Abstract
Background
Endodontic literature search revealed that no study has been conducted to evaluate the prevalence of apical periodontitis (AP) in root canal treated teeth from an adult Nepalese population of Madhesh Province. Consequently, little is known about the extent and risk factors associated with it. This study aimed to determine AP prevalence in root canal treated teeth from an adult Nepalese subpopulation and to analyze the related risk factors including age, sex, tooth type, type of coronal restoration and quality of root canal treatment and coronal restoration as predictors of AP.
Methods
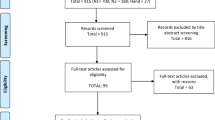
Digital panoramic radiographs were evaluated. Periapical status of 300 root canal-treated teeth was scored by using the periapical index. The quality of root canal treatment and coronal restorations were categorized as adequate or inadequate through radiographic and clinical evaluation. The data were analyzed using univariate and multivariate logistic regression models.
Results
Prevalence of AP in the present study was 31.7%. In 45.7% of the treated teeth, quality of root canal treatment was adequate whereas 46% of the cases had adequate coronal restorations. Multivariate logistic regression analysis revealed statistically significant associations and remarkably increased risk for AP in teeth with inadequate root canal treatment (odds ratio [OR] = 7.92; 95% CI: 3.96–15.82; p < 0.001) whereas lower risk for AP was found in females (OR = 0.51; 95% CI: 0.28–0.90; p = 0.021) and in teeth restored with crown (OR = 0.22; 95% CI: 0.09–0.51; p < 0.001) and filling (OR = 0.18; 95% CI: 0.08–0.42; p < 0.001). Quality of coronal restoration, tooth type and age of the patient were not found to be the predictors of AP.
Conclusions
Within the limits of this study, a high prevalence of AP and poor overall quality of root canal treatment and coronal restoration was found in the subpopulation studied. Quality of root canal treatment, type of coronal restoration and sex of the patient are significant predictors of possible AP development in root canal treated teeth. Substantial efforts are needed to improve the endodontic treatment standards.
Similar content being viewed by others
Background
The oral cavity consists of tissues and organs that form an integral part of the stomatognathic system [1]. Many infectious and inflammatory diseases of the oral cavity have been associated with systemic diseases [2]. Dental caries and periodontitis are two of the most common oral diseases that present a significant public health problem and result in a high economic burden [3]. Apical periodontitis (AP) is an inflammatory disease [4] which in most cases is a direct sequela of dental caries [5]. Caries leads to necrosis of pulpal tissue and continual spread of infection in the periapical region [6]. For diagnosis of AP, radiographic evaluation is important since AP can develop and continue without detectable clinical signs [4].
Root canal treatment (RCT) is indicated for irreversible pulpitis and/or apical periodontitis [7]. The objective of RCT is to prevent and treat AP by eliminating microorganisms and necrotic pulp through chemomechanical debridement and providing an adequate root filling so as to seal the canals and prevent reinfection [8]. Contamination of root canal may occur in teeth with or without previous root canal treatment [9]. A systematic review with meta-analysis showed a very high AP prevalence (39%) in root treated teeth compared to nontreated teeth (3%) [10].
A cross sectional study has been shown to be the best measure of the status of health, disease and therapy in a population [11]. In developing countries, reports on oral diseases are limited. Thus, the basis for the scope of oral health schemes may be the study carried out in different countries which does not correctly signify the situations of developing countries [12]. Taking into account the high prevalence of AP globally [6], the unequal distribution of oral diseases across populations [3] and RCT as one of the most frequent treatments performed worldwide [13], it is reasonable to evaluate the epidemiology of AP in root canal treated teeth from Nepalese population. This will help in the identification and treatment of patients or teeth having higher probability of developing AP. Moreover, it will enable the purposeful distribution of resources, arrangement, and drafting of dental, specifically endodontic, workforce and training [4].
Endodontic literature search revealed that no study has been conducted to evaluate the prevalence of apical periodontitis (AP) in root canal treated teeth from an adult Nepalese population of Madhesh Province. Consequently, little is known about the extent and risk factors associated with it. The aim of the present study was to determine AP prevalence in root canal treated teeth from an adult Nepalese subpopulation and to analyze the related risk factors including age, sex, tooth type, type of coronal restoration and quality of root canal treatment and coronal restoration as predictors of AP.
