Abstract
Background
The most severe complication that can occur after mandibular third molar (MM3) surgery is inferior alveolar nerve (IAN) damage. It is crucial to have a comprehensive radiographic evaluation to reduce the possibility of nerve damage. The objective of this study is to assess the diagnostic accuracy of panoramic radiographs (PR) and posteroanterior (PA) radiographs in identifying the association between impacted MM3 roots and IAN.
Methods
This study included individuals who had PR, PA radiographs, and cone beam computed tomography (CBCT) and who had at least one impacted MM3. A total of 141 impacted MM3s were evaluated on CBCT images, and the findings were considered gold standard. The relationship between impacted MM3 roots and IAN was also evaluated on PR and PA radiographies. The data was analyzed using the McNemar and Chi-squared tests. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy of PR and PA radiographies were determined.
Results
Considering CBCT the gold standard, the relationship between MM3 roots and IAN was found to be statistically significant between PR and CBCT (p = 0.00). However, there was no statistically significant relationship between PA radiography and CBCT (0.227). The study revealed that the most prevalent limitation of the PR in assessing the relationship between MM3 roots and IAN was the identification of false-positive relationship.
Conclusions
PA radiography may be a good alternative in developing countries to find out if there is a contact between MM3 roots and IAN because it is easier to get to, cheaper, and uses less radiation.
Similar content being viewed by others
Background
An impacted tooth refers to a tooth that is unable to emerge into the dental arch within the anticipated timeframe due to a physical obstruction, insufficient space, or improper positioning [1]. Mandibular third molars (MM3s) have the highest likelihood of becoming impacted [2]. Numerous reasons have been elucidated in the literature regarding the impaction of the lower third molars. The most common causes of impaction of the lower third molar include abnormal positioning of the tooth germ, insufficient space in the dental arch, ankylosis of the deciduous or permanent tooth, bone that does not resorb due to local or systemic reasons, bone obstruction along the eruption path, or obstruction by adjacent teeth, and various syndromes [3]. Various etiological factors may contribute to the impaction of third molars, but craniofacial development is certainly one of the most significant factors. It has been reported that there is a correlation between the impaction classification types of lower third molars and ramus height/gonial angle. A lower gonial angle was found to be significantly associated with a higher prevalence of impaction of the lower third molars. A decreased gonial angle is associated with a reduced retromolar space, thereby supporting the impaction of the lower third molars and their closer proximity to IAN during development [4, 5]. Impacted MM3s can lead to a variety of problems, including caries, pericoronitis, resorption, bone loss in the distal surface of the second molar, cystic or neoplastic conditions, and myofascial and neurogenic pains [1, 6] Furthermore, impacted MM3s may cause temporomandibular joint disorders, dental problems like crowding, weaken the mandibular angle, and potentially cause fractures [2].
Surgical removal of impacted MM3s is a frequently performed operation in oral and maxillofacial surgery for prophylactic, therapeutic, and orthodontic reasons [1, 7]. The extraction of impacted MM3s can lead to various complications, such as swelling, pain, infection, excessive bleeding, and reduced mouth opening [8,9,10]. However, one of the most severe postoperative complications is the injury of the inferior alveolar nerve (IAN), which results in reduced sensation in the lower lip and mandible. Postoperative sensory impairment might exhibit either permanent or temporary characteristics [1, 11]. If individuals with IAN injuries do not show spontaneous healing within a period of 6 months, the IAN damage is deemed to be permanent [12]. According to various studies, the incidence of cases with permanent IAN damage has been reported as less than 1% [13, 14]. The occurrence of temporary nerve injuries is often estimated to range from 0.4 to 8% [13, 14]. However, in cases where there is close proximity between the MM3 roots and IAN, the incidence can be as high as 30% [13]. IAN damage may affect patients’ quality of life by causing mental and social problems [13, 15]. It has also been reported that this is the most common cause of complaints against oral and maxillofacial surgeons in forensic courts, increasing the public’s belief that surgical negligence occurs during surgery [13].
The incidence of IAN damage is influenced by several factors, including the surgeon’s experience, the gender and age of the patient, the type of anesthesia, and the anatomical relationship between the mandibular canal and MM3 [12]. In contrast, Ghaeminia et al [16] reported that there is no significant relationship between IAN injury and the experience of the surgeon, age, or gender of the patient. It has been suggested that the close proximity of the MM3 roots to the IAN and their positional relationship are the most important risk factors. IAN injury can occur during the surgical removal of MM3s due to many factors, such as indirect compression, insufficient bone cortex around the IAN, or direct trauma. When the MM3s anatomically contact the IAN, the risk of IAN damage increases after tooth extraction [17]. To limit this risk, it is important to determine the location of the IAN relative to the MM3 roots before the surgery using a radiographic examination [11].
