Abstract
Background
The characteristics and outcomes of palliative patients who visited the Emergency Department (ED) in Thailand, a country in which no standard palliative care system existed, have not been comprehensively studied. We aimed to report the characteristics of ED palliative patients and investigate factors associated with mortality.
Methods
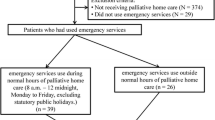
A prospective observational study was conducted at Siriraj Hospital, Bangkok, Thailand, between March 2019 and February 2021 by means of interviewing palliative patients and/or their caregivers and medical record review. Palliative patients with either incurable cancer or other end-stage chronic diseases were included.
Results
A total of 182 patients were enrolled. Their mean age was 73 years, 61.5% were female, and 53.8% had incurable cancer. Of these, 20.3% had previously visited the palliative clinic. Approximately 60% had advanced directives, 4.9% had a living will, and 27.5% had plans on their preferred place of death. The most common chief complaint was dyspnea (43.4%), and the main reason for ED visits was ‘cannot control symptoms’ (80%). At the ED, 17% of the patients had been seen by the palliative care team, and 23.1% died. Although 51% were admitted, 48.9% could not survive to discharge. Cancer, having received morphine, a palliative performance scale > 30, and ED palliative consultation were independently associated with hospital mortality.
Conclusion
The recognition and utilization of palliative care were largely inadequate, especially for non-cancer patients. An improvement and promotion in the palliative care system from the ED through home care are mandatory to improve the quality of life of palliative patients.
Similar content being viewed by others

Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
With our move toward an ageing society, more people have developed chronic and incurable diseases. Patients with these advanced illnesses usually receive supportive and symptomatic palliative treatment at home or other nursing residences. However, during the last period of their lives, they generally visit the Emergency Department (ED) more frequently [1,2,3]. Some of these visits are avoidable by integrating appropriate and high-quality palliative treatment into the standard of care, while many others are not. Previous studies have reported variable rates of unavoidable ED visits ranging from 45 to 95% with various presenting symptoms, such as pain, respiratory and gastrointestinal problems, fatigue, and altered mental status [2, 4,5,6,7,8]. Although unavoidable visits may occur due to unprecedented symptoms and conditions for which patients truly require urgent care, most are still a result of suboptimal palliative treatment. Advance care planning is often initiated too late in the disease trajectory. Also, patients, families, and healthcare providers are often not educated well enough and are thus not timely prepared for expected future problems. Consequently, these patients have to visit and be admitted to the ED and the hospital despite their wishes [9, 10]. These visits are an indicator of poor end-of-life care and ineffective palliative care systems, and can also result in caregiver burden and ED crowding [7, 11, 12]. Many studies have also emphasized the significant amount of ED resources utilized by the palliative population [4, 6, 8, 13]. Moreover, some patients could not survive to discharge and had to spend their true end-of-life in the hospital against their wishes. According to previous studies, patients particularly at higher risk of in-hospital mortality were those presenting with dyspnea, altered mental status and weakness/fatigue, and patients with gastrointestinal tract cancer, hypoalbuminemia, and poor performance status [14, 15].
In Thailand, the National Health Act of Thailand launched in 2007 has highlighted the right of the people to make a living will to refuse health services that are provided merely to prolong their terminal stage of life [16]. After this act was published, the Ministry of Public Health has emphasized policies relating to palliative care starting from the primary care system to the hospitals nationwide. However, there are still no governmental hospices or standard systematic long-term care services for palliative patients up until now. With such a distinctive scenario, the characteristics of palliative patients visiting the ED in Thailand may differ significantly from other settings with more standardized practices and systems. Also, understanding the causes and consequences of these visits, as well as factors associated with poor outcomes, may facilitate future development of appropriate and effective palliative care services. Therefore, this study was conducted to investigate the characteristics of palliative patients who visited the ED and the causes of their visits. We also aimed to analyze factors associated with mortality in the ED and at hospital discharge in these patients.
