Abstract
Objective
To assess the maxillofacial growth of patients with isolated cleft palate following the Sommerlad-Furlow modified technique and compare it with the effect of the Sommerlad technique.
Study design
A Retrospective Cohort Study.
Methods
A total of 90 participants, 60 patients with non-syndromic isolated soft and hard cleft palate (ISHCP) underwent primary palatoplasty without relaxing incision (30 patients received the Sommerlad-Furlow modified (S-F) technique and 30 received Sommerlad (S) technique). While the other 30 were healthy noncleft participants with skeletal class I pattern (C group). All participants had lateral cephalometric radiographs at least 5 years old age. All the study variables were measured by using stable landmarks, including 11 linear and 9 angular variants.
Results
The means age at collection of cephalograms were 6.03 ± 0.80 (5–7 yrs) in the S group, 5.96 ± 0.76 (5–7 yrs) in the S-F group, and 5.91 ± 0.87 (5–7 yrs) in the C group. Regarding cranial base, the results showed that there were no statistically significant differences between the three groups in S–N and S–N-Ba. The S group had a significantly shortest S-Ba than the S-F & C groups (P = 0.01), but there was no statistically significant difference between S-F and C groups (P = 0.80). Regarding skeletal maxillary growth, the S group had significantly shorter Co-A, S- PM and significantly less SNA angle than the C group (P = < 0.01). While there was no significant difference between S-F & C groups (P = 0.42). The S group had significantly more MP-SN inclination than the C group (P = < 0.01). Regarding skeletal mandibular growth, there were no statistically significant differences in all linear and angular mandibular measurements between the three groups, except Co-Gn of the S group had a significantly shorter length than the C group (P = 0.05). Regarding intermaxillary relation, the S-F group had no significant differences in Co-Gn—Co-A and ANB as compared with the C group. The S group had significantly less ANB angle than S-F & C groups (P = 0.01 & P = < 0.01). In addition, there were no significant differences in all angular occlusal measurements between the three groups.
Conclusion
As a preliminary report, Sommerlad-Furlow modified technique showed that maxillary positioning in the face tended to be better, and the intermaxillary relationship was more satisfactory than that in Sommerlad technique when compared them in healthy noncleft participants.
Similar content being viewed by others
Introduction
The cleft palate is the most frequent birth abnormality overall and the most common developmental deformity in the craniofacial region [1,2,3]. It has a significant socioeconomic and psychological impact on patients and their families [4, 5]. Palatoplasty has advanced further than just closing the gap to properly functioning reconstruction of the palate with minimal influence on maxillofacial growth in recent years [6]. Although numerous techniques for cleft palate repair have been established, there is no agreement on the ideal palatoplasty technique for all cleft palate types [7,8,9]. The ideal surgical outcomes of a palate repair should include disconnection of the oral and nasal cavities and competent velopharyngeal closing for speech recovery while maintaining the normal potential growth in the relevant region [10]. No general agreement exists on what causes maxillary growth restrictions in cleft palate patients following primary palatoplasty. No scientific evidence correlates growth restriction with any of its putative factors [11,12,13]. Maxillofacial growth was reported to be inhibited following V–Y pushback and von Langenbeck approaches [14, 15], and the disruption of potential growth is mostly attributed to the denuded bone as resulting of relaxing incisions left for secondary intent healing [7, 16,17,18,19] Numerous animal studies have shown that denudating the palatal bone by the relaxing incision impairs maxillary growth. Techniques without relaxing incisions have less potential to affect maxillary growth adversely when compared with other techniques with relaxing incisions [20,21,22,23]. Maxillary dysgenesis is thought to be influenced by scar tissue that forms in the denuded bone region following palate formation. Recent palatoplasty techniques have been developed to limit the impact of this scarring by minimizing the denuded bone [24]. Therefore, there has been a tendency toward emphasizing palatoplasty techniques that avoid relaxing incisions on the hard palate in a functional cleft palate repair [25, 26]. But, considering that there is no relaxing incision, the number of approaches for wide cleft repair will probably be limited. While Sommerlad palatoplasty can improve the function of the palate, there is some debate over its effect on maxillofacial growth.
