics was mentioned as a barrier to the establishment of early co-treatment. Ten of these unconsented recommendations were revised by the study team based on participants’ free text comments. One recommendation that did not achieve consensus for either feasibility or relevance in this first Delphi round was rejected because it was perceived to contradict another recommendation that received greater agreement. The aim of the revision was to adapt the content and/or improve the comprehensibility of the unconsented recommendations. Only these revised recommendations were presented in the second Delphi round.
Second Delphi round
Following the first revision cycle, a second Delphi round was carried out with the 10 revised recommendations (see Table 3 and Fig. 1). In this round, four recommendations achieved consensus (i.e., 1 from the core theme “care provision,” 2 from the core theme “professions and cooperation,” 1 from the core theme “financing”). Participants disagreed on 6 items, as they regarded them as unfeasible. Specifically, their free text comments indicated concern that palliative day clinics cannot shoulder early co-treatment on a large scale, due to a lack of facility capacities (i.e., staff, space) and the generally small number of palliative day care clinics in Germany. Furthermore, participants asked for clarification of the role of different therapeutic professions. Three recommendations were revised once again and transferred to the third Delphi round. As with the first revision, participants’ free-text comments were used to revise the recommendations. Another 3 recommendations were rejected because they contradicted other recommendations or because participants’ comments did not indicate how they could be improved. Table 3 presents detailed information on participants’ relevance and feasibility ratings in the second Delphi round.
Third Delphi round
In the third Delphi round, 3 recommendations were presented. Of these recommendations, 1 (i.e., core theme “professions and cooperation”) was consented. The other two were finally rejected, as participants still regarded them as unfeasible due to a lack of palliative day care clinic capacities.
Hence, consensus was ultimately achieved on 22 of the initial 28 recommendations. The final set included 2 recommendations on the core theme of “establishment of palliative day care clinics,” 6 recommendations addressing “care provision” (i.e., access to palliative day care clinics, integration of family caregivers, opening hours, appointment allocation, public relations), 12 addressing “professions and cooperation,” and 2 on “financing.” Table 4 provides detailed information on the 23 participants’ ratings in this round.
Discussion
Summary and discussion of the results
The present Delphi study generated 22 consented practical recommendations for the needs-based development and expansion of palliative day care clinics in Germany. Of these, 17 were immediately consented in the first round, four in the second, and one in the third. Throughout all three Delphi rounds, relevance was consistently rated as high for the great majority of the recommendations. In most cases, the major barrier to consensus was perceived unfeasibility. The consented recommendations aim at supporting the needs-based development of palliative day care clinics and the meaningful integration of such clinics into existing structures. The integration of newly established services requires cooperation between palliative and hospice care network actors, and previous studies have demonstrated that networking and collaboration between all providers in a patient’s care network promotes high-quality care [6, 26,27,28,29]. Four recommendations address the issue of cooperation with other care providers, aimed at enabling more tailored care to meet individual patient needs. The recommendations that palliative day care clinics should introduce themselves to local providers in their respective hospice and palliative care networks when they are newly established, and that information should be exchanged with other care providers on a regular basis, intend to support the interlinking of services and the smooth transition between forms of care.
Other recommendations aim at setting standards for palliative day care clinics. One recommendation calls for the involvement of therapists and another suggests the permanent assignment of nursing staff with specialized palliative care training. A third recommendation is to encourage cooperation with volunteer outpatient hospice services, to build a bridge between palliative day care and care in the patient’s home. Although these three recommendations received approval of at least 96.8% on relevance and 80% on feasibility, some participants indicated concern about their feasibility, due to a shortage of qualified staff. Several additional recommendations that received high agreement regarding relevance, did not achieve consensus for this reason.
A challenge for the implementation of the Delphi study was participants’ divided ratings and free text comments, particularly regarding recommendations for the integration of palliative day care clinic services into the existing palliative and hospice care landscape. Some participants expressed strongly that palliative day care clinics must be careful not to form a parallel structure to existing inpatient and outpatient services.
In general, the consented set of recommendations was practice-oriented, rather than political. Some participants criticized this fact, while others seemed to support it. This disagreement might be due to the fact that approximately one-third of the participants were involved in the development or establishment of a palliative day care clinic or day hospice.
Strengths and limitations
A strength of the present study is that experts with long-standing experience in the field of palliative care in Germany participated in the three Delphi rounds. The assessments of these heterogeneous participants were—expectedly, due to their original activities—influenced by their particular interests and motivations. However, some recommendations were rejected because the free text comments contained little or no information on how they should be revised, and the study team thus had insufficient guidance on how to reformulate them.
