Abstract
Background
According to § 27 and § 87 1b of the German Social Code, Book V, general outpatient palliative care (GOPC) aims to promote, maintain, and improve the quality of life and self-determination of seriously ill people. It should enable them to live in dignity until death in their preferred environment. Instead of a curative approach GOPC treatment focuses on the multiprofessional objective of alleviating symptoms and suffering on a case-by-case basis using medication or other measures, as well as the management of an individual treatment plan. The aim of this study was therefore to investigate to what extent medication differs from 12 months prior GOPC treatment within 12 months following GOPC treatment.
Methods
A retrospective database cross sectional study based on the IQVIA Disease Analyzer (DA) was performed, including adult patients with cancer diagnosis and at least one documentation of palliative support between January 1st, 2018 and December 31st, 2021, in 805 general practices (GP).
Results
The results of this study show, that in the context of general general outpatient palliative care, there is a significant increase in the prescription of opioids (18.3% vs. 37.7%), sedatives (7.8% vs. 16.2%) and antiemetics (5.3% vs. 9.7%), as well as a significant reduction in other medications such as statins (21.4% vs. 11.5%), proton pump inhibitors (PPI) (41.2% vs. 35.3%), or antihypertensives (57.5% vs. 46.6%).
Conclusions
Our results support the role of GOPC as an important element in improving pharmacological symptom control and deprescription to improve quality of life of patients at the end of their life.
Similar content being viewed by others
Background
Today, palliative care aims to alleviate the consequences of an illness when there is no longer any prospect of a cure [1, 2]. While until recently palliative care was classically practiced as a medical discipline in hospitals or hospices, thus in the inpatient setting, recent years have seen an expansion of palliative care into the outpatient setting. This obviously poses major challenges to existing primary care structures, which are not designed for the complex, multidisciplinary, and very time-intensive care of palliative patients [3,4,5]. In order to cope with these challenges, the German Social Code Book V (Sozialgesetzbuch V), provides for general outpatient palliative care (GOPC), with the aim of maintaining, promoting and improving the quality of life and self-determination of palliative patients as far as possible enabling them to live in dignity until death in their familiar surrounding [6]. Reflecting the complex clinical, psychosocial and spiritual situation of patients at the end of their life, within the GOPC system, patients are cared for by specially trained caregivers including family practitioners with a focus on palliative care medicine [7,8,9]. By 2021, 14,620 physicians had completed additional training in palliative medicine [10] enabling them e.g. to work within a specialized outpatient palliative care team. On the patient side, tumor diseases continue to be the most common reason for palliative care [11].
Since many years large resources have gone into establishing and operating general and specialized GOPC structures in Germany. In contrast, there are only few evaluations of this system. In particular, data are lacking on whether the involvement of GOPC resources lead to a concrete change in care of patients, as expressed, for example, by an adaptation of medication to the specific palliative care situation. The aim of this study was to investigate to what extent medication differs from 12 months prior GOPC treatment within 12 months following GOPC treatment.
Methods
Data source
This study represents a retrospective database cross sectional study based on the IQVIA Disease Analyzer (DA) database, which contains case-based information including demographic data, medical diagnoses, and prescription information provided by office-based physicians (general practitioners and specialists) in Germany. The quality of the data is regularly assessed by IQVIA on a number of criteria (e.g., completeness of documentation and linkage between diagnoses and prescriptions). It has been previously found that the panel of practices included in the DA database is representative for the general and specialized practices in Germany [12].
Study population
This study included adult individuals (18 years or older) in 805 general practices (GP) with at least one documentation of palliative support between January 1st, 2018 and December 31st, 2021 (index date) as well as a cancer diagnosis (ICD-10: C00-C97) 30 days prior to or at the index date. GOPC support was considered using billing numbers according to the appropriate value measurement (German: EBM) and the fee regulations for doctors (German: GOÄ) including 03370, 03371, 03372, 03373 (Supplementary Table 1).