To expand the surgical indication for palatoplasty without relaxing incision to include wider clefts, we at West China Hospital of Stomatology developed a novel palatoplasty technique called the Sommerlad-Furlow modified palatoplasty (S-F) technique, which involves the most advantageous features of the Sommerlad technique (radicle muscular dissection) and the Furlow technique (Z- plasty). Recently, we explored the incidence of postoperative complications following the S.F technique, including oronasal fistula, velopharyngeal insufficiency, and inadequate quality of life [6, 8, 9, 27]. Meanwhile, the influence of the S-F technique on maxillofacial growth remains unknown [6, 8, 27]. Thus, the current study is the first long-term study that aimed to assess the maxillofacial growth of patient with isolated cleft palate following the S-F technique and compare it with the effect of Sommerlad technique.
Materials and methods
Subjects
A retrospective study was conducted on 90 participants, 60 patients with non-syndromic isolated soft and hard cleft palate (ISHCP) who underwent primary palatoplasty without relaxing incision (30 patients received S-F technique and 30 received S technique). While the other 30 were normal participants with skeletal class I pattern.
Two highly experienced cleft surgeons trained by the same surgeon (Shi Bing) performed all cleft palate repairs. They all worked as a team at the same centre, the West China Stomatology Hospital Sichuan University, from 2011 to 2021. Patients were selected based on the subsequent inclusion criteria; Han Chinese patients with nonsyndromic ISHCP who underwent primary palatoplasty by either S-F technique or S technique without relaxing incision within 1–1.6 years old, patients who had lateral cephalometric imaging at least five years following a palatoplasty [5, 28, 29], patients who had not undergone any other surgery besides palatoplasty as Cheiloplasty, Rhinoplasty or, preoperative or postoperative orthodontic treatment, no history of other types of congenital malformation. However, patients with relaxing incisions on the hard palate and secondary palate repair were excluded. The study protocol was reviewed and approved by the Research Subject Review Board and Ethical Scientific Board of Sichuan University (No. WCHS-CRSE-2023–113-R2-P). As well as, it has been conducted by the guidelines of the Declaration of Helsinki. Each of their parents had given informed consent. The control (C) group was matched with both study (S-F & S) groups in number, age, and gender (Table 1).
Sample size calculation
The G*power 3.0.10 software was used to calculate the sample size. An effect size of 0.39 was obtained from a previous study [28] for the outcome of S–N between three groups after palatoplasty. The power of the study was set at 0.85, and the alpha error (p-value) was set at 0.05. In addition, it was conducted based on previous comparable studies [5, 30, 31].
Surgical technique
The present S.F. technique was invented based on the principles of both Sommerlad and Furlow techniques. The S–F technique's surgical procedures are summarized as follows (Fig. 1): an incision was made along the edge of the cleft to separate the oral and nasal mucosa (Fig. 1A), then adequate elevation of the oral mucoperiosteal flaps on the hard palate and to release of the greater palatine neurovascular pedicles, making a nasopharyngeal incision on the medial pterygoid plate using an electrotome (Fig. 1B), and the nasal mucoperiosteum was peeled off from the medial pterygoid plate toward the base of the skull and also anteriorly from the palatine bone, the nasal mucosa of the left side underwent radical muscular dissection (Fig. 1C). After suturing the nasal layer of the hard palate, Z-plasty flaps on the nasal layer of the soft palate were designed (Fig. 1C). Complete suturing of the nasal layer of the soft palate, then suturing of the dissected palatal muscular flap to the right myomucosal flap (Fig. 1D), lastly, suturing the oral layer without relaxing the incisions (Fig. 1E).
The surgical procedures of palatoplasty using the Sommerlad-Furlow modified technique. A an incision was made along the edge of the cleft to separate the oral mucosa layer and nasal mucosa layer. B A considerable amount of hard palate mucoperiosteal flap elevation and release of greater palatine neurovascular pedicles, nasopharyngeal incision is made on the medial pterygoid plate using an electrotome. C The nasal mucoperiosteum was peeled off anteriorly from the palatine bone and medially from the medial pterygoid plate toward the cranial base and suturing the nasal layer of the hard palate. The nasal musculomucosal layer was subjected to radical muscle dissection. then Z-plasty flaps on the nasal layer of the soft palate were designed. D Complete suturing of the nasal layer of soft palate then suturing the dissected palatal muscle. E The oral layer is sutured without relaxing incisions
The Sommerlad technique is summarized as follows [32]: incising the cleft margin, suturing of the nasal mucosa layer, dissecting and retro-positioning the palatal muscles across the posterior part of the velum, and finally suturing the oral mucosa layer.
