Abstract
Background
Provision of paediatric palliative care for children with life-threatening or life-limiting conditions and their families is often complex. Guidelines can support professionals to deliver high quality care. Stakeholders expressed the need to update the first Dutch paediatric palliative care guideline with new scientific literature and new topics. This paper provides an overview of the methodology that is used for the revision of the Dutch paediatric palliative care guideline and a brief presentation of the identified evidence.
Methods
The revised paediatric palliative care guideline was developed with a multidisciplinary guideline panel of 72 experts in paediatric palliative care and nine (bereaved) parents of children with life-threatening or life-limiting conditions. The guideline covered multiple topics related to (refractory) symptom treatment, advance care planning and shared-decision making, organisation of care, psychosocial care, and loss and bereavement. We established six main working groups that formulated 38 clinical questions for which we identified evidence by updating two existing systematic literature searches. The GRADE (CERQual) methodology was used for appraisal of evidence. Furthermore, we searched for additional literature such as existing guidelines and textbooks to deal with lack of evidence.
Results
The two systematic literature searches yielded a total of 29 RCTs or systematic reviews of RCTs on paediatric palliative care interventions and 22 qualitative studies on barriers and facilitators of advance care planning and shared decision-making. We identified evidence for 14 out of 38 clinical questions. Furthermore, we were able to select additional literature (29 guidelines, two textbooks, and 10 systematic reviews) to deal with lack of evidence.
Conclusions
The revised Dutch paediatric palliative care guideline addresses many topics. However, there is limited evidence to base recommendations upon. Our methodology will combine the existing evidence in scientific literature, additional literature, expert knowledge, and perspectives of patients and their families to provide recommendations.
Similar content being viewed by others
Background
In the Netherlands, each year 5000 to 7000 children aged 0 to 18 years are suffering from life-threatening or life-limiting conditions [1]. In 2021, 983 children, adolescents and young adults aged 0 to 20 years died due to the consequences of these conditions [2]. Although these numbers seem small, the impact of these diseases for children and their families involved, is immeasurable. All these children and their families need paediatric palliative care.
Paediatric palliative care is a specialty that encompasses the care of all children with life-threatening or life-limiting conditions regardless of their diagnosis or stage of disease [3]. The World Health Organization (WHO) defines paediatric palliative care as the prevention and relief of suffering of paediatric patients and their families, facing problems associated with life-threatening or life-limiting conditions [4]. These problems include the physical, psychological, social and spiritual suffering of children and the psychological, social and spiritual suffering of family members [4]. Thus, paediatric palliative care relates not only to the child but to the whole family [5].
Both health care providers and parents face multiple challenges in providing the best paediatric palliative care, as it is a complex trajectory where curative and palliative care intertwine. Additionally, the child continues to develop physically, emotionally and cognitively which contributes to many varieties in the child’s communication skills and ability to understand the condition [5]. Since the number of children living with life-threatening or life-limiting conditions is small and many conditions are extremely rare or specific to childhood, there is only limited knowledge on paediatric palliative care [5].
To ensure that all children in need of palliative care receive high quality care, clinical practice guidelines (CPGs) are needed. Care consistent with CPGs has led to more efficient care delivery and improved patient outcomes [6,7,8]. Therefore, the Dutch multidisciplinary CPG for paediatric palliative care was developed in 2013. This CPG provides recommendations on symptom relief, decision-making and organisation of care. Several years after the development of the first national CPG, stakeholders expressed a need to update this CPG with newly published evidence and to include new topics, specifically delirium, palliative sedation, restriction of hydration and nutrition in case of palliative sedation, advance care planning, shared decision-making, psychosocial care, and loss and bereavement. As a result, the revision of the first Dutch CPG for paediatric palliative care was initiated.
This article provides an overview of the methodology for this revision of the Dutch CPG for paediatric palliative care and provides a brief presentation of the identified evidence. In subsequent manuscripts we will discuss the evidence and recommendations on (1) treatment of symptoms including refractory symptoms, (2) advance care planning, shared decision-making, and organisation of care and (3) psychosocial care, and loss and bereavement.
Methods
Aim and scope
The aim of this CPG is to provide guidance on all aspects of palliative care including physical, psychological, social, and spiritual aspects, for all children aged 0 to 18 years with life-threatening or life-limiting conditions and their caregivers, brothers, and sisters (hereafter referred to as families) throughout the entire palliative trajectory (from palliative diagnosis till after end-of-life), with the ultimate goal to improve quality of paediatric palliative care. This CPG is intended for all health care providers from different specialisms who are involved in paediatric palliative care and for all children aged 0 to 18 years with life-threatening or life-limiting conditions and their families.
The guideline is an update of the first CPG for paediatric palliative care that was published in 2013, which provided recommendations on symptom relief, decision making and organisation of care.
Topic selection
In 2018, an invitational conference among experts in paediatric palliative care was convened to evaluate the first CPG for paediatric palliative care and identify new topics that needed to be addressed. This formed the basis for the online survey that was conducted among 89 health care providers to prioritize new topics (Appendix A). In this survey, professionals were asked to weigh topics that should be included during the revision of the CPG on a 5-point Likert scale that ranged from not important to very important. In addition, another survey was conducted among patient representatives and mostly bereaved parents of children with life-threatening or life-limiting conditions (n = 16) to indicate their priorities towards the identified topics in the invitational conference (Appendix B).
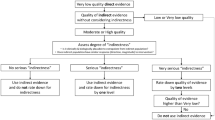
Multiple suggestions for new topics were derived from the results of the invitational conference and surveys. A preliminary topic list was generated which included topics covered in the CPG of 2013 (n = 12) and the suggestions for new topics (n = 8). The core group made a final selection based on practical and financial feasibility, and priorities of professionals, and patient and parent representatives. This resulted in a final list of 16 topics of which five topics were newly added. Figure 1 shows the selection process including reasons for exclusion of topics.
Process of topic selection
a Topics covered in the CPG for paediatric palliative care 2013 are: anxiety and depression; dyspnoea; haematological symptoms; coughing; skin complaints; nausea and vomiting; neurological symptoms; pain; death rattle; fatigue; decision making; and organisation of care. b Suggestions for topics identified in the invitational conference and surveys are: delirium; refractory symptoms; psychosocial care; loss and bereavement; advance care planning; practicing communication skills; financing; and complementary care. c Reasons for removal from topic list are: practicing communication skills and financing are outside the scope of this CPG; and, complementary care will be covered in another CPG. d Topics covered in the revised CPG for paediatric palliative care are: anxiety and depression; delirium; dyspnoea; haematological symptoms; coughing; skin complaints; nausea and vomiting; neurological symptoms; pain; death rattle; fatigue; refractory symptoms; advance care planning and shared decision making; organisation of care; psychosocial care; and loss and bereavement. e Newly added topics are: delirium; refractory symptoms; advance care planning and shared decision making; psychosocial care; and loss and bereavement. f Topics of which the content will be refined: anxiety and depression; dyspnoea; haematological symptoms; coughing; skin complaints; nausea and vomiting; neurological symptoms; pain; death rattle; fatigue; and organisation of care
Multidisciplinary guideline development panel
A guideline development panel was established which consisted of 72 experts in paediatric palliative care and nine (bereaved) parents (see representation of patients and their families). Professionals from various disciplines such as paediatricians, paediatric oncologists, neurologists, anaesthesiologists, nurses, psychologists, pharmacists, medical pedagogical care providers and researchers, were included in the expert panel. Each working group (WG) consisted of members with expertise knowledge relevant to the specific topic addressed (Appendix C). The WG members were selected based on their experience with paediatric palliative care, of whom some had specific certified training in paediatric palliative care. The Netherlands Comprehensive Cancer Organisation recruited the panel members. Members were either mandated by their professional associations or participated on personal title. All members disclosed conflicts of interest at the start and end of the guideline development process.