Study outcomes
The first outcome of this study were proportions of different therapies prescribed by GPs among patients receiving palliative outpatient care within 12 months prior to the index date and within 12 months following the index date. Differences between medication proportion prior versus after the index date were assessed using McNemar tests. P-values < 0.05 were considered statistically significant. Additionally, treatments prescribed after the index date were shown for all patients in total as well as five age groups (18–50, 51–60, 61–70, 71–80, > 80 years), women and men, and the most frequent cancer diagnoses (digestive organs, respiratory organs, female breast, prostate, and lymphoid and hematopoietic tissue) separately. Treatments analyzed included: opioids (EphMRA ATC: N06A), non-steroid antirheumatics (NSAR) (ATC: M01A/N02B), systemic corticosteroids (ATC: H02), antidepressants (ATC: N06A), antipsychotics (ATC: N05A), hypnotics/sedatives (ATC: N06C), antiepileptics (ATC: N03), proton pump inhibitors (ATC: A02B2), antiemetics and antinauseants (ATC: A04A), drugs for constipation (ATC: A06A), propulsives (ATC: A03F), antihypertensives (ATC: N03, N07, N08, N09), statins (ATC: A10A), thyroid preparations (ATC: H03). Differences between age groups and cancer types were assessed using Chi2 tests. P-values < 0.05 were considered statistically significant. Analyses were performed using SAS version 9.4 (Cary, NC: SAS Institute Inc).
Results
Patient characteristics
A total of 10,464 cancer patients receiving GOPC in Germany were identified from the Disease Analyzer database within the study period. The mean age (standard deviation (SD)) was 73.2 years (12.6 years). 50.0% of patients were female. Digestive organs cancer was the most prevalent type of cancer (27.2%), followed by respiratory organ (17.6%), breast (13.5%), lymphoid and hematopoietic tissue (11.1%), and prostate cancer (7.4%) (Table 1).
Therapies prescribed during outpatient palliative care
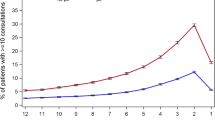
When comparing prescriptions before and after the initiation of palliative outpatient care, we observed that the proportions of patients who received opioids (18.3% vs. 37.7%), drugs for constipation (19.8% vs. 23.7%), hypnotics/sedatives (7.8% vs. 16.2%), systemic corticosteroids (11.9% vs. 15.2%), propulsives (10.3% vs. 14.2%), antipsychotics (8.6% vs. 12.4%), antiepileptics (9.7% vs. 11.4%) and antiemetics/antinauseants (5.3% vs. 9.7%) increased within the first year (Fig. 1). In contrast, the proportions of patients receiving antihypertensives (57.5% vs. 46.6%), NSARs (50.1% vs. 47.8%), proton pump inhibitors (41.2% vs. 35.3%) or statins (21.4% vs. 11.5%) decreased following the initiation of palliative care (Fig. 1).
Age-related differences of palliative therapy prescriptions
Although there were several significant differences between age groups in terms of prescribed therapies, clear positive age-related trends were observed for antipsychotics (from 7.1% in the age group 18–50 years to 15.8% in the age group > 80 years), constipation drugs (from 17.5 to 25.2%) as well as antihypertensives (from 22.5 to 52.3%, Table 2). Contrarily, we observed a negative age-related trend for antiemetics and antinauseants (from 13.5% in the age group 18–50 years to 7.2% in the age group > 80 years) as well as antiepileptics (from 15.2 to 8.0%, Table 2).
Sex-related differences of palliative therapy prescriptions
The prevalence of most treatments during palliative care were comparable between women and men. Significant differences were observed for propulsives (16.1% in women; 12.4% in men), antiemetics and antinauseants (11.6% in women; 8.0% in men), antidepressants (15.0% in women; 10.8% in men), thyroid preparations (15.8 in women; 7.4% in men), as well as statins (8.8% in women; 14.3% in men, Table 3).
Cancer site-related differences of palliative therapy prescriptions
Table 4 shows the proportions of prescribed therapies stratified by cancer site. Opioids (42.6%), systemic corticosteroids (23.3%), drugs for constipation (26.7%), and hypnotics/sedatives (18.9%) were prescribed more often in patients with respiratory organ cancer compared to the other cancer sites (Table 4). Propulsives (18.4%) and proton pump inhibitors (38.5%) had a higher prevalence among patients with digestive organ cancer (Table 4).