The survey was further impacted by two technical limitations. First, the survey system apparently allowed participants to deactivate their consent to participate after having filled in the questionnaire. One recommendation, addressing the patients served by palliative day care clinics, reached 80% agreement in Delphi round 1, but the survey system assigned it an agreement value of only 79%. This is because the data of one participant, who had later deactivated their consent to participate, was included in the survey results. The study team only realized this fault when they included this one recommendation in the second Delphi round. Also, it was not possible to exclude this single participant who did not give consent for Delphi round 2. The survey system only enabled two options: (1) inviting all participants from the former round or (2) inviting all participants who had filled in the survey in the former round (even if they had deleted their consent to participate after completing the survey). This is why 27, instead of 26, experts were invited to participate in the second round.
Conclusions
The present study generated 22 practical recommendations for the targeted, evidence- and needs-based development of palliative day care clinics in Germany. The findings show a concrete need for standards setting and the meaningful integration of these clinics into existing structures.
Availability of data and material
The datasets analyzed in this study are available from the corresponding author upon reasonable request.
References
Bundesministerium der Justiz. Gesetz zur Verbesserung der Hospiz- und Palliativversorgung in Deutschland (Hospiz- und Palliativgesetz—HPG). Bundesgesetzblatt. 2015;48:2114–8.
Clark D, ten Have H, Janssens R. Common threads? Palliative care service developments in seven European countries. Palliat Med. 2000;14(6):479–90. https://doi.org/10.1191/026921600701536408.
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF). Erweiterte S3-Leitlinie Palliativmedizin für Patienten mit einer nicht-heilbaren Krebserkrankung. Langversion 1.1. 2015; https://www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/Palliativmedizin/LL_Palliativmedizin_Langversion_1_1.pdf. Accessed 11 Sept 2023.
Tebbit P. Palliative Care 2000: commissioning through partnership. London: NationalCouncil for Hospice and Specialist Palliative Care Services; 1999.
Gagnon B, et al. Palliative day-care centers and day hospitals. In: von Gunten C, Bruera E, Higginson I, et al., editors. Textbook of palliative medicine and supportive care. Boca Raton, FL: CRC Press; 2015. p. 293–303.
Higginson IJ, Hearn J, Myers K, et al. Palliative day care: What do services do? Palliat Med. 2000;14:277–86. https://doi.org/10.1191/026921600667691270.
Terjung T, Stiel S, Schneider N, Herbst FA. Status, demand and practice models of palliative day-care clinics and day hospices: a scoping review. BMJ Support Palliat Care. 2021. https://doi.org/10.1136/bmjspcare-2021-003171.
Douglas HR, Higginson IJ, Myers K, et al. Assessing structure, process and outcome in palliative day care: a pilot study for a multicentre trial. Health Soc Care Community. 2000;8:336–44. https://doi.org/10.1046/j.1365-2524.2000.00258.x.
Kilonzo I, Lucey M, Twomey F. Implementing outcome measures within an enhanced palliative care day care model. J Pain Symptom Manage. 2015;50:419–23. https://doi.org/10.1016/j.jpainsymman.2015.04.006.
Goodwin DM, Higginson IJ, Myers K, et al. What is palliative day care? A patient perspective of five UK services. Support Care Cancer. 2002;10:556–62. https://doi.org/10.1007/s00520-002-0380-1.
Greaves N. Adult palliative day-care services: An investigation of the factors influencing access to services using the case of a cancer network in the United Kingdom. United Kingdom: Doctoral thesis, University of Warwick, 2012.
Hearn J, Myers K. Palliative day care in practice. Oxford: Oxford University Press; 2001.
Douglas H, Normand CE, Higginson IJ, et al. Palliative day care: What does it cost to run a centre and does attendance affect use of other services? Palliat Med. 2003;17:628–37. https://doi.org/10.1191/0269216303pm799oa.
Andersson Svidén G, Fürst C, Von Koch L, et al. Palliative day care—A study of well-being and health-related quality of life. Palliat Med. 2009;23:441–7. https://doi.org/10.1177/0269216309104891.
Goodwin DM, Higginson IJ, Myers K, et al. Effectiveness of palliative day care in improving pain, symptom control, and quality of life. J Pain Symptom Manage. 2003;25:202–12.
Davies E, Higginson IJ. Systematic review of specialist palliative day-care for adults with cancer. Support Care Cancer. 2005;13:607–27. https://doi.org/10.1007/s00520-004-0739-6.
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF). Erweiterte S3-Leitlinie Palliativmedizin für Patienten mit einer nicht-heilbaren Krebserkrankung. Langversion 2.2. 2020; https://www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/Palliativmedizin/Version_2/LL_Palliativmedizin_Langversion_2.2.pdf. Accessed 11 Sept 2023.
Apolinarski B, Herbst F, Röwer H, et al. Status quo palliativmedizinischer Tageskliniken und Tageshospize in Deutschland: Ergebnisse einer gemischt-methodischen Studie. Z Palliativmedizin. 2021;22(4):215–24. https://doi.org/10.1055/a-1514-8871.