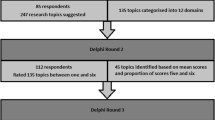
Based on the final selection of topics, six main WGs were formed. These WGs focused on symptom treatment (WG1), refractory symptom treatment (WG2), advance care planning and shared decision-making (WG3), organisation of care (WG4), psychosocial care (WG5), and loss and bereavement (WG6). Sub-WGs were established for WGs that covered multiple topics. Figure 2 provides a full overview of the (sub)WGs. The members of the expert panel were appointed to the (sub)WGs according to their expertise. Moreover, a core group was established to ensure consistency and transparency throughout the guideline. An overview of the working structure and guideline development process is shown in Appendix D and E.
Representation of patients and their families
Different methods were used to ensure representation of patients and their families. First, we conducted a survey to identify patient priorities for topic selection. Second, two members of the core group were dedicated to ensure the representation of patients and their families during the entire guideline process. Third, a panel consisting of nine (bereaved) parents of children with life-threatening or life-limiting conditions was established to review guideline texts and recommendations (Appendix C). We ensured the panel represented a broad spectrum of experiences regarding paediatric palliative care by including parents of children with a variety of palliative conditions, age, and stage of disease (currently receiving palliative care or deceased). The parents were recruited by the Child and Hospital Foundation and attended a short training on guideline development.
The panel reviewed the first drafts of all guideline texts and recommendations. Additionally, the panel reviewed the complete concept guideline to ensure their input was incorporated correctly. Lastly, parents were asked to share their experiences during the interactive conference for organisation of care (WG4) (see consensus-based approach).
Formulation of clinical questions
Each (sub-)WG proposed several clinically relevant questions. Questions were developed according to the PICOS format, which defines the patient group, intervention, comparison to the intervention, relevant outcomes, and study design for each clinical question. The core group assessed all clinical questions carefully. If necessary, clinical questions were adjusted. The core group sent the final clinical questions to the (sub-)WGs for approval.
Below we describe the methods used to answer the clinical questions. In Table 1, an overview of the methods used per WG is presented.
Identification of evidence – quantitative studies
Systematic literature search
WG1 to WG6 formulated a total 37 clinical questions related to the effect of paediatric palliative care interventions (Appendix F).
We updated the systematic literature search of the former CPG (which searched from 1970 to 2011) [9] to identify new studies on paediatric palliative care. All originally included studies were also included in the revised CPG. We searched for studies published from January 1, 2010 to January 24, 2020 (initial search October 5, 2018; top-up search, January 24, 2020), in the databases Ovid MEDLINE and PreMEDLINE, MEDLINE (PubMed), CENTRAL and the Cochrane Database of systematic reviews using a combination of the search terms “child”, “palliative care”, “randomized controlled trial” and “systematic review” (Appendix G).
The following inclusion criteria were defined: (1) randomized controlled trials (RCTs), controlled clinical trials (CCTs) including at least 10 patients and systematic reviews (SRs) of RCTs, (2) study population consisting of children aged 0 to 18 with life-threatening conditions and life-limiting conditions (according to the definition of the WHO [4]); at least 75% of the study population should be aged 0 to 18 years, (3) paediatric palliative care interventions related to (a) treatment of anxiety and depression, delirium, dyspnoea, haematological symptoms, coughing, skin complaints, nausea and vomiting, pain, neurological symptoms and fatigue, (b) treatment of refractory symptoms, (c) advance care planning and shared decision-making, (d) organisation of care, (e) psychosocial care, and (f) loss and bereavement. Only studies published in English or Dutch language were included. Studies that described interventions on complementary or alternative medicine were excluded (Appendix H).
We searched for eligible studies in reference lists of included studies and identified SRs, guidelines, and textbooks. Moreover, we asked WG members to provide eligible studies.
Study selection
The studies were selected through two rounds of screening, title/abstract screening, and full text screening. One independent reviewer screened the titles and/or abstracts of all citations. The full text screening was performed by one independent reviewer. In case of doubt, the citations were discussed in the core group and were included only if there was consensus. The selected citations were distributed among the WGs. When citations were relevant for multiple WGs, they were included in all relevant WGs.
Summary and appraisal of evidence
All studies were summarized in evidence tables. Evidence tables described study characteristics (study type, setting, duration and years), participant characteristics (number and diagnosis of participants, age, and sex), intervention and control characteristics, outcomes and results, and strengths, limitations, and study quality.
We determined individual study quality by assessing risk of bias according to the criteria of Cochrane Risk of Bias tool [10]. This tool assesses risk of selection bias, attrition bias, detection bias and performance bias of each study. Risk of bias can be classified as either low, high, or unclear.
We categorized evidence by outcome measures in summary of findings tables for every clinical question. We then formulated conclusions of evidence for each outcome measure. We assessed the quality of the total body of evidence with the Grading Recommendation Assessment Development and Evaluation (GRADE) criteria [11]. The GRADE appraisal was performed by two reviewers. Quality of evidence was downgraded if study limitations, inconsistency, indirectness, imprecision, or publication bias were present. Quality of evidence was upgraded if a dose response effect or large magnitude of effect was identified.
Identification of evidence – qualitative studies
Systematic literature search
WG3 (advance care planning and shared decision-making) formulated one clinical question on barriers and facilitators of advance care planning and shared decision-making (Appendix F). We performed a systematic literature search to identify qualitative studies on barriers and facilitators for advance care planning and shared decision-making. We updated the literature search that was conducted in the guideline ‘End of life care for infants, children and young people with life-limiting conditions (2016)’ of the National Institute for Health and Care Excellence (NICE) [12]. We searched Medline (PubMed) from January 1, 2016 to September 16, 2020 using the search terms “child”, “palliative care”, “advance care planning”, “shared decision-making”, “qualitative study” (Appendix G).
The following inclusion criteria were defined: (1) qualitative studies, mixed-methods observational studies with qualitative data and SRs of qualitative studies, (2) study population consisting of children aged 0 to 18 years old with life-threatening or life-limiting conditions, their parents and health care providers, (3) study outcomes were barriers and facilitators on advance care planning or shared decision-making. Moreover, only studies published in English or Dutch language were included (Appendix H).
We asked WG members to provide eligible studies and searched for eligible studies in identified SRs and guidelines on barriers facilitator for advance care planning and shared decision-making.
Study selection
Both title/abstract screening and full text screening were performed by two independent reviewers. One reviewer performed title/abstract screening and full text screening for all identified citations. For the second review, citations were divided among eight WG members. In case of doubt, citations were discussed in the core group and included only if there was consensus.