For an optimal radiographic assessment of impacted MM3s, it is important to assess dental features such as root development, morphology, and number of roots. Additionally, the relationship between the impacted tooth and the surrounding bone, neighboring teeth, and anatomical structures should be assessed [18]. There is no specific protocol for the radiographic evaluation of MM3s [19]. Panoramic radiographs (PRs), which are the most commonly used in radiographic examination, are the first choice of dentists in determining the relationship between MM3 roots and the IAN due to their short scanning time, low radiation dose, and easy accessibility [17]. Furthermore, PR is also employed to assess the root morphology, degree of impaction, and angulation of the MM3s [20]. Nevertheless, PR has drawbacks, including poor image resolution, anatomical noise, overlapping of structures, geometric distortion, and the occurrence of phantom images [1, 17]. Establishing the connection between MM3 roots and IAN on PR might be challenging owing to the overlapping of the roots on the IAN, particularly when tooth roots are positioned on the buccal or lingual side of the IAN [17]. Hence, the exact anatomical relationship between MM3s and IAN cannot be determined using PRs [20]. Rood and Shehab [21] proposed the utilization of seven radiographic indicators that demonstrate the proximity between MM3 and IAN in PR. If a relationship between MM3 roots and IAN in PR is suspected based on these signs, it may be necessary to evaluate the relationship with cone beam computed tomography (CBCT). CBCT, which is one of the advanced imaging methods, provides a three-dimensional representation of the relationship between impacted MM3s and IAN, which contributes to simplifying preoperative planning and minimizing the likelihood of IAN damage [17]. However, CBCT is not commonly employed as a routine radiographic examination because of its limited accessibility, high cost, and radiation exposure [15, 17].
The posteroanterior (PA) radiograph is the second most commonly utilized skull radiograph in dentistry [22]. PA radiographs are necessary for assessing the transverse dimensions of the dentoalveolar structures and craniofacial skeleton [23]. For all that, it has been reported that PA radiographs can be utilized to determine the relationship between impacted MM3 roots and IAN [18].
The utilization of the CBCT technique is widely regarded as the most reliable method for assessing the relationship between the roots of MM3 and IAN [24]. The aim of this study is to evaluate the reliability of PR and PA radiographs in detecting the relationship between impacted MM3 roots and IAN. The null hypothesis of this study was that ‘there is no statistically significant difference between PR and PA radiographs in detecting the relationship between impacted MM3 roots and IAN’.
Methods
This study was carried out in accordance with the principles outlined in the Declaration of Helsinki and received ethical approval from the Pamukkale University Non-Interventional Clinical Research Ethics Committee (E-60116787-020-374406). The sample size was calculated for the effect size (d, effect size = 0.85), type I error (α = 0.05), and 85% power values, the sample size was determined to be at least 80 for the study group.
Individuals who had all PR, PA radiography, and CBCT images obtained in the same week in the Pamukkale University Faculty of Dentistry archive and had at least one impacted MM3 were included in the present study. Images displaying incomplete root development and bone pathology in the evaluated area were omitted from the study. For the study on the CBCT images of 83 patients (25 males, accounting for 30.12%, and 58 females, accounting for 69.88%), a total of 141 impacted MM3s were evaluated, and CBCT was considered the gold standard. The PR and PA radiographs were obtained with the same device (Instrumentarium OP 200D, Tuusula, Finland), and CBCT images were obtained with Newtom 5G XL (Cefla, Imola, Italy) following the instructions provided by the manufacturer.
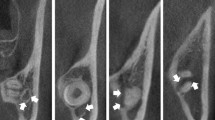
The angulations of the impacted MM3s, the locations of the impacted MM3 roots according to the IAN, and the presence of contact between the IAN and the impacted MM3s were evaluated on CBCT images. Two observers, one with 2 years of experience and the other with 13 years of experience in dentomaxillofacial radiography, assessed these factors (Figs. 1 and 2). The angulations of the impacted MM3s were evaluated according to the classification system of Winter as vertical, mesioangular, horizontal, distoangular, buccolingual, and others on all imaging techniques included in the study [25].