Cephalometry
All of the lateral cephalometric radiographs were taken with the same equipment by the same experienced radiologist while the participants were in centric occlusion and a standardized upright position, with the transporionic axis and Frankfort horizontal plane parallel to the surface of the floor [28, 33]. Two well-trained assessors (an oral surgeon, S. Elayah and an orthodontist, W. Al-Gumai) used DOLPHIN Imaging Software (Dolphin Imaging Version 11.95.07.24 Premium, Chatsworth) [34] to trace twice to eliminate measurement errors. All the study variables were measured using stable landmarks, including 12 linear (mm) and 10 angular (°) variants. On each lateral cephalogram, the following landmarks were identified:
Cranial Base; Anterior Cranial Base length, S–N (mm); Posterior Cranial Base length, S-Ba (mm) and Cranial Base Angle, S–N-Ba (°) (Fig. S1).
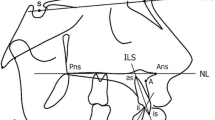
Maxilla; Maxillary Length, Co-A (mm); Anterior Upper Facial Height, N-ANS (mm); Posterior Upper Facial Height, S- PM (mm); Maxillary Sagittal Position, SNA (°) and Maxillary anteroposterior inclination, SN-PP(°) (Fig. S2).
Mandible: Mandibular length, Co-Gn (mm); Corpus (Body) Length, Go-Gn (mm); Ramus Height, Ar-Go (mm); Mandibular sagittal Position, SNB (°); Total Anterior Facial Height, N-Me (mm); Lower Anterior Facial height, ANS-Me(mm); Total Posterior Facial Height, S-Go (mm) and Mandible anteroposterior inclination, MP-SN(°) (Fig. S3).
Intermaxillary relation; Maxillomandibular differences, Co-Gn—Co-A(mm); Sagittal Intermaxillary Relationship, ANB (°); and Palatal-Mandibular Angle, PP-MP (°) (Fig. S4).
Occlusion; Occlusal Plane to SN Plane, OP-SN (°); Occlusal Plane to FH Plane, OP-FH (°) and Occlusal Plane to Mandibular Plane, OP-MP (°) (Fig. S5).
Statistical analysis
Statistical Package for Social Sciences (SPSS) version 27(Chicago, USA) was used to compute descriptive and analytical statistics. Kolmogorov–Smirnov confirmed the data to evaluate the normality distribution. Kruskal Wallis H and Mann–Whitney tests were used to assess differences in craniofacial morphology among the three groups. In addition, the inter-observer reliability of measures was analyzed using the intraclass correlation coefficient test (ICC). For all metrics, ICC tests were more than 0.9, indicating an acceptable level of agreement. P < 0.05 was regarded to be significant.
Results
90 participants, 60 patients with non-syndromic cleft palate underwent surgical repair using the S-F technique (30) and S technique (30) with no significant difference found between them regarding cleft width, cleft type, and age at repair (Table 2). While the other 30 were normal participants with skeletal class I pattern, with no significant difference found among groups regarding gender and age at cephalogram collection. The means age at collection of cephalograms were 6.03 ± 0.80 (5–7) in the S group, 5.96 ± 0.76 (5–7) in the S-F group, and 5.91 ± 0.87 (5–7) in the control group (Table 1). Our comparison of maxillofacial morphology among three groups showed in (Table 3).
Regarding cranial base, the results showed that there were no statistically significant differences between the three groups (S, S-F & C) in S–N (54.7 ± 4.3, 55.4 ± 4.3 & 56.7 ± 4.3 and S–N-Ba; 131.7 ± 5.2, 128.8 ± 6.7 & 129.4 ± 5.3) respectively. The S group had a significantly shortest S-Ba than the S-F & C groups (P = 0.01), but there was no statistically significant difference between S-F and C groups (P = 0.80).
Regarding skeletal maxilla, the S group had significantly shorter Co-A, S- PM and significantly less SNA angle than the C group (P = < 0.01). While there was no significant difference between S-F & C groups (P = 0.42). The S group had significantly more SN-PP inclination than the C group (P = < 0.01), with no significant difference between S-F & C groups (P = 0.09).
Regarding mandibular bone, there were no statistically significant differences in all linear and angular mandibular measurements between the three groups, except Co-Gn of the S group had significantly shorter length than the C group (P = 0.05).