Methods
Study design and setting
This prospective observational study was conducted between March 2019 and February 2021 at the ED of Siriraj Hospital, the largest tertiary university hospital in Bangkok, Thailand, with over 18,000 annual ED visits and over 2000 inpatient beds. The ED provides care for patients triaged as level 1 or 2 based on the Emergency Severity Index (ESI) criteria [17]. Patients with ESI triage level 3 to 5 are taken care of in a separate urgency unit next to the ED, which is covered by general practitioners and internal medicine physicians. In our hospital, some patients with advanced illnesses are referred to the hospital’s palliative care clinic at the primary physician’s discretion on an outpatient basis. The clinic is operated by the palliative care team, a multidisciplinary team consisting of family physicians, nurses, and other healthcare professionals specializing in palliative care, as well as anesthesiologists specializing in pain management. They not only offer outpatient services at the palliative clinic but also operate a 4-bed palliative inpatient ward and provide consultant services for inpatients of other wards as well as ED patients during office hours on weekdays.
Participants
Palliative patients over 18 years of age who visited the ED during the study period were prospectively enrolled. We defined palliative patients as those with at least one of the following conditions; 1) cancer of incurable stages or cancer with untreatable status, 2) organ failures affecting daily living, such as end-stage heart disease [18], decompensated liver cirrhosis [19], end-stage renal disease with no plans of renal replacement therapy, and end-stage lung disease (i.e., severe chronic obstructive pulmonary disease, severe pulmonary hypertension, pulmonary fibrosis) [20], and 3) neurodegenerative disorders, such as severe dementia, advanced-stage Parkinson’s disease, and previous stroke with totally dependent status. We also required that the primary treating physician of each included participant agreed with the palliative treatment decision.
Ethics, study process, and data collection
The study protocol was ethically approved by the Siriraj Institutional Review Board (certificate no. 091/2019). All participants or their next of kin provided written informed consent prior to the study inclusion.
When eligible patients visited the ED, the ED attending physicians, who provided initial management to the patients, notified the study investigators of potential recruitment. The study investigators would wait until eligible patients were stabilized before initiating the enrollment and study process. After eligibility was confirmed and written consent obtained, a trained study investigator verbally interviewed each participant if their consciousness allowed and if they were not in any significant distress due to their conditions. Otherwise, the primary caregiver of the participant was the only interviewee. Data collected by means of an interview included patients’ and caregivers’ characteristics, while details of clinical manifestations, management, and outcomes were collected by using medical record review. The palliative performance score (PPS) was evaluated by interviewing the caregivers and having them assess the patients’ status prior to developing the symptoms that led them to the index ED presentation [21]. The main outcomes of the study were mortality in the ED and mortality at hospital discharge.
The study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline [22].
Statistical analysis
Descriptive statistics were employed to describe the patients’ and caregivers’ characteristics. Categorical data are reported as frequency and percentage. Continuous variables are reported as mean and standard deviation (SD) or median and interquartile range, as appropriate. Between-group comparisons were performed using the Chi-squared or Fisher’s Exact test for categorical data and an independent t-test or the Mann Whitney U test for continuous data. Characteristics were compared between patients discharged dead and alive and between those with and without cancer.
Multivariable logistic regression analyses were employed to assess independent factors associated with mortality in the ED and at hospital discharge. Factors included in the models were potential predictors of the outcomes based on literature review, scientific rationale, and univariable logistic regression analyses. They were age, sex, known case of cancer, documented advance care planning, previous palliative clinic consultation within 24 h before arrival, having been prescribed morphine within the index ED visit, palliative care team consultation in the index ED visit, and a PPS > 30 [21]. Independent factors associated with the outcome were chosen by using backward stepwise regression method. Results are reported as adjusted odds ratio (aOR) and its 95% confidence interval (CI). There were no missing outcomes. Although some variables in the models had missing data, the rate of missingness was negligible (< 5%); thus, they were judged to be missing completely at random, and no imputation techniques were attempted.
For all the analyses, a p-value of < 0.05 was considered statistically significant. All analyses were performed using SPSS version 18.0 (Chicago, IL., USA).