Methods
This cross-sectional study was carried out on patients attending the dental outpatient department (OPD) of National Medical College & Teaching Hospital (NMCTH), Birgunj, Nepal for the first time seeking routine dental care between December 2022 and May 2023. Ethical clearance for the study was obtained from the Institutional Review Committee of NMCTH Birgunj (Ref. F-NMC/613/079–080). Informed consent was obtained from all subjects and/or their legal guardian(s) prior to inclusion in the study. This study was reported in compliance with the “strengthening the reporting of observational studies in epidemiology” (STROBE statement) [14].
Patient selection
The inclusion criteria of the study were as follows:
-
Adult patients ≥ 18 years of age.
-
Patients with full complementary natural teeth or a minimum of 10 remaining natural teeth.
-
Patients undergoing orthopantomography (OPG) for diagnosis and treatment plan.
-
Patients with ≥ 1 root canal treated tooth. RCTs were performed either at NMCTH, Birgunj or other centers in Madhesh Province.
The exclusion criteria of the study were as follows:
-
Medically compromised patients.
-
Root-treated teeth that have undergone endodontic surgery i.e., root resections or hemi-section.
-
Third molars teeth.
-
Immature teeth.
-
Teeth that could not be assessed radiographically due to superimposition of anatomic structures.
The sample size of the study was calculated based on standard formula [15], considering 85% power at a 95% confidence interval (CI).
With reference to the findings of a published study [16], the prevalence (P) of AP was evaluated at 23.8%. Using the above formula, the sample size estimated was 279 teeth. Considering that 5% of the OPGs could not be evaluated because of inadequate quality, the final sample size taken was 300 teeth.
Clinical examination
Clinical examination was carried out by one examiner (MAH). Any ambiguous situations were further discussed with two other observers and a consensus was reached. The clinical examination procedures given by the American Association of Endodontics [17] were followed which included parameters such as the presence of periodontal pockets, sinus tract formation, tooth mobility, facial symmetry, tenderness on percussion and palpation of adjacent soft tissues. The type of coronal restoration (CR) was recorded. Direct restoration i.e., a direct chairside amalgam or composite filling were categorized as filling. Indirect restoration i.e., a ceramic or a metal-ceramic crown, fabricated in a laboratory and then cemented were categorized as crown. The quality of coronal restorations was evaluated clinically and radiographically in terms of anatomical form, marginal integrity and presence of recurrent caries using the simplified form of the Modified Ryge’s criteria [18].
Radiographic examination
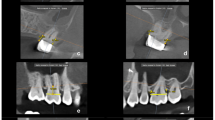
Digital orthopantomograms (OPGs) of all the participants were taken at the Department of Oral Radiology, National Medical College, Birgunj by a well-trained dental radiographer using a panoramic digital radiography device PaX-i 2D Imaging System (VATECH Global, Korea, Model: PCH-2500). All the digital images were assessed by a single examiner (MAH), who is an endodontist. For assessment of the radiographs, an 18.5-inch liquid crystal monitor (E1912H; Dell, Austin, Texas, United States; resolution: 1280 × 1024 64-bit color; graphic card: HD Graphics; Intel, Santa Clara, California, United States) using EzDent-i software (VATECH Global, Korea) was used. Software image enhancement functions were used by the examiner whenever the need was felt for better assessment. Before the study, 20 OPGs, of which 20 reference root canal-treated teeth not included in this cross-sectional evaluation were used for calibration of the single examiner. Intra-examiner agreement for the periapical index scores in root canal-treated teeth was measured by computing Cohen’s Kappa coefficient (κ) after re-examining the reference teeth. The κ value for intra-examiner agreement was 0.78 indicating substantial agreement.
Root canal treatment evaluation
Teeth obturated with a radio-opaque material in the pulp chamber and/or in one or more of the root canals were categorized as root canal treated. In multirooted teeth, the canal with the most incomplete filling was taken into consideration. The evaluation criteria described previously by Tronstad et al. [19] and Tavares et al. [20] were used in slightly modified form, which states:
-
Adequate treatment: All canals obturated. Voids not present. Root canal fillings end from 0 to 2 mm short of the radiographic apex.
-
Inadequate treatment: Grossly deficient root fillings (Root canal fillings end > 2 mm short of the radiographic apex or with inadequate density, unfilled canals, and/or poor compaction) or grossly overfilled.