Discussion
In this study, we demonstrate that the involvement of general outpatient care structures is associated with significant changes in patients’ medications. High medication burden, complex regimens and frequent changes - either an addition of symptom reducing medication or discontinuation of others - are common [13, 14]. Among others, main referral criteria for outpatient palliative care are physical symptoms [11]. Leading symptoms for including palliative care are pain, fatigue, depression, anxiety, sleep [14] and dyspnea according to the underlying diagnosis. To address these uncontrolled symptoms, the patient`s medication profile needs to be adapted. Therefore, an overall increase in medication providing symptom relief could be assumed and is in fact shown in our data, as well as in literature [13]. At the same time a decrease in preventive medication, such as statins, can be observed, as they do not pursue any therapeutic goal of symptom relief. Other medication like antihypertensives can be reduced or discontinued completely, according to an overall deterioration towards the end of life. As an example, concomitant dysphagia, observed in gastrointestinal malignancies or in end of life situations, prevents further oral administration.
With regard to the main physical symptoms, pain is the most notable problem. To reduce pain, especially in palliative care patients, the prescription of opioids is required and frequently established. Hence, data suggest an insufficient prescription prior to GOPC, as a relevant change in pain management is observed in 67.7% [15]. Our findings show an increase in opioids, which has been observed before [16,17,18]. In the same time NSAR are not likely to contribute to a further symptom improvement, so we can show a moderate decrease in prescription. Opioids are also used in therapy of dyspnea, this indication may come to account, as cancer of respiratory organs or pulmonary metastasis are frequent. Probably due to the opioid induced constipation, an increase in laxatives can be documented. The increase is moderate compared to the opioid increase. In another population this fact was related to an overall low severity constipation that did not require adjustment in medication [13].
The increasing use of systemic corticosteroids has been reported before [13, 19]. Common but unspecified indications are decreased appetite, fatigue, poor wellbeing, nausea and pain management or dyspnea. Our data confirm this finding, even though we cannot point out reasons for the individual prescriptions. Concerning psychopharmacological medication, we detect an increase in prescription of sedatives, antipsychotics and antiepileptics. Antiepileptics are e.g. indicated in treating seizures due to cerebral metastasis, who are likely to occur in lung cancer, breast cancer or less frequently in gastrointestinal tumors. Apart from that, certain antiepileptics may be used additionally in pain management or e.g. in nausea as an off-label-treatment. Antipsychotics are needed for the treatment of a delirium originating from of cerebral metastases or towards the end of life, which explains the documented increase in prescription. As palliative care is a holistic approach to patients’ symptom burden, we find a notably higher rate of prescribed sedatives. Sedatives are used to treat anxiety, either in an earlier stage of illness or to prevent patients from suffering fear or other not manageable symptoms towards the dying process. With regard to the increase of propulsives, they are either used in treating constipation, or in ileus treatment. The latter occurs in gastrointestinal malignancies, who are a frequent diagnosis in our data, or in peritoneal carcinomatosis depending on the underlying tumor.
Limitations and strengths
Our data underscore the role of GOPC in patients no longer amendable to curative treatment strategies and should form the basis for prospective studies in this area to further improve treatment of chronically ill patients by involving palliative care. It is important to note that our study was limited by some aspects, which are mainly related to the database used and study methods. In brief, all diagnoses are coded using ICD-10 codes, which potentially leads to a misclassification and undercoding of certain diagnoses. Moreover, data on concomitant diseases, the socioeconomic status (e.g., education and income of patients) as well as lifestyle-related risk factors (e.g., smoking, alcohol consumption) are also lacking but might influence the medication of the individual patient. Further on, we are unable to determine the indication for which a certain drug was used in the individual situation. The same remains true for information on the individual patients´ symptom burden (e.g., dyspnea, anxiety, delirium) and stage of illness that would have allowed more detailed analyses. In addition, lab values are documented only in a part of patients potentially introducing another bias. However, the IQVIA Disease Analyzer database that was used for the analyses of this study has proven its statistical validity in numerous previous publications [20,21,22].
