Abstract
Background
Patients with incurable cancer are frequently hospitalized within their last 30 days of life (DOL) due to numerous symptoms and concerns. These hospitalizations can be burdensome for the patient and the caregivers and are therefore considered a quality indicator of end-of-life care. This retrospective cohort study aims to investigate the rates and potential predictors of hospitalizations and re-hospitalizations within the last 30 DOL.
Methods
This register data study included 383 patients with non-curable cancer who died in the pre-covid period between July 2018 and December 2019. Descriptive statistics with Chi-squared tests for the categorical data and logistic regression analysis were used to identify factors associated with hospitalization within the last 30 DOL.
Results
A total of 272 (71%) had hospitalizations within the last 30 days of life and 93 (24%) had > 1 hospitalizations. Hospitalization was associated with shorter time from palliative care unit (PCU) referral to death, male gender, age < 80 years and systemic anticancer therapy (SACT) within the last 30 DOL. The most common treatment approaches initiated during re-hospitalizations remained treatment for suspected or confirmed infection (45%), pleural or abdominal paracentesis (20%) and erythrocytes transfusion (18%).
Conclusion
Hospitalization and re-hospitalization within the last 30 DOL were associated with male gender, age below 80, systemic anticancer therapy and suspected or confirmed infection.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Several health service quality indicators have previously been identified as important to quality of care at the end-of-life (EOL) for cancer patients [1]. These indicators include the following five: frequency and duration of hospital admissions, intensive care unit (ICU) utilization, deaths in hospital and palliative care unit (PCU) utilization [1, 2]. Measuring these quality indicators can provide insights into areas where the quality and timing of health care provided is not optimized, and subsequently enabling continual improvement of quality of care and priorities to be set [3, 4]. Cancer patients are frequently hospitalized within the last 30 days of life (DOL) [5, 6] and the causes for admissions are often related to the cancer diagnosis or treatments, such as pain, infection or dyspnea [7, 8]. To our knowledge, factors associated with repeated hospitalizations within the last 30 DOL have to a lesser degree been explored. In this study, we hypothesized that certain disease-specific symptomology, demographic and logistic factors are increasing the risk of acute hospitalizations and re-hospitalizations within the last 30 DOL. Identifying potential risk factors for both hospitalizations and re-hospitalizations could contribute to improved health service quality by reducing the rate of burdensome acute re-hospitalizations and futile costly treatment close to death. Therefore, our aims were twofold; first, to assess the five health service quality indicators previously identified as important to quality of care at the EOL. Secondly, to identify risk factors associated with hospital hospitalizations and re-hospitalizations within the last 30 DOL, and describe the inpatient health care utilization during these hospitalizations. Additionally, differences in survival in relation to hospitalizations were assessed.
Methods
Material
We conducted a retrospective review of medical records for all patients who died in the pre-covid period between July 1, 2018, and December 31, 2019 and who were treated at the Oncology Department at a hospital in the southern part of Norway in the same period. Patients were eligible for the study if the malignant disease was documented in the patient record to be incurable and non-hematological. Since pediatric patients and patients with primary gynecologic cancer, head and neck cancer, pulmonary and neuro malignancies were treated in other departments, we did not include those. All hospitalizations within or extending into the last 30 DOL were mapped. Emergency department (ED) visits without subsequently hospitalizations were not included because they are mainly observational stays. Information on main cause of referral and main diagnosis during hospitalization was determined and classified by the first author by reviewing the medical records, and subsequently confirmed by co-author AS. Procedures of less intrusive character and related medications, such as fluid therapy and pain and nausea management, were not registered. These medications are frequently administered and altered in these patients, both in a community-based health care setting and during hospitalizations, independently of main cause of admission.
Statistical considerations
Dichotomization was performed based on the presence or absence of hospitalization within the last 30 DOL and served as dependent variable. For categorical variables, Pearson`s chi-squared test was used for group comparisons. Cox regression analysis and Kaplan–Meier test were used for exploring significance and differences in survival time. To analyze which factors were significantly associated with hospitalization at EOL, we used logistic regression analysis. All patients had a cancer diagnosis; however, particular cancer type was excluded from the regressions analysis due to low frequency in many of the cancer types. Significance level was defined as < 0.05 and all testes were two-tailed.