Regarding intermaxillary relation, the S-F group had no significant differences in Co-Gn—Co-A and ANB as compared with the C group. The S group had significantly less ANB angle than S-F & C groups (P = 0.01 & P = < 0.01).
Regarding occlusion, there were no significant differences in all angular occlusal measurements between the three groups.
Discussion
Patients with isolated cleft palate (ICP) should not be included with those with cleft lip and palate (CLP) in scientific studies due to variations in etiology and anatomy. Consequently, scientific studies on patients with clefts should be designed to study subgroups individually [35, 36]. Furthermore, racial factors may play a significant role in cleft palate repair [37], so many studies compare patients with clefts without non-cleft control groups of the same ethnicity [36, 38]. To be more specific and accurate, our study was conducted with patients with the same cleft type ISHCP; participants in three groups were from the same ethnicity.
Our current study assessed the influence of the S-F technique on maxillofacial growth in patients with isolated cleft palate and compared it with the S technique. The anterior cranial base length and angle values in S-F group were closer to C group than the S group without a statistically significant difference. While the S group had significantly shortest posterior cranial base than the S-F & C groups with no statistically significant difference between S-F and C groups. Kulewicz et al. [39] found that the palatoplasty did not significantly affect the growth of the anterior cranial base length. While Liao et al. [40] reported that the stage of palate repair had a significant effect on the means of the length of the posterior cranial base (S-Ba) (p = 0.05). As well as, a systematic review concluded that the posterior cranial base is not totally stable, as its dimensions change throughout craniofacial growth and a minor dimensional change is observed even in late adulthood [41]. Some studies hypothesized that the shorter cranial base length in bilateral cleft lip and palate patients was likely caused by early growth retardation and caught-up growth in adulthood [34].
While comparing the measurements of the maxilla, the S.F technique had slightly affected the maxillary measurements, which are insignificant as compared with the C group, but the maxillary length, posterior upper facial height, angle of maxillary sagittal position, and maxillary anteroposterior inclination were significantly affected by S technique. The minimal incision technique in Karsten’s study [42] resulted in better growth of Maxilla. Compared to the Von Langenbeck technique, the isolated cleft palate repair that uses the Sommerlad technique has the advantages of less damage and less tissue scarring while showing no inhibition on the growth of the maxilla [43]. On the other hand, Shibasaki et al. [44] came to the conclusion that treated isolated cleft palate patients had maxillary underdevelopment but with adequate facial balance as a result of positional alterations of the mandible. Recently, Vitali Azouz et al. [45] concluded that there was a low incidence of maxillary hypoplasia after isolated cleft palate repair.
Regarding the mandible, there were no statistically significant differences in all linear and angular mandibular measurements between the three groups except the mandibular length in the S group; it had a significantly shortest length than S.F & C groups. Our results support previous studies, which found that the hard palate repair had no noticeable effect on the mandible's protrusion or the mandibular plane inclination [29, 46, 47]. On the other hand, Shibasaki and Ross [44] reported that the mandible is of normal length but retro-positioned due to the functional response of the mandible to the altered maxilla. This may explain why the S group's mandibular length was shorter than the S-F group.
Regarding the intermaxillary relation, the S-F group had no significant differences in an intermaxillary relationship compared to the C group. The S group had significantly less sagittal intermaxillary angle than S-F & C groups. Some studies [29, 46] reported that the palatoplasty did not significantly affect jaw relation (ANB), whereas another study [39] reported that it did. The influence of the palatoplasty technique has been limited to the transverse development of the maxillary dental arch [48]. Da Silva et al. [49] the intermaxillary relationship was regarded as satisfactory after the primary palatoplasty. On the other hand, more palatal scar tissue from the technique may have a more significant effect on the teeth and the alveolar process than on maxillary growth [29]. Similarly, Karsten et al. [42] reported that a minimal incision technique resulted in better development of the maxilla with better dental occlusion than the Veau–Wardill–Kilner technique, which is claimed to produce relatively large areas of denuded palatal bone.
Scarred palatal mucosa may partially resist further growth if there is tissue undermining and hamulus fracture in the area of the pterygopalatomaxillary junction during the palatal repair.