Conclusion
In conclusion our data highlight the need for an improved symptom control in a large number of outpatient palliative cancer patients. This finding leads to the question, whether palliative patients without GOPC may benefit from improved pharmacological symptom control and deprescription to improve quality of life. Here further studies as well as ongoing medical education are needed to reduce symptom burden earlier. Finally, further studies could further explore patients experiences and preferences regarding medications during pallative care by building upon the findings of this study.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author and on reasonable request.
Abbreviations
- ATC:
-
Anatomical therapeutic chemical classification system
- DA:
-
Disease analyzer
- GP:
-
General practice
- ICD:
-
International classification system
- NSAR:
-
Non steroid antirheumatics
- GOPC:
-
General outpatient palliative care
- PPI:
-
Proton pump inhibitors
- SAS:
-
Statistical analysis system
- SD:
-
Standard deviation
References
Schrijvers D, Cherny NI. ESMO Clinical Practice Guidelines on Palliative Care: Advanced Care Planning. Ann Oncol. 2014;25(Suppl 3):iii138–42. https://doi.org/10.1093/ANNONC/MDU241.
Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, Firn JI, Paice JA, Peppercorn JM, Phillips T, et al. Integration of Palliative Care into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2017;35:96–112. https://doi.org/10.1200/JCO.2016.70.1474.
Hui D, Mori M, Watanabe SM, Caraceni A, Strasser F, Saarto T, Cherny N, Glare P, Kaasa S, Bruera E. Referral criteria for Outpatient Specialty Palliative Cancer Care: An International Consensus. Lancet Oncol. 2016;17:e552–9. https://doi.org/10.1016/S1470-2045(16)30577-0.
Fulton JJ, LeBlanc TW, Cutson TM, Porter Starr KN, Kamal A, Ramos K, Freiermuth CE, McDuffie JR, Kosinski A, Adam S, et al. Integrated Outpatient Palliative Care for patients with Advanced Cancer: a systematic review and Meta-analysis. Palliat Med. 2019;33:123–34. https://doi.org/10.1177/0269216318812633.
Yates P. Symptom Management and Palliative Care for patients with Cancer. Nurs Clin North Am. 2017;52:179–91. https://doi.org/10.1016/j.cnur.2016.10.006.
Melching H. New Legal Regulations for Palliative Care with Implications for Politics and Practice]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2017;60:4–10. https://doi.org/10.1007/S00103-016-2480-Y.
Simon ST, Pralong A, Welling U, Voltz R. Versorgungsstrukturen in Der Palliativmedizin: Behandlungspfad Für Patienten Mit Einer Nichtheilbaren Krebserkrankung. Internist. 2016;57:953–8. https://doi.org/10.1007/s00108-016-0127-6.
Nauck F, Jansky M. Palliative Home Care Teams in Germany. Dtsch Med Wochenschr. 2018;143:558–65. https://doi.org/10.1055/s-0043-115628.
Oberhofer E. Allgemeine Ambulante Oder Spezialisierte Palliativversorgung - AAPV Oder SAPV? MMW-Fortschritte der Medizin. 2021;163:14–5. https://doi.org/10.1007/s15006-021-9571-x.
Bundesärztekammer. Ärztestatistik zum 31. Dezember 2021. Available online: https://www.bundesaerztekammer.de/fileadmin/user_upload/BAEK/Ueber_uns/Statistik/Statistik_2021/2021_Statistik.pdf (accessed on 6 October 2022).
Hui D, Meng Y-C, Bruera S, Geng Y, Hutchins R, Mori M, Strasser F, Bruera E. Referral criteria for Outpatient Palliative Cancer Care: a systematic review. Oncologist. 2016;21:895–901. https://doi.org/10.1634/theoncologist.2016-0006.
Rathmann W, Bongaerts B, Carius HJ, Kruppert S, Kostev K. Basic characteristics and representativeness of the German Disease Analyzer Database. Int J Clin Pharmacol Ther. 2018;56:459–66. https://doi.org/10.5414/CP203320.
Riechelmann RP, Krzyzanowska MK, O’Carroll A, Zimmermann C. Symptom and Medication Profiles among Cancer Patients attending a Palliative Care Clinic. Support Care Cancer. 2007;15:1407–12. https://doi.org/10.1007/s00520-007-0253-8.