The location of the MM3 roots was classified as at the lingual, interradicular, buccal, and inferior of the IAN on the CBCT images [26]. The presence of the relationship between impacted MM3 roots and IAN was also evaluated on PR and PA radiographies independently by the same two observers under dim lightning conditions on a medical monitor (Barco MDNC-2221monitor, resolution 1600 × 1200, size 432 × 324, Barco, Kortrijk, Blegium), and inter-observer agreement was evaluated.
Statistical analysis
The data was analyzed by using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). Inter-observer agreement was analyzed with the Cohen’s kappa test. Kappa values less than or equal to 0 were classified as indicating no agreement. Values ranging from 0.01 to 0.20 were considered to indicate no to minor agreement, while values between 0.21 and 0.40 were classified as fair agreement. Kappa values ranging from 0.41 to 0.60 were considered to indicate moderate agreement, while values between 0.61 and 0.80 were classified as significant agreement. Finally, values between 0.81 and 1.00 were considered to indicate practically perfect agreement [27]. Descriptive statistics were carried out, and results on categorical measurements were given as numbers and percentages. The data was analyzed using McNemar and Chi-squared tests. p ≤ 0.05 values were considered statistically significant. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy of PR and PA radiographies were determined.
Sensitivity: True positive (TP)/(False negative(FN) + TP)
Specificity: True negative (TN)/(False positive (FP) + TN)
PPV: TP/(TP + FP)
NPV: TN/(FN + TN)
Diagnostic accuracy: (TP + TN)/(TP + FP + TN + FN)
Results
The present study sample consisted of 141 impacted third molars from 83 individuals, whose ages ranged from 18 to 42, with a mean age of 25.95 ± 7.9 years. Out of the total number of teeth, 76 (53.9%) were found in the left mandible, while 65 (46.1%) were found in the right mandible. The evaluations on CBCT images were performed with consensus by two observers with 2 and 13 years of experience in dentomaxillofacial radiology. PR and PA radiography were evaluated independently by two observers, and kappa values were 0,862 and 0,815, respectively. The different assessments were re-evaluated by two observers, and the final decision was made. According to the results of the kappa analysis, the interobserver agreement was found to be almost perfect.
Table 1 shows the distribution of angulation types of MM3s on PR, PA radiography, and CBCT images. When the teeth were evaluated according to angulation, the highest canal relationship was seen in the buccolingual position, followed by the horizontal position. According to the location of roots relative to IAN, the presence of a relationship between IAN and impacted MM3 roots were most common in the lingual and interradicular positions, respectively. The difference between PR and PA radiographs was statistically significant in terms of the angulation of impacted MM3s (p = 0.00). The distribution of the presence of a relationship between MM3 roots and IAN according to angulations and the locations of the MM3 roots relative to IAN is seen in Tables 2 and 3. When the predictability of the relationship between MM3 roots and IAN was evaluated for PR and PA radiography according to the CBCT as gold standard, while the difference between PR and CBCT assessments was found to be statistically significant (p = 0.00), there was no significant difference between PA radiography and CBCT (p = 0.227). According to the results of our study, false positive relationship diagnosis was the most common handicap of the PR in evaluating contact between MM3 roots and IAN (Table 4).
The diagnostic accuracy of PR and PA radiography was 0.6 and 0.92, respectively, which indicates that the the presence of the relationship between MM3 roots and IAN is predictable at 60% in PR and 92% in PA radiography. When the diagnostic performance of the two imaging modalities was evaluated, the most significant difference was seen to be specificity at 0.22 and 0.88, respectively, for PR and PA radiography. PPV (0.56) and NPV (0.83) were also lower in PR compared to PA radiography. The sensitivity of both PR and PA radiographies was 0.96, which states that predictability is high for both imaging methods when there is a contact. (Table 5).
Discussion
Before deciding to remove the MM3s, taking a radiographic image allows for the evaluation of the whole tooth, the bone around it, and its relationship with adjacent anatomical tissues. This aids the oral and maxillofacial surgeon in selecting the most suitable surgical approach [7, 19]. Oral and maxillofacial surgeons must inform the patient about the likelihood of IAN injury that may occur during the extraction of MM3s [19].
In this study, the Winter [25] classification was used to evaluate the angulation of impacted MM3s. Vertical position was the most common type, followed by mesioangular, horizontal, and buccolingual, respectively. This result is in disagreement with some other studies, which found the mesioangular position most common [14, 20, 28,29,30]. However, similar to this study, there are also studies showing that the vertical position is the most common, followed by the mesioangular position [30, 31].