Results
During the study period, 184 palliative patients visited the ED, 2 (1.1%) had died shortly after ED arrival and thus could not be recruited. Therefore, 182 patients were included in the study. The characteristics of the patients and their caregivers are presented in Tables 1 and 2, respectively. The patients’ mean age (± SD) was 73 ± 15 years, and 61.5% of them were female. Of all the patients, 98 (53.8%) had incurable cancer. Among cancer patients, 82.7% had metastatic cancer. On the other hand, neurodegenerative diseases were the most common cause of palliation in non-cancer patients (59%), followed by heart failure (8.2%), kidney failure (7.7%), and liver failure (4.9%). Most patients (74.1%) were brought to the ED based on the decision made by their relatives or nursing home staffs. Approximately 40% of all patients used emergency medical service as their mode of transportation to the hospital. Most patients visited the ED on weekdays (74.2%), and 52.2% came to the ED in the morning shift. Only 20.3% of included patients had previously visited the palliative clinic of our center.
The two most common chief complaints were dyspnea (43.4%) and altered mental status (17.6%). Commonly reported reasons for visiting the ED were ‘cannot control symptoms’ (80%) and ‘need to work-up other causes’ (36.3%). The majority of the patients (60.4%) had some form of advance care plan; however, only 4.9% had a living will and 72.5% had no plan regarding their preferred place of death. Among those with such plan, home was the most preferable location (15.9%). Additional patients’ characteristics are presented in Supplementary Appendix Table 1.
As for the caregivers, the patients’ child was the primary caregiver in 113 patients (62.1%). Most caregivers (66.5%) still worked full-time, while 8.8% had to quit their job. Approximately 80% understood the palliative treatment plan and knew the planned management had the patients gotten worse. However, 62.1% still had concerns about taking care of the patients at home. Discordant to the patients’ will, the most preferred place of death for the caregivers was the hospital (36.3%).
After ED arrival, the palliative care team was consulted by the ED physicians in 17% of the cases. Primary ED diagnoses mainly were related to infection, with respiratory tract infection as the most prevalent diagnosis (39.6%). Therefore, antibiotics administration was the most common management at the ED (83.5%). Although approximately half of the patients were admitted, only 9.9% were admitted to the palliative ward.
Of all palliative patients visiting the ED, 42 (23.1%) died in the ED, and 89 (48.9%) could not survive to discharge. Table 3 demonstrates the characteristics of patients stratified by mortality status at hospital discharge. Cancer was slightly more prevalent in those who died than in those discharged alive (p = 0.071). Non-survivors also received more palliative care consultation and morphine (both p < 0.001). On the contrary, survivors to discharge had a higher PPS (p = 0.025), and more of them decided to visit the ED by themselves (p = 0.035). We also analyzed independent factors associated with mortality (Table 4). Having received morphine and a PPS > 30 were significantly associated with mortality in the ED (aOR 4.05; 95%CI 1.81–9.03 and 0.27; 95%CI 0.1–0.7, respectively). While factors independently associated with in-hospital death were morphine, PPS > 30, cancer, and ED palliative consultation (aOR 4.92; 95%CI 2.24–10.81, 0.31; 95%CI 0.13–0.71, 2.62; 95%CI 1.07–6.41, and 3.88; 95%CI 1.23–12.22, respectively).
When stratified the patients by the presence of cancer, we found that more cancer patients decided to visit the ED by themselves (p < 0.001) and more had previous palliative clinic visits (p < 0.001) than non-cancer patients (Table 5).
Discussion
In Thailand, the palliative care system has not been well-established despite an increasing number of patients with incurable illnesses. This study describes the characteristics of palliative patients who visited the ED of the largest tertiary university hospital in Thailand. In the present study, approximately half of palliative patients did not have cancer but had other end-staged diseases, which was discordant with other studies in which most patients included were cancer patients [2, 4,5,6,7, 9,10,11]. Our finding indicates the need to expand the provision of palliative care and the field of palliative research to more extensive and diverse populations.
In many previous studies, dyspnea and pain were among the most common presenting symptoms that brought the patients to the ED [1, 2, 6, 23]. In this study, although we also found dyspnea as the most common chief complaint, pain was only reported in 1.6% of the patients. This discordance might have been because of effective home pain management provided by our healthcare providers and the palliative care team or due to the fact that our ED only provides care for very high-acuity patients triaged as level 1 or 2. While patients presenting with pain are usually triaged to level 3 to 5, and were thus sent to the urgency unit instead, thereby not being included in the present study. Moreover, we found that only a quarter of all patients decided to visit the ED by themselves, corresponding to a previous review stating that palliative patients, most of whom were cancer patients, often did not want to visit the ED [12]. However, in the present study, a significant number of non-cancer patients with neurodegenerative diseases and decreased cognitive ability were also enrolled, thus possibly underestimating the true prevalence of self-decision makers.