Summary and appraisal of evidence
All studies were summarized in evidence tables. Evidence tables described study characteristics (study type, objective, setting, duration, and years), participant characteristics (number and diagnosis of participants, age, sex, ethnicity, religious preference, and level of education), outcomes and results, and strengths, limitations, and study quality.
We determined individual study quality by assessing the methodological limitations according to the criteria of Critical Appraisal Skills Programme (CASP) checklist tool [13]. This tool assesses the aim and appropriateness of the qualitative study design, rigor in study design, sample selection, data collection, data analysis and results. Methodological limitations are classified as low, high, or unclear.
We assessed the quality the total body of evidence with the adapted GRADE Confidence in the Evidence from Reviews of Qualitative research (GRADE CERQual) methodology [14]. The GRADE CERQual appraisal was performed by two reviewers. Quality of evidence was downgraded if methodological limitations were present or if there was a lack of coherence, relevance or data saturation [15]. Quality of each conclusion of evidence was classified as high, moderate, low, or very low.
Identification of additional literature
As the expectation was that the systematic searches would yield little to no evidence, we searched for additional literature.
For all WGs, we searched for guidelines on paediatric palliative care, general paediatrics, and adult palliative care. To identify relevant (inter)national guidelines on paediatric palliative care, general paediatrics, and adult palliative care, we searched multiple databases. We searched the Guideline International Network database from 2010 to January 24, 2020, using the search terms “child” and “palliative care”, to identify guidelines on paediatric palliative care. Furthermore, we searched databases of the NICE, International Paediatric Oncology Guidelines in supportive care network (iPOG), the Dutch Association for Paediatrics, and Pallialine to identify guidelines on paediatric palliative care, general paediatrics, and adult palliative care. Guideline panel members were also asked to supply additional guidelines (Appendix G).
For the selection of guidelines, our first choice was to include(inter)national guidelines on paediatric palliative care. If guidelines on paediatric palliative care were not available, we included guidelines on general paediatrics if deemed relevant such as for topics related to (refractory) symptom treatment. We only included guidelines on adult palliative care, if no (relevant) guidelines on paediatric palliative care or guidelines on general paediatrics were identified (Appendix H). Throughout the guideline process, we manually checked for all selected guidelines if more recent versions were available.
In case we did not find recommendations from guidelines on paediatric palliative care, general paediatrics, or adult palliative care, we included two textbooks on paediatric palliative care to refine considerations and recommendations. Since most topics were covered in recommendations from selected guidelines, we only used the textbooks for WG1 (symptom treatment) and WG2 (refractory symptom treatment).
Lastly, we derived SRs of observational, qualitative, or mixed-method studies from the systematic literature search on paediatric palliative care and through referencing. The inclusion of these SRs was only considered relevant for WG6 (loss and bereavement). We summarized the results of the SRs in evidence tables and translated these into conclusions of evidence. As the results of SRs included multiple studies from multiple study designs, we were not able to determine individual study quality nor the quality of the total body of evidence. The formulated conclusions were used to base recommendations upon.
Consensus-based approach
We found that not all included clinical questions in the revised CPG could be appropriately answered through an evidence-based approach, as some questions were considered as highly specific to the Dutch context. In particular, WG4 (organisation of care) formulated clinical questions that focused on issues specific to the Dutch health care system and professional roles and institutions within this system (for example, methods to assist the general practitioner and other health care providers in improving continuity of paediatric palliative care at home). Therefore, an Ideafactory was organized. This is an interactive conference with a competitive element that is designed to find the best solutions for problems (formulated as questions). These solutions were used as the basis for formulating the recommendations. The methods and results will be presented in a subsequent manuscript.
Formulation of recommendations
When formulating recommendations, several factors were taken into account: (1) the quality of the evidence (the higher the quality, the more likely it is to formulate a strong recommendation), (2) additional literature, (3) patient perspectives (values and needs), (4) professional perspectives (clinical expertise, values and needs), (5) acceptability (legal and ethical considerations), (6) feasibility (sufficient time, knowledge and manpower) and (7) benefits versus harms of the interventions.
For each clinical question, WG members described the relevant considerations. Decisions were made through group consensus. The strength of each recommendation was graded according to published evidence-based methods [16, 17] (Appendix I). Recommendations were categorised as strong to do (green), moderate to do (yellow) or strong not to do (red). A strong recommendation reflected a high degree of certainty. Moderate recommendations have a higher degree of uncertainty, therefore factors such as the clinical expertise, the patients and family’s situation and preferences, feasibility and relevant harms and benefits need to be considered.
All recommendations were supported unanimously by the core group, WG members, and parent representatives.
Results
Identification of quantitative studies
For the 37 formulated clinical questions on paediatric palliative care interventions of WG1 to WG6, the updated systematic literature search yielded 5078 citations. A total of 4337 citations were excluded based on title/abstracts and 168 citations were included for full text screening. Main reasons for exclusion of full texts were wrong study design (other than RCTs, CCTs or SRs) or wrong study population (other than children in the palliative setting).
A total of 29 studies (25 RCTs and 4 SRs of RCTs) were eligible for inclusion. This included 11 RCTs that were identified in the previous CPG of 2013 and 18 newly published studies (Appendix J). We subsequently categorized all 29 citations according to topic. Then, we distributed the citations among the different WGs. Figure 3 shows a flow diagram of the study selection process.
Identification of qualitative studies
For the formulated clinical question on barriers and facilitators of advance care planning and shared decision-making of WG3, the updated systematic literature search yielded 1232 eligible studies. A total of 1147 citations were excluded based on title/abstract and 85 citations were included for full text screening. Main reasons for exclusion of full texts were wrong study subject (no advance care planning or shared decision-making), wrong study design, or wrong study outcome (no barriers and facilitators).
A total of 33 studies on barriers and facilitators of advance care planning and shared decision-making were included. This included 22 newly published qualitative studies and 11 qualitative studies that were identified in the search of the NICE-guideline ‘End of life care for infants, children and young people with life-limiting conditions (2016)’ [12] (Appendix J). We used the conclusions of evidence of the 11 included studies in the NICE guideline and integrated these in our conclusions of evidence. Figure 4 shows a flow diagram of the selection process.
Identification of additional literature
The search for guidelines identified 378 potential CPGs. In total, we included 29 CPGs of which 6 were paediatric palliative care CPGs, 11 were general paediatric CPGs and 12 were adult palliative care CPGs (Appendix J). Moreover, we included two textbooks on paediatric palliative care.
In addition, we included 10 SRs of observational, qualitative, or mixed-method studies on bereavement intervention components and features of communication strategies.
Evidence base
Table 2 gives an overview of the selected studies from the systematic literature searches and selected additional literature per WG and clinical question. The systematic literature searches identified studies for 14 out of 38 formulated clinical questions, meaning that for 24 clinical questions the systematic literature searches identified no evidence. The number of identified studies from the systematic literature searches differed per WG and clinical question. Moreover, we were able to select additional literature, namely guidelines, textbooks, or SRs of observational, qualitative, or mixed-method studies for almost every clinical question.
