Abstract
Objectives
To investigate the potential mechanisms of shikonin in preventing and treating periodontitis using network pharmacology and molecular docking methods.
Materials and methods
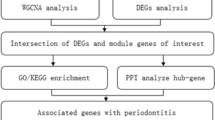
The targets of shikonin were obtained in TCMSP and SEA databases, and targets of periodontitis were gathered from the OMIM, GeneCards and Drugbank Databases. The intersecting targets were entered into the DAVID database to obtain the relevant biological functions and pathways by GO and KEGG enrichment analysis. The obtained targets were analysed the protein–protein interaction (PPI) in STRING platform. In Cytoscape 3.8.0, the network analysis function with the MCODE plug-in were used to obtain the key targets, of shikonin and periodontitis. Molecular docking and molecular dynamics simulation (MD) were used to assess the affinity between the shikonin and the key targets.
Results
Shikonin was screened for 22 targets and periodontitis was screened for 944 targets, the intersecting targets were considered as potential therapeutic targets. The targets played important roles in cellular response to hypoxia, response to xenobiotic stimulus and positive regulates of apoptotic process by GO enrichment analysis. 10 significant pathways were analyzed by KEGG, such as human cytomegalovirus infection and PI3K-Akt signaling pathway, etc. Cytoscape software screened the key genes including AKT1, CCL5, CXCR4, PPARG, PTEN, PTGS2 and TP53. Molecular docking and MD results showed that shikonin could bind stably to the targets.
Conclusions
The present study enriched the molecular mechanisms in periodontitis with shikonin, providing potential therapeutic targets for periodontitis.
Similar content being viewed by others
Introduction
Periodontitis, an inflammatory disease in periodontal tissues, is a chronic infectious disease which influenced by multiple factors. In the 2019 Global Burden of Disease (GBD) Study, the global prevalence, age-standardised rate (ASR) and estimated annual percentage changes (EAPCs) of periodontitis showed an increasing trend [1, 2]. There were 1,087,367,744.0 cases (including 91,518,820.6 new cases) of periodontitis globally in 2019 [2]. China's fourth national oral health survey showed that the prevalence of periodontal disease among people over 35 years was 82.6%—88.4% [3]. Therefore, periodontitis is a globally important public health problem, and its prevention and treatment are urgent. Periodontitis is the invasion of gingival tissues with bacteria and periodontal pathogens [4]. Periodontitis is referred to as a ‘mixed bacterial infection’, and it often leads to gum tissue damage and tooth loss [5, 6]. The common causative organisms including porphyromonas gingivalis [7], tannerella forsythia [8], treponema denticola [9], fusobacterium nucleatum [10] and aggregatibacter actinomycetemcomitans [11], which produce vasoactive amines [12], tumor necrosis factor-alpha (TNF-α), Interleukin-1β (IL-1β), prostaglandin E2 and matrix metalloproteinases (MMPs). Then the factors lead to irreversible destruction of the alveolar bone and periodontal ligaments [13]. In addition, periodontitis is an important risk factor for other systemic diseases [14], such as diabetes [15], cardiovascular disease [16], non-alcoholic fatty liver disease [17], Alzheimer's disease [18], cancer [19]. During periodontal infection, pathogenic microorganisms can easily spread into the circulation through the ulcerated epithelium of the deep periodontal pockets, affecting other tissues and organs [20, 21]. People with periodontitis are more likely to suffer from heart disease, hypertension, atherosclerosis and immune diseases (arthritis) [20]. Periodontitis also increases mortality in chronic kidney disease. Numerous studies have found that periodontitis increases the incidence of cancer. For example, periodontitis reduce alveolar bone 1 mm will lead to a fivefold increase in the incidence rate of tongue cancer [21]. Common clinical symptoms of periodontitis including swollen and bleeding gums, toothache, loose and shifting tooth, and even tooth loss [13]. The treatments for periodontitis including basic, surgical and pharmacological treatments [12, 22]. Basic treatment consists of oral hygiene instructions [23], supragingival scaling [24], subgingival scaling [25] and root planing [26]. Surgical treatments include flap procedures [27, 28], gingivoplasty [28, 29], gingivectomy [28], and guided tissue regeneration [30]. Since surgical treatment requires to considerate the tolerance of patients. Drugs are uesd to reduce and eliminate the infection in periodontitis [31], with antibiotics [32] and non-steroidal anti-inflammatory drugs [33]. However, antibiotics and other drugs are often associated with resistance and adverse effects, such as gastrointestinal tract dysfunction and the damage in liver and kidney [34, 35]. The use of natural compounds (natural medicines) is a viable treatment option for periodontitis as they have lower adverse effects. In addition, the natural compounds have shown great therapeutic effects in multiple diseases [36,37,38].
Shikonin (SHI) is an active ingredient from a traditional Chinese medicinal herb: Lithospermum erythrorhizon. Shikonin has be well-defined anti-microbial [39, 40], anti-inflammatory [41] and anti-tumour effects [42,43,44]. It was found that shikonin reduced the expression of IL-1β, IL-6 and TNF-α in the human periodontal ligament cells (hPDLCs) inflammation model [45]. Furthermore, shikonin can inhibit osteoclast differentiation, enhance bone mesenchymal stem cells, achieve bone regeneration and repair bone defects in periodontitis [46]. Numerous studies found that shikonin had beneficial effects in periodontitis, but its specific mechanism need to be further explored.
Network pharmacology integrates systems biology, pharmacology, computer-based virtual laboratory simulations and network topology analysis to assess the pharmacological effects at multiple levels and directions [47, 48]. In order to obtain relevant targets and potential mechanisms of diseases and drugs, network pharmacology is widely used to assist the research in various diseases [49, 50]. Molecular docking is a computer simulation technique which can explain the interactions between ligands and proteins [51,52,53]. In this study, the potential mechanisms and targets of shikonin in periodontitis were analysed by network pharmacology, molecular docking and MD.
Materials and methods
Gene dataset acquisition of shikonin and periodontitis
Target genes of shikonin were gathered from two databases: Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform Database (https://tcmsp-e.com/) and Similarity Ensemble Approach (SEA) Database (https://sea.bkslab.org/). Target genes of periodontitis were gathered from three databases, including the Online Mendelian Inheritance in Man Database (http://www.omim.org/), GeneCards Database(https://www.genecards.org/) and Drugbank Database (https://go.drugbank.com) with “Periodontitis” as the keyword.
GO analysis and KEGG pathway enrichment analysis
DAVID Bioinformatics Database (https://david.ncifcrf.gov) have a variety of functions, such as gene annotation, online analysis, functional enrichment, interactive analysis, etc. It also contains the Kyoto Encyclopedia of Genes and Genomes (KEGG) database and GO database. The analysis of KEGG can provide a access for biological functions and relevant candidate targets. GO enrichment can analysis the biological process (BP), molecular function (MF) and cellular component (CC). The targets of shikonin and periodontitis were imported into the DAVID database, and "Homo sapiens" was used as the selected condition to obtain the biological functions and important targets.
Construction of protein–protein interaction network
The STRING database (https://string-db.org/) bases on their network topological features to provide a intuitive access for the dynamic network of proteins. shikonin and periodontitis targets were imported into an online Veen diagram platform to obtain the overlapping genes. The obtained target genes were imported into the STRING platform to analyse the protein–protein interaction (PPI) with the "Homo sapiens" and confidence level of 0.9 as the screening condition.
Network construction
Cytoscape software performs visual analyses to obtain inner associations between genes based on network topology features [54]. Genes obtained by Cytoscape software may be pivotal genes for shikonin to treat periodontitis.
