Abstract
Background
Few studies have been conducted on treating temporomandibular disorders (TMDs) with new digital occlusal splints, which has increasingly attracted wide attention.
Methods
To evaluate the clinical efficacy and quality of life (QoL) of Kovacs digital occlusal splint (KDOS) treatment in patients with TMD.
Materials and methods
Eighty-nine patients with TMD who were treated using KDOS were analyzed. The patients were divided into three groups according to the Wilkes stage. The clinical symptoms and QoL scores of the patients in each group were recorded before and at least three months after treatment, and the data were statistically analyzed and compared. The relationships between the disease severity, sex, age, and level of QoL before treatment and improvement in the clinical symptoms were analyzed using binary logistic regression.
Results
The mean age and follow-up period of the patients were 28.0 ± 10.4 years and 4.9 ± 2.1 months, respectively. After KDOS treatment, the improvement rates of joint noise and pain were 80.4% and 69.8%, respectively. Additionally, the patients’ maximum mouth opening and global QoL mean scores significantly improved compared to those before treatment (p < 0.001). Binary logistic regression analysis revealed that the factors affecting the improvement in the clinical symptoms were disease severity and level of QoL before treatment.
Conclusions
KDOS can improve the clinical symptoms and QoL of patients with TMD. Moreover, patients without osteoarthritis and with low pretreatment QoL levels are more likely to demonstrate clinical improvement.
Trial registration
The trial was registered with Chinese Clinical Trial Registry (ChiCTR) (ID: ChiCTR2300076518) on 11/10/2023.
Similar content being viewed by others
Background
Temporomandibular disorders (TMDs) do not comprise a single disease entity, it is a general term for diseases involving pain and dysfunction of the temporomandibular joint and masticatory muscles. The main symptoms are joint crackling, murmurs, joint pain, and jaw movement disorders [1]. TMDs are very common in the general population [2,3,4]. The prevalence of symptoms varies from 25 to 50% while the prevalence of clinical signs varies from 40 to 90% [5]. Previous studies on patient samples have indicated substantial negative effects of TMD on the oral health-related quality of life (OHRQoL) [6, 7]. The etiology of TMD is vast and unclear with various complicated theories, thereby affecting the establishment of a correct diagnosis [8, 9]. Since occlusal factors are the most dominant pathogenic factors of TMD, treatment using occlusal splints, which is widely used in clinical practice, has been recognized as an area of increasing interest among researchers [10, 11].
Currently, the stabilization splint is the most commonly used occlusal splint. However, owing to the complicated traditional manufacturing process and low degree of automation, ensuring accuracy of occlusal splints is often challenging. Many inconveniences of the traditional methods can be solved with the help of digital technology [12]. Kovacs digital occlusal splint (KDOS) is an innovation of traditional occlusal splint technology, which obtains ideal jaw position after muscle deprogramming, and customizes complete digital and comfortable occlusal splints for patients with TMD [13]. It can standardize the production process, thereby saving time by reducing the influence of human factors and patient visits.
Being a common disease, TMD affects many patients and impairs their QoL. KDOS, which is a new digital occlusal splint for TMD treatment, has generated great interest. The present study aimed to evaluate the clinical efficacy and QoL of patients with TMD using KDOS.
Methods
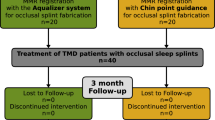
This study was approved by the Ethics Committee of Wenzhou Medical University (WYKQ2022013); all the authors have read the Declaration of Helsinki, and each patient provided signed informed consent. The patients in this study were diagnosed with TMD and received KDOS treatment in our department between September 2022 and May 2023. The inclusion criteria for the study were as follows: (1) anterior disc displacement with or without reduction (ADDwR or ADDwoR) confirmed by magnetic resonance imaging, (2) age ≥ 18 years, (3) no history of any treatment for TMD, and (4) at least having a 3-month follow-up record. The exclusion criteria were as follows: (1) long-term chronic diseases, such as diabetes and immune diseases, which may affect the QoL of the patients; (2) cognitive dysfunction; and (3) incomplete follow-up data. The enrolled patients were divided into three groups based on the Wilkes–Bronstein classification: (1) ADDwR, (2) ADDwoR, and (3) ADDwoR + osteoarthritis (OA) groups. The period before and at least 3 months after treatment when the patients returned to the hospital for examination was selected as the time point, the relevant clinical symptoms were recorded by the same experienced doctor, and a trained specialist nurse guided the eligible patients to complete the questionnaire. Any concerns regarding the questionnaire guidelines were clarified, and the integrity of the completed questionnaire was assessed. The issuance, guidance, and collection of the questionnaires were conducted by the same nurses to ensure accuracy. The research flowchart is presented in Fig. 1.