Discussion
Over the years, significant progress has been made in improving and integrating paediatric palliative care in the Netherlands [109]. The first Dutch CPG for paediatric palliative care contributed to the quality and organisation of palliative care for children with life-threatening and life-limiting conditions [109]. Several years after the development of the first Dutch CPG for paediatric palliative care, health care providers, parents, and other stakeholders expressed the need for more guidance on specific topics that were not covered in the first CPG (such as palliative sedation and forgoing hydration and nutrition). This, together with the need to review evidence and build a stronger evidence-base from scientific literature, inspired the revision of the Dutch CPG for paediatric palliative care.
In this paper, we provide a complete overview of our methodology to revise the Dutch CPG for paediatric palliative care and give a brief presentation of the identified evidence. By sharing our methodology, we hope to promote transparency in CPG development and support others in developing approaches which we used to deal with expected challenges (multiple topics, lack of evidence, improve applicability and implementation) and unexpected challenges (high workload).
First, we used an evidence-based approach to revise the Dutch CPG for paediatric palliative care. We expected this would be challenging, as we chose to include a total of 38 clinical questions covering 16 topics related to paediatric palliative care. Therefore, we developed an approach that prevented unmanageable amounts of work without compromising quality. We decided to update existing systematic literature searches and mainly focus on high quality evidence. For all clinical questions on paediatric palliative care interventions, we updated the systematic literature search that was used in the first CPG to identify quantitative evidence (RCTs/CCTs and SRs of RCTs) on all paediatric palliative care interventions. For the clinical question on barriers and facilitators of advance care planning and shared decision-making, we updated the systematic literature search to identify qualitative evidence. This search was originally developed by the NICE guideline ‘End of life care for infants, children and young people with life-limiting conditions: planning and management’ [12]. By re-using evidence from previous systematic literature searches and combine it with new identified evidence, we were able to formulate a large set of recommendations.
Additionally, we developed an approach to deal with the lack of evidence. As the systematic literature search that was conducted for the first CPG identified little evidence, we expected a lack of evidence for the update as well. To deal with this challenge, we decided to search for additional literature sources to base recommendations upon. We used textbooks on paediatric palliative care, and guidelines on paediatric palliative care, general paediatrics, and adult paediatric palliative care and SRs of observational, qualitative, or mixed-method studies. Additional literature was selected according to its relevance.
Moreover, as stakeholders expressed a need for more guidance on certain topics related to paediatric palliative care, we created an approach to further improve applicability as well as implementation of this guideline. Therefore, we decided to not only focus on physical aspects (symptom relief), decision-making, and organisation of care but also on other topics such as advance care planning, psychological, social, and spiritual support, and loss and bereavement. These topics are increasingly recognised as important within paediatric palliative care [109]. Furthermore, the selected topics are based on priorities of health care providers and parents. As a result, we believe this increases the likelihood that the recommendations of this guideline will be applied in practice.
To further improve dissemination and implementation of the guideline, we collaborated with many stakeholders including health care providers from multiple disciplines and parent representatives. It has been shown that patient values improve quality of CPGs and is invaluable [110]. Therefore, parent representatives have been involved in different ways throughout the entire guideline process, which ensures representation of patients and their families. Additionally, this guideline is approved by all relevant professional and patient associations in the Netherlands, meaning that these associations consider the CPG as a standard for provision of paediatric palliative care. Ultimately, we believe that this approach will lead to increased dissemination and implementation of the revised CPG among health care providers, parents, and children.
The revision of this guideline entailed a significantly greater amount of effort than we initially anticipated due to time-intensive tasks such as the selection and appraisal of evidence, and instruction and motivation of all guideline panel members. We appointed one researcher who coordinated the entire guideline development process on a fulltime basis for more than three years. This approach turned out to be very beneficial as it improved collaboration between all guideline panel members and contributed to a smooth process as issues were timely addressed. We therefore highly recommend others to adopt this approach, especially in situations where lack of time and resources might be an issue.
Unfortunately, despite our efforts to deal with (un)expected challenges, we found that there are still many knowledge gaps in paediatric palliative care for children. We identified no evidence for 24 out of 38 clinical questions, mainly including questions on (refractory) symptoms. It should be noted that we included evidence from 1970 to 2020. Therefore, it is plausible that we missed some recently published evidence. However, based on the little studies we found in a large time frame; it is plausible we miss only a small number of studies that most likely will not have a direct influence on our identified knowledge gaps. As a result, we emphasize the need for more high-quality research on paediatric palliative care interventions to further improve quality of care.
Furthermore, we acknowledge that we describe the methodology of a national CPG for paediatric palliative care. Although we use international evidence, our recommendations will be largely based on national clinical expertise and patient experiences due to identified knowledge gaps. Based on our previous experiences, we believe that the targeted recommendations we will provide in this guideline, will positively influence the further integration of paediatric palliative care in the Netherlands. Moreover, as we used international evidence, we believe that a large proportion of provided recommendations, except recommendations that are specific for the Dutch context (organisation of care), will be applicable to other contexts and can be of great added value. Especially, since we provide a comprehensive set of recommendations for all children and their families in need of palliative care from beginning of diagnosis till after the-end-life. However, country-specific factors such as availability of (non)pharmacological interventions, infrastructure, financial resources, and cultural backgrounds, should always be carefully considered before applying any recommendations in other contexts.
Conclusions
We developed a transparent evidence-based methodology for the revision of the Dutch CPG for paediatric palliative care. Within this methodology, we developed approaches to deal with lack of evidence and improve applicability of the guideline by incorporating patient and family values and experiences throughout the entire guideline process. Our methodology combines existing evidence from scientific literature, additional literature, expert knowledge, and perspectives of patients and their families to formulate recommendations on all domains of paediatric palliative care (medical, psychological, social, and spiritual care). By using this methodology, we aim to develop the most comprehensive evidence-based guideline in paediatric palliative care.
Availability of data and materials
All data analysed during this study is included in this published article and Additional information file 1.
Abbreviations
- CASP:
-
Critical Appraisal Skills Programme
- CPG:
-
Clinical Practice Guideline
- CCT:
-
Controlled Clinical Trial
- CENTRAL:
-
Cochrane Central Register of Controlled Trials
- GRADE:
-
Grading Recommendation Assessment Development and Evaluation
- GRADE CERQual:
-
Grading Recommendation Assessment Development and Evaluation Confidence in the Evidence from Reviews of Qualitative research
- iPOG:
-
International Paediatric Oncology Guidelines in supportive care
- MEDLINE:
-
Medical Literature Analysis and Retrieval System Online
- NICE:
-
National Institute of Health Care Excellence
- PICOS:
-
Patient, Intervention, Comparison, Outcomes, Study design
- RCT:
-
Randomized Controlled Trial
- SR:
-
Systematic Review
- WG:
-
Working Group
- WG1:
-
Working group 1: Symptom treatment
- WG2:
-
Working group 2: Refractory symptom treatment
- WG3:
-
Working group 3: Advance care planning and shared decision making
- WG4:
-
Working group 4: Organisation of care
- WG5:
-
Working group 5: Psychosocial care
- WG6:
-
Working group 6: Loss and bereavement
- WHO:
-
World Health Organization
References
Kenniscentrum kinderpalliatieve zorg. Wist U dat?. 2019. Available from: https://kinderpalliatief.nl/over-kinderpalliatieve-zorg/wat-is-kinderpalliatieve-zorg/kinderpalliatieve-zorg. Updated 2019, March 26; Cited 2021 July 21.