Molecular docking
Molecular docking can predict the binding mechanism and activity between molecules and relevant targets [55]. The molecular structure of shikonin was obtained from the PubChem database (https://pubchem.ncbi.nlm.nih.gov/). Protein kinase B (AKT1, PDB ID: 6HHH), C–C chemokine ligand 5 (CCL5, PDB ID: 6AEZ), C-X-C chemokine receptor type 4 (CXCR4, PDB ID: 3ODU), Peroxisome proliferator-activated receptor gamma (PPARG, PDB ID: 6FZG), Phosphatase and tensin homolog (PTEN, PDB ID: 1D5R), Prostaglandin-endoperoxide synthase 2 (PTGS2, PDB ID: 5F19) and Cellular tumor antigen p53 (TP53, PDB ID: 7LIN) in PDB format were obtained from the Protein Data Bank (https://www.rcsb.org/). BIOVIA Discovery Studio Visualizer 2021 was used to screening active ingredients and preparing proteins [56]. After removing the crystalline water molecules and replenishing incomplete amino acid residues, using LibDockScore to assess the affinity between the shikonin and the targets. In addition, Pymol software [57], a sub-software of python software, was used to process and analyse the molecular docking results [55, 58].
Molecular dynamic simulation
Molecular dynamics simulation (MD) was perfored by GROMACS 2023 software package [59]. The protein and ligand used the CHARMM 36 and GAFF2 force field parameter. Using periodic boundary conditions, the protein–ligand complexes were placed in a cubic box with a boundary of 12 Å, and water molecules were filled into the box using the TIP3P water model. Using the steepest descent method, the system was be optimized at 50000 steps. The system was gradually heated in NVT ensemble, then subjected to NPT. Van-der-Waals and Coulomb interactions were calculated(1.0 nm). 100 ns molecular dynamics simulations were performed with a time step of 2 fs (constant temperature:300 K and constant pressure:1 bar) [60].
Results
Gene targets of shikonin
Twenty-two targets were obtained from the TCMSP database, and the SEA database retrieved 10 target genes. A total of 22 target genes was identified (Supplementary Table 1: The 22 target genes of shikonin).
Gene targets of periodontitis
Target genes of periodontitis were gathered from three databases, 11 in OMIM, 935 in GeneCards Database and 14 in Drugbank Database. A total of 944 gene targets were identified in periodontitis (Supplementary Table 2: The 944 genes were associated with periodontitis).
GO and KEGG enrichment analysis
The common target genes of shikonin and periodontitis were imported into the DAVID database for GO and KEGG analysis (Fig. 1a). The respective top enriched terms of BP, CC, and MF were presented in Fig. 1b. The results of GO enrichment analysis indicated that the targets were involved in many important biological functions. In the biological process category, targets played important roles in cellular response to hypoxia, response to xenobiotic stimulus and positive regulates of apoptotic process. In the cellular component category, including enzyme binding, identical protein binding and protein kinase binding. We performed KEGG pathway analysis to retrieve 10 significant pathways (P < 0.05), such as human cytomegalovirus infection, lipid and atherosclerosis, human papillomavirus infection and PI3K-Akt signaling pathway, etc. (Fig. 1c). Based on the above analysis, we knowed that the treatment of shikonin in periodontitis may be associated with inhibition of inflammation.
Construction of PPI network and cytoscape network
The overlapping genes of shikonin and periodontitis were imported into the STRING database to produce PPI network and obtain protein information (Fig. 2a and b, Table 1). Based on the network topological features, the graph information in PPI network was imported into Cytoscape software to screen the key nodes, then revealing the key target genes including AKT1, CCL5, CXCR4, PPARG, PTEN, PTGS2 and TP53 (Fig. 2c).
Molecular docking
To validate the findings of Network Pharmacology, molecular docking was used to assess the binding relationship between shikonin and the targets. The 7 targets (AKT1, CCL5, CXCR4, PPARG, PTEN, PTGS2, TP53) obtained from the PPI network and Cytoscape, and the docking results were shown in Table 2 and Fig. 3. Shikonin bound to AKT1 (6HHH) by 1 hydrogen bonds between it and SER-205. Shikonin bound to CCL5 (6AEZ) by 4 hydrogen bonds between it and ILE-16, LYS-56 and ASN-53. Shikonin bound to CXCR4 (3ODU) by 5 hydrogen bonds with ASN-1055, LEU1013, LEU1015 and LYS-1016. Shikonin bound to PPARG (6FZG) by 1 hydrogen bonds between it and TYR-355. Shikonin bound to PTEN (1D5R) by 1 hydrogen bonds between it and GLN-171. Shikonin bound to PTGS2 (5F19) by 1 hydrogen bonds between it and ALA-219. Shikonin bound to TP53 (7LIN) by 2 hydrogen bonds between it and ASP-63. The binding energies of ligand and receptors were -6.37 kcal/mol (AKT1), -6.12 kcal/mol (CCL5), -3.89 kcal/mol (CXCR4), -4.23 kcal/mol (PPARG), -4.25 kcal/mol (PTEN), -4.55 kcal/mol (PTGS2), -4.13 kcal/mol (TP53). It is generally accepted that binding energies less than -1.19 kcal/mol indicate that docking between ligand and receptor is feasible [61]. Binding energies less than -5 kcal/mol indicate good binding activity between ligand and receptor. Based on the docking results, we concluded that shikonin binds well to AKT1 and CCL5. The docking results were imported into PyMOL for preprocessing, as shown in Fig. 3.
Molecular docking diagrams of related targets in shikonin and periodontitis. a Molecular docking of AKT1 and shikonin. b Molecular docking of CCL5 and shikonin. c Molecular docking of CXCR4 and shikonin. d Molecular docking of PPARG and shikonin. e Molecular docking of PTEN and shikonin. f Molecular docking of PTGS2 and shikonin. g Molecular docking of TP53 and shikonin
molecular dynamic simulation
Based on the docking results, we concluded that shikonin has great binding ability with AKT1 and CCL5. We verified the binding ability between comedones and key target proteins by molecular dynamics simulation (MD). The equilibration of the simulation system was assessed using RMSD. The complex shikonin/CCL5 and shikonin/akt reached stability after about 10 ns. RMSD results also showed that shikonin/CCL5 has relatively high stability compared to shikonin/akt (Fig. 4a). In addition, the Radius of Gyration (Rg) can be used to describe the overall structural changes and the compactness of the protein structure. The shikonin/CCL5 complex had lower Rg than shikonin/akt (Fig. 4b). The results indicated that the Rg of shikonin/CCL5 is more likely to be stabilised at lower values and is more structurally stable. Therefore, the compound may directly bind to the CCL5 protein to exert its pharmacological effects.
Discussion and future prospects
The Federation Dentaire Internationale (FDI) reported that periodontitis is a common chronic infectious disease with a global prevalence of 50 percent [62]. It is always known that severe periodontitis can lead to impaired chewing dysfunction, tooth loss and facial collapse [13, 63, 64]. In modern medicine, in order to manage and cure periodontitis, dentists should start from reducing the risk factors, suppressing the etiology and improving the treatment plan of periodontitis. In 2020, the European Federation of Periodobology (EFP) published clinical guidelines for the treatment of periodontitis including Stage I, Stage II. and Stage III. Mild to moderate cases of periodontitis (Stage I, II.) should be treated as early as possible, such as home care, scaling, root planing and antibiotic therapy [26, 65]. Severe cases of periodontitis, teeth with periodontal pocket depth (PD) ≥ 6 mm after Stage I and Stage II treatment, require surgical treatment and adjunctive systemic antibiotics [66,67,68].