Overall, the current favorable outcomes observed in both primary palatoplasty techniques may be clarified through the conclusion of two systematic review studies; it is widely accepted that cleft lip repair could have a negative effect on maxillofacial growth; therefore, lip closure is the most important factor in restricting of maxillary growth in patients with UCLP [50, 51]. However, tension from upper lip closure causes retro-inclined upper incisors, a retruded maxilla, and an obtuse nasolabial angle [52]. Typically, this results in an anterior crossbite [53].
The favorable outcomes observed in the S-F technique may be attributed to the three concepts that the S-F technique designed to close the cleft palate under palatal muscle reconstruction using Sommerlad muscle dissection, decreasing the pharyngeal cavity by nasal Z-plasty and a novel incision on the medial pterygoid plate's surface which was designed to make the S-F technique applicable in wider clefts without relaxing incision on the hard palate [27]. In contrast, the Sommerlad technique does not use of Z-plasty flaps, which may result in tension and growth limitation.
The outcomes associated with this study may have been impacted by its limitations. The groups were assessed before puberty. Another limitation was that the enrolled patients were not from a single surgeon. However, both surgeons in the present study had more than 12 years of experience and worked in almost one team. Further studies with large size samples after growth complete will be required for better evaluation and understanding of craniofacial morphology of ICP.
Conclusion
As a preliminary report, Sommerlad-Furlow modified technique showed maxillary positioning in the face tended to be better, and the intermaxillary relationship was more satisfactory than that in Sommerlad technique when compared them in healthy noncleft participants. While current study has shed light on the effects of cleft palate repair techniques on the maxillofacial growth before puberty, the dynamic nature of skeletal growth necessitates a more extended observation period.
Availability of data and materials
The datasets used and analyzed during the study are available from the corresponding author upon reasonable request.
References
Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. 2011;12(3):167–78.
Jugessur A, Murray JC. Orofacial clefting: recent insights into a complex trait. Curr Opin Genet Dev. 2005;15(3):270–8.
Eppley BL, van Aalst JA, Robey A, Havlik RJ, Sadove AM. The spectrum of orofacial clefting. Plast Reconstr Surg. 2005;115(7):101e–14e.
Cheng X, Bo Z, Yin H, Yang K, Li J, Shi B. Age and Preoperative Velar Closure Ratio Are Significantly Associated With Surgical Outcome of Furlow Double-Opposing Z-Plasty in Palatal Re-Repair. J Oral Maxillofac Surg. 2020;78(3):431–9.
Xu X, Cao C, Zheng Q, Shi B. The Influence of Four Different Treatment Protocols on Maxillofacial Growth in Patients with Unilateral Complete Cleft Lip, Palate, and Alveolus. Plast Reconstr Surg. 2019;144(1):180–6.
Sakran KA, Yin J, Yang R, Alkebsi K, Elayah SA, Al-Rokhami RK, Holkom MA, Liu Y, Wang Y, Yang C, Shi B, Huang H. Evaluation of late cleft palate repair by a modified technique without relaxing incisions. J Stomatol Oral Maxillofac Surg. 2023;124(4):101403. https://doi.org/10.1016/j.jormas.2023.101403.
Li F, Wang HT, Chen YY, Wu WL, Liu JY, Hao JS, Luo DY. Cleft relapse and oronasal fistula after Furlow palatoplasty in infants with cleft palate: incidence and risk factors. Int J Oral Maxillofac Surg. 2017;46(3):275–80.
Sakran KA, Wu M, Alkebsi K, Mashrah MA, Al-Rokhami RK, Wang Y, Mohamed AA, Elayah SA, Al-Sharani HM, Huang H, Shi B. The Sommerlad-Furlow Modified Palatoplasty Technique: Postoperative Complications and Implicating Factors. Laryngoscope. 2023;133(4):822–9. https://doi.org/10.1002/lary.30385.
Sakran KA, Yin J, Yang R, Elayah SA, Alkebsi K, Zhang S, Wang Y, Shi B, Huang H. Early Cleft Palate Repair by a Modified Technique Without Relaxing Incisions. Cleft Palate Craniofac J. 2022:10556656221135288. https://doi.org/10.1177/10556656221135288.
Shi B, Losee JE. The impact of cleft lip and palate repair on maxillofacial growth. Int J Oral Sci. 2015;7(1):14–7.
Liau JY, Sadove AM, van Aalst JA. An evidence-based approach to cleft palate repair. Plast Reconstr Surg. 2010;126(6):2216–21.