Centraal Bureau voor Statistiek. Overledenen; Doodsoorzaak (uitgebreide lijst), leeftijd, Geslacht. Statline; 2022. Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/7052_95/table?ts=1662990503553. Updated 2022, Dec 20; Cited 2023 Feb 22.
Fraser LK, Bluebond-Langner M, Ling J. Advances and challenges in European Paediatric Palliative Care. Med Sci. 2020;8(2):20.
World Health Organization. Integrating palliative care and symptom relief into paediatrics: a WHO guide for health-care planners, implementers and managers. 2018.
Chambers L. A Guide to Children’s Palliative Care. 4th ed. Bristol: Together for Short Lives; 2018. Available from: (https://www.togetherforshortlives.org.uk/wp-content/uploads/2018/03/TfSL-A-Guide-to-Children%E2%80%99s-Palliative-Care-Fourth-Edition-FINAL-SINGLE-PAGES.pdf). Cited 2021 July 21.
Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342(8883):1317–22.
Lugtenberg M, Burgers JS, Westert GP. Effects of evidence-based clinical practice guidelines on quality of care: a systematic review. Qual Saf Health Care. 2009;18(5):385–92.
Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8(6):iii–iv.
Knops RR, Kremer LC, Verhagen AA, Dutch Paediatric Palliative Care Guideline Group for S. Paediatric palliative care: recommendations for treatment of symptoms in the Netherlands. BMC Palliat Care. 2015;14:57.
Higgins JP, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions 2022. Available from: https://training.cochrane.org/handbook.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
National Institute for Health and Care Excellence. End of life care for infants, children and young people with life-limiting conditions: planning and management. London: NICE; 2016. (Available from: https://www.nice.org.uk/guidance/ng61). Cited 2021 March 1.
CASP. Critical Appraisal Skills Programme (CASP), (Qualitative checklist). 2018 . Available from: https://casp-uk.net/casp-tools-checklists/. Cited 2022 January.
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(Suppl 1):2.
Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for Health and Social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLoS Med. 2015;12(10): e1001895.
Gibbons RJ, Smith S, Antman E. American College of Cardiology/American Heart Association clinical practice guidelines: part I: where do they come from? Circulation. 2003;107(23):2979–86.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454): 1490.
Bolier L, Speetjens P, Volker D, Sinnema H. JGZ-Richtlijn Angst: Nederlands Centrum Jeugdgezondheid; 2016 [cited 2021 July 13]. Available from: https://www.ncj.nl/richtlijnen/alle-richtlijnen/richtlijn/angst.
Oud M, van der Zanden R, Coronenberg I, Sinnema H. JGZ-richtlijn Depressie [Internet]: Nederlands Centrum Jeugdgezondheid; 2016 [cited 2021 July 13]. Available from: https://www.ncj.nl/richtlijnen/alle-richtlijnen/richtlijn/depressie.
National Institute for Health and Care Excellence. Care of dying adults in the last days of life. [Internet]. London: NICE; 2015 [cited 2021 March, 1]. Available from: https://www.nice.org.uk/guidance/ng31.
National Institute for Health Care and Excellence. Depression in Children and Young People: identification and mangement. [Internet]. London: NICE; 2019 [cited 2021 March 1]. Available from: https://www.nice.org.uk/guidance/NG134.
Goldman A, Hain R, Liben S. Oxford Textbook of Palliative Care for Children. 2nd ed. Oxford: Oxford University Press; 2012.
Nederlandse Vereniging voor Psychiatrie. Multidisciplinaire richtlijn pediatrisch delier (PD) en emergence delier (ED) 2021 [cited 2022 June 1]. Available from: https://richtlijnendatabase.nl/richtlijn/pediatrisch_delier_pd_en_emergence_delier_ed/startpagina_-_pediatrisch_delier_pd_en_emergence_delier_ed.html.
de Jong W, van Aalderen WM, Kraan J, Koeter GH, van der Schans CP. Inspiratory muscle training in patients with cystic fibrosis. Respir Med. 2001;95(1):31–6.
Lima CA, Andrade Ade F, Campos SL, Brandao DC, Fregonezi G, Mourato IP, et al. Effects of noninvasive ventilation on treadmill 6-min walk distance and regional chest wall volumes in cystic fibrosis: randomized controlled trial. Respir Med. 2014;108(10):1460–8.
Integraal Kankercentrum Nederland. Dyspneu in de palliatieve fase (3.0). 2015. Available from: https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/dyspneu.
Büyükpamukçu M, Varan A, Kutluk T, Akyüz C. Is epoetin alfa a treatment option for chemotherapy-related anemia in children? Med Pediatr Oncol. 2002;39(4):455–8.
Razzouk BI, Hord JD, Hockenberry M, Hinds PS, Feusner J, Williams D, et al. Double-blind, placebo-controlled study of quality of life, hematologic end points, and safety of weekly epoetin alfa in children with cancer receiving myelosuppressive chemotherapy. J Clin Oncol. 2006;24(22):3583–9.
Wolfe J, Hinds P. Textbook of Interdisciplinary Pediatric Palliative Care: Saunders; 2011.
Federatie Medisch Specialisten. Bloedtransfusiebeleid 2019. Available from: https://richtlijnendatabase.nl/richtlijn/bloedtransfusiebeleid/startpagina_-_bloedtransfusiebeleid.html.
Nederlandse vereniging voor kindergeneeskunde. Erytrocytentransfusies bij kinderen & neonaten met kanker [internet]2022. Available from: https://richtlijnendatabase.nl/richtlijn/erytrocytentransfusies_bij_kinderen_neonaten_met_kanker/startpagina_-_erytrocytentransfusies.html#:~:text=Erytrocytentransfusies%20bij%20kinderen%20en%20neonaten%20met%20kanker%20in,-%20snelheden%20bij%20kinderen%20en%20neonaten%20met%20kanker.
Nederlandse Vereniging voor Kindergeneeskunde. Trombocytentransfusies bij kinderen met kanker [Internet]2022. Available from: https://richtlijnendatabase.nl/richtlijn/trombocytentransfusies_bij_kinderen_met_kanker/startpagina_-_trombocytentransfusies.html
Integraal Kankercentrum Nederland. Hoesten (2.0). 2010. Available from: https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/hoesten.
Integraal Kankercentrum Nederland. Richtlijn Jeuk in de palliatieve fase.2022 21–02–2022. Available from: https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/jeuk.
Integraal Kankercentrum Nederland. Oncologische Ulcera 2010. Available from:https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/oncologische-ulcera .
Nederlands Centrum Jeugdgezondheid. Huidafwijkingen, taakomschrijving en richtlijn voor de preventie, signalering, diagnnostiek, begeleiding, behandeling en verwijzing [Internet]2012 [cited 2021 May 1]. Available from: https://assets.ncj.nl/docs/d3452a1b-34b2-4154-8106-9977ef5426f3.pdf.
Verpleegkundigen & Verzorgenden Nederland. Smetten (Intertrigo) preventie en behandeling [Internet]2018 [cited 2021 January 19th]. Available from: https://www.venvn.nl/media/n0fppki5/richtlijn-smetten-september-2018.pdf.