Clear diagnosis, reduction of risk factors, improvement of home care education, and effective treatments are the keys of clinical prevention and treatment in periodontitis. The non-surgical treatment methods for periodontitis include home care education, tooth cleaning, root planing, and medication, which can improve the symptoms of periodontitis [69]. But there are some shortcomings in scaling, polishing, root planing, and drugs [70]. Frequent scaling and polishing can increase the sensitivity of teeth. Due to the effects of pacemakers, blood disorders and oral anticoagulants, scaling and root planing may be contraindicated for some people. In addition, there is an increased risk of infectious diseases if the healthcare environment is unsafe. Numerous studies have reported that drug therapy is also one of the main non-surgical treatments, mainly using antibiotics such as nitroimidazole, tetracycline, macrolide, and nonsteroidal anti-inflammatory drugs, which have significant therapeutic effects [69, 71, 72]. However, long-term drug treatment can also lead to drug resistance, dysbiosis, bone loss and other adverse reactions [70]. Chlorhexidine is a common clinical mouthwash that can reduce plaque, but it has some side effects [34]. For example, allergic reactions, tooth staining and harmful effects on host cells [34]. Surgical treatment can cause tooth loss and reduce tooth survival [73]. Removal of periodontal surgery may cause dentin hypersensitivity, food impaction, and aesthetic problems [74]. In addition, surgical treatment will also increase the incidence rate of oral cancer [21].
Pathogens infecting periodontal tissue or the oral cavity can stimulate T-cell activation, produce inflammatory factors, decrease leukocyte activity and increase the inflammatory response [75]. Therefore, eliminating or controlling the inflammation of periodontal tissues to promote cell homing and tissue repair is one of the main treatments for periodontitis [76]. Traditional Chinese medicine also has good effects in treating oral diseases such as periodontitis. In a clinical randomized controlled trial with oral mucosal inflammation, it was found that the traditional Chinese medicine group can significantly improve oral mucosal dryness, alleviate pain and inflammation [77]. Specific herbal mouthwashes also have an inhibitory effect on plaque and inflammation in periodontitis [78]. Numbers of natural compounds have been shown as low side effects and adverse effects [79,80,81]. A study reported that Trans-cinnamic aldehyde inhibited the inflammatory factors and reduced bone loss in periodontitis [82]. β-carotene can inhibit the progression of periodontitis by inhibiting nuclear factor kappa-B (NF-κB) activity and reducing the inflammatory cytokines [83]. Notopterol reduces the release of inflammatory mediators and reactive oxygen species in periodontitis by regulating NF-κB /Akt signaling [84, 85]. Resveratrol, psoralen and angelicin can reduce inflammation in periodontitis [86]. In addition, the combination of natural compounds and existing treatment methods can achieve better results in treating periodontitis, such as increasing anti-inflammatory and antibacterial effects, shortening treatment courses, and reducing recurrence rates. The combination of anthocyanins and Secnidazole can reduce the pathogenic bacteria in periodontitis [84]. The combination of curcumin and chlorhexidine can also alleviate symptoms in patients with periodontitis [87].
Shikonin is an active compound, and its anti-inflammatory effects have been demonstrated in the treatment of various diseases [88, 89]. The anti-inflammatory effects of shikonin in periodontitis have also received a lot of attention. In 2016, Satoru Shindo et al. [39] demonstrated that shikonin had a therapeutic effect on periodontitis for the first time. In vitro, a periodontitis model was constructed by stimulating HPDLC with IL-1β and TNF-α, and shikonin significantly reduced the expression of IL-6, IL-18, and cysteine-cysteine motif chemokine ligand 20 (CCL20) [39]. A study also found that the high levels of inflammatory cytokines, matrix metalloproteinase-2 (MMP-2), MMP-9, and cyclooxygenase-2 (COX-2) produced by LPS stimulation in hPDLC were also reversed by shikonin [45]. In addition, shikonin can promote the proliferation and migration of human gingival fibroblasts (hGF), stimulate the expression of osteopontin (OPN) and osteogenic differentiation to repair bone and periodontal tissues [90]. A study also reported that Shikonin can act as a specific inhibitor of PKM2, inhibiting osteoclastogenesis and alleviating bone loss in periodontitis [91].
The efficacy of shikonin in periodontitis has been well reported, however, the specific mechanisms are not clear. In this study, network pharmacology was used to explore the relationship between shikonin and periodontitis. The KEGG enrichment analysis was used to enrich for targets of shikonin and periodontitis, and obtained that the signalling pathways which related with inflammatory and infectious diseases. The PPI network was analysed by Cytoscape and obtained key targets, including AKT1, CCL5, CXCR4, PPARG, PTEN, PTGS2 and TP53. The relationships between shikonin and key targets were verified by molecular docking. Shikonin can treat rheumatoid arthritis [92], kidney injury [93], cancer [94],and myocardial ischaemia–reperfusion injury [95] by inhibiting the PI3K-Akt signalling pathway. It was found that shikonin can induce apoptosis in Burkitt's lymphoma by inhibiting the phosphatidylinositide 3-kinase (PI3K)/AKT/mammalian target of rapamycin (mTOR) pathway [96]. Shikonin also protected the dental pulp by stimulating differentiation of dental pulp stem cells (DPSCs) via the AKT-mTOR signalling pathway [97]. Shikonin inhibited the expression of CCL5 [98] and CXCR4 [99] and suppressed the proliferation of neutrophils in chronic granulocytic leukaemia. Shikonin attenuated oxidative stress, apoptosis,and neuroinflammation in Parkinson's disease [100] and renal impairment disorders [93] by the Akt/Extracellular regulated protein kinases (ERK)/c-Jun N-terminal kinase (JNK)/NF-κB pathway. A Study reported that shikonin may act as an antagonist of PPARγ to inhibit lipogenesis [101], which involved in the treatment of type 2 diabetes [102], fatty liver disease [103] and obesity. LPS induced the upregulated expression of PTEN and p-AKT, but shikonin reversed the phenomenon [104, 105]. Furthermore, It had been demonstrated that the key targets (AKT1 [106], CCL5 [107], CXCR4 [108], PPARG [109], PTEN [106], PTGS2 [110, 111] and TP53 [112, 113]) had a close association with periodontitis.
As is well known, traditional Chinese medicine works on diseases through multiple targets and pathways. We topologically analyzed on the protein–protein interaction network using Cytoscape to construct a network (active ingredients-common targets) [114]. Combining literature and KEGG Map information, CCL5 and AKT are correlated with inflammatory responses in the toll-like receptor signaling pathway (map04620). The virus binds to CCL5 or CXCR4 receptors, activating downstream AKT pathways, leading to inflammation or apoptosis reactions (map05170). It was found that cordycepin attenuated inflammation and apoptosis by inhibiting the Akt/NF-κB signaling pathway mediated by CCL5 [115]. There is also a positive correlation between CCL5 and Akt in microglia and macrophages [116]. CXCR4 has been found to be an important inflammatory regulator in periodontitis, inhibiting inflammation and reducing pain by regulating the PI3K/Akt [117] and Akt/NF-κB [118] pathway. Bavachinin and cardamonin are natural components of traditional Chinese medicine. Bavachinin can alleviate inflammation, apoptosis, and oxidative stress in periodontitis by regulating PPARG/PI3K/AKT/ PTEN signaling [119, 120]. Cardamonin also has an anti-inflammatory effects on HPDLC,which was mediated by reducing the expression of CCL5 and PTGS2 [121]. In addition, it has been found that the correlation of Akt with PTGS2 in animal and cell studies of periodontitis [122, 123]. It can be seen that the targets analyzed by Cytoscape also have significant correlations with each other. Therefore, we speculate that shikonin can improve the periodontitis by targeting multiple targets.