Results
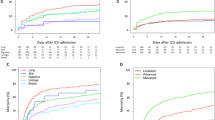
In total 416 patients were identified from record search and among these 383 patients were analyzed. The reasons for exclusion were: malignant entities treated at other departments or other hospitals (n = 19), curative intention of treatment (n = 11) and hematological malignancies (n = 3). The majority of patients in our study had gastrointestinal cancer (n = 200) and were males (n = 237). A total of 272 (71%) had hospitalizations within the last 30 days of life and 93 (34%) of these had > 1 admissions (range 2–4). Mean time spent in hospital within the last 30 DOL was 8 days (range 0–29), which makes up 27% of the time. Mean duration of each stay was 5.6 days (n = 386). Median interval from first hospitalization within the last 30 DOL to re-hospitalizations was 7 days. Time from last hospitalization and last out-patient appointment to the first hospitalization within the last 30 DOL, was 41 days (median) and 29 days (median) respectively. Patients with two or more hospitalizations (n = 93) within the last 30 DOL had a mean age of 68 compared to 72 among those only hospitalized once (p = 0.014). Interval from diagnosis until death was significantly shorter among those with two or more hospitalizations, compared to those with only one hospitalization (mean 443 vs 799 days, p = 0.008, Fig. 1). Demographic and clinical characteristics of patients hospitalized and those not hospitalized within the last 30 DOL is found in Table 1.
Patients with 2 or more hospitalizations (n = 93) were more likely to be living at a nursing home facility by hospitalization number two, three and four (n = 114) compared to index hospitalization and those with only one hospitalization (27% vs 13%, p < 0.001). Utilization of nursing home care services was not significantly higher prior to re-hospitalization in those still living at home compared to the index hospitalization and those with only one hospitalization (72% vs 52%, p = 0.100). Out-of-hours municipal medical center was involved in 11% of the index hospitalizations and those with only one hospitalization within the last 30 DOL (n = 272), decreasing to 4% in the 114 re-hospitalizations.
Suspected or confirmed infection (30%), bronchopulmonary insufficiency (13%), pain (12%) and bile obstruction (8%) remained the most common main diagnosis in re-hospitalizations (n = 114). In hospitalization number three or four (n = 21), suspected or confirmed infection was the main diagnosis in half of the hospitalizations. Characterizations of referrals and hospital stays within the last 30 DOL is found in Table 2.
Antibiotics (45%), pleural or abdominal paracentesis (20%) and erythrocytes transfusion (18%) remained the most common treatment approaches initiated during re-hospitalizations (n = 114) compared to index hospitalization and those with only one hospitalization (n = 272). There was a decrease in imaging utilization in re-hospitalizations compared to index hospitalization and in those with only one hospitalization; Magnetic Resonance Imagination (MRI) (4% vs 10%), Ultrasound (31% vs 39%) and Computer tomography (32% vs 51%). Details on imaging utilization and new treatment approaches initiated in 386 hospitalizations within the last 30 DOL is found in Table 3. Regression analysis on factors associated with hospitalization within the last 30 DOL is presented in Table 4. Age below 80, male gender and SACT the last 30 DOL remained associated with hospitalizations in the analysis.
Discussion
This study assesses the health care utilization in the last 30 DOL in an unselected cohort in a cancer department setting. Our aims were twofold; first, we examined five health service quality indicators previously identified as important to quality care at the EOL. Secondly, we identified the factors leading to hospitalizations and re-hospitalizations within the last 30 DOL and described the inpatient health care utilization during these hospitalizations.
A total of 383 patients were included and among these 272 (71%) were hospitalized with a total of 386 admissions within the last 30 DOL. This rate is higher than findings in several other countries where frequencies vary from 43.2 to 62.6% [9, 10]. Only SACT within the last 30 DOL, age below 80 and male gender remained significant predictors for hospitalizations in the regression analysis. The association between SACT and hospitalizations have previously been well established [11,12,13]. Our findings are in accordance with this association as the vast majority of patients receiving chemotherapy or targeted therapy within the last 30 DOL also where hospitalized.
The proportion of patients with more than one hospitalization within the last 30 DOL was considerable higher at 24% in this study, compared to findings in several other European countries where frequencies vary from < 1% and 11.7% [3, 11]. The reason for our higher rate is not easy to explain. It may be attributed to the characteristics of the patient cohort or local treatment tradition. Our findings are also higher than suggested performance standard stating that less than 4% should have more than one admission within the last 30 DOL [14].