Verpleegkundigen & Verzorgenden Nederland. Richtlijn Decubitus. 2021.
Maxwell LG, Kaufmann SC, Bitzer S, Jackson EVJ, McGready J, Kost-Byerly S, et al. The Effects of a Small-Dose Naloxone Infusion on Opioid-Induced Side Effects and Analgesia in Children and Adolescents Treated with Intravenous Patient-Controlled Analgesia: A Double-Blind, Prospective, Randomized. Controlled Study Anesthesia & Analgesia. 2005;100(4):953–8.
Jacknow DS, Tschann JM, Link MP, Boyce WT. Hypnosis in the prevention of chemotherapy-related nausea and vomiting in children: a prospective study. Journal of Developmental and Behavioral Pediatrics. 1994.
Dupuis LL, Robinson PD, Boodhan S, Holdsworth M, Portwine C, Gibson P, et al. Guideline for the prevention and treatment of anticipatory nausea and vomiting due to chemotherapy in pediatric cancer patients. Pediatr Blood Cancer. 2014;61(8):1506–12.
Integraal Kankercentrum Nederland. Misselijkheid en braken (4.0). 2014. Available from:https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/misselijkheid-braken .
Aksoylar S, Akman SA, Ozgenc F, Kansoy S. Comparison of tropisetron and granisetron in the control of nausea and vomiting in children receiving combined cancer chemotherapy. Pediatr Hematol Oncol. 2001;18(6):397–406.
Brock P, Brichard B, Rechnitzer C, Langeveld N, Lanning M, Söderhäll S, et al. An increased loading dose of ondansetron: a north European, double-blind randomised study in children, comparing 5 mg/m2 with 10 mg/m2. Eur J Cancer. 1996;32(10):1744–8.
Gore L, Chawla S, Petrilli A, Hemenway M, Schissel D, Chua V, et al. Aprepitant in adolescent patients for prevention of chemotherapy-induced nausea and vomiting: a randomized, double-blind, placebo-controlled study of efficacy and tolerability. Pediatr Blood Cancer. 2009;52(2):242–7.
Köseoglu V, Kürekçi A, Sorici Ü, Atay A, Özcan O. Comparison of the efficacy and side-effects of ondansetron and metoclopramide-diphenhydramine administered to control nausea and vomiting in children treated with antineoplastic chemotherapy: a prospective randomized study. Eur J Pediatr. 1998;157(10):806–10.
Orchard PJ, Rogosheske J, Burns L, Rydholm N, Larson H, DeFor TE, et al. A prospective randomized trial of the anti-emetic efficacy of ondansetron and granisetron during bone marrow transplantation. Biol Blood Marrow Transplant. 1999;5(6):386–93.
Parker RI, Prakash D, Mahan RA, Giugliano DM, Atlas MP. Randomized, double-blind, crossover, placebo-controlled trial of intravenous ondansetron for the prevention of intrathecal chemotherapy-induced vomiting in children. J Pediatr Hematol Oncol. 2001;23(9):578–81.
Riad W, Altaf R, Abdulla A, Oudan H. Effect of midazolam, dexamethasone and their combination on the prevention of nausea and vomiting following strabismus repair in children. Eur J Anaesthesiol. 2007;24(8):697–701.
Flank J, Robinson PD, Holdsworth M, Phillips R, Portwine C, Gibson P, et al. Guideline for the Treatment of Breakthrough and the Prevention of Refractory Chemotherapy-Induced Nausea and Vomiting in Children With Cancer. Pediatr Blood Cancer. 2016;63(7):1144–51.
National Institute for Health and Care Excellence. Spasticity in under 19s: Management. [Internet]. London: NICE; 2012 [cited 2021 March 1]. Available from:https://www.nice.org.uk/guidance/cg145.
National Institute for Health and Care Excellence. Epilepsies: diagnosis and management [Internet]. London2019 [cited 2021 March, 1]. Available from:https://www.nice.org.uk/guidance/cg137.
Nederlandse Vereniging van Revalidatieartsen. Cerebrale en/of spinale spasticiteit [Internet]: VRA; 2016 [cited 2021 July 9]. Available from: https://richtlijnendatabase.nl/richtlijn/cerebrale_en_of_spinale_spasticiteit/cerebrale_en_of_spinale_spasticiteit_-_startpagina.html.
Nederlandse Vereniging voor Neurologie. Epilepsie. 2020. Available from:https://richtlijnendatabase.nl/richtlijn/epilepsie/startpagina_-_epilepsie.html.
Copeland L, Edwards P, Thorley M, Donaghey S, Gascoigne-Pees L, Kentish M, et al. Botulinum toxin A for nonambulatory children with cerebral palsy: a double blind randomized controlled trial. J Pediatr. 2014;165(1):140–6 e4.
Olesch CA, Greaves S, Imms C, Reid SM, Graham HK. Repeat botulinum toxin-A injections in the upper limb of children with hemiplegia: a randomized controlled trial. Dev Med Child Neurol. 2010;52(1):79–86.
Eccleston C, Fisher E, Law E, Bartlett J, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2015(4):CD009660.
Joanna Briggs Institute. Effectiveness of non-pharmacological pain management in relieving chronic pain for children and adolescents. Best Practice: evidence-based information sheets for health professionals. 2010;14(17):1–4.
Beecham E, Candy B, Howard R, McCulloch R, Laddie J, Rees H, et al. Pharmacological interventions for pain in children and adolescents with life‐limiting conditions. Cochrane Database Syst Rev. 2015(3):CD010750.
Wiffen PJ, Cooper TE, Anderson AK, Gray AL, Gregoire MC, Ljungman G, et al. Opioids for cancer-related pain in children and adolescents. Cochrane Database Syst Rev. 2017;7:CD012564.
Integraal Kankercentrum Nederland. Zorg in de stervensfase (1.0). 2010. Available from: https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/stervensfase.
Integraal Kankercentrum Nederland. Vermoeidheid bij kanker in de palliatieve fase (3.0). 2019. Available from:Vermoeidheid bij kanker - Richtlijnen Palliatieve zorg (palliaweb.nl).
Nederlandse Vereniging voor Kindergeneeskunde. Somatisch onvoldoende verklaarde lichamelijke klachten (SOLK) bij kinderen 2019 [cited 2021, July 22]. Available from: https://assets.nvk.nl/p/491522/files/SOLK.pdf.
Integraal Kankercentrum Nederland. Richtlijn palliatieve sedatie 2022. Available from: https://palliaweb.nl/richtlijnen-palliatieve-zorg/richtlijn/palliatieve-sedatie.
Anderson A-K, Burke K, Bendle L, Koh M, McCulloch R, Breen M. Artificial nutrition and hydration for children and young people towards end of life: consensus guidelines across four specialist paediatric palliative care centres. BMJ Support Palliative Care. 2019:bmjspcare-2019–001909.
Lyon ME, D’Angelo LJ, Dallas RH, Hinds PS, Garvie PA, Wilkins ML, et al. A randomized clinical trial of adolescents with HIV/AIDS: pediatric advance care planning. AIDS Care. 2017;29(10):1287–96.