Coronal restoration evaluation
The coronal restoration quality was determined both clinically and radiographically. The evaluation criteria used were somewhat modified from those stated by Tronstad et al. [19] and Song et al. [21] as follows:
-
Adequate restoration: Any permanent restoration that seemed intact radiographically and had no comment on the clinical examination record.
-
Inadequate restoration: Any permanent restoration with detectable radiographic signs of overhangs, recurrent caries, open margins or presence of temporary coronal restoration or comments such as “ill-fitting margin” or “secondary dental caries” on the clinical examination record. Teeth with no coronal restorations, permanent or temporary, were also included in this group.
Periapical status evaluation
The Periapical Index (PAI) scoring system [22] was used to assess the presence or absence of AP in each sample tooth, using a scale ranging from 1 to 5. Healthy teeth were designated by scores of 1 or 2 while scores of 3 to 5 specified the presence of AP. Multirooted teeth were categorized according to the root with the worst score. The five categories used were as follows:
-
1.
Normal periapical structures.
-
2.
Small changes in periapical bone structure.
-
3.
Changes in periapical bone structure along with some mineral loss.
-
4.
Periodontitis with a well-defined radiolucent area.
-
5.
Severe periodontitis with elements showing expansion of the lesion.
All teeth were categorized according to the Fédération Dentaire Internationale (FDI) nomenclature. The data recorded on a structured proforma for each patient were: age and sex; teeth present (excluding third molars); type of teeth that were root canal treated: incisors, canines, premolars or molars; type of coronal restorations in root treated teeth: an indirect restoration i.e., full coverage crown or a direct restoration i.e., filling; quality of RCT, quality of CR, and the PAI score of the root-treated teeth.
Statistical analysis
Raw data obtained were entered and coded in Excel sheets (Microsoft; Redmond, WA, USA). All statistical analyses were performed by using SPSS software (Statistical Package for Social Sciences, version 24.0, IBM, Chicago, IL, USA). Risk of AP was evaluated by means of odds ratios (OR) and the corresponding 95% confidence interval. A p-value of < 0.05 was considered statistically significant. The outcome variable was the presence versus absence of AP in the tooth. Univariate logistic regression model was used to investigate the association of diverse variables with AP. The variables having significant associations in univariate analysis were entered in multivariate regression model to find significant predictors of AP.
Results
A total of 172 patients were selected in the present study, of whom 74 were males and 98 were females. The average patient age was 41.55 years (range = 18–80 years). From the selected patients, a total number of 300 root canal treated teeth were assessed. Table 1 shows a descriptive analysis of the study sample. Of the 300 teeth, 128 (42.7%) were from males and 172 (57.3%) were from females. The highest prevalence of root treated teeth was in the 18–29 years age category (22.7%) followed by the ≥ 60 years age category (21.7%). Among the types of teeth, molars were the most commonly root canal treated (54.3%). On the basis of PAI scoring criteria, 205 (68.3%) teeth were categorized as healthy and 95 (31.7%) teeth had AP.
Table 2 presents the descriptive data of root canal treatment and coronal restoration quality. Short obturation i.e., grossly deficient root fillings, was found in 38.3% of the sample. Coronal restorations with recurrent caries were seen in 19% of root treated teeth.
Table 3 depicts the results of unadjusted (univariable) logistic regression model for diverse variables association with AP. A decreased risk for AP was demonstrated in females (OR = 0.51; 95% CI: 0.31–0.84; p = 0.009) than males. In contrast, the association between the variables age category and tooth type with AP was not apparent. The number of teeth with adequate root canal therapy was 137 (45.7%). Of these adequately treated teeth, 89.8% were classified as healthy (AP absent) and 10.2% were classified as diseased (AP present). The number of root fillings ranked as inadequate was 167 (54.3%). Out of these teeth with inadequate treatment, 50.3% were scored as healthy and 49.7% had AP. The teeth with inadequate root canal treatment showed an increased AP risk (OR = 8.67; 95% CI: 4.61–16.33; p < 0.001).