Based on the docking results, we concluded that shikonin has great binding ability with AKT1 and CCL5. Based on the MD results, the complex shikonin/CCL5 and shikonin/akt reached stability after about 10 ns. RMSD results also showed that shikonin/CCL5 has relatively high stability compared to shikonin/akt. The shikonin/CCL5 complex had lower Rg than shikonin/akt. Therefore, we hypothesised that CCL5 and AKT are the targets of shikonin in periodontitis.
Although shikonin has not yet been applied in the clinical treatment of periodontitis, it has been widely used in other diseases. Clinical studies have found that shikonin can improve the symptoms of mild to moderate diaper dermatitis in children [124]. Shikonin can reduce the expression of serum inflammatory markers TNF-α in psoriasis patients and improve the skin barrier function [125, 126]. Shikonin also has therapeutic effects on wound healing and inflammatory reactions after anal fistula surgery [127]. Numerous clinical studies have confirmed that shikonin is safe and beneficial for clinical treatment. Therefore, there is also potential for the use of shikonin in periodontitis.
Periodontitis is an important oral disease for human health. Existing treatments have significant efficacy, but some side effects (such as drug resistance, imbalance of intestinal flora and adverse reactions) are accompanied. In recent years, Chinese herbs (natural compound components) have attracted attention for good therapeutic effects in periodontitis through multiple targets and pathways [81]. In clinical, animal and cellular studies, it has been found that shikonin has good anti-inflammatory effects in various diseases. In particular, shikonin also can promote hGF proliferation and migration, osteogenic differentiation. Therefore, the definite mechanism for shikonin needs to be explored in periodontitis. The results of this study enrich the pathways of shikonin in periodontitis, and identify potential targets (AKT1, CCL5, CXCR4, PPARG, PTEN, PTGS2 and TP53) for its anti-inflammatory effects. Performing molecular docking and molecular dynamic simulation to verify the results. A study have shown that when drugs (natural compounds) are incorporated into nanoparticle carriers can increase their antimicrobial activity in periodontitis [86]. Therefore, we speculate that natural compounds (shikonin) combine nanotechnology can bring good news for patients with periodontitis in the future. The present study enriches the connotation and the potential mechanism of shikonin in periodontitis. We will conduct experimental verification for our results in the future. Meanwhile, the results (targets) obtained in this study may be an important pivot in the prevention and treatment of periodontitis, in order to provide a rich foundation for future clinical treatment of periodontitis.
Conclusion
In this study, we investigated the mechanisms of shikonin in periodontitis and obtained the potential targets, including AKT1, CCL5, CXCR4, PPARG, PTEN, PTGS2, TP53. The results provided a new direction and a theoretical basis for the treatment of periodontitis, but the validation with network pharmacology and molecular docking still had some limitations. Experimental validation of the theoretical results will be the next step in our research.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- AKT:
-
Protein kinase B
- BP:
-
Biological process
- CCL5:
-
C–C chemokine ligand 5
- CC:
-
Cellular component
- CXCR4:
-
C-X-C chemokine receptor type 4
- COX-2:
-
Cyclooxygenase-2
- CCL20:
-
Cysteine-cysteine motif chemokine ligand 20
- DPSCs:
-
Dental pulp stem cells
- EFP:
-
European Federation of Periodobology
- hPDLCs:
-
Human periodontal ligament cells
- hGF:
-
Human gingival fibroblasts
- IL-1β:
-
Interleukin-1β
- MMPs:
-
Molecular dynamics simulation
- MD:
-
Matrix metalloproteinases
- MF:
-
Molecular function
- mTOR:
-
Mammalian target of rapamycin
- NF-κB:
-
Nuclear factor kappa-B
- OPN:
-
Osteopontin
- PD:
-
Pocket depth
- PPI:
-
Protein–protein interaction
- PPARG:
-
Peroxisome proliferator-activated receptor gamma
- PTEN:
-
Phosphatase and tensin homolog
- PTGS2:
-
Prostaglandin-endoperoxide synthase 2
- PI3K:
-
Phosphatidylinositide 3-kinase
- SHI:
-
Shikonin
- TP53:
-
Cellular tumor antigen p53
- TNF-α:
-
Tumor necrosis factor-alpha
References
Zhang X, et al. The global burden of periodontal diseases in 204 countries and territories from 1990 to 2019. Oral Dis. 2024;30(2):754–68.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9. Erratum in: Lancet. 2020 Nov 14;396(10262):1562. PMID: 33069326; PMCID: PMC7567026.
Zhang H, et al. The mechanism of the Shuang Bai Su Qing recipe in treating periodontitis based on network pharmacology and molecular docking technology. Medicine (Baltimore). 2023;102(44):e35139.
Zhou M, Graves DT. Impact of the host response and osteoblast lineage cells on periodontal disease. Front Immunol. 2022;11(13):998244. https://doi.org/10.3389/fimmu.2022.998244. PMID:36304447;PMCID:PMC9592920.
Hajishengallis G, Lamont RJ. Beyond the red complex and into more complexity: the polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Mol Oral Microbiol. 2012;27(6):409–19.
Pinto KP, et al. What Is the Microbial Profile in Persistent Endodontic Infections? A Scoping Review J Endod. 2023;49(7):786-798.e7.
Chen R, et al. Anti-Porphyromonas gingivalis nanotherapy for maintaining bacterial homeostasis in periodontitis. Int J Antimicrob Agents. 2023;61(6):106801.
Aravindraja C, Jeepipalli S, Duncan W, Vekariya KM, Bahadekar S, Chan EKL, Kesavalu L. Unique miRomics Expression Profiles in Tannerella forsythia-Infected Mandibles during Periodontitis Using Machine Learning. Int J Mol Sci. 2023;24(22):16393. https://doi.org/10.3390/ijms242216393. PMID:38003583;PMCID:PMC10671577.
Kwon D, et al. Treponema denticola as a prognostic biomarker for periodontitis in dogs. PLoS ONE. 2022;17(1):e0262859.
Zhou LJ, et al. Periodontitis exacerbates atherosclerosis through Fusobacterium nucleatum-promoted hepatic glycolysis and lipogenesis. Cardiovasc Res. 2023;119(8):1706–17.
Fine DH, Patil AG, Velusamy SK. Aggregatibacter actinomycetemcomitans (Aa) Under the Radar: Myths and Misunderstandings of Aa and Its Role in Aggressive Periodontitis. Front Immunol. 2019;16(10):728. https://doi.org/10.3389/fimmu.2019.00728. PMID:31040843;PMCID:PMC6476972.
Moraes RM, Schlagenhauf U, Anbinder AL. Outside the limits of bacterial viability: Postbiotics in the management of periodontitis. Biochem Pharmacol. 2022;201:115072. https://doi.org/10.1016/j.bcp.2022.115072. Epub 2022 May 2 PMID: 35513043.
Kwon T, Lamster IB, Levin L. Current Concepts in the Management of Periodontitis. Int Dent J. 2021;71(6):462–76.
Teles F, et al. Viruses, periodontitis, and comorbidities. Periodontol 2000. 2022;89(1):190–206.
Simpson TC, et al. Treatment of periodontitis for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev. 2022;4(4):CD004714.
Naderi S, Merchant AT. The Association Between Periodontitis and Cardiovascular Disease: an Update. Curr Atheroscler Rep. 2020;22(10):52.