The proximity of the MM3 roots to the mandibular canal may cause injury to IAN during the extraction of MM3s [32]. Paresthesia, albeit transient, is the primary source of discomfort and concern for patients [33]. Hence, a comprehensive radiographic assessment of this anatomical relationship is essential to apprise the patient of the potential hazards and formulate suitable surgical strategies [19, 20].
Currently, there is no definitive protocol for pre-extraction radiographic examination of MM3s, and therefore, there are no strict guidelines for dentists to follow. However, dentists should not perform surgery on MM3s without adequate radiographic evaluation. Without sufficient imaging procedures, a correct diagnosis cannot be made and may adversely affect the decision on appropriate treatment. Pathological findings may go unnoticed. In order to ensure thorough and well-informed consent, it is necessary to have radiological findings and clinical information that substantiate the pathology and associated risks. Hence, despite the lack of definitive evidence on the reduction of morbidity or complication rate, it is imperative to thoroughly investigate the region by radiographic imaging prior to surgical intervention [18].
Despite the disadvantages of magnification, distortion, and overlapping, PRs are the first choice of dentists to assess the surrounding anatomy of MM3s and the IAN due to their short scanning times, low radiation dosage, and easy accessibility [12, 17]. However, it is indeterminable whether the IAN course is positioned buccally or lingually of the MM3 roots or between the roots with PR [34]. Tantanapornkul et al. [35] found that the sensitivity and specificity of PR were 70% and 63%, respectively, and concluded that CBCT is significantly superior to PR for predicting the relationship between IAN and MM3s. In a study conducted by Sedaghatfar et al. [14] the researchers assessed the sensitivity and specificity of several predictors on PR. The sensitivity rates ranged from 17 to 71%, while the specificity rates ranged from 66 to 91%. However, in the case of the study in question, it was not specified which relationship type should be preferred in estimating the existence of exposure. The study conducted by Bell et al. [36] found that the sensitivity and specificity values for assessing the relationship between MM3 roots and IAN on PR are %66 and %74, respectively. The study found that the sensitivity of PR in predicting the contact between MM3 roots and IAN was 96%, whereas the specificity was 22%. In research conducted by Gomes et al. [37], it was shown that 61% of the cases had symptoms suggesting a connection between IAN and MM3s in PR. However, only 3.5% of the patients experienced paresthesia, and PR was not able to predict neurosensory problems.
On the other hand, several authors have reported that radiographic signs observed in PR, which serve as indications of the close anatomical relationship between MM3 roots and IAN, can be valuable in predicting IAN sensory impairment before surgery [15, 21, 26, 32]. The known classifications made on 2D radiographs by authors such as Winter, Pell&Gregory, and Rood&Shehab are still widely used for risk assessment in the removal of MM3s [21, 25, 38]. Although there are studies reporting that the angulation of impacted third molars is not a risk factor for inferior alveolar nerve damage [34, 39], there are also studies determining that angulation is associated with inferior alveolar nerve damage [30, 32]. Although Rood & Shehab suggested seven radiographic signs to predict the closeness between MM3 and IAN, four of these signs were found to be more effective in detecting the relationship [14]. Furthermore, Flygare and Ohman [40] reported that PR is generally acceptable for assessing the distance between MM3 roots and IAN in cases where there is no overlap between the two. Luo et al. [6] proposed that the close relationship between MM3 and IAN via the PR could be enough to anticipate future hypoesthesia of the chin or lip. Based on their study findings, they concluded that having a quality PR image and well-planned surgery can effectively reduce the likelihood of damage to the IAN.
While PR has traditionally been the main radiographic method used to assess different risk factors related to MM3 extraction, the development of additional methods has made it essential to compare these approaches with PR [20]. European guidelines advise the use of presurgical CBCT evaluation when the two-dimensional image indicates a significant proximity between the MM3 roots and the mandibular canal [41].