Forty-six percent of the root canal treated teeth comprised in this study presented coronal restoration classified as adequate. Of these, 84.8% were ranked as healthy. Inadequate coronal restorations were found in 54% of the teeth. Of these, only 54.3% were scored as healthy. A significant association with presence of AP was seen in teeth with inadequate quality restorations (OR = 4.68, 95% CI: 2.68–8.18; p < 0.001; Table 3). Regarding the type of coronal restorations, 42.0% of the endodontically treated teeth were restored with crown and 42.7% with filling, whereas 15.3% had no coronal restorations i.e., lost restorations. Taking lost restoration as a reference category, statistically significant association and decreased AP risk was demonstrated in teeth restored with crown and filling, (OR = 0.20; 95% CI: 0.10–0.42; p < 0.001) and (OR = 0.20; 95% CI: 0.09–0.41; p < 0.001), respectively.
Univariate logistic regression was also applied to analyse the association of combined quality of root canal treatment and coronal restoration with AP (Table 4). The combination of adequate RCT and adequate CR showed the lowest AP prevalence (2.2%) and this combination was taken as a reference category. Statistically significant associations and increased AP risk was seen in teeth with adequate RCT and inadequate CR (OR = 16.52; 95% CI: 3.54–77.03; p < 0.001), teeth with inadequate RCT and adequate CR (OR = 28.60; 95% CI: 6.24-130.97; p < 0.001) and teeth with inadequate RCT and inadequate CR (OR = 52.05; 95% CI: 12.22–221.60; p < 0.001).
In multivariate model, only those variables having significant associations in univariate regression analysis, were included (Table 5). The results showed that three variables i.e., sex, root canal treatment quality and coronal restoration type maintained the significant associations with AP presence. Females were less susceptible to AP development in root canal treated teeth in contrast to males (OR = 0.53; 95% CI: 0.30–0.95; p = 0.035). Regarding root canal treatment quality, the OR for the AP presence was 7.92 times higher if RCT quality was inadequate (OR = 7.92; 95% CI: 3.96–15.82; p < 0.001). When comparing to the lost restorations, root canal treated teeth restored with crown and filling showed significantly decreased odds for AP presence, (OR = 0.30; 95% CI: 0.12–0.71; p = 0.007) and (OR = 0.25; 95% CI: 0.10–0.59; p = 0.002), respectively.
Discussion
The current study aimed to evaluate the prevalence and determining factors of AP in root canal treated teeth from an adult Nepalese subpopulation of Madhesh Province. The findings of this study demonstrate that the AP prevalence in root treated teeth was 31.7%, which is comparable to earlier studies that used panoramic radiographs [23, 24]. A systematic review with meta-analysis [11] showed AP presence in 36% of cases. High AP prevalence observed in this study was mostly associated to the higher prevalence of teeth with inadequate root canal therapy.
This study marks the inaugural research effort of its kind conducted in the Madhesh Province. The sample examined consisted of patients who visited dental OPD of NMCTH Birgunj, situated in the Madhesh Province of Nepal. Similar screening criteria based on dental school patient selection have been employed in several other prevalence studies [16, 21, 24]. As NMCTH Birgunj stands as the sole dental institute and tertiary care referral dental center in Madhesh Province, individuals from all districts of the province avail themselves of its specialized dental services. Madhesh Province, located in the southeastern Terai region of Nepal and bordering Koshi Pradesh to the east and north, Bagmati Province to the north, and India’s Bihar state to the south and west, exhibits a population distribution of 50.1% males and 49.9% females [25]. Nonetheless, it is crucial to note that our subjects did not constitute a random sample of the Madhesh province population; rather, they were individuals actively seeking dental treatment. Therefore, the results are limited to the specific group studied and may not be applicable to the general population. However, in this study, the AP frequency and its associations with variables can be identified.
Based on the existing data, Nepal has a dentist-to-population ratio of 1:20000, nearly three times below the World Health Organization’s (WHO) recommended ratio [26]. The majority of practitioners in the province are general dentists, and the distribution of specialization in subdisciplines is limited. Regrettably, instances of quackery and fraudulent dental practices are noted within the province [26].
In the present study, panoramic radiograph was used to score the periapical status. Several epidemiological studies have used dental panoramic radiographs for evaluating the AP and the technical quality of RCT [16, 24]. Panoramic radiographs were employed in this study due to their availability, given that full-mouth periapical radiographs were not routinely taken in our college. With panoramic images, all teeth present can be visualized on one radiograph and a large amount of data is comfortably accumulated without exposing the individuals to extra radiation. These features make panoramic radiographs beneficial compared to full-mouth periapical radiographs [24]. Additionally, in the identification of periapical lesions, no significant difference has been found between the sensitivities of panoramic and full-mouth periapical radiographs [27, 28]. Contemporary panoramic machines generate higher-quality radiographic images, including improved clarity in the anterior region. Consequently, panoramic radiographs are considered a suitable diagnostic tool for assessing apical lesions in epidemiological studies related to dental care [27, 28].