Kuraji R, et al. Periodontal disease-related nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: An emerging concept of oral-liver axis. Periodontol 2000. 2021;87(1):204–40.
Lu J, et al. Periodontitis-related salivary microbiota aggravates Alzheimer’s disease via gut-brain axis crosstalk. Gut Microbes. 2022;14(1):2126272.
Ding M, et al. Association between periodontitis and breast cancer: two-sample Mendelian randomization study. Clin Oral Investig. 2023;27(6):2843–9.
Ray RR. Periodontitis: An Oral Disease with Severe Consequences. Appl Biochem Biotechnol. 2023;195(1):17–32.
Komlós G, et al. Periodontitis as a risk for oral cancer: a case-control study. BMC Oral Health. 2021;21(1):640.
Swarnamali H, Medara N, Chopra A, Spahr A, Jayasinghe TN. Role of Dietary Fibre in Managing Periodontal Diseases-A Systematic Review and Meta-Analysis of Human Intervention Studies. Nutrients. 2023;15(18):4034. https://doi.org/10.3390/nu15184034. PMID:37764817;PMCID:PMC10536522.
Mueller M, et al. Relationship between dental experiences, oral hygiene education and self-reported oral hygiene behaviour. PLoS ONE. 2022;17(2):e0264306.
Haas AN, et al. New tendencies in non-surgical periodontal therapy. Braz Oral Res. 2021;35(Supp 2):e095.
Oliveira LM, de Oliveira CA, Angst PDM, Antoniazzi RP, Zanatta FB. Should supragingival scaling be performed separately prior to subgingival scaling and root planning in nonsurgical periodontal therapy? A systematic review of randomized trials. Int J Dent Hyg. 2024;22(1):35–44. https://doi.org/10.1111/idh.12731. Epub 2023 Sep 3 PMID: 37661290.
Cobb CM, Sottosanti JS. A re-evaluation of scaling and root planing. J Periodontol. 2021;92(10):1370–8.
Zuhr O, et al. Surgery without papilla incision: tunneling flap procedures in plastic periodontal and implant surgery. Periodontol 2000. 2018;77(1):123–49.
Kajimoto NC, et al. Gingival fenestration defect treated with gingivectomy and gingivoplasty: A case report with an 8-year follow-up. Clin Adv Periodontics. 2023;13(2):102–5.
Mazzotti C, et al. Soft-tissue dehiscence coverage at peri-implant sites. Periodontol 2000. 2018;77(1):256–72.
Liu Y, et al. Challenges and Tissue Engineering Strategies of Periodontal-Guided Tissue Regeneration. Tissue Eng Part C Methods. 2022;28(8):405–19.
Chatzopoulos GS, Koidou VP, Tsalikis L. Local drug delivery in the treatment of furcation defects in periodontitis: a systematic review. Clin Oral Investig. 2023;27(3):955–70.
Abullais SS, et al. Synergistic antibacterial activity of herbal extracts with antibiotics on bacteria responsible for periodontitis. J Infect Dev Ctries. 2021;15(11):1685–93.
Ren J, et al. The role of non-steroidal anti-inflammatory drugs as adjuncts to periodontal treatment and in periodontal regeneration. J Transl Med. 2023;21(1):149.
Poppolo DF, Ouanounou A. Chlorhexidine in Dentistry: Pharmacology, Uses, and Adverse Effects. Int Dent J. 2022;72(3):269–77.
Rajeshwari HR, Dhamecha D, Jagwani S, Rao M, Jadhav K, Shaikh S, Puzhankara L, Jalalpure S. Local drug delivery systems in the management of periodontitis: A scientific review. J Control Release. 2019;307:393–409. https://doi.org/10.1016/j.jconrel.2019.06.038. Epub 2019 Jun 27 PMID: 31255689.
Taylor E, Kim Y, Zhang K, Chau L, Nguyen BC, Rayalam S, Wang X. Antiaging Mechanism of Natural Compounds: Effects on Autophagy and Oxidative Stress. Molecules. 2022;27(14):4396. https://doi.org/10.3390/molecules27144396. PMID:35889266;PMCID:PMC9322024.
Ng MY, Lin T, Chao SC, Chu PM, Yu CC. Potential Therapeutic Applications of Natural Compounds in Diabetes-Associated Periodontitis. J Clin Med. 2022;11(13):3614. https://doi.org/10.3390/jcm11133614. PMID:35806899;PMCID:PMC9267692.
Fakheran O, Khademi A, Bagherniya M, Sathyapalan T, Sahebkar A. The Effects of Nutraceuticals and Bioactive Natural Compounds on Chronic Periodontitis: A Clinical Review. Adv Exp Med Biol. 2021;1328:59–80. https://doi.org/10.1007/978-3-030-73234-9_5. PMID: 34981471.
Shindo S, et al. Shikonin Inhibits Inflammatory Cytokine Production in Human Periodontal Ligament Cells. Inflammation. 2016;39(3):1124–9.
Kumar A, Shashni S, Kumar P, Pant D, Singh A, Verma RK. Phytochemical constituents, distributions and traditional usages of Arnebia euchroma: A review. J Ethnopharmacol. 2021;271:113896. https://doi.org/10.1016/j.jep.2021.113896. Epub 2021 Jan 29 PMID: 33524510.
Liang Y, Ju D, Liu W, Wu D, Zhao Y, Du Y, Li X, Zhao M. Natural Shikonin Potentially Alters Intestinal Flora to Alleviate Acute Inflammation. Microorganisms. 2023;11(9):2139. https://doi.org/10.3390/microorganisms11092139. PMID:37763983;PMCID:PMC10534322.
Guo C, He J, Song X, Tan L, Wang M, Jiang P, Li Y, Cao Z, Peng C. Pharmacological properties and derivatives of shikonin-A review in recent years. Pharmacol Res. 2019;149:104463. https://doi.org/10.1016/j.phrs.2019.104463. Epub 2019 Sep 22 PMID: 31553936.
Sun Q, Gong T, Liu M, Ren S, Yang H, Zeng S, Zhao H, Chen L, Ming T, Meng X, Xu H. Shikonin, a naphthalene ingredient: Therapeutic actions, pharmacokinetics, toxicology, clinical trials and pharmaceutical researches. Phytomedicine. 2022;94:153805. https://doi.org/10.1016/j.phymed.2021.153805. Epub 2021 Oct 24 PMID: 34749177.
Guo H, Sun J, Li D, Hu Y, Yu X, Hua H, Jing X, Chen F, Jia Z, Xu J. Shikonin attenuates acetaminophen-induced acute liver injury via inhibition of oxidative stress and inflammation. Biomed Pharmacother. 2019;112:108704. https://doi.org/10.1016/j.biopha.2019.108704. Epub 2019 Feb 25 PMID: 30818140.
Fan C, Zhang X, Upton Z. Anti-inflammatory effects of shikonin in human periodontal ligament cells. Pharm Biol. 2018;56(1):415–21.
Lohberger B, Kaltenegger H, Eck N, Glänzer D, Sadoghi P, Leithner A, Bauer R, Kretschmer N, Steinecker-Frohnwieser B. Shikonin Derivatives Inhibit Inflammation Processes and Modulate MAPK Signaling in Human Healthy and Osteoarthritis Chondrocytes. Int J Mol Sci. 2022;23(6):3396. https://doi.org/10.3390/ijms23063396. PMID:35328817;PMCID:PMC8955849.