Lee YH, Liao YF. Hard palate-repair technique and facial growth in patients with cleft lip and palate: a systematic review. Br J Oral Maxillofac Surg. 2013;51(8):851–7.
Richard B, Russell J, McMahon S, Pigott R. Results of randomized controlled trial of soft palate first versus hard palate first repair in unilateral complete cleft lip and palate. Cleft Palate Craniofac J. 2006;43(3):329–38.
Campbell A, Costello BJ, Ruiz RL. Cleft lip and palate surgery: an update of clinical outcomes for primary repair. Oral Maxillofac Surg Clin North Am. 2010;22(1):43–58.
Zhang B, Yang C, Yin H, Zheng Q, Shi B, Li J. Preoperative velopharyngeal closure ratio correlates with Furlow palatoplasty outcome among patients with nonsyndromic submucous cleft palate. J Craniomaxillofac Surg. 2020;48(10):962–8.
Bruneel L, Luyten A, Bettens K, D’Haeseleer E, Dhondt C, Hodges A, Galiwango G, Vermeersch H, Van Lierde K. Delayed primary palatal closure in resource-poor countries: Speech results in Ugandan older children and young adults with cleft (lip and) palate. J Commun Disord. 2017;69:1–14.
Parwaz MA, Sharma RK, Parashar A, Nanda V, Biswas G, Makkar S. Width of cleft palate and postoperative palatal fistula–do they correlate? J Plast Reconstr Aesthet Surg. 2009;62(12):1559–63.
Sakran KA, Liu R, Yu T, Al-Rokhami RK, He D. A comparative study of three palatoplasty techniques in wide cleft palates. Int J Oral Maxillofac Surg. 2021;50(2):191–7.
Losee JE, Kirschner RE. 61 Facial Growth and Development in Individuals with Clefts. In: Comprehensive Cleft Care, Volume 2. 2nd Ed edn. Stuttgart: Georg Thieme Verlag KG; 2016. https://doi.org/10.1055/b-0037-142282.
Dong Y, Dong F, Zhang X, Hao F, Shi P, Ren G, Yong P, Guo Y. An effect comparison between Furlow double opposing Z-plasty and two-flap palatoplasty on velopharyngeal closure. Int J Oral Maxillofac Surg. 2012;41(5):604–11.
Leenstra TS, Maltha JC, Kuijpers-Jagtman AM, Spauwen PH. Wound healing in beagle dogs after palatal repair without denudation of bone. Cleft Palate Craniofac J. 1995; 32(5):363–369. discussion 369–370.
Kremenak CR Jr, Huffman WC, Olin WH. Maxillary growth inhibition by mucoperiosteal denudation of palatal shelf bone in non-cleft beagles. Cleft Palate J. 1970;7:817–25.
Leenstra TS, Kuijpers-Jagtman AM, Maltha JC. The healing process of palatal tissues after operations with and without denudation of bone: an experimental study in dogs. Scand J Plast Reconstr Surg Hand Surg. 1999;33(2):169–76.
Yoshida H, Takahashi M, Yamaguchi T, Takizawa H, Takakaze M, Maki K. Comparison of Maxillofacial Morphology Between Modified Furlow's and Modified two-Flap Palatoplasty in Orofacial Clefts During the Primary Dentition Period. Cleft Palate Craniofac J. 2023;60(10):1313–20. https://doi.org/10.1177/10556656221104374.
Luyten A, Bettens K, D’Haeseleer E, De Ley S, Hodges A, Galiwango G, Bonte K, Vermeersch H, Van Lierde K. The impact of palatal repair before and after 6 months of age on speech characteristics. Int J Pediatr Otorhinolaryngol. 2014;78(5):787–98.
Barutca SA, Aksan T, Usçetin I, Sahin D, Akan M. Effects of palatine bone denudation repair with periosteal graft on maxillary growth: an experimental study in rats. J Craniomaxillofac Surg. 2014;42(1):e1–7.
Sakran KA, Wu M, Yin H, Wang Y, Li C, Alkebsi K, Telha WA, Zheng Q, Huang H, Shi B. Evaluation of Postoperative Outcomes in Two Cleft Palate Repair Techniques without Relaxing Incisions. Plast Reconstr Surg. 2023;152(1):145–54. https://doi.org/10.1097/PRS.0000000000010230.
Xu X, Kwon HJ, Shi B, Zheng Q, Yin H, Li C. Influence of different palate repair protocols on facial growth in unilateral complete cleft lip and palate. J Craniomaxillofac Surg. 2015;43(1):43–7.