KDOS treatment
Eligible patients were treated using KDOS. First, the dentition and occlusal relationship of the patient were scanned using an oral scanner (3shape, Copenhagen, Denmark), and a balancer was fabricated according to the digital data. Second, the stable therapeutic jaw position was recorded after wearing a balancer and performing muscle-deprogrammed movements, which were imported into the Exocad software (Version 3.0, Exocad GmbH, Darmstadt, Germany) for the design of the occlusal splint. Finally, a semi-anatomical occlusal splint made of resin discs (PMMA disk; Yamahachi Dental, Japan) was automatically ground using the SELECT five-axis engraving machine (Wieland, Germany) [13]. The KDOS production flow chart is shown in Fig. 2. All the clinical procedures were performed by an experienced physician. The patients were required to visit the doctor three times for KDOS treatment, and corresponding adjustments were made during the first week after wearing it. Follow-ups were conducted once every 1–2 months according to the condition of the patient.
Clinical symptoms and questionnaire data collection
Before and at least three months after wearing KDOS, pain, joint noise, and maximal mouth opening (MMO) were measured using the pain-visual analog scale (pain-VAS), joint noise score (JNS) in the Friction Index, and straight edge, respectively. Pain-VAS scores from 0 to 10 and JNS scores from 0 to 4 represent low to high levels. MMO, the maximum distance at which the patients could open their mouth, was evaluated as the distance between the edges of the maxillary and mandibular incisors. The pain-VAS score and JNS were considered improved in cases of a decline by more than or equal to 30% after treatment. The improvement rates before and after treatment were compared. The Depression, Anxiety, and Stress Scale-21 (DASS-21) and Oral Health Impact Profile for TMDs (OHIP-TMD) were used to record the QoL of the patients before and after treatment. To measure and distinguish the symptoms of depression, anxiety, and stress, the DASS-21 consists of three sections, each with seven items, with responses ranging from 0 ( does not apply to me at all) to 3 (applicable to me very much or most of the time). The Chinese version has been validated across cultures [14]. The OHIP-TMD includes 22 items in seven domains, namely functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. Each item was assessed using a 5-point response scale as follows: 0 = never, 1 = hardly ever, 2 = sometimes, 3 = fairly often, and 4 = very often. Higher scores indicate worse QoL. The validated standard Chinese version of the OHIP-TMD was used according to the respective guidelines [15].
Statistical analysis
SPSS Statistics version 27.0 software (IBM Corp., Armonk, NY, USA) was used for the data analysis. The Wilcoxon signed-rank test was used to analyze the changes in the questionnaire scores and MMO before and after treatment. The chi-square test was used to compare the improvement rates of the JNS and Pain-VAS scores before and after treatment. Binary logistic regression was used to analyze whether the sex, age, group, and pre-treatment QoL scores were associated with improved clinical outcomes.
Results
Eighty-nine patients were finally enrolled in the study; 33, 30, and 26 patients were present in the ADDwR, ADDwoR, and ADDwoR + OA groups, respectively, which included 62 women and 27 men, with an average age of 28.0 ± 10.4 years and an average follow-up of 4.9 ± 2.1 months (Table 1). The overall age distribution ranges from 18 to 55 years old, with 42.7% of the respondents between 20 and 30 years old. Following KDOS treatment, the improvement rate of the ADDwR group was the highest, whereas that of the ADDwoR + OA group was the worst. The improvement rates of the JNS and Pain-VAS score were 80.4% and 69.8%, respectively, which were significantly improved compared with those before treatment (p < 0.001, Table 2). MMO also improved significantly (30.8 ± 6.6, 36.2 ± 5.7, p < 0.001, Table 2).
OHIP-TMD
Global OHIP scores before and after treatment fluctuated between 0 and 18 and 0–17, respectively. Most domain scores demonstrated an upward trend from the ADDwR to the ADDwoR + OA group. The mean global OHIP score following KDOS treatment was significantly lower than that before treatment (6.1 ± 3.2, 7.2 ± 3.7, respectively; p < 0.001). Significant differences in the mean scores before and after treatment were also observed in all the seven domains. After treatment with KDOS, a significant decrease in the scores in each domain was observed. Only the ADDwoR + OA group demonstrated no significant difference in the domain scores of physical disability and handicap before and after treatment (5.1 ± 1.5, 5.0 ± 1.6, p = 0.718; 4.8 ± 1.4, 4.4 ± 1.6, p = 0.058, respectively). The OHIP scores are presented in Table 3.