Wang Y, Yuan Y, Wang W, He Y, Zhong H, Zhou X, Chen Y, Cai XJ, Liu LQ. Mechanisms underlying the therapeutic effects of Qingfeiyin in treating acute lung injury based on GEO datasets, network pharmacology and molecular docking. Comput Biol Med. 2022;145:105454. https://doi.org/10.1016/j.compbiomed.2022.105454. Epub 2022 Mar 26 PMID: 35367781.
Zhao L, Zhang H, Li N, Chen J, Xu H, Wang Y, Liang Q. Network pharmacology, a promising approach to reveal the pharmacology mechanism of Chinese medicine formula. J Ethnopharmacol. 2023;309:116306. https://doi.org/10.1016/j.jep.2023.116306. Epub 2023 Feb 27 PMID: 36858276.
Niu B, Xie X, Xiong X, Jiang J. Network pharmacology-based analysis of the anti-hyperglycemic active ingredients of roselle and experimental validation. Comput Biol Med. 2022;141:104636. https://doi.org/10.1016/j.compbiomed.2021.104636. Epub 2021 Jul 27 PMID: 34809966.
Zhang P, Zhang D, Zhou W, Wang L, Wang B, Zhang T, Li S. Network pharmacology: towards the artificial intelligence-based precision traditional Chinese medicine. Brief Bioinform. 2023;25(1):bbad518. https://doi.org/10.1093/bib/bbad518. PMID: 38197310; PMCID: PMC10777171.
Agu PC, et al. Molecular docking as a tool for the discovery of molecular targets of nutraceuticals in diseases management. Sci Rep. 2023;13(1):13398.
Oyewusi HA, Huyop F, Wahab RA. Molecular docking and molecular dynamics simulation of Bacillus thuringiensis dehalogenase against haloacids, haloacetates and chlorpyrifos. J Biomol Struct Dyn. 2022;40(5):1979–94.
Lu Z, et al. Network pharmacology and molecular docking approach to elucidate the mechanisms of Liuwei Dihuang pill in diabetic osteoporosis. J Orthop Surg Res. 2022;17(1):314.
Dong Y, Zhao Q, Wang Y. Network pharmacology-based investigation of potential targets of astragalus membranaceous-angelica sinensis compound acting on diabetic nephropathy. Sci Rep. 2021;11(1):19496.
Zhang MM, et al. Identification of the active substances and mechanisms of ginger for the treatment of colon cancer based on network pharmacology and molecular docking. BioData Min. 2021;14(1):1.
Azfaralariff A, Farahfaiqah F, Shahid M, Sanusi SA, Law D, Mohd Isa AR, Muhamad M, Tsui TT, Fazry S. Marantodes pumilum: Systematic computational approach to identify their therapeutic potential and effectiveness. J Ethnopharmacol. 2022;283:114751. https://doi.org/10.1016/j.jep.2021.114751. Epub 2021 Oct 15 PMID: 34662662.
Khan SA, et al. Network pharmacology and molecular docking-based prediction of active compounds and mechanisms of action of Cnidii Fructus in treating atopic dermatitis. BMC Complement Med Ther. 2022;22(1):275.
Zhang L, Han L, Wang X, Wei Y, Zheng J, Zhao L, Tong X. Exploring the mechanisms underlying the therapeutic effect of Salvia miltiorrhiza in diabetic nephropathy using network pharmacology and molecular docking. Biosci Rep. 2021;41(6):BSR20203520. https://doi.org/10.1042/BSR20203520. PMID: 33634308; PMCID: PMC8209169.
Feng S, et al. CHARMM-GUI Membrane Builder: Past, Current, and Future Developments and Applications. J Chem Theory Comput. 2023;19(8):2161–85.
Fu S, et al. Network pharmacology and molecular docking technology-based predictive study of the active ingredients and potential targets of rhubarb for the treatment of diabetic nephropathy. BMC Complement Med Ther. 2022;22(1):210.
Dong Y, et al. Molecular mechanism of Epicedium treatment for depression based on network pharmacology and molecular docking technology. BMC Complement Med Ther. 2021;21(1):222.
Liu X, Yang L, Tan X. PD-1/PD-L1 pathway: A double-edged sword in periodontitis. Biomed Pharmacother. 2023;159:114215. https://doi.org/10.1016/j.biopha.2023.114215. Epub 2023 Jan 9 PMID: 36630848.
Uy S, et al. Food intake, masticatory function, tooth mobility, loss of posterior support, and diminished quality of life are associated with more advanced periodontitis stage diagnosis. J Clin Periodontol. 2022;49(3):240–50.
Yuan H, et al. Assessment of early wound healing, pain intensity, quality of life and related influencing factors during periodontal surgery: a cross-sectional study. BMC Oral Health. 2022;22(1):596.
Herrera D, Sanz M, Kebschull M, Jepsen S, Sculean A, Berglundh T, Papapanou PN, Chapple I, Tonetti MS. EFP Workshop Participants and Methodological Consultant Treatment of stage IV periodontitis: The EFP S3 level clinical practice guideline. J Clin Periodontol. 2022;49(Suppl 24):4–71. https://doi.org/10.1111/jcpe.13639. PMID: 35688447.
Sanz M, et al. Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47(Suppl22):4–60.
Hagenfeld D, et al. Long-term changes in the subgingival microbiota in patients with stage III-IV periodontitis treated by mechanical therapy and adjunctive systemic antibiotics: A secondary analysis of a randomized controlled trial. J Clin Periodontol. 2023;50(8):1101–12.
Karrabi M, Baghani Z. Amoxicillin/Metronidazole Dose Impact as an Adjunctive Therapy for Stage II - III Grade C Periodontitis (Aggressive Periodontitis) at 3- And 6-Month Follow-Ups: a Systematic Review and Meta-Analysis. J Oral Maxillofac Res. 2022;13(1):e2.
Feres M, et al. Unraveling the effectiveness of antibiotics for peri-implantitis treatment: A scoping review. Clin Implant Dent Relat Res. 2023;25(4):767–81.
Yuan X, et al. Systemic antibiotics increase microbiota pathogenicity and oral bone loss. Int J Oral Sci. 2023;15(1):4.
Cope AL, et al. Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults. Cochrane Database Syst Rev. 2024;5(5):010136.
Cosgarea R, et al. Clinical, microbiological, and immunological effects of 3- or 7-day systemic antibiotics adjunctive to subgingival instrumentation in patients with aggressive (Stage III/IV Grade C) periodontitis: A randomized placebo-controlled clinical trial. J Clin Periodontol. 2022;49(11):1106–20.
Jepsen K, Sculean A, Jepsen S. Complications and treatment errors related to regenerative periodontal surgery. Periodontol 2000. 2023;92(1):120–34.
Roccuzzo A, et al. Clinical outcomes of dental implants in patients with and without history of periodontitis: A 20-year prospective study. J Clin Periodontol. 2022;49(12):1346–56.
Yang B, Pang X, Li Z, Chen Z, Wang Y. Immunomodulation in the Treatment of Periodontitis: Progress and Perspectives. Front Immunol. 2021;19(12):781378. https://doi.org/10.3389/fimmu.2021.781378. PMID:34868054;PMCID:PMC8640126.
Santonocito S, Ferlito S, Polizzi A, Ronsivalle V, Sclafani R, Valletta A, Lo Giudice A, Cavalcanti R, Spagnuolo G, Isola G. Therapeutic and Metagenomic Potential of the Biomolecular Therapies against Periodontitis and the Oral Microbiome: Current Evidence and Future Perspectives. Int J Mol Sci. 2022;23(22):13708. https://doi.org/10.3390/ijms232213708. PMID:36430182;PMCID:PMC9693164.