CBCT images provide valuable data for evaluating the relationship between MM3 roots and IAN in three dimensions. Additionally, these three-dimensional images are beneficial for preoperative planning and identifying alternate surgical methods [42]. Several previous studies have examined the characteristics of PR and CBCT in relation to impacted MM3s and IAN [1, 7, 20, 32, 43]. Multiple studies have consistently indicated that CBCT is superior to PR in assessing the relationship between the IAN and MM3 [7, 13, 35, 43]. Research has indicated that the additional information obtained from CBCT scans might potentially alter the surgical technique, leading to a decreased likelihood of damage to the IAN [26, 33, 35, 42]. Conversely, several studies have found that CBCT does not have any impact on either the treatment plan or the outcome of patients after surgery [1, 19, 34]. Surgical planning with CBCT for the removal of MM3s was found to have minimal impact on permanent IAN damage at long-term follow-up [33, 42]. Matzen et al. [19] reported that preoperative radiography techniques alone do not have an impact on the occurrence of IAN injuries. However, they noted that other factors, such as the anesthetic method employed during surgery, might potentially lead to IAN damage. The skill and proficiency of the performing surgeon have a significant impact on the extent of the IAN injury [43]. However, several oral and maxillofacial surgeons routinely obtain CBCT before MM3 surgery to eliminate legal liability [34].
The increasing complexity of cross-sectional imaging techniques plays a crucial role in the diagnosis of conditions related to third molars, which can be challenging for inexperienced radiologists in dental imaging [44]. Comprehensive knowledge of the imaging features of these abnormalities assists the practicing radiologist in achieving an accurate diagnosis, thus improving patient care [45]. CBCT enables detailed evaluation of impacted molars, odontogenic lesions, and jaw malformations. The angle of the impacted tooth and the distance between MM3 and IAN can be accurately determined in CBCT images without magnification [44,45,46]. CBCT imaging is often characterized by a longer time needed and a higher cost compared to two-dimensional radiographs. The mentioned cost depends not only on the high price of the CBCT device but also on the need to employ additional personnel [23, 47]. Petersen et al. [48] discovered that the cost of CBCT examinations is three to four times higher than the cost of PR examinations. Furthermore, it is crucial to acknowledge that while CBCT has a lower radiation dosage in comparison to spiral CT, it nevertheless subjects the patient to a higher level of radiation when compared to conventional radiographs [22, 23].
The utilization of CBCT is less common, particularly in developing countries, as a result of socioeconomic circumstances. While PR does not permit buccolingual dimensional assessment, it can nonetheless serve as the only radiographic examination technique prior to MM3 surgery in developing countries [15, 34]. Hence, it has been proposed that, if feasible, other methods with lower radiation levels should be taken into account to assess the radiationship between MM3 roots and IAN [33, 41].
When looking at the maxillofacial area, PA cephalometric radiographs are very important because they provide valuable mediolateral information, which is essential for evaluating the transverse relationships between craniofacial skeleton and dentoalveolar structures. Furthermore, PA cephalometric radiographs are characterized by their inexpensive cost and low radiation dose. PA cephalometric radiographs offer unique diagnostic insights that are not attainable by other two-dimensional imaging techniques [49]. Nevertheless, due to the nature of PA radiography being a two-dimensional technology, the picture is subject to distortion and projection. This impacts the precision of linear measurements acquired from PA radiographs. However, PA radiography may be utilized to compare the structures on both sides of the head, as they are positioned at about similar distances from the film and X-ray source [23]. PA radiographs can be used to determine the relationship between impacted MM3 and IAN [18]. In this study, the sensitivity and specificity of PA in predicting nerve exposure were 96% and 88%, respectively. The rates in question exhibit a significant disparity when compared to PR, the alternative approach assessed in this study.
PA radiography is not commonly performed as part of the standard diagnostic and treatment planning processes. Hence, there is a possibility of inaccuracies in the interpretation and recognition of anatomical landmarks on PA radiographs. Particularly in individuals aged 11 to 15, the superimposition of third molars might make it challenging to detect dental landmarks [50]. These are the limitations of using PA radiographs [51]. However, it has been reported that the occurrence of interpretation mistakes may be diminished with the use of precise definitions and comprehensive training [52]. According to Major et al. [53], operator expertise plays a crucial role in recognizing anatomical landmarks in radiological images due to their increasing familiarity with these appearances. Tai et al. [51] conducted research to assess the reliability of transverse dimensions in PA and CBCT. The study found no significant bias in intraobserver agreement. When the mandibular molar region was evaluated with PA, interobserver agreement was reported to be excellent [52]. Likewise, there was a significant level of agreement among observers in this study.
Obtaining both CBCT and PA radiography from a patient to assess their reliability raises ethical concerns. Consequently, the main limitation of this study is that it is a retrospective archival analysis with a relatively limited sample size. Therefore, it was a study in which only radiographic findings were evaluated, without clinical results, and since the study was an archive analysis, we did not have a role in improving the image quality by minimizing errors that may occur during radiographic imaging. In addition, in our study, only the presence of a relationship between MM3 roots and IAN was evaluated. A detailed classification based on radiographic signs (such as Rood and Shehap’s signs) and the correlation between patient age and MM3 and IAN were not evaluated. Future studies will contribute to the literature by investigating the radiographic signs that are used to determine the relationship between MM3 and IAN in PA radiographs.