DASS-21
The scores before and after treatment fluctuated between 0 and 19 and 0–17, respectively. The average scores of stress, anxiety, and depression following KDOS treatment were 9.9 ± 3.4, 6.4 ± 3.0, and 6.1 ± 2.9, respectively, which were significantly different from the average scores of 11.4 ± 4.0, 7.2 ± 3.6, and 7.1 ± 3.5 before treatment (p < 0.001). The mean scores of the three groups in the three sections were significantly lower than those before treatment (p < 0.05). Except for stress, the ADDwoR group demonstrated the highest average score, ADDwoR + OA group had the highest average score in the other two parameters, followed by the ADDwoR group, and the ADDwR group had the lowest score. The mean DASS-21 scores of the three groups are presented in Table 4.
Binary logistic regression
Binary logistic regression revealed that (1) compared with the ADDwoR + OA group, the ADDwR and ADDWoR groups were more likely to demonstrate improved clinical outcomes following treatment; (2) patients with low QoL scores before treatment were more likely to demonstrate improved clinical outcomes after treatment; and (3) there was no significant correlation between the improvement in the clinical outcomes and age or sex. The results are presented in Table 5; Fig. 3.
Discussion
Over the past few years, there has been growing interest in the OHRQoL. Oral diseases can affect various aspects of an individual’s mental and physical health [16]. TMD, which mainly involves the temporomandibular joint and/or masticatory muscles, causes clinical symptoms, such as oral and maxillofacial pain, joint noise, and mandibular movement disorders, which significantly impact the patients’ physical and mental health and QoL [17, 18]. Although the etiology of TMD is vast and various theories exist describing the pathogenesis of TMD, the theory of multifactor co-pathogenesis has been accepted by many researchers. Various treatment methods exist for managing the different pathogeneses of TMD; the chief treatment methods can be classified as reversible treatments, such as physical therapy and drug therapy, and irreversible treatments, such as adjustment of bite and joint surgery [1, 2, 19]. Since the pathogenesis of TMD is still unclear, and long-term research results reveal that the success rate of conservative and non-conservative treatment is similar, clinical treatment mainly comprises non-invasive conservative treatment [2, 20].
Occlusal splint is a conservative treatment modality with wide clinical application and experimentally verified clinical efficacy. The occlusal splint is a removable appliance that can be used to treat oral-maxillary system dysfunction by adjusting the jaw position and occlusal contact, changing the position of the condyle in the articular fossa, and reducing abnormal muscle activity [21, 22]. At present, the stabilization occlusal splint is the most common occlusal splint used for TMD treatment. In recent years, the wide application and rapid development of digital technology in the field of dental prosthetics has resulted in great innovation in traditional design concepts and production modes. For example, Dedem and Türp [23] used computer-aided design for fabricating occlusal splints; intraoral testing demonstrated good retention and stability. However, complete digitalization includes at least three components, namely digital impression technology, digital design, and digital production [24]. KDOS digitizes the entire process and treats TMD by using the balancer to deprogram the muscles to determine the therapeutic jaw position.
Pain, which greatly affects the QoL of patients, is the most common symptom of TMD [25]. The majority of the patients reported pain in the masticatory muscle and / or preauricular region, which was easily exacerbated by chewing or other jaw activity [26]. Chronic pain reportedly has a strong negative impact on the patients’ QoL [9, 27, 28]. In this study, 53 patients (59.6%) had pain symptoms, and the average score in the domain of physical pain was the highest among the seven domains in the OHIP (11.8 ± 2.7). The second highest scoring domain was psychological disability (10.9 ± 2.8), which is supported by a bio-psychosocial model on TMD [29]. After KDOS treatment, the average physical pain score of the patients significantly reduced (10.2 ± 2.4, p < 0.001), and the improvement rate reached 69.8%, which was similar to the improvement rate (71.6%) in a previous KDOS study by Hua et al. [13]. Consistent with their study, the pain improvement rate in the ADDwoR + OA group was the lowest among the three Wilkes stage groups, which may be related to greater tissue damage in the disease. However, according to Pficer et al.‘s 2017 meta-analysis [30], the effect of the stabilization occlusal splint on the pain outcomes was significantly better than that of the control group in the short-term, while this effect gradually disappeared in the long-term study; therefore, a longer follow-up period is warranted to support the results of our study. Furthermore, in this study, the JNS was separated from the Friction index, and a quantitative index was applied to ensure objectivity of the compared result. Joint noise and MMO also significantly improved after treatment, with the joint noise improvement rate reaching 80.4%. Tecco et al. [31] demonstrated that more than 50% of the patients still experienced persistent joint noise three months after treatment, regardless of whether they were treated with a repositioning or stabilization occlusal splint, indicating that joint noise is likely to have a persistent impact on the patients’ QoL. Previous studies have demonstrated that both the MMO and OHIP scores improved after occlusal splint treatment [32, 33]. Our study supported this view; all seven domains of the OHIP and global mean scores significantly improved following KDOS treatment.