Median total bed days of eight within the last 30 DOL is comparable to findings of seven and nine days in other studies [5, 15]. Hospital death rate of 38% is also similar to findings in other European countries where frequencies vary from 29.4 to 67% [5, 9, 16]. Referral to PCU was not associated with fewer hospitalizations within the last 30 DOL in this cohort, contrary to findings in several other studies [17,18,19]. However, time from referral to PCU until death was significantly shorter in those hospitalized. With an interval of only 56.5 days (median) from referral to PCU until death, there is a limited opportunity window for interventions and facilitation of the last part of life. Early palliative care (i.e. > 6 months prior to death) decreases the risk of receiving hospital care and dying in hospital and increases the probability to receive supportive home care nursing in the last month of life [18]. Taking into account that those not hospitalized in our study were referred only 3 months (median 102 days) prior to death, there seems to be potential for improvement in timing of PCU utilization. Our analysis also showed that whether the patients were referred to PCU prior to the last 30 DOL or not, had no impact on the frequencies of procedures initiated during those last 30 DOL. This also emphasizes the importance of adequate timing of referral to PCU. Our findings of ICU utilization at 4% can be considered in the lower range compared to findings in other Western countries where rates varied between 3.5% and 27.1% [9]. This variation might be attributable to differences in ICU capacity, but also cultural differences in PCU utilization between countries. Previously suggested performance standard of no higher than 4% ICU utilization within the last 30 DOL [14], complies with our findings.
A significant share of the referrals happened out-of-office-hours (43%), similar to findings in other studies [20, 21]. These acute referrals are patient- or caregiver initiated or often involve physicians not known to the patient. Unacquaintance with the patient, the medical history and the field of palliative care, can lower the barrier for referral and hospitalizations [22]. The involvement of General Practitioners (GPs) in connection with hospitalizations at the end-of-life seemed to be quite low and decreased with increasing numbers of re-hospitalizations. Although most patients were living at home when admitted, there was an increasing share of patients living in nursing homes upon re-hospitalizations, which can explain the descending involvement of GPs in re-hospitalizations. Previous studies have shown that palliative care provided by GPs is associated with less time spent in hospital, fewer hospitalizations and non-institutional deaths [3, 23, 24].
Reasons for referrals and main diagnosis during hospitalizations were similar to findings in other studies on cancer patients [7, 20, 21]. Most common treatment approaches initiated during re-hospitalizations within the last 30 DOL were treatment for suspected or confirmed infection, drainage or erythrocyte transfusions. This highlights the importance of advance directives (AD) and EOL care planning. The need of drainage and erythrocytes transfusions can to a certain degree be predicted and planned at the later stage of disease, resulting in minimalized discomfort and time spent in hospital. Also, fever or infection as the most frequent cause of re-hospitalizations in our cohort, emphasizes the challenges in potentially time-critical decision-making processes in pre-hospital settings.
We do not know the clinical implications of the high imaging utilization in this cohort, mainly due to the retrospective character of the study with data from diseased patients with no description on the intention of imaging. As far as we know, such study has not been performed in other comparative hospitals and we therefore have no reference on the use of imaging in this target group. Advanced imaging, such as MRI, might lead to appropriate palliative treatment approaches and de-escalate the intensity of care by reducing futile treatment. However, it can also distract patients from achievable end-of-life goals and are time-consuming and costly procedures [25].
Our findings should be interpreted in the context of its limitations. Although comprehensive data was gathered, some relevant data was not available due to the retrospective design of the study. Access to informal care, patients- and caregivers’ preferences and activities of daily life are factors, which can influence end-of-life management and utilization of health care [13, 22]. A prospective design including qualitative data and patient-reported outcomes might give a more precis description of factors leading to hospitalizations and differences in treatment intensity. We did neither map preexisting comorbidities, cancer stage and details regarding histology of cancers and mutations with treatment and prognostic implications. These factors can also influence the decision-making process regarding treatment intensity and health care utilization [13]. Particular cancer types were too low in numbers to be analyzed as risk factors. However, the association between health care utilization and different cancer types has previously been explored [8, 19, 26]. Cancer patients at the end-of-life often have multiple complaints. By identifying solely main symptom and diagnosis, we probably do not encompass the complex clinical picture and the need of treatment approaches in these patients. The high number of procedures initiated unrelated to main diagnosis during hospitalization in our study, such as abdominal and pleural paracentesis, illustrates the symptom complexity in these patients. However, by conducting a journal review we were able to uncover reasons for hospitalizations more precisely, compared to classification by database coding solely, which can lead to misclassification in a multifaceted hospitalization trajectory. We did not map rate of advanced directives and limitations on life-sustaining treatments, which are associated with improved quality of care at the end-of-life [27,28,29]. These factors have most likely influenced re-hospitalization rates and treatment procedures initiated in this cohort. Actual cause of death was not registered, but in this population, the cancer diagnosis is likely to contribute to death. Since our study includes hospitalizations extending into the last 30 DOL, days hospitalized preceding the last 30 DOL have been included. This makes direct comparison of days spent in hospital somewhat inaccurate. Patients with suspected or confirmed incurable cancer diagnosis never assessed at the Cancer Department, were not included in our study. Many of those may have been regarded as not eligible for SACT and therefore not referred to an oncologist from their GPs or nursing home doctors. This may represent a potential selection bias to our cohort, as we do not know the frequency of hospitalizations at EOL in those patients. On the other hand, real-world evidence studies, including patient registries and electronic health record studies, can provide valuable information on treatment practices and patient characteristics. Ultimately, this information can be used in guidance on treatment decisions and increase end-of-life quality. Further, comparing our immediate pre-pandemic findings to post-pandemic, could illuminate the consequences of the pandemic on health care services utilization in this vulnerable group, including hospitalizations, anti-cancer therapy and PCU-utilization.