Conclusions
CBCT is unequivocally superior to other procedures due to its ability to assess the interrelationships of anatomical components in three dimensions without overlap and with little dimensional magnification. However, considering the accessibility in developing countries, the cost and radiation dose of CBCT, and due to their handicap, false positive relationship diagnosis of PR, PA radiography may be a reasonable option to evaluate the relationship between MM3 roots and IAN by providing mediolateral information.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality of personal information but are available from the corresponding author on reasonable request.
Abbreviations
- MM3:
-
Mandibular third molar
- IAN:
-
Inferior alveolar nerve
- PR:
-
Panoramic radiograph
- CBCT:
-
Cone beam computed tomography
- PA:
-
Posteroanterior
References
Patel P, Shah J, Dudhia B, Butala P, Jani Y, MacWan R. Comparison of panoramic radiograph and cone beam computed tomography findings for impacted mandibular third molar root and inferior alveolar nerve canal relation. Indian J Dent Res. 2020;31(1):91–102.
Eshghpour M, Nezadi A, Moradi A, Mahvelati Shamsabadi R, Rezaei NM, Nejat A. Pattern of mandibular third molar impaction: a cross-sectional study in northeast of Iran. Niger J Clin Pract. 2014;17(6):673–7.
Jeevitha JY, Thiagarajan A, Sivalingam B. Influence and impact of Mandibular Ramal dimensions on the incidence of Lower Third Molar Impaction: a prospective study. J Pharm Bioallied Sci. 2022;14(Suppl 1):364–8.
Barone S, Antonelli A, Averta F, et al. Does Mandibular Gonial Angle Influence the Eruption Pattern of the Lower Third Molar? A three-dimensional study. J Clin Med. 2021;10(18):4057.
Gümrükçü Z, Balaban E, Karabağ M. Is there a relationship between third-molar impaction types and the dimensional/angular measurement values of posterior mandible according to Pell & Gregory/Winter classification? Oral Radiol. 2021;37(1):29–35.
Luo Q, Diao W, Luo L, Zhang Y. Comparisons of the Computed Tomographic scan and panoramic radiography before mandibular third molar extraction surgery. Med Sci Monit. 2018;24:3340–7.
Saha N, Kedarnath N, Singh M. Orthopantomography and Cone-Beam Computed Tomography for the relation of Inferior Alveolar nerve to the impacted Mandibular Third molars. Ann Maxillofac Surg. 2019;9(1):4–9.
Antonelli A, Barone S, Bennardo F, Giudice A. Three-dimensional facial swelling evaluation of pre-operative single-dose of prednisone in third molar surgery: a split-mouth randomized controlled trial. BMC Oral Health. 2023;23(1):1–15.
Rizqiawan A, Lesmaya YD, Rasyida AZ, Amir MS, Ono S, Kamadjaja DB. Postoperative complications of impacted mandibular third molar extraction related to Patient’s Age and Surgical Difficulty Level: a cross-sectional retrospective study. Int J Dent. 2022;2022:7239339.
Guillaumet-Claure MA, Juiz-Camps AM, Gay-Escoda C. Prevalence of intraoperative and postoperative iatrogenic mandibular fractures after lower third molar extraction: a systematic review. J Clin Exp Dent. 2022;14(1):e85–94.
Choi E, Lee S, Jeong E, Shin S, Park H, Youm S, et al. Artificial intelligence in positioning between mandibular third molar and inferior alveolar nerve on panoramic radiography. Sci Rep. 2022;12(1):2456.
Xu GZ, Yang C, Fan XD, Yu CQ, Cai XY, Wang Y, et al. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br J Oral Maxillofac Surg. 2013;51(8):e215–9.
Saraydar-Baser R, Dehghani-Tafti M, Navab-Azam A, Ezoddini-Ardakani F, Nayer S, Safi Y, et al. Comparison of the diagnostic value of CBCT and Digital Panoramic Radiography with surgical findings to determine the proximity of an impacted third mandibular molar to the inferior alveolar nerve canal. J Med Life. 2015;8:83–9.
Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;63(1):3–7.
Elkhateeb SM, Awad SS. Accuracy of panoramic radiographic predictor signs in the assessment of proximity of impacted third molars with the mandibular canal. J Taibah Univ Med Sci. 2018;13(3):254–61.