Studies have demonstrated that TMD can hinder daily, social, and family activities, which can lead to poor mental and emotional states [27, 34]. This study reached the same conclusion; in the DASS-21, the average scores for stress, anxiety, and depression exceeded the normal range (11.4 ± 4.0, 7.2 ± 3.6, 7.1 ± 3.5, respectively). A large proportion of patients with TMD report difficulty falling asleep or staying asleep, indicating that poor sleep quality in patients with TMD is an important issue, as physical and mental health is associated with effective sleep and contributes to good QoL [35, 36]. While sleep quality is closely related to stress levels, the average stress score in this study was the highest among the three items; however, no relevant evidence exists for the effect of sleep on the QoL. Additionally, since emotional stress caused by TMD can lead to anxiety and depression, most patients require psychological assistance [37]. After KDOS treatment, the patients demonstrated significant improvement in their average scores concerning stress, anxiety and depression (9.9 ± 3.4, 6.4 ± 3.0, 6.1 ± 2.9, respectively; p < 0.001). Pficer et al. [30] demonstrated a similar result for the stabilization occlusal splint, which supports the findings of this study.
The binary logistic regression analysis revealed that patients with low QoL scores before treatment and those in the ADDwR and ADDwoR groups were likely to demonstrate a higher rate of improvement in the clinical symptoms following treatment with KDOS, which is similar to the results of Hua [13] and Clark et al. [38] GHE et al. [39] also reported that patients with joint pain or OA had lower QoL than those with myofascial pain or disc displacement. The present study concluded that the improvement rate of clinical symptoms was not associated with the age and sex of the patients; moreover, Emshoff et al. [40] did not find any influence of age on the prognosis of stabilization occlusal splint treatment; however, Hua et al. [13] demonstrated that the older the patient, the higher the possibility of improvement, which may be attributed to the difference in sample size and population characteristics.
In this study, patients with TMD demonstrated significant improvement in their clinical symptoms and QoL scores following treatment with KDOS; however, some studies have shown that occlusal splints and other treatments (such as acupuncture, counseling, and masticatory muscle exercises) have little or no significant benefit in alleviating symptoms [41,42,43]. Additionally, some studies have highlighted the limited efficacy of occlusal splint for TMD patients with OA. However, the application of arthroscopic surgery and/or platelet-rich plasma has been shown to significantly ameliorate clinical symptoms in OA patients, including pain and mouth opening [44, 45]. Furthermore, our study’s findings revealed no significant improvement in most items related to OHRQoL scores following the use of KDOS in the ADDWoR + OA group. Thus, further research should focus on randomized controlled trials comparing KDOS with other treatments.
Conclusions
KDOS can improve the clinical symptoms and QoL of patients with TMD. Clinical improvement is related to the severity of the disease and the level of QoL before treatment.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TMDs:
-
Temporomandibular disorders
- OHRQoL:
-
Oral health-related quality of life
- KDOS:
-
Kovacs digital occlusal splint
- ADDwR:
-
Anterior disc displacement with reduction
- ADDwoR:
-
Anterior disc displacement without reduction
- OA:
-
Osteoarthritis
- MMO:
-
Maximal mouth opening
- Pain-VAS:
-
Pain-visual analog scale
- JNS:
-
Joint noise score
- DASS-21:
-
Depression, Anxiety, and Stress Scale-21
- OHIP-TMD:
-
Oral Health Impact Profile for TMDs
References
Wang XD, Zhang JN, Gan YH, Zhou YH. Current understanding of pathogenesis and treatment of TMJ osteoarthritis. J Dent Res. 2015;94(5):666–73.