Wang C, et al. Efficacy of Traditional Chinese Medicine in Treatment and Prophylaxis of Radiation-Induced Oral Mucositis in Patients Receiving Radiotherapy: A Randomized Controlled Trial. Integr Cancer Ther. 2018;17(2):444–50.
Cai H, Chen J, Panagodage Perera NK, Liang X. Effects of Herbal Mouthwashes on Plaque and Inflammation Control for Patients with Gingivitis: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Evid Based Complement Alternat Med. 2020;20(2020):2829854. https://doi.org/10.1155/2020/2829854. PMID:32419797;PMCID:PMC7201456.
Salatin S, et al. Antimicrobial Benefits of Flavonoids and their Nanoformulations. Curr Pharm Des. 2022;28(17):1419–32.
Rahman MM, Sarker MT, Alam Tumpa MA, Yamin M, Islam T, Park MN, Islam MR, Rauf A, Sharma R, Cavalu S, Kim B. Exploring the recent trends in perturbing the cellular signaling pathways in cancer by natural products. Front Pharmacol. 2022;8(13):950109. https://doi.org/10.3389/fphar.2022.950109. PMID:36160435;PMCID:PMC9498834.
Petrocelli G, Marrazzo P, Bonsi L, Facchin F, Alviano F, Canaider S. Plumbagin, a Natural Compound with Several Biological Effects and Anti-Inflammatory Properties. Life (Basel). 2023;13(6):1303. https://doi.org/10.3390/life13061303. PMID:37374085;PMCID:PMC10301567.
Chung J, et al. Trans-cinnamic aldehyde inhibits Aggregatibacter actinomycetemcomitans-induced inflammation in THP-1-derived macrophages via autophagy activation. J Periodontol. 2018;89(10):1262–71.
Kajiura Y, et al. β-carotene suppresses Porphyromonas gingivalis lipopolysaccharide-mediated cytokine production in THP-1 monocytes cultured with high glucose condition. Cell Biol Int. 2018;42(1):105–11.
Li M, et al. The efficacy of proanthocyanidins and secnidazole in the treatment of chronic periodontitis after scaling and root planing therapy. J Biol Regul Homeost Agents. 2017;31(1):93–7.
Zhou J, et al. Notopterol Inhibits the NF-κB Pathway and Activates the PI3K/Akt/Nrf2 Pathway in Periodontal Tissue. J Immunol. 2023;211(10):1516–25.
Li X, Yu C, Hu Y, Xia X, Liao Y, Zhang J, Chen H, Lu W, Zhou W, Song Z. New Application of Psoralen and Angelicin on Periodontitis With Anti-bacterial, Anti-inflammatory, and Osteogenesis Effects. Front Cell Infect Microbiol. 2018;5(8):178. https://doi.org/10.3389/fcimb.2018.00178. PMID:29922598;PMCID:PMC5996246.
Zhang Y, et al. Clinical efficacy of curcumin versus chlorhexidine as an adjunct to scaling and root planing for the treatment of periodontitis: A systematic review and meta-analysis. Phytother Res. 2021;35(11):5980–91.
Guo Y, Zhou M, Mu Z, Guo J, Hou Y, Xu Y, Geng L. Recent advances in shikonin for the treatment of immune-related diseases: Anti-inflammatory and immunomodulatory mechanisms. Biomed Pharmacother. 2023;165:115138. https://doi.org/10.1016/j.biopha.2023.115138. Epub 2023 Jul 14 PMID: 37454591.
Yuan L, Wang Y, Chen Y, Chen X, Li S, Liu X. Shikonin inhibits immune checkpoint PD-L1 expression on macrophage in sepsis by modulating PKM2. Int Immunopharmacol. 2023;121:110401. https://doi.org/10.1016/j.intimp.2023.110401. Epub 2023 Jun 9 PMID: 37302371.
Lin X, et al. Shikonin promotes rat periodontal bone defect repair and osteogenic differentiation of BMSCs by p38 MAPK pathway. Odontology. 2023;111(3):649–57.
Li F, Liu X, Li M, Wu S, Le Y, Tan J, Zhu C, Wan Q. Inhibition of PKM2 suppresses osteoclastogenesis and alleviates bone loss in mouse periodontitis. Int Immunopharmacol. 2024;129:111658. https://doi.org/10.1016/j.intimp.2024.111658. Epub 2024 Feb 15 PMID: 38359663.
Liu C, He L, Wang J, Wang Q, Sun C, Li Y, Jia K, Wang J, Xu T, Ming R, Wang Q, Lin N. Anti-angiogenic effect of Shikonin in rheumatoid arthritis by downregulating PI3K/AKT and MAPKs signaling pathways. J Ethnopharmacol. 2020;260:113039. https://doi.org/10.1016/j.jep.2020.113039. Epub 2020 Jun 1 PMID: 324976752.
Balaha MF, Alamer AA, Eisa AA, Aljohani HM. Shikonin Alleviates Gentamicin-Induced Renal Injury in Rats by Targeting Renal Endocytosis, SIRT1/Nrf2/HO-1, TLR-4/NF-κB/MAPK, and PI3K/Akt Cascades. Antibiotics (Basel). 2023;12(5):826. https://doi.org/10.3390/antibiotics12050826. PMID:37237729;PMCID:PMC10215741.
Ma Y, Yang X, Han H, Wen Z, Yang M, Zhang Y, Fu J, Wang X, Yin T, Lu G, Qi J, Lin H, Wang X, Yang Y. Design, synthesis and biological evaluation of anilide (dicarboxylic acid) shikonin esters as antitumor agents through targeting PI3K/Akt/mTOR signaling pathway. Bioorg Chem. 2021;111:104872. https://doi.org/10.1016/j.bioorg.2021.104872. Epub 2021 Mar 29 PMID: 33838560.
Wang S, Zhu Y, Qiu R. Shikonin protects H9C2 cardiomyocytes against hypoxia/reoxygenation injury through activation of PI3K/Akt signaling pathway. Biomed Pharmacother. 2018;104:712–7. https://doi.org/10.1016/j.biopha.2018.04.144. Epub 2018 May 25 PMID: 29807220.
Ni F, et al. Shikonin exerts antitumor activity in Burkitt’s lymphoma by inhibiting C-MYC and PI3K/AKT/mTOR pathway and acts synergistically with doxorubicin. Sci Rep. 2018;8(1):3317.
Kajiura K, et al. Shikonin induces odontoblastic differentiation of dental pulp stem cells via AKT-mTOR signaling in the presence of CD44. Connect Tissue Res. 2021;62(6):689–97.
Chen X, et al. Shikonin, a component of chinese herbal medicine, inhibits chemokine receptor function and suppresses human immunodeficiency virus type 1. Antimicrob Agents Chemother. 2003;47(9):2810–6.
Chen Y, et al. The Critical Role of PTEN/PI3K/AKT Signaling Pathway in Shikonin-Induced Apoptosis and Proliferation Inhibition of Chronic Myeloid Leukemia. Cell Physiol Biochem. 2018;47(3):981–93.
Guo L, et al. Shikonin ameliorates oxidative stress and neuroinflammation via the Akt/ERK/JNK/NF-κB signalling pathways in a model of Parkinson’s disease. Clin Exp Pharmacol Physiol. 2022;49(11):1221–31.
Park UH, Youn H, Kim EJ, Um SJ. Shikonin Binds and Represses PPARγ Activity by Releasing Coactivators and Modulating Histone Methylation Codes. Nutrients. 2023;15(7):1797. https://doi.org/10.3390/nu15071797. PMID:37049636;PMCID:PMC10097191.