Ghaeminia H, Gerlach NL, Hoppenreijs TJM, Kicken M, Dings JP, Borstlap WA, et al. Clinical relevance of cone beam computed tomography in mandibular third molar removal: a multicentre, randomised, controlled trial. J Craniomaxillofac Surg. 2015;43(10):2158–67.
Zhu T, Chen D, Wu F, Zhu F, Zhu H. Artificial Intelligence Model to detect real contact relationship between Mandibular Third molars and Inferior alveolar nerve based on panoramic radiographs. Diagnostics (Basel). 2021;11(9):1664.
Matzen LH, Wenzel A. Efficacy of CBCT for assessment of impacted mandibular third molars: a review - based on a hierarchical model of evidence. Dentomaxillofac Radiol. 2015;44(1):20140189.
Matzen LH, Petersen LB, Wenzel A. Radiographic methods used before removal of mandibular third molars among randomly selected general dental clinics. Dentomaxillofac Radiol. 2016;45(4):20150226.
Issrani R, Prabhu N, Sghaireen M, Alshubrmi HR, Alanazi AM, Alkhalaf ZA, et al. Comparison of Digital OPG and CBCT in Assessment of Risk factors Associated with Inferior nerve Injury during Mandibular Third Molar surgery. Diagnostics (Basel). 2021;11(12):2282.
Rood JP, Nooraldeen Shehab BAA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28(1):20–5.
White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation, 7th Edition, Elsevier, Health Sciences Division, Amsterdam, 2014.
Damstra J, Fourie Z, Ren Y. Evaluation and comparison of postero-anterior cephalograms and cone-beam computed tomography images for the detection of mandibular asymmetry. Eur J Orthod. 2013;35(1):45–50.
Razumova S, Brago A, Howijieh A, Barakat H, Kozlova Y, Razumov N. Evaluation the relationship between Mandibular Molar Root Apices and Mandibular Canal among residents of the Moscow Population using Cone-Beam computed tomography technique. Contemp Clin Dent. 2022;13(1):3–8.
Winter GB. Principles of exodontia as applied to the impacted third molar. St.Louis: American Medical Books; 1926.
Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Bergé SJ. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg. 2009;38(9):964–71.
Cohen J. A coefficient of Agreement for Nominal scales. Educ Psychol Meas. 1960;20(1):37–46.
Santos KK, Lages FS, Maciel CAB, Glória JCR, Douglas-de-Oliveira DW. Prevalence of Mandibular Third molars according to the Pell & Gregory and Winter classifications. J Maxillofac Oral Surg. 2022;21(2):627–33.
Waseem N, Asim MA, Maqsood A, Ghafoor MW, Mirza NUA, Khalid MO. Evaluatıon of patterns of impacted Thırd molars and Theır Assocıatıon Wıth Vıtal structures by Radıographıc Examınatıon. Pakistan Armed Forces Med J. 2021;71(1):255–60.
Chen Y, Liu J, Pei J, Liu Y, Pan J. The risk factors that can increase possibility of Mandibular Canal Wall damage in Adult: A Cone-Beam Computed Tomography (CBCT) study in a Chinese Population. Med Sci Monit. 2018;24:26–36.
Bataineh AB, Albashaireh ZS, Hazza’a AM. The surgical removal of mandibular third molars: a study in decision making. Quintessence Int. 2002;33:613–7.
Nunes WJP, Vieira AL, Guimarães LD, de Alcântara A, de Verner CEP, de Carvalho FS. Reliability of panoramic radiography in predicting proximity of third molars to the mandibular canal: a comparison using cone-beam computed tomography. Imaging Sci Dent. 2021;51(1):1–8.
Del Lhano NC, Ribeiro RA, Martins CC, Picorelli Assis NMS, Devito KL. Panoramic versus CBCT used to reduce inferior alveolar nerve paresthesia after third molar extractions: a systematic review and meta-analysis. Dentomaxillofac Radiol. 2020;49(4):20190265.
Tassoker M. Diversion of the mandibular canal: is it the best predictor of inferior alveolar nerve damage during mandibular third molar surgery on panoramic radiographs? Imaging Sci Dent. 2019;49(3):213–8.
Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(2):253–9.
Bell GW, Rodgers JM, Grime RJ, Edwards KL, Hahn MR, Dorman ML, et al. The accuracy of dental panoramic tomographs in determining the root morphology of mandibular third molar teeth before surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(1):119–25.