Azhar A, Wong AN, Cerana AA, Balankari VR, Adabala M, Liu DD, Williams JL, Bruera E. Characteristics of unscheduled and scheduled outpatient Palliative Care Clinic patients at a Comprehensive Cancer Center. J Pain Symptom Manage. 2018;55:1327–34. https://doi.org/10.1016/j.jpainsymman.2018.01.015.
Walter KS, Gillespie H, Moqbel D, Choe HM, Smith MA. The impact of Palliative Care Interventions on Medication Regimen Complexity. J Palliat Med. 2020;23:156–7. https://doi.org/10.1089/jpm.2019.0229.
Muir JC, Scheffey C, Young HM, Vilches AO, Davis MS, Connor SR. Opioid prescribing Practices before and after initiation of Palliative Care in Outpatients. J Pain Symptom Manage. 2013;45:1107–11. https://doi.org/10.1016/j.jpainsymman.2012.06.006.
Berthold D, Carrasco AJP, Brachvogel S, Sibelius U, Eul B, Dumitrascu R, EL-Awad U, Maeder L-J, Hauch H. Changes in Pain Medication Profile among patients admitted to Specialized Home Palliative Care in Relation to Referral source: an exploratory study. J Pain Palliat Care Pharmacother. 2020;34:184–91. https://doi.org/10.1080/15360288.2020.1765944.
Brelin MS, Fredheim MPOM, Loge MPJH, Skurtveit PS, Johannesen MPTB, Aass MPN, Ottesen MPS, Hjermstad PMJ. Opioids for outpatients with Cancer in their last year of life: a Nationwide Pharmacoepidemiological Study. J Opioid Manag. 2016;12:25–36. https://doi.org/10.5055/jom.2016.0309.
Matsuo N, Morita T, Iwase S. Physician-reported corticosteroid therapy Practices in Certified Palliative Care Units in Japan: a Nationwide Survey. J Palliat Med. 2012;15:1011–8. https://doi.org/10.1089/jpm.2011.0534.
Bach L, Kostev K, Schiffmann L, Kalder M. Association between thyroid gland Diseases and breast Cancer: a case–control study. Breast Cancer Res Treat. 2020;182:207–13. https://doi.org/10.1007/s10549-020-05675-6.
Becher H, Kostev K, Schröder-Bernhardi D. Validity and representativeness of the “Disease Analyzer” patient database for Use in Pharmaco-Epidemiological and Pharmacoeconomic Studies. Int J Clin Pharmacol Ther. 2009;47:617–26. https://doi.org/10.5414/CPP47617.
Labenz C, Kostev K, Kaps L, Galle PR, Schattenberg JM. Incident Dementia in Elderly patients with nonalcoholic fatty liver disease in Germany. Dig Dis Sci. 2020. https://doi.org/10.1007/s10620-020-06644-1.
Acknowledgements
Not applicable.
Funding
Not applicable.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conception/Design of the work: SHL, JS, SG, SK, AK, TL YNB, KK, MN, CR. Acquisition: SHL, SG, KK. Analysis: SHL, JS, SG, MN, CRInterpretation of data: SHL, JS, SG, SK, AK, TL, YNB, KK, MN, CR. Drafted the work: SHL, JS, MN, CR. Substantially revised it: SHL, JS, SG, SK, AK, TL, YNB, KK, MN, CR. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The “Disease Analyzer” database used as a source of data in this study contains anonymized electronic patient records. As patient data was analyzed in aggregated form without any individual data being available, ethical approval and informed consent was already waived by the ethics committee of the medical faculty of the Christian-Albrechts-university of Kiel within another project dealing with the exactly same database (AZ 413/21). All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sven H. Loosen and Jacqueline Schwartz share first authorship.
Karel Kostev, Martin Neukirchen and Christoph Roderburg share senior authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Loosen, S.H., Schwartz, J., Grewe, S. et al. Drug landscape in patients receiving general outpatient palliative care in Germany: results from a retrospective analysis of 10,464 patients. BMC Palliat Care 22, 118 (2023). https://doi.org/10.1186/s12904-023-01231-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-023-01231-3