Conclusion
Hospitalizations rates within the last 30 DOL were high, and timing of PCU-utilization not optimized. Male gender, age below 80 and systemic anticancer therapy were associated with hospitalizations. Antibiotics, pleural or abdominal drainage and transfusions were the most common treatment approaches in re-hospitalizations, emphasizing the importance of advance care planning.
Availability of data and materials
The data that support the findings of this study are available from the corresponding authors, upon reasonable request.
References
Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003;21(6):1133–8.
Peruselli C, Marinari M, Brivio B, Castagnini G, Cavana M, Centrone G, et al. Evaluating a home palliative care service: development of indicators for a continuous quality improvement program. J Palliat Care. 1997;13(3):34–42.
De Roo ML, Francke AL, Van den Block L, Donker GA, Alonso JE, Miccinesi G, et al. Hospitalizations of cancer patients in the last month of life: quality indicator scores reveal large variation between four European countries in a mortality follow-back study. BMC Palliat Care. 2014;13:54.
Ferrell B, Connor SR, Cordes A, Dahlin CM, Fine PG, Hutton N, et al. The national agenda for quality palliative care: the National Consensus Project and the National Quality Forum. J Pain Symptom Manage. 2007;33(6):737–44.
Vestergaard AHS, Neergaard MA, Christiansen CF, Nielsen H, Lyngaa T, Laut KG, et al. Hospitalisation at the end of life among cancer and non-cancer patients in Denmark: a nationwide register-based cohort study. BMJ Open. 2020;10(6):e033493.
Amado-Tineo JP, Oscanoa-Espinoza T, Vásquez-Alva R, Huari-Pastrana R, Delgado-Guay MO. Emergency Department Use by Terminally Ill Patients: A Systematic Review. J Pain Symptom Manage. 2021;61(3):531–43. https://doi.org/10.1016/j.jpainsymman.2020.08.009.
Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? Can Med Assoc J. 2010;182(6):563–8.
Rivera DR, Gallicchio L, Brown J, Liu B, Kyriacou DN, Shelburne N. Trends in adult cancer-related emergency department utilization: an analysis of data from the Nationwide Emergency Department Sample. JAMA Oncol. 2017;3(10):e172450.
Bekelman JE, Halpern SD, Blankart CR, Bynum JP, Cohen J, Fowler R, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272–83.
Merchant SJ, Lajkosz K, Brogly SB, Booth CM, Nanji S, Patel SV, et al. The final 30 days of life: a study of patients with gastrointestinal cancer in Ontario. Canada J Palliat Care. 2017;32(3–4):92–100.
García-Martín E, Escudero-Vilaplana V, Fox B, Collado-Borrell R, Marzal-Alfaro B, Sánchez-Isac M, et al. Aggressiveness of end-of-life cancer care: what happens in clinical practice? Support Care Cancer. 2021;29(6):3121–7.
Schulkes KJG, van Walree IC, van Elden LJR, van den Bos F, van Huis-Tanja L, Lammers JJ, et al. Chemotherapy and healthcare utilisation near the end of life in patients with cancer. Eur J Cancer Care (Engl). 2018;27(2):e12796.
Lodewijckx E, Kenis C, Flamaing J, Debruyne P, De Groof I, Focan C, et al. Unplanned hospitalizations in older patients with cancer: Occurrence and predictive factors. J Geriatr Oncol. 2021;12(3):368–74.