Lyon ME, Garvie PA, Briggs L, He J, Malow R, D’Angelo LJ, et al. Is it safe? Talking to teens with HIV/AIDS about death and dying: a 3-month evaluation of Family Centered Advance care (FACE) planning–anxiety, depression, quality of life. Hiv/aids (Auckland, NZ). 2010;2:27.
Lyon ME, Jacobs S, Briggs L, Cheng YI, Wang J. Family-centered advance care planning for teens with cancer. JAMA Pediatr. 2013;167(5):460–7.
Lyon ME, Jacobs S, Briggs L, Cheng YI, Wang J. A longitudinal, randomized, controlled trial of advance care planning for teens with cancer: anxiety, depression, quality of life, advance directives, spirituality. J Adolesc Health. 2014;54(6):710–7.
Beecham E, Oostendorp L, Crocker J, Kelly P, Dinsdale A, Hemsley J, et al. Keeping all options open: Parents’ approaches to advance care planning. Health Expect. 2017;20(4):675–84.
Cicero-Oneto CE, Valdez-Martinez E, Bedolla M. Decision-making on therapeutic futility in Mexican adolescents with cancer: a qualitative study. BMC Med Ethics. 2017;18(1):74.
Day E, Jones L, Langner R, Stirling LC, Hough R, Bluebond-Langner M. "We just follow the patients' lead": Healthcare professional perspectives on the involvement of teenagers with cancer in decision making. Pediatr Blood Cancer. 2018;65(3):e26898.
Edwards JD, Morris MC, Nelson JE, Panitch HB, Miller RL. Decisions around Long-term Ventilation for Children. Perspectives of Directors of Pediatric Home Ventilation Programs. Ann Am Thorac Soc. 2017;14(10):1539–47.
Edwards JD, Panitch HB, Nelson JE, Miller RL, Morris MC. Decisions for Long-Term Ventilation for Children. Perspectives of Family Members. Ann Am Thorac Soc. 2020;17(1):72–80.
Fahner J, Rietjens J, van der Heide A, Milota M, van Delden J, Kars M. Evaluation showed that stakeholders valued the support provided by the Implementing Pediatric Advance Care Planning Toolkit. Acta Paediatr. 2021;110(1):237–46.
Fahner JC, Tholking TW, Rietjens JAC, van der Heide A, van Delden JJM, Kars MC. Towards advance care planning in pediatrics: a qualitative study on envisioning the future as parents of a seriously ill child. Eur J Pediatr. 2020;179(9):1461–8.
Hein K, Knochel K, Zaimovic V, Reimann D, Monz A, Heitkamp N, et al. Identifying key elements for paediatric advance care planning with parents, healthcare providers and stakeholders: A qualitative study. Palliat Med. 2020;34(3):300–8.
Henderson A, Young J, Herbert A, Bradford N, Pedersen LA. Preparing Pediatric Healthcare Professionals for End-of-Life Care Discussions: An Exploratory Study. J Palliat Med. 2017;20(6):662–6.
Jack BA, Mitchell TK, O’Brien MR, Silverio SA, Knighting K. A qualitative study of health care professionals’ views and experiences of paediatric advance care planning. BMC Palliat Care. 2018;17(1):93.
Kelly KP, Mowbray C, Pyke-Grimm K, Hinds PS. Identifying a conceptual shift in child and adolescent-reported treatment decision making: "Having a say, as I need at this time". Pediatr Blood Cancer. 2017;64(4):e26262.
Lord S, Moore C, Beatty M, Cohen E, Rapoport A, Hellmann J, et al. Assessment of Bereaved Caregiver Experiences of Advance Care Planning for Children With Medical Complexity. JAMA Netw Open. 2020;3(7): e2010337.
Lotz JD, Daxer M, Jox RJ, Borasio GD, Fuhrer M. “Hope for the best, prepare for the worst”: A qualitative interview study on parents’ needs and fears in pediatric advance care planning. Palliat Med. 2017;31(8):764–71.
Mekelenkamp H, Lankester AC, Bierings MB, Smiers FJW, de Vries MC, Kars MC. Parental experiences in end-of-life decision-making in allogeneic pediatric stem cell transplantation: “Have I been a good parent?” Pediatr Blood Cancer. 2020;67(5): e28229.
Mitchell S, Spry JL, Hill E, Coad J, Dale J, Plunkett A. Parental experiences of end of life care decision-making for children with life-limiting conditions in the paediatric intensive care unit: a qualitative interview study. BMJ Open. 2019;9(5): e028548.
Murrell DV, Crawford CA, Jackson CT, Lotze TE, Wiemann CM. Identifying Opportunities to Provide Family-centered Care for Families With Children With Type 1 Spinal Muscular Atrophy. J Pediatr Nurs. 2018;43:111–9.
Odeniyi F, Nathanson PG, Schall TE, Walter JK. Communication Challenges of Oncologists and Intensivists Caring for Pediatric Oncology Patients: A Qualitative Study. J Pain Symptom Manage. 2017;54(6):909–15.
Orkin J, Beaune L, Moore C, Weiser N, Arje D, Rapoport A, et al. Toward an Understanding of Advance Care Planning in Children With Medical Complexity. Pediatrics. 2020;145(3):e20192241.
Sasazuki M, Sakai Y, Kira R, Toda N, Ichimiya Y, Akamine S, et al. Decision-making dilemmas of paediatricians: a qualitative study in Japan. BMJ Open. 2019;9(8): e026579.
Sisk BA, Friedrich A, Blazin LJ, Baker JN, Mack JW, DuBois J. Communication in Pediatric Oncology: A Qualitative Study. Pediatrics. 2020;146(3):e20201193.
Superdock AK, Barfield RC, Brandon DH, Docherty SL. Exploring the vagueness of Religion & Spirituality in complex pediatric decision-making: a qualitative study. BMC Palliat Care. 2018;17(1):107.
Zaal-Schuller IH, Willems DL, Ewals F, van Goudoever JB, de Vos MA. How parents and physicians experience end-of-life decision-making for children with profound intellectual and multiple disabilities. Res Dev Disabil. 2016;59:283–93.
Goldbeck L, Fidika A, Herle M, Quittner AL. Psychological interventions for individuals with cystic fibrosis and their families. Cochrane Database Syst Rev. 2014(6):CD003148.
Rosenberg AR, Bradford MC, Barton KS, Etsekson N, McCauley E, Curtis JR, et al. Hope and benefit finding: Results from the PRISM randomized controlled trial. Pediatr Blood Cancer. 2019;66(1): e27485.
Steineck A, Bradford MC, Lau N, Scott S, Yi-Frazier JP, Rosenberg AR. A Psychosocial Intervention's Impact on Quality of Life in AYAs with Cancer: A Post Hoc Analysis from the Promoting Resilience in Stress Management (PRISM) Randomized Controlled Trial. Children (Basel). 2019;6(11).
Rosenberg AR, Bradford MC, Junkins CC, Taylor M, Zhou C, Sherr N, et al. Effect of the Promoting Resilience in Stress Management Intervention for Parents of Children With Cancer (PRISM-P): A Randomized Clinical Trial. JAMA Netw Open. 2019;2(9): e1911578.
Beheshtipour N, Nasirpour P, Yektatalab S, Karimi M, Zare N. The effect of educational-spiritual intervention on the burnout of the parents of school age children with cancer: a randomized controlled clinical trial. International journal of community based nursing and midwifery. 2016;4(1):90.