Also concordant with many previous studies, the main reason for ED visits in this study was that the patients could not control their symptoms [9, 10]. This could partly reflect the quality of our palliative system of care. In fact, palliative care recognition and utilization were immensely inadequate as only about 20% of the patients, most of whom were those with cancer, had previously visited our palliative clinic. Also, had there been a system of home consultation or home care services, ED visits due to this specific reason could have been reduced. Therefore, improving the quality of the palliative system and promoting its utilization, especially in non-cancer patients, are essential to enhance the well-being of end-of-life patients and reduce ED visits. Nonetheless, the rate of avoidable ED visits in this study was only 1.6% (data not shown), which was significantly lower than in other studies [4, 6, 7, 24], and the discharge rate was only 17.6%, demonstrating the very high-acuity and severity of the patients. Thus, it is questionable if improving the palliative care system will ever reduce ED visits to a large extent. Nevertheless, the lack of a standard system of palliative care might influence the quality of life of palliative patients in general, thus leading to, though unavoidable, unnecessary ED visits. Furthermore, a study by Verhoef MJ, et al. found that patients who had a proactive symptom management plan had lower in-hospital death (29.5%) than those without such plans [2]. Whereas in our study, only a handful of patients had those plans and even a smaller proportion truly understood them, corresponding to such a high rate of in-hospital mortality (48.9%).
The most common ED diagnosis was infection (67.1%), similar to a previous study [2] and concordant with the percentage of antibiotics administration. However, due to the lack of long-term care and hospices, the patients who required intravenous antibiotics had to be admitted. Nonetheless, the proportion of patients admitted to the hospital in this study was not different from other settings with long-term care and hospices implemented [5,6,7]. This paradoxical similarity was most likely because of the limited inpatient beds in our hospital, especially for palliative patients, as most of them had to stay in the ED. This crowding in the ED could also partly explain the high ED mortality rate in the present study [25].
Although approximately 60% of the patients had advance care plan, only 4.9% had a living will. This might have been because of Thai culture and tradition that limit the patients and families, who are the patients’ main caregivers, from discussing about advance care plan despite the patients having chronic diseases or cancer [26]. In fact, most of the main caregivers of the patients in the present study were their children, unlike a study by Lawson BJ, et al., from which the patients’ main caregivers were their spouses [13], who might have been more likely to discuss advanced care planning with the patients and have more influence on the family’s decision based on the Thai culture. Nonetheless, the families and physicians tended to choose the goals of treatment and advance care plan that they see fit and should meet the patients’ expectations [27]. However, our result showed that the patients preferred to die at home while their caregivers preferred otherwise. This finding was similar to a previous study in Thailand, which reported a diverse direction of perceptions between the patients and their caregivers [28]. Consequently, initiating palliative care as early as possible is fundamental to bring the patients and their caregivers together on the same page. The first step usually involves a discussion with all parties involved on the goals of care. Although initiating such an essential step in the ED has shown to provide benefits for the patients and lessen the burden of the health care system by reducing ED visits [1, 29], most emergency physicians were not comfortable doing so primarily because they did not have prior relationships with the patients and their families [2, 12]. Also, they did not consider themselves qualified in terms of knowledge and skills, and some also feared having conflicts with the patients’ families that may result in legal consequences [30]. Furthermore, the quality of this critical step performed in the ED may not be as desirable considering the time constraint in the ED setting.
We also found that having received morphine and a low PPS were associated with both ED and in-hospital death, concordant to a previous study [15]. However, cancer and palliative care team consultation in the ED were only independently associated with higher hospital mortality while failing to show significant associations with ED mortality. This discordance might have been because more patients with cancer were admitted, and very severe patients could have died in the ED before palliative consultation was initiated. In fact, the patients who had palliative care consultation could have been associated with higher in-hospital mortality because their symptoms were so severe, and they were judged to be approaching death, thus triggering the consultation for the purpose of both palliative ward admission and symptoms control. Regardless, these results emphasize the necessity of having a standardized and effective palliative care system aimed at both cancer and non-cancer patients. A specialized palliative care team and palliative care education for healthcare providers in the ED should also be encouraged.