Our study sample consisted of more females (56.97%) than males (43.02%), which may reflect the considerable interest of females within Nepal in receiving dental treatment. The predominance of female patients has also been shown in similar epidemiologic studies; however, those studies reported that gender did not correlate with the presence of AP [29, 30]. According to our results, females are less likely to have AP development in root canal-treated teeth than males. It is difficult to clarify the observed gender difference in our study. It would make sense if the males underwent root canal treatment when their teeth were in worse condition than females, potentially resulting in a poorer prognosis for therapy in males. Unfortunately, in this study, the preoperative condition, as well as details about the individuals who performed endodontic treatment, were not known. Future studies could help in understanding gender differences in the development of periapical lesions in root-filled teeth. In alignment with our study, Bürklein et al. [31] also observed a gender difference and linked it to diverse biopsychosocial factors affecting pain perception, including genetic factors, endogenous opioid function, sex hormones, pain coping, and gender roles. They further added that women tend to be more pain-sensitive and are more likely to seek dental care [31]. Corroborating our findings on gender differences, Jakovljevic et al. [6], in a meta-analysis, emphasized that despite conflicting outcomes in primary studies regarding the role of gender as a predisposing factor for the development of AP, numerous investigations have highlighted significant variations in oral hygiene practices between males and females.
More than half of the cases evaluated in the present study had inadequate root canal treatment. Similar findings have been observed in earlier studies conducted on different populations [32,33,34]. When analysing the causes of inadequate quality of RCTs, it was found that the most common cause was short obturation. This finding is consistent with previous studies [35, 36]. According to Strindberg [37], the success rate of endodontic treatment was highest when the root canal filling length was 1 mm shorter than the apex. The existence of microorganisms in the non-instrumented portions of the root canal may have caused the failure in teeth having short root fillings [38].
Previous studies have shown a lower apical disease rate in teeth with adequately filled root canals [19, 39]. Similar findings were observed in this study where 89.8% of adequate root treated teeth showed absence of AP. Furthermore, consistent with the earlier findings [21, 24], adequately root canal-treated teeth had significantly better periapical health than inadequately treated teeth. According to Siqueir Jr et al. [38], the major aetiological factor of post-treatment AP is persistent intra-radicular infection resulting from inadequate treatment which is similar to the finding of this study. Actually, multivariate logistic regression analysis demonstrated that the quality of root canal therapy was the most significant predictor of AP in root treated teeth. Compared to the teeth with adequate root canal treatment, AP was present approximately eight times more frequently in teeth with inadequate treatment. On the other hand, few cross-sectional studies [40, 41] have revealed no significant relationship between the quality of root canal therapy and the AP presence.
10% of teeth, despite having adequate quality RCTs, still had AP in the current study. This shows that the RCT quality is not the solitary factor affecting the periapical health of endodontically treated teeth. As stated by Moreno et al. [42], the coronal restoration quality is another factor that may affect the apical status. Similar to their findings [42], only 46% of the coronal restorations were classified as adequate in this study. The most common cause of inadequate quality restorations was recurrent caries. This emphasizes the significance of an adequate coronal seal after endodontic treatment. In univariate analysis, significantly better periapical health was found in teeth with adequate coronal restorations compared to the inadequate restorations. This result is analogous with the studies performed in Kuwait [43] and Jordan [29]. However, corresponding to the findings of Bukmir et al. [30], when the multivariate logistic regression was applied, this relationship did not remain significant. The presence of other significant variables in the multivariate model may have influenced this outcome.
In this study, a significant association was found between the type of coronal restoration and presence of AP. This is in agreement with the study by Frisk et al. [44]. This association may be due to the microleakage occurring from poor marginal integrity of the restorations which could not be identified clinically [44]. Moreover, other determining factors of AP might also have influenced the periapical status of the root-treated teeth. Contrary to this association, El Ouarti [45] found no relationship between coronal restoration type and AP.