Borjalilu S, Shahidi S, Mazaheri MA, Emami AH. Spiritual Care Training for Mothers of Children with Cancer: Effects on Quality of Care and Mental Health of Caregivers. Asian Pac J Cancer Prev. 2016;17(2):545–52.
Raitio K, Kaunonen M, Aho AL. Evaluating a bereavement follow-up intervention for grieving mothers after the death of a child. Scand J Caring Sci. 2015;29(3):510–20.
Aschenbrenner AP, Winters JM, Belknap RA. Integrative review: parent perspectives on care of their child at the end of life. J Pediatr Nurs. 2012;27(5):514–22.
Chong PH, Walshe C, Hughes S. Perceptions of a Good Death in Children with Life-Shortening Conditions: An Integrative Review. J Palliat Med. 2019;22(6):714–23.
Dias N, Hendricks-Ferguson VL, Wei H, Boring E, Sewell K, Haase JE. A Systematic Literature Review of the Current State of Knowledge Related to Interventions for Bereaved Parents. Am J Hosp Palliat Care. 2019;36(12):1124–33.
Donovan LA, Wakefield CE, Russell V, Cohn RJ. Hospital-based bereavement services following the death of a child: a mixed study review. Palliat Med. 2015;29(3):193–210.
Kochen EM, Jenken F, Boelen PA, Deben LMA, Fahner JC, van den Hoogen A, et al. When a child dies: a systematic review of well-defined parent-focused bereavement interventions and their alignment with grief- and loss theories. BMC Palliat Care. 2020;19(1):28.
Lichtenthal WG, Sweeney CR, Roberts KE, Corner GW, Donovan LA, Prigerson HG, et al. Bereavement Follow-Up After the Death of a Child as a Standard of Care in Pediatric Oncology. Pediatr Blood Cancer. 2015;62(Suppl 5):S834–69.
Longden JV. Parental perceptions of end-of-life care on paediatric intensive care units: a literature review. Nurs Crit Care. 2011;16(3):131–9.
Sieg SE, Bradshaw WT, Blake S. The Best Interests of Infants and Families During Palliative Care at the End of Life: A Review of the Literature. Adv Neonatal Care. 2019;19(2):E9–14.
Stevenson M, Achille M, Lugasi T. Pediatric palliative care in Canada and the United States: a qualitative metasummary of the needs of patients and families. J Palliat Med. 2013;16(5):566–77.
Thornton R, Nicholson P, Harms L. Scoping Review of Memory Making in Bereavement Care for Parents After the Death of a Newborn. J Obstet Gynecol Neonatal Nurs. 2019;48(3):351–60.
Vallianatos S, Huizinga CSM, Schuiling-Otten MA, Schouten-van Meeteren AYN, Kremer LCM, Verhagen AAE. Development of the Dutch structure for integrated children’s palliative care. Children (Basel). 2021;8(9):741.
Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Impact of patient involvement on clinical practice guideline development: a parallel group study. Implement Sci. 2018;13(1):55.
Acknowledgements
Collaborators of the Dutch paediatric palliative care guideline panel (in alphabetic order).
First name | Middle initials | Surname |
Inge | M. L. | Ahout |
Mattijs | W. | Alsem |
Esther | M. M. | van den Bergh |
Loes | Berkhout | |
Karin | G. C. B. | Bindels-de Heus |
Govert | Brinkhorst | |
Arno | Colenbrander | |
Linda | Corel | |
Catharina | M. | Delsman-van Gelder |
Jennifer | van Dijk | |
Jurrianne | C. | Fahner |
Jeannette | L. | Falkenburg |
Laurent | Favié | |
Annemie | F.S. | Galimont-Collen |
Karin | Geleijns | |
Rosa | Geurtzen | |
Annelies | Gijsbertsen-Kool | |
Saskia | J. | Gischler |
Marinka | A. R. | de Groot |
Anne | Haag | |
Lisette | ‘t Hart-Kerkhoffs | |
Hanneke | Heinen | |
Katja | M. J | Heitink-Polle |
Petra | Honig-Mazer | |
Carolien | S.M. | Huizinga |
Cindy | Joosen | |
Carla | C. M. | Juffermans |
Marijke | C. | Kars |
Karolien | Kisman | |
Hennie | Knoester | |
Eline | M. | Kochen |
Barbara | de Koning | |
Tom | de Leeuw | |
Jeffry | Looijestijn | |
Hilda | Mekelenkamp | |
Maarten | O. | Mensink |
Selma | Mulder | |
Mariska | P. | Nieuweboer |
Sebastianus | B.J. | Oude Ophuis |
Suzanne | G. M. A. | Pasmans |
Elise | M. | van de Putte |
Emmy | Räkers | |
Liesbeth | Rietveld | |
Irma | M. | Rigter |
Christel | D. | Rohrich |
Tanja | van Roosmalen | |
Elisabeth | J. | Ruijgrok |
Jolanda | H. | Schieving |
Kim | van der Schoot | |
Antoinette | Y. N. | Schouten-van Meeteren |
Ellen | Siegers-Bennink | |
Henriette | Sjouwke | |
Tanneke | Snijders-Groenendijk | |
Mara | van Stiphout | |
Suzanne | van de Vathorst | |
Leo | van Vlimmeren | |
Mirjam | A. | de Vos |
Nellie | van Wageningen | |
Anne | Weenink | |
Willemien | de Weerd | |
Ilse | H. | Zaal-Schuller |
Funding
The Netherlands Association for Health Research and Development (ZonMw). The funding bodies played no role in the design of the study and collection, analysis, interpretation of data, and in writing the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
KvT, LK, EV, JV, HR, BB, EM, and RM contributed to the conception and design of the methodology.KvT, LK, EV, EM, RM contributed to the search strategy, study selection and quality appraisal.KvT, RM and EM drafted the manuscript. Subsequently, LK, EV, BB, JV and HR critically revised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. For the surveys, all participants have given informed consent. No institutional or other licensing committee’s approval is needed for guideline creation, as participants are not subjected to procedures and are not required to follow rules of behaviour. Therefore, in accordance to the Dutch law (Medical Research Involving Human Subjects Act (WMO), article 1b) ethics approval was deemed unnecessary: https://english.ccmo.nl/investigators/legal-framework-for-medical-scientific-research/your-research-is-it-subject-to-the-wmo-or-not.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix (A).
Survey among health care professionals to select guideline topics. Appendix (B). Survey among patient representatives and parents to select guideline topics. Appendix (C). Paediatric palliative care guideline panel; Appendix (D). Working structure for guideline development; Appendix (E). Guideline development process; Appendix (F). Clinical questions; Appendix (G). Search strategies; Appendix (H). Inclusion criteria; Appendix (I). Criteria for appraisal of evidence and strength of recommendations; Appendix (J). Results: identified evidence and selected additional literature.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
van Teunenbroek, K.C., Kremer, L.C.M., Verhagen, A.A.E. et al. Palliative care for children: methodology for the development of a national clinical practice guideline. BMC Palliat Care 22, 193 (2023). https://doi.org/10.1186/s12904-023-01293-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-023-01293-3