Limitations
Despite the study being one of the first among those conducted in suboptimal healthcare settings, the study had some limitations. First, it was a single-center study involving one tertiary university hospital, which may limit the study’s generalizability to other settings. The palliative care system in Thailand is different from other countries. With no standardized system, each region and hospital has their own distinct system, which may vary to a very large extent. Second, our ED only provides care for very high-acuity patients triaged as level 1 or 2, thereby underestimating the proportion of patients with unavoidable visits. Thirdly, we collected the data from the persons who came to the ED with the patients, some of whom might not have been the primary caregivers. Lastly, there were still some missing data from the questionnaire completed via in-person interview, which might have been caused by such a lengthy and detailed questionnaire. Further studies should thus emphasize on optimizing the format and length of the questionnaire and also the training of the interviewers.
Conclusion
Approximately half of all palliative patients who visited the ED were non-cancer patients. The most common presenting symptom was shortness of breath, and the main reason for ED visits was an inability to control the symptoms. The patients and their caregivers still had limited and discordant understanding and perceptions. More importantly, the recognition and utilization of palliative care were largely inadequate, especially for patients without cancer. Therefore, an improvement and promotion in the palliative care system from the ED through home care as well as in-hospital services are mandatory to improve the quality of life of palliative patients.
Availability of data and materials
The dataset is not available but can be requested from the corresponding author.
Abbreviations
- ED:
-
Emergency Department
- ESI:
-
Emergency Severity Index
- PPS:
-
Palliative performance score
- SD:
-
Standard deviation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Lowery DS, Quest TE. Emergency medicine and palliative care. Clin Geriatr Med. 2015;31(2):295–303.2.
Verhoef MJ, de Nijs E, Horeweg N, Fogteloo J, Heringhaus C, Jochems A, et al. Palliative care needs of advanced cancer patients in the emergency department at the end of life: an observational cohort study. Support Care Cancer. 2020;28(3):1097–107.
Burge F, Lawson B, Johnston G. Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care. 2003;41(8):992–1001.
Oh TK, Jo YH, Choi JW. Associated factors and costs of avoidable visits to the emergency department among cancer patients: 1-year experience in a tertiary care hospital in South Korea. Support Care Cancer. 2018;26(11):3671–9.
Alsirafy SA, Raheem AA, Al-Zahrani AS, Mohammed AA, Sherisher MA, El-Kashif AT, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2016;33(7):658–62.
Delgado-Guay MO, Kim YJ, Shin SH, Chisholm G, Williams J, Allo J, et al. Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage. 2015;49(3):497–504.
Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253–6.
Taylor P, Stone T, Simpson R, Kyeremateng S, Mason S. Emergency department presentations in palliative care patients: a retrospective cohort study. BMJ Support Palliat Care. 2022. https://doi.org/10.1136/bmjspcare-2022-003563.
Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6):563–8.
Henson LA, Higginson IJ, Daveson BA, Ellis-Smith C, Koffman J, Morgan M, et al. “I’ll be in a safe place”: a qualitative study of the decisions taken by people with advanced cancer to seek emergency department care. BMJ Open. 2016;6(11):e012134.
Raijmakers N, Galushko M, Domeisen F, Beccaro M, LundhHagelin C, Lindqvist O, et al. Quality indicators for care of cancer patients in their last days of life: literature update and experts’ evaluation. J Palliat Med. 2012;15(3):308–16.
Cooper E, Hutchinson A, Sheikh Z, Taylor P, Townend W, Johnson MJ. Palliative care in the emergency department: a systematic literature qualitative review and thematic synthesis. Palliat Med. 2018;32(9):1443–54.
Lawson BJ, Burge FI, Mcintyre P, Field S, Maxwell D. Palliative care patients in the emergency department. J Palliat Care. 2008;24(4):247.