Wu L, et al. Discovery of Dimethyl Shikonin Oxime 5a, a Potent, Selective Bombesin Receptor Subtype-3 Agonist for the Treatment of Type 2 Diabetes Mellitus. J Med Chem. 2023;66(12):8011–29.
Yang W, et al. Effects of shikonin from Zicao on high-fat diet-induced nonalcoholic fatty liver disease in rats. Pak J Pharm Sci. 2020;33(6):2527–33.
Jia Y, Li Z, Wang T, Fan M, Song J, Lv P, Jin W. Shikonin Attenuates Chronic Cerebral Hypoperfusion-Induced Cognitive Impairment by Inhibiting Apoptosis via PTEN/Akt/CREB/BDNF Signaling. Evid Based Complement Alternat Med. 2021;7(2021):5564246. https://doi.org/10.1155/2021/5564246. PMID:34211568;PMCID:PMC8205575.
Peng Y, et al. Shikonin attenuates kidney tubular epithelial cells apoptosis, oxidative stress, and inflammatory response through nicotinamide adenine dinucleotide phosphate oxidase 4/PTEN pathway in acute kidney injury of sepsis model. Drug Dev Res. 2022;83(5):1111–24.
Wu X, et al. Phosphatase and tensin homologue determine inflammatory status by differentially regulating the expression of Akt1 and Akt2 in macrophage alternative polarization of periodontitis. J Clin Periodontol. 2023;50(2):220–31.
Barczak K, Droździk A, Bosiacki M, Łagocka R, Cenariu D, Uriciuc WA, Baranowska-Bosiacka I. CCL5’s Role in Periodontal Disease: A Narrative Review. Int J Mol Sci. 2023;24(24):17332. https://doi.org/10.3390/ijms242417332. PMID:38139161;PMCID:PMC10744061.
Luo H, et al. Genetically engineered CXCR4-modified exosomes for delivery of miR-126 mimics to macrophages alleviate periodontitis. J Nanobiotechnology. 2023;21(1):116.
Cirelli T, Nicchio IG, Bussaneli DG, Silva BR, Nepomuceno R, Orrico SRP, Cirelli JA, Theodoro LH, Barros SP, Scarel-Caminaga RM. Evidence Linking PPARG Genetic Variants with Periodontitis and Type 2 Diabetes Mellitus in a Brazilian Population. Int J Mol Sci. 2023;24(7):6760. https://doi.org/10.3390/ijms24076760. PMID:37047733;PMCID:PMC10095581.
Zhang S, et al. Alteration of PTGS2 promoter methylation in chronic periodontitis. J Dent Res. 2010;89(2):133–7.
Jurdziński KT, Potempa J, Grabiec AM. Epigenetic regulation of inflammation in periodontitis: cellular mechanisms and therapeutic potential. Clin Epigenetics. 2020;12(1):186.
Redman RS, et al. Botryoid odontogenic cyst Exploration of proliferative activity, apoptosis and expression of TP53 and BCL2 compared to the histologically identical lateral periodontal and gingival cysts. Biotech Histochem. 2017;92(8):569–76.
Felthaus O, et al. Transcription factors TP53 and SP1 and the osteogenic differentiation of dental stem cells. Differentiation. 2012;83(1):10–6.
Xie R, Li B, Jia L, Li Y. Identification of Core Genes and Pathways in Melanoma Metastasis via Bioinformatics Analysis. Int J Mol Sci. 2022;23(2):794. https://doi.org/10.3390/ijms23020794. PMID:35054979;PMCID:PMC8775799.
Cui ZY, Park SJ, Jo E, Hwang IH, Lee KB, Kim SW, Kim DJ, Joo JC, Hong SH, Lee MG, Jang IS. Cordycepin induces apoptosis of human ovarian cancer cells by inhibiting CCL5-mediated Akt/NF-κB signaling pathway. Cell Death Discov. 2018;23(4):62. https://doi.org/10.1038/s41420-018-0063-4. PMID:29844932;PMCID:PMC5966410.
Yu-Ju WC, et al. CCL5 of glioma-associated microglia/macrophages regulates glioma migration and invasion via calcium-dependent matrix metalloproteinase 2. Neuro Oncol. 2020;22(2):253–66.
Yang F, et al. SDF1-CXCR4 Signaling Contributes to the Transition from Acute to Chronic Pain State. Mol Neurobiol. 2017;54(4):2763–75.
Lai X, et al. CXCL14 Protects against Polymicrobial Sepsis by Enhancing Antibacterial Functions of Macrophages. Am J Respir Cell Mol Biol. 2022;67(5):589–601.
Deng H, et al. Bavachinin Ameliorates Rheumatoid Arthritis Inflammation via PPARG/PI3K/AKT Signaling Pathway. Inflammation. 2023;46(5):1981–96.
He L, et al. Circular RNA hsa_circ_0084054 promotes the progression of periodontitis with diabetes via the miR-508-3p/PTEN axis. J Periodontal Res. 2023;58(4):827–40.
Okamoto R, et al. Cardamonin decreases inflammatory mediator expression in IL-1β-stimulated human periodontal ligament cells. Mol Biol Rep. 2024;51(1):222.
Lee HY, et al. Ixeris dentata and Lactobacillus gasseri media protect against periodontitis through Nrf2-HO-1 signalling pathway. Sci Rep. 2023;13(1):12861.
Park CM, Yoon HS. Chlorogenic Acid as a Positive Regulator in LPS-PG-Induced Inflammation via TLR4/MyD88-Mediated NF-κB and PI3K/MAPK Signaling Cascades in Human Gingival Fibroblasts. Mediators Inflamm. 2022;9(2022):2127642. https://doi.org/10.1155/2022/2127642. PMID:35437426;PMCID:PMC9013303.
Hua SY, Zhang ZH, Yang Y, et al. Clinical Efficacy of Compound Lithospermum Oil in the Treatment of Mild to Moderate Diaper Dermatitis in Infants. 2023 National Conference on Integrated Traditional Chinese and Western Medicine in Dermatology and Venereology. 2023. p. 110. Chinese. https://doi.org/10.26914/c.cnkihy.2023.009401.
Yang XB, Wang Y, Yang J, et al. Analysis of the therapeutic effect of the combination of Scorgizumab and Zicao Su on recurrent moderate to severe plaque psoriasis. World Clin Drugs. 2023;43(12):1568–73. Chinese.
Zhang M, Lu JJ, Wu WW, et al. [Clinical observation on the treatment of psoriasis vulgaris with different doses of Zicao mixture. Chinese J Integr TCM, Dermatol Venereol. 2018;17(02):149–51. Chinese.
Jia J, Wei YS, Zhou Y, et al. Clinical observation of using purple grass oil and Kangfuxin liquid to alleviate wound healing after surgery for perianal abscess. Chinese J Exp Formulology. 2023;29(03):87. Chinese.
Acknowledgements
This study was supported by the 2022 Medical and Health Research Projects of Heilongjiang Province, China, (No. 20220808050672).
Funding
2022 Medical and Health Research Projects of Heilongjiang Province, China, Grant/Award Numbers: 20220808050672.
Author information
Authors and Affiliations
Contributions
Qingliang Zhao and Lin Guo drafted the manuscript. Xiangyan Liu designed and supervised manuscript. Lin Hou revised the manuscript. Kun Wang critically revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, Q., Wang, K., Hou, L. et al. Based on network pharmacology and molecular docking to explore the potential mechanism of shikonin in periodontitis. BMC Oral Health 24, 839 (2024). https://doi.org/10.1186/s12903-024-04618-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04618-7