Earle CC, Neville BA, Landrum MB, Souza JM, Weeks JC, Block SD, et al. Evaluating claims-based indicators of the intensity of end-of-life cancer care. Int J Qual Health Care. 2005;17(6):505–9.
Rautakorpi L, Jyrkkiö S, Löyttyniemi E, Hirvonen O. End-of-life care among patients with pancreatic cancer with or without palliative intervention: a retrospective single-centre study. Acta Oncol (Stockholm, Sweden). 2021;60(1):106–11.
Melac AT, Lesuffleur T, Bousquet PJ, Fagot-Campagna A, Gastaldi-Ménager C, Tuppin P. Cancer and end of life: the management provided during the year and the month preceding death in 2015 and causes of death in France. Support Care Cancer. 2020;28(8):3877–87.
Pellizzari M, Hui D, Pinato E, Lisiero M, Serpentini S, Gubian L, et al. Impact of intensity and timing of integrated home palliative cancer care on end-of-life hospitalization in Northern Italy. Support Care Cancer. 2017;25(4):1201–7.
Seow H, Sutradhar R, Burge F, McGrail K, Guthrie DM, Lawson B, et al. End-of-life outcomes with or without early palliative care: a propensity score matched, population-based cancer cohort study. BMJ Open. 2021;11(2):e041432.
Henson LA, Gao W, Higginson IJ, Smith M, Davies JM, Ellis-Smith C, et al. Emergency department attendance by patients with cancer in their last month of life: a systematic review and meta-analysis. J Clin Oncol. 2015;33(4):370–6.
Verhoef MJ, de Nijs E, Horeweg N, Fogteloo J, Heringhaus C, Jochems A, et al. Palliative care needs of advanced cancer patients in the emergency department at the end of life: an observational cohort study. Support Care Cancer. 2020;28(3):1097–107.
Mayer DK, Travers D, Wyss A, Leak A, Waller A. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol. 2011;29(19):2683–8.
Giezendanner S, Bally K, Haller DM, Jung C, Otte IC, Banderet HR, et al. Reasons for and frequency of end-of-life hospital admissions: general practitioners’ perspective on reducing end-of-life hospital referrals. J Palliat Med. 2018;21(8):1122–30.
Kjellstadli C, Allore H, Husebo BS, Flo E, Sandvik H, Hunskaar S. General practitioners’ provision of end-of-life care and associations with dying at home: a registry-based longitudinal study. Fam Pract. 2020;37(3):340–7.
Henson LA, Gomes B, Koffman J, Daveson BA, Higginson IJ, Gao W. Factors associated with aggressive end of life cancer care. Support Care Cancer. 2016;24(3):1079–89.
Andersen ER, Brandsæter I, Hofmann BM, Kjelle E. The use of low-value imaging: the role of referral practice and access to imaging services in a representative area of Norway. Insights Imaging. 2023;14(1):29.
Wong TH, Lau ZY, Ong WS, Tan KB, Wong YJ, Farid M, et al. Cancer patients as frequent attenders in emergency departments: a national cohort study. Cancer Med. 2018;7(9):4434–46.
Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. 2013;61(2):209–14.
Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55(2):189–94.
Garrido MM, Balboni TA, Maciejewski PK, Bao Y, Prigerson HG. Quality of life and cost of care at the end of life: the role of advance directives. J Pain Symptom Manage. 2015;49(5):828–35.
Funding
Open access funding provided by OsloMet - Oslo Metropolitan University The study was funded by Østfold Hospital Trust.
Author information
Authors and Affiliations
Contributions
A.S. and J.S. acquired and analyzed the data. M.T. contributed to the analysis. A.S. and E.K.G. supervised the project. While J.S. wrote the main manuscript text, A.S. and E.K.G. reviewed and edited the manuscript’s first versions. All authors contributed to the interpretation of data and critically revised the final manuscript. The authors have read and approved the manuscript to be published and have agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was evaluated and approved by the Data Protection Official at the hospital. The Regional Committee of Ethics in Norway evaluated this register data study and found it not to be within the mandate of the Norwegian Health legislation (# 593639, 05/15/2023). Informed consent was waived after assessment and approval by the Data Protection Official at The Østfold Hospital Trust (Data Protection Official, dated 13.02.2020). The study was carried out in accordance with relevant guidelines and regulations. The STROBE guidelines were utilized.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Singh, J., Grov, E.K., Turzer, M. et al. Hospitalizations and re-hospitalizations at the end-of-life among cancer patients; a retrospective register data study. BMC Palliat Care 23, 39 (2024). https://doi.org/10.1186/s12904-024-01370-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-024-01370-1