Wu FM, Newman JM, Lasher A, Brody AA. Effects of initiating palliative care consultation in the emergency department on inpatient length of stay. J Palliat Med. 2013;16(11):1362–7.
da Costa Rosa KS, de Paiva Cypriano R, Albuquerque NM, de Oliveira LC. Predictive factors of death on hospitalization in patients with advanced cancer in palliative care. Am J Hosp Palliat Care. 2021;38(10):1189–94.
National Health Commission Office. National Health Act Thailand (2007). Nonthaburi: National Health Commission Office; 2007.
Gilboy N, Tanabe P, Travers DA, Rosenau AM, Eitel DR. Emergency Severity Index, version 4: implementation handbook. Rockville: AHRQ Publication; 2005.
Teuteberg Jeffrey J, Teuteberg Winifred G. Palliative care for patients with heart failure - American College of Cardiology. [update 2016 Feb 11; cited 2022 Apr 6]. Available from: https://www.acc.org/latest-in-cardiology/articles/2016/02/11/08/02/palliative-care-for-patients-with-heart-failure.
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–6.
Cohen RG. End-stage lung disease | The patient guide to heart, lung, and esophageal surgery. [update 2016 July; cited 2022 Apr 6]. Available from: https://ctsurgerypatients.org/lung-esophageal-and-other-chest-diseases/end-stage-lung-disease.
Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative performance scale (PPS): a new tool. J Palliat Care. 1996;12(1):5–11.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Spilsbury K, Rosenwax L, Arendts G, Semmens JB. The association of community-based palliative care with reduced emergency department visits in the last year of life varies by patient factors. Ann Emerg Med. 2017;69(4):416–25.
Wong J, Gott M, Frey R, Jull A. What is the incidence of patients with palliative care needs presenting to the emergency department? a critical review. Palliat Med. 2014;28(10):1197–205.
Hirvonen OM, Alalahti JE, Syrjänen KJ, Jyrkkiö SM. End-of-life decisions guiding the palliative care of cancer patients visiting emergency department in south western Finland: a retrospective cohort study. BMC Palliat Care. 2018;17(1):1–8.
Kunakornvong W, Ngoasri K. Public awareness and attitude toward palliative care in Thailand. Siriraj Med J. 2020;72(5):424–30.
Sittisombut S, Maxwell C, Love EJ, Sitthi-Amorn C. Physicians’ attitudes and practices regarding advanced end-of-life care planning for terminally ill patients at Chiang Mai university hospital. Thailand Nurs Health Sci. 2009;11(1):23–8.
Srinonprasert V, Manjavong M, Limpawattana P, Chotmongkol V, Pairojkul S, Chindaprasirt J, et al. A comparison of preferences of elderly patients for end-of-life period and their relatives’ perceptions in Thailand. Arch Gerontol Geriatr. 2019;84.
Wang DH. Beyond code status: palliative care begins in the emergency department. Ann Emerg Med. 2017;69(4):437–43.
Martina D, Lin CP, Kristanti MS, Bramer WM, Mori M, Korfage IJ, et al. Advance care planning in Asia: a systematic narrative review of healthcare professionals’ knowledge, attitude, and experience. J Am Med Dir Assoc. 2021;22(2):349.e1–349.e28.
Acknowledgements
Not applicable.
Funding
The study received financial support from Siriraj Research and Development Fund.
Author information
Authors and Affiliations
Contributions
AM and OR conceived the study and designed the trial. AM, TC, and PC supervised the conduct of the trial. AM, TC, NP, US, CL, and WC completed the data collection. OR, TC and AM managed the data. OR and AM analyzed the data and drafted the article. OR takes responsibility for the paper as a whole. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Siriraj Institutional Review Board (certificate of approval Si 091/2019). Written informed consent was provided by all participants before the study inclusion. The study was conducted in accordance with the Declaration of Helsinki and adhered to Good Clinical Practice guidelines.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Additional patients’ characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Monsomboon, A., Chongwatcharasatit, T., Chanthong, P. et al. Characteristics and factors associated with mortality in palliative patients visiting the Emergency Department of a large tertiary hospital in Thailand. BMC Palliat Care 21, 115 (2022). https://doi.org/10.1186/s12904-022-01009-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-022-01009-z