Gomes ACA, do Egito Vasconcelos BC, de Oliveira Silva ED, de França Caldas A, Neto ICP. Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J Oral Maxillofac Surg. 2008;66(2):256–9.
Pell GJ, Gregory BT. Impacted mandibular third molars, classification and modified technique for removal. Dent Dig. 1933;39:330–8.
Cheung LK, Leung YY, Chow LK, Wong MCM, Chan EKK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010;39(4):320–6.
Flygare L, Öhman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig. 2008;12(4):291–302.
Horner K, Panel SGD. Cone Beam CT for Dental and Maxillofacial Radiology (evidence based guidelines). Vol. Radiation. European Commission, Directorate-General for Energy X11; 2012.
Korkmaz YT, Kayıpmaz S, Senel FC, Atasoy KT, Gumrukcu Z. Does additional cone beam computed tomography decrease the risk of inferior alveolar nerve injury in high-risk cases undergoing third molar surgery?Does CBCT decrease the risk of IAN injury? Int J Oral Maxillofac Surg. 2017;46(5):628–35.
Ghai S, Choudhury S. Role of panoramic imaging and Cone Beam CT for Assessment of Inferior alveolar nerve exposure and subsequent paresthesia following removal of impacted Mandibular Third Molar. J Maxillofac Oral Surg. 2018;17(2):242–7.
Loureiro RM, Sumi DV, Tames HLVC, Ribeiro SPP, Soares CR, Gomes RLE, et al. Cross-sectional imaging of third molar-related abnormalities. AJNR Am J Neuroradiol. 2020;41(11):1966–74.
Barone S, Antonelli A, Bocchino T, Cevidanes L, Michelotti A, Giudice A. Managing Mandibular Second Molar Impaction: a systematic review and Meta-analysis. J Oral Maxillofac Surg. 2023;81(11):1403–21.
Vasegh Z, Bakhshaei P, Jahanbani M, Mahmoudi Anzabi R. Evaluation of anatomical relationships in the mandibular third molar region based on its angulation and depth of impaction: a CBCT-based study. Oral Maxillofac Surg. 2023.
Hol C, Hellén-Halme K, Torgersen G, Nilsson M, Moystad A. How do dentists use CBCT in dental clinics? A Norwegian nationwide survey. Acta Odontol Scand. 2015;73(3):195–201.
Petersen LB, Olsen KR, Christensen J, Wenzel A. Image and surgery-related costs comparing cone beam CT and panoramic imaging before removal of impacted mandibular third molars. Dentomaxillofac Radiol. 2014;43(6):20140001.
Gökçe G, Akan B, Veli İ. A postero-anterior cephalometric evaluation of different rapid maxillary expansion appliances. J World Fed Orthod. 2021;10(3):112–8.
Sicurezza E, Greco M, Giordano D, Maiorana F, Leonardi R. Accuracy of landmark identification on postero-anterior cephalograms. Prog Orthod. 2012;13(2):132–40.
Tai B, Goonewardene MS, uresh, Murray K, Koong B, Islam SM, ohammed S. The reliability of using postero-anterior cephalometry and cone-beam CT to determine transverse dimensions in clinical practice. Aust Orthod J. 2014;30(2):132–42.
Ulkur F, Ozdemir F, Germec-Cakan D, Kaspar EC. Landmark errors on posteroanterior cephalograms. Am J Orthod Dentofac Orthop. 2016;150(2):324–31.
Major PW, Johnson DE, Hesse KL, Glover KE. Landmark identification error in posterior anterior cephalometrics. Angle Orthod. 1994;64(6):447–54.
Acknowledgements
Not applicable.
Funding
The authors declared that this study has received no financial support.
Author information
Authors and Affiliations
Contributions
Design of Study: BKA. Data Acquisition: BKA, EU. Data Analysis: DI. Writing up: BKA, DI, EU, KO. Submission and Revision: BKA, EU. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with the principles outlined in the Declaration of Helsinki and received ethical approval from the Pamukkale University Non-Interventional Clinical Research Ethics Committee (E-60116787-020-374406). This is a retrospective archive study. However, informed consent is obtained from all patients examined in our clinic.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Apaydın, B.K., Icoz, D., Uzun, E. et al. Investigation of the relationship between the mandibular third molar teeth and the inferior alveolar nerve using posteroanterior radiographs: a pilot study. BMC Oral Health 24, 371 (2024). https://doi.org/10.1186/s12903-024-04123-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04123-x