Gauer RL, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician. 2015;15(6):378–86.
Kokkola O, Suominen AL, Qvintus V, et al. Efficacy of stabilisation splint treatment on the oral health-related quality of life-a randomised controlled one-year follow-up trial. J Oral Rehabil. 2018;45(5):355–62.
List T, Jensen RH. Temporomandibular disorders: old ideas and new concepts. Cephalalgia. 2017;37(7):692–704.
Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13(4):232–7.
Almoznino G, Zini A, Zakuto A, et al. Oral health-related quality of life in patients with Temporomandibular disorders. J Oral Facial Pain Headache. 2015;29(3):231–41.
Bayat M, Abbasi AJ, Noorbala AA, Mohebbi SZ, Moharrami M, Yekaninejad MS. Oral health-related quality of life in patients with temporomandibular disorders: a case-control study considering psychological aspects. Int J Dent Hyg. 2018;16(1):165–70.
Forssell H, Kalso E. Application of principles of evidence-based medicine to occlusal treatment for temporomandibular disorders: are there lessons to be learned? J Orofac Pain. 2004;18(1):9–22. discussion 23–32.
McNeill C. Management of temporomandibular disorders: concepts and controversies. J Prosthet Dent. 1997;77(5):510–22.
Konstantinović VS, Lazić V. Occlusion splint therapy in patients with craniomandibular disorders (CMD). J Craniofac Surg. 2006;17(3):572–8.
Ohrbach R, Bair E, Fillingim RB, et al. Clinical orofacial characteristics associated with risk of first-onset TMD: the OPPERA prospective cohort study. J Pain. 2013;14(12 Suppl):T33–50.
Lin R, Yu CH, Sun J. [Construction and preliminary clinical evaluation of digital stabilization occlusal splint system]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;9(12):983–6.
Hua J, Fan X, Nie X, He D. Preliminary evaluation of Kovacs digital occlusal splint in the treatment of temporomandibular disorders: a single-centre, cross-sectional study. J Oral Rehabil. 2023;50(8):687–97.
Wang K, Shi HS, Geng FL, et al. Cross-cultural validation of the Depression anxiety stress Scale-21 in China. Psychol Assess. 2016;28(5):e88–100.
He SL, Wang JH. Validation of the Chinese version of the oral health impact profile for TMDs (OHIP- TMDs-C). Med Oral Patol Oral Cir Bucal. 2015;20(2):e161–166.
Dahlström L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand. 2010;68(2):80–5.
Manfredini D, Thomas DC, Lobbezoo F. Temporomandibular disorders within the Context of Sleep disorders. Dent Clin North Am. 2023;67(2):323–34.
Vaira LA, De Riu G. Temporomandibular Joint disorders: functional and conservative treatment. J Clin Med. 2023;12(14).
Li DTS, Leung YY. Temporomandibular disorders: current concepts and controversies in diagnosis and management. Diagnostics (Basel). 2021;11(3).
Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am. 2013;57(3):465–79.
Denardin ACS, do Nascimento LP, Valesan LF, et al. Disocclusion guides in occlusal splints on temporomandibular disorders and sleep bruxism: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2023;135(1):51–64.
Tran C, Ghahreman K, Huppa C, Gallagher JE. Management of temporomandibular disorders: a rapid review of systematic reviews and guidelines. Int J Oral Maxillofac Surg. 2022;51(9):1211–25.
Dedem P, Türp JC. Digital Michigan splint - from intraoral scanning to plasterless manufacturing. Int J Comput Dent. 2016;19(1):63–76.
Silva DN, Gerhardt de Oliveira M, Meurer E, Meurer MI, Lopes da Silva JV, Santa-Bárbara A. Dimensional error in selective laser sintering and 3D-printing of models for craniomaxillary anatomy reconstruction. J Craniomaxillofac Surg. 2008;36(8):443–9.
Vrbanović E, Alajbeg IZ. Long-term effectiveness of Occlusal Splint Therapy compared to Placebo in patients with chronic Temporomandibular disorders. Acta Stomatol Croat. 2019;53(3):195–206.
Pan X, Cen X, Zhang B, et al. Circular RNAs as potential regulators in bone remodeling: a narrative review. Ann Transl Med. 2021;9(19):1505.