Combined data for coronal restoration and root canal treatment quality yielded noticeable results. When both coronal restoration and root canal treatment were adequate, only 2.2% of the treated teeth had AP, however if both were inadequate, 53.91% of the teeth had AP. This strongly denotes that both factors i.e., quality of endodontic treatment and quality of coronal restoration play important roles in maintaining the periapical health of root treated teeth. Significantly worse outcome and remarkably increased odds for AP was found when either root canal treatment or coronal restoration was inadequate or when both were inadequate. The meta-analysis conducted by Gillen et al. [46] validated this finding, which showed that the odds for healing capacity of AP increase in teeth with both adequate endodontic treatment and adequate coronal restoration.
The main limitation of the present study was the usage of OPGs for assessing the periapical status. Disadvantages of OPGs are well known including a two-dimensional image of three-dimensional structures, superimposition, anatomic noise and geometric distortion. Furthermore, to be radiographically apparent, apical radiolucency should reach approximately 30-50% of the bone mineral loss. Thus, AP might be existing though not identified radiographically [47]. Cone beam computed tomography (CBCT) surpasses panoramic and periapical radiographs, as three-dimensional view permits more accurate estimation of the size and location of the lesion in addition to the detection of lateral voids and missed canals in the evaluation of technical quality [48]. But all dental practices are not equipped with CBCT [49]. More notably, owing to augmented risk of radiation, the CBCT indications are highly regulated, mostly limited to the zone of interest instead of the complete dentition [50].
Other limitations of this study were the lack of information concerning the evaluated cases which may affect the root canal treatment outcome, for example the operator factor, whether trained or untrained doctor performed the treatment in single or multiple visits and whether permanent restoration was placed just after root canal treatment completion. Furthermore, there was no information about the absence or presence of periapical radiolucency before root canal treatment (no preoperative radiograph was available), elapsed time of endodontic treatment, microbiological environment of the root canal, periodontal status and oral hygiene habits of the patients. Further prospective controlled trials are recommended to evaluate the detail role of each factor responsible for AP, clinically and radiographically.
Conclusions
Within the limits of this study, a high prevalence of AP and poor overall quality of root canal treatment and coronal restoration was found in the subpopulation studied. Quality of root canal treatment, type of coronal restoration and sex of the patient are significant predictors of possible AP development in root canal treated teeth. Substantial efforts are needed to improve the endodontic treatment standards.
Data availability
The datasets used during the present study are available from the corresponding author on reasonable request.
Abbreviations
- AP:
-
Apical periodontitis
- RCT:
-
Root canal treatment
- CR:
-
Coronal restoration
- OPG:
-
Orthopantomogram
- PAI:
-
Periapical index
- SPSS:
-
Statistical package for social sciences
- OR:
-
Odds ratio
- FDI:
-
Fédération Dentaire Internationale
- NMCTH:
-
National Medical College & Teaching Hospital
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- CI:
-
Confidence interval
- CBCT:
-
Cone-beam computed tomography
- WHO:
-
World Health Organization
References
Zieliński G, Filipiak Z, Ginszt M, Matysik-Woźniak A, Rejdak R, Gawda P. The Organ of Vision and the Stomatognathic System-Review of Association Studies and evidence-based discussion. Brain Sci. 2021;12(1):14.
Babu NC, Gomes AJ. Systemic manifestations of oral diseases. J Oral Maxillofac Pathol. 2011;15(2):144–7.
WHO Global oral health status report: towards universal health coverage for oral health by 2030. 2022. https://www.who.int/team/noncommunicable-diseases/global-status-report-on-oral-health-2022 Accessed 24 Sept 2023.
Hussein FE, Liew AK, Ramlee RA, Abdullah D, Chong BS. Factors Associated with apical periodontitis: a Multilevel Analysis. J Endod. 2016;42(10):1441–5.
Kassebaum N, Bernabé E, Dahiya M, Bhandari B, Murray C, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94(5):650–8.
Jakovljevic A, Nikolic N, Jacimovic J, Pavlovic O, Milicic B, Beljic-Ivanovic K, Miletic M, Andric M, Milasin J. Prevalence of apical periodontitis and conventional nonsurgical root canal treatment in general adult population: an updated systematic review and meta-analysis of cross-sectional studies published between 2012–2020. J Endod. 2020;46(10):1371–86. e8.
American Association of Endodontists: Glossary of endodontic terms. 2020. https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/ Accessed 24 Sept 2023.