Müller A, Paul A, Best J, et al. “My everyday life has returned to normal”—Experiences of patients and relatives with a palliative day care clinic: A qualitative evaluation study. BMC Palliat Care. 2023;22(1):26. https://doi.org/10.1186/s12904-023-01140-5.
Apolinarski B, Ernst A, Röwer H, et al. Handreichung: Empfehlungen für den bedarfsgerechten Auf- und Ausbau von palliativmedizinischen Tageskliniken und Tageshospizen in Deutschland. 2023; https://www.mhh.de/fileadmin/mhh/allgemeinmedizin/downloads/weitere_Downloadelemente/AllPallMed_Abpatite_Handreichung.pdf. Accessed 11 Sept 2023.
Stevens E, Martin CR, White CA. The outcomes of palliative care day services: a systematic review. Palliat Med. 2011;25:153–69. https://doi.org/10.1177/0269216310381796.
Radbruch L, Payne S. White paper on standards and norms for hospice and palliative care in Europe: Part 2. Euro J Palliat Care. 2010;17(1):22–33.
Apolinarski B, Burger B, Stahmeyer JT, et al. Finanzierung von Tageshospizen und palliativmedizinischen Tageskliniken: Ergebnisse quantitativer Befragungen von Einrichtungsleitungen und Krankenkassen in Deutschland. Gesundheitsökonomie & Qualitätsmanagement. 2022;27(2):74–80. https://doi.org/10.1055/a-1640-2460.
Herbst F, Stiel S, Damm K, et al. Exploring the status of and demand for palliative day-care clinics and day hospices in Germany: A protocol for a mixed-methods study. BMC Palliat Care. 2021;20:94. https://doi.org/10.1186/s12904-021-00792-5.
Jünger S, Payne SA, Brine J, et al. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat Med. 2017;31(8):684–706. https://doi.org/10.1177/0269216317690685.
Bradley SE, Frizelle D, Johnson M. Why do health professionals refer individual patients to specialist day hospice care? J Palliat Med. 2011;14:133–8. https://doi.org/10.1089/jpm.2010.0372.
Kernohan WG, Hasson F, Hutchinson P, et al. Patient satisfaction with hospice daycare. Support Care Cancer. 2006;14:462–8. https://doi.org/10.1007/s00520-005-0901-9.
Schrader S, van Baal K, Schleef T, et al. das klassische Problem ist zu sagen, man ist ja jetzt palliativ“—Versorgung am Lebensende an den Schnittstellen zur hausärztlichen Versorgung in ländlich geprägten Regionen—eine qualitative multiperspektivische Studie. Z Palliativmedizin. 2020;21(6):309–15. https://doi.org/10.1055/a-1228-6556.
Vandaele B, Chambaere K, Devisch I. The strengths and challenges of palliative day-care centers: Qualitative study with the professionals involved. J Palliat Care. 2017;32:55–60. https://doi.org/10.1177/0825859717733833.
Acknowledgements
The authors gratefully thank all participating experts for sharing their opinions. The authors also thank Carolin Huperz for her participation in the development of the initial recommendations for the first Delphi round. Finally, the authors acknowledge Valerie Appleby for her copy-editing of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The present Delphi survey represents one part of the study “Improving health care for patients with terminal, progressive illnesses: Status and demand analysis for palliative day-care clinics and day hospices and recommendations for health care planning” (ABPATITE), financed by the Innovation Fund of the Joint Federal Committee (G-BA) (Grant N° 01VSF19034). The funding body was not involved in the study design, the preparation of this paper, or the decision to submit this paper for publication. The funding body was neither involved in the collection, analysis, or interpretation of the study data.
Author information
Authors and Affiliations
Contributions
SSt (female) and FAH (female) wrote the draft of the manuscript and developed the tables. AE (female), HAAR (female), and BA (female) contributed to the writing and developed a figure. AE and BA analyzed the data. SSt, AE, BA, BB, HAAR, LdJ, SSch, NSch, KD, JTS, and FH participated in the process of recommendation development. All authors enhanced the quality of the manuscript by revising it critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved on February 25, 2020 by the Ethics Committee of Hannover Medical School (8892_BO_S_2020) and the appointed data protection officer of Hannover Medical School. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Prior to accessing the anonymous Delphi survey, experts were informed that the survey data would be treated anonymously and in accordance with data protection guidelines. Informed consent was obtained from all subjects. Experts had to tick a box in the online form to indicate whether they agreed to participation and data processing. To thank participants for taking part in all survey rounds, the study team invited them to voluntarily enter a random draw for gift vouchers. The contact data for the lottery (i.e., email addresses) were collected separately and could not be linked to the survey data.
Consent for publication
The manuscript does not include any potentially identifiable participant data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stiel, S., Ernst, A., Apolinarski, B. et al. Consensus-based recommendations for the development and expansion of palliative day care clinics in Germany: results of a Delphi study. BMC Palliat Care 23, 116 (2024). https://doi.org/10.1186/s12904-024-01441-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-024-01441-3