Bitiniene D, Zamaliauskiene R, Kubilius R, Leketas M, Gailius T, Smirnovaite K. Quality of life in patients with temporomandibular disorders. A systematic review. Stomatologija. 2018;20(1):3–9.
Schlenk EA, Erlen JA, Dunbar-Jacob J, et al. Health-related quality of life in chronic disorders: a comparison across studies using the MOS SF-36. Qual Life Res. 1998;7(1):57–65.
Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9(6):613–33.
Kuzmanovic Pficer J, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS ONE. 2017;12(2):e0171296.
Tecco S, Festa F, Salini V, Epifania E, D’Attilio M. Treatment of joint pain and joint noises associated with a recent TMJ internal derangement: a comparison of an anterior repositioning splint, a full-arch maxillary stabilization splint, and an untreated control group. Cranio. 2004;22(3):209–19.
Alajbeg IZ, Boric Brakus R, Brakus I. Comparison of Amitriptyline with stabilization splint and placebo in chronic TMD patients: a pilot study. Acta Stomatol Croat. 2018;52(2):114–22.
Alajbeg IZ, Gikić M, Valentić-Peruzović M. Changes in pain intensity and oral health-related quality of life in patients with temporomandibular disorders during stabilization splint therapy–a pilot study. Acta Clin Croat. 2014;53(1):7–16.
Cioffi I, Perrotta S, Ammendola L, et al. Social impairment of individuals suffering from different types of chronic orofacial pain. Prog Orthod. 2014;16(1):27.
Peixoto KO, Resende C, Almeida EO, et al. Association of sleep quality and psychological aspects with reports of bruxism and TMD in Brazilian dentists during the COVID-19 pandemic. J Appl Oral Sci. 2021;29:e20201089.
Sánchez Romero EA, Martínez-Pozas O, García-González M et al. Association between Sleep disorders and Sleep Quality in patients with Temporomandibular Joint Osteoarthritis: a systematic review. Biomedicines. 2022;10(9).
Castro AR, Siqueira SR, Perissinotti DM, Siqueira JT. Psychological evaluation and cope with trigeminal neuralgia and temporomandibular disorder. Arq Neuropsiquiatr. 2008;66(3b):716–9.
Clark GT, Baba K, McCreary CP. Predicting the outcome of a physical medicine treatment for temporomandibular disorder patients. J Orofac Pain. 2009;23(3):221–9.
Tjakkes GH, Reinders JJ, Tenvergert EM, Stegenga B. TMD pain: the effect on health related quality of life and the influence of pain duration. Health Qual Life Outcomes. 2010;2:8:46.
Emshoff R, Rudisch A. Likelihood ratio methodology to identify predictors of treatment outcome in temporomandibular joint arthralgia patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):525–33.
Al-Ani Z, Gray RJ, Davies SJ, Sloan P, Glenny AM. Stabilization splint therapy for the treatment of temporomandibular myofascial pain: a systematic review. J Dent Educ. 2005;69(11):1242–50.
List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010;37(6):430–51.
Niemelä K, Korpela M, Raustia A, Ylöstalo P, Sipilä K. Efficacy of stabilisation splint treatment on temporomandibular disorders. J Oral Rehabil. 2012;39(11):799–804.
Chung PY, Lin MT, Chang HP. Effectiveness of platelet-rich plasma injection in patients with temporomandibular joint osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127(2):106–16.
Al-Moraissi EA, Wolford LM, Ellis E 3rd, Neff A. The hierarchy of different treatments for arthrogenous temporomandibular disorders: a network meta-analysis of randomized clinical trials. J Craniomaxillofac Surg. 2020;48(1):9–23.
Acknowledgements
Doctor Yang and Doctor Rao are thanked for their contribution during the treatment.
Funding
This work was supported by the Wenzhou Municipal Science and Technology Bureau, Zhejiang Province, China (Y20220381).
Author information
Authors and Affiliations
Contributions
Material preparation, data collection and analysis were performed by XQ, LJ, HSQ, WC and CY. XQ wrote the main manuscript text. NX and XJ suggested changes of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Institutional Review Committee, Wenzhou Medical University (WYKQ2022013). All the authors have read the Declaration of Helsinki, and each patient provided signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, Q., Li, J., Wang, C. et al. Evaluation of the efficacy and quality of life in patients with temporomandibular joint disorders treated with Kovacs digital occlusal splint: a pilot study. BMC Oral Health 24, 802 (2024). https://doi.org/10.1186/s12903-024-04572-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04572-4