Colombo M, Bassi C, Beltrami R, et al. Radiographic technical quality of root canal treatment performed by a new rotary single-file system. Ann Stomatol (Roma). 2017;8(1):18–22.
Van der Veken D, Curvers F, Fieuws S, Lambrechts P. Prevalence of apical periodontitis and root filled teeth in a Belgian subpopulation found on CBCT images. Int Endod J. 2017;50(4):317–29.
Tibúrcio-Machado CS, Michelon C, Zanatta FB, Gomes MS, Marin JA, Bier CA. The global prevalence of apical periodontitis: a systematic review and meta-analysis. Int Endod J. 2021;54(5):712–35.
Pak JG, Fayazi S, White SN. Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod. 2012;38(9):1170–76.
Kandelman D, Arpin S, Baez RJ, Baehni PC, Petersen PE. Oral health care systems in developing and developed countries. Periodontol 2000. 2012;60(1):98–109.
León-López M, Cabanillas-Balsera D, Martín-González J, Montero-Miralles P, Saúco-Márquez JJ, Segura-Egea JJ. Prevalence of root canal treatment worldwide: a systematic review and meta-analysis. Int Endod J. 2022;55(11):1105–27.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
Daniel WW, Biostatistics. A Foundation for Analysis in the Health Sciences. 7th ed. New York: Wiley; 1999.
López-López J, Jané-Salas E, Estrugo‐Devesa A, Castellanos‐Cosano L, Martín‐González J, Velasco‐Ortega E, Segura‐Egea JJ. Frequency and distribution of root‐filled teeth and apical periodontitis in an adult population of Barcelona, Spain. Int Dent J. 2012;6:40–6.
American Association of Endodontists (AAE). Guide to Clinical Endodontics. 2013. https://www.aae.org/specialty/clinical-resources/guide-clinical-endodontics/ Accessed 24 Sept 2023.
Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig. 2005;9(4):215–32.
Tronstad L, Asbjørnsen K, Døving L, Pedersen I, Eriksen HM. Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol. 2000;16(5):218–21.
Tavares PB, Bonte E, Boukpessi T, Siqueira JF Jr, Lasfargues JJ. Prevalence of apical periodontitis in root canal-treated teeth from an urban French population: influence of the quality of root canal fillings and coronal restorations. J Endod. 2009;35(6):810–13.
Song M, Park M, Lee C-Y, Kim E. Periapical status related to the quality of coronal restorations and root fillings in a Korean population. J Endod. 2014;40(2):182–6.
Ørstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Dent Traumatol. 1986;2(1):20–34.
Archana D, Gopikrishna V, Gutmann JL, Savadamoorthi KS, Kumar ARP, Narayanan LL. Prevalence of periradicular radiolucencies and its association with the quality of root canal procedures and coronal restorations in an adult urban Indian population. J Conserv Dent JCD. 2015;18(1):34.
Di Filippo G, Sidhu S, Chong B. Apical periodontitis and the technical quality of root canal treatment in an adult sub-population in London. Br Dent J. 2014;216(10):E22.
Government of Nepal National Data. http://nationaldata.gov.np/Province/Index/2 Accessed 2 Jan 2024.
Humagain M, Bhattarai BP, Rokaya D. Quackery in Dental Practice in Nepal. JNMA J Nepal Med Assoc. 2020;58(227):543–6.
Ahlqwist M, Halling A, Hollender L. Rotational panoramic radiography in epidemiological studies of dental health. Swed Dent J. 1986;10:79–84.
Muhammed AH, Mason-Hing LR, Ala B. A comparison of panoramic and intraoral radiographic surveys in evaluating a dental clinic population. Oral Surg Oral Med Oral Pathol. 1982;54:108–17.
Al-Omari MA, Hazaa A, Haddad F. Frequency and distribution of root filled teeth and apical periodontitis in a Jordanian subpopulation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(1):e59–65.
Persic Bukmir R, Paljevic E, Vidas J, Glazar I, Pezelj-Ribaric S. Brekalo Prso I. is coronal restoration a predictor of posttreatment apical periodontitis? Eur J Dent. 2022;16(2):386–95.
Bürklein S, Schäfer E, Jöhren HP, Donnermeyer D. Quality of root canal fillings and prevalence of apical radiolucencies in a German population: a CBCT analysis. Clin Oral Investig. 2020;24(3):1217–27.
De Moor R, Hommez G, De Boever J, Delmé K, Martens G. Periapical health related to the quality of root canal treatment in a Belgian population. Int Endod J. 2000;33(2):113–20.
Loftus J, Keating A, McCartan B. Periapical status and quality of endodontic treatment in an adult Irish population. Int Endod J. 2005;38(2):81–6.
Kabak Y, Abbott PV. Prevalence of apical periodontitis and the quality of endodontic treatment in an adult Belarusian population. Int Endod J. 2005;38(4):238–45.
Ricucci D, Russo J, Rutberg M, et al. A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:825–42.
Dammaschke T, Steven D, Kaup M, Reiner KH. Long-term survival of root-canaltreated teeth: a retrospective study of 10 years. J Endod. 2003;29:638–43.
Strindberg LZ. The dependence of the results of pulp therapy on certain factors. Acta Odontol Scand. 1956;14:1–175.
Siqueira JF Jr, Rôças IN, Ricucci D, Hülsmann M. Causes and management of post-treatment apical periodontitis. Br Dent J. 2014;216(6):305–12.
Sarıyılmaz E, Keskin C, Ozcan O. Retrospective analysis of post-treatment apical periodontitis and quality of endodontic treatment and coronal restorations in an elderly Turkish population. J Clin Gerontol Geriatr. 2016;7:17–20.
Marques MD, Moreira B, Eriksen HM. Prevalence of apical periodontitis and results of endodontic treatment in an adult, Portuguese population. Int Endod J. 1998;31(3):161–5.
Da Silva K, Lam JM, Wu N, Duckmanton P. Cross-sectional study of endodontic treatment in an Australian population. Aust Endod J. 2009;35(3):140–6.
Moreno JO, Alves FR, Gonçalves LS, Martinez AM, Rôças IN, Siqueira JF Jr. Periradicular status and quality of root canal fillings and coronal restorations in an urban Colombian population. J Endod. 2013;39(5):600–4.
Maslamani M, Khalaf M, Mitra AK. Association of Quality of Coronal Filling with the outcome of Endodontic Treatment: a follow-up study. Dent J (Basel). 2017;5(1):5.
Frisk F, Hugosson A, Kvist T. Is apical periodontitis in root filled teeth associated with the type of restoration? Acta Odontol Scand. 2015;73(3):169–75.
El Ouarti I, Chala S, Sakout M, Abdallaoui F. Prevalence and risk factors of apical periodontitis in endodontically treated teeth: cross-sectional study in an adult Moroccan subpopulation. BMC Oral Health. 2021;21(1):124.
Gillen BM, Looney SW, Gu L-S, Loushine BA, Weller RN, Loushine RJ, Pashley DH, Tay FR. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod. 2011;37(7):895–902.
Nardi C, Calistri L, Pradella S, Desideri I, Lorini C, Colagrande S. Accuracy of Orthopantomography for apical periodontitis without Endodontic Treatment. J Endod. 2017;43(10):1640–46.
Karabucak B, Bunes A, Chehoud C, et al. Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. J Endod. 2016;42:538–41.
Estrela C, Bueno MR, Leles CR, et al. Accuracy of cone beam computed tomography and panoramic radiography for detection of apical periodontitis. J Endod. 2008;34:273–9.
The American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry. J Am Dent Asso. 2012;143:899–902.
Acknowledgements
None.
Funding
The present study didn’t receive any funding.
Author information
Authors and Affiliations
Contributions
MAH: conception, investigation, data curation, data analysis & interpretation, methodology, project administration, visualization, writing-original draft, writing-review & editing. SKS: methodology, supervision, validation and writing-review & editing. SN: supervision, validation and writing-review & editing. MH: acquisition and reviewed manuscript. HKS: project administration and reviewed manuscript. AS – statistical analysis, data interpretation and writing-review & editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance for the study was obtained from the Institutional Review Committee of National Medical College, Birgunj (Ref. F-NMC/613/079–080). All participants gave their written consent prior to inclusion in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hussain, M.A., Singh, S.K., Naz, S. et al. Predictors of apical periodontitis in root canal treated teeth from an adult Nepalese subpopulation: a cross-sectional study. BMC Oral Health 24, 400 (2024). https://doi.org/10.1186/s12903-024-04139-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04139-3