Fudalej PS, Katsaros C, Dudkiewicz Z, Bergé SJ, Kuijpers-Jagtman AM. Cephalometric outcome of two types of palatoplasty in complete unilateral cleft lip and palate. Br J Oral Maxillofac Surg. 2013;51(2):144–8.
Cho BC, Kim JY, Yang JD, Lee DG, Chung HY, Park JW. Influence of the Furlow palatoplasty for patients with submucous cleft palate on facial growth. J Craniofac Surg. 2004; 15(4):547–554. discussion 555.
Fan X, Liu W, Nie J, Chen X, Dong Y, Lu Y. Comparison of velopharyngeal morphology of two palatoplasty techniques in patients with hard and soft cleft palate. Front Surg. 2022;9:1080955.
Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112(6):1542–8.
Grummons DC, Kappeyne van de Coppello MA. A frontal asymmetry analysis. J Clin Orthod. 1987;21(7):448–65.
Liu Y, Huang H, Shi B, Wang Y. The influence of lip repair on the growth of craniofacial structures in bilateral cleft lip and palate patients with unoperated palate from childhood to adulthood. Journal of Craniofacial Surgery. 2020;31(5):1218–22.
Yoshida H, Nakamura A, Michi K, Wang GM, Liu K, Qiu WL. Cephalometric analysis of maxillofacial morphology in unoperated cleft palate patients. Cleft Palate Craniofac J. 1992;29(5):419–24.
Kato RM, Moura PP, Zechi-Ceide RM, Tonello C, Peixoto AP, Garib D. Comparison Between Treacher Collins Syndrome and Pierre Robin Sequence: A Cephalometric Study. Cleft Palate Craniofac J. 2021;58(1):78–83.
Wu RT, Peck CJ, Shultz BN, Travieso R, Steinbacher DM. Racial Disparities in Cleft Palate Repair. Plast Reconstr Surg. 2019;143(6):1738–45.
Madachi K, Takagi R, Asahito T, Kodama Y, Ominato R, Iida A, Ono K, Saito I. Cephalometric evaluation after two-stage palatoplasty combined with a Hotz plate: a comparative study between the modified Furlow and Widmaier-Perko methods. Int J Oral Maxillofac Surg. 2017;46(5):539–47.
Kulewicz M, Dudkiewicz Z. Craniofacial morphological outcome following treatment with three different surgical protocols for complete unilateral cleft lip and palate: a premilinary study. Int J Oral Maxillofac Surg. 2010;39(2):122–8.
Liao YF, Yang IY, Wang R, Yun C, Huang CS. Two-stage palate repair with delayed hard palate closure is related to favorable maxillary growth in unilateral cleft lip and palate. Plast Reconstr Surg. 2010;125(5):1503–10.
Currie K, Sawchuk D, Saltaji H, Oh H, Flores-Mir C, Lagravere M. Posterior cranial base natural growth and development: A systematic review. Angle Orthod. 2017;87(6):897–910.
Karsten A, Larson M, Larson O. Dental occlusion after Veau-Wardill-Kilner versus minimal incision technique repair of isolated clefts of the hard and soft palate. Cleft Palate Craniofac J. 2003;40(5):504–10.
Lu Y, Shi B, Wang Z, Zhan X. STUDY ON WOUND HEALING AFTER Sommerlad TECHNIQUE REPAIR OF ISOLATED CLEFT PALATE. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(7):869–72.
Shibasaki Y, Ross RB. Facial growth in children with isolated cleft palate. Cleft Palate J. 1969;6:290–302.
Azouz V, Ng M, Patel N, Murthy AS. Low incidence of maxillary hypoplasia in isolated cleft palate. Maxillofac Plast Reconstr Surg. 2020;42(1):8.
Silva Filho OG, Calvano F, Assunção AG, Cavassan AO. Craniofacial morphology in children with complete unilateral cleft lip and palate: a comparison of two surgical protocols. Angle Orthod. 2001;71(4):274–84.
Johnston CD, Leonard AG, Burden DJ, McSherry PF. A comparison of craniofacial form in Northern Irish children with unilateral cleft lip and palate treated with different primary surgical techniques. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 2004;41(1):42–6.
Bishara SE, Enemark H, Tharp RF. Cephalometric comparisons of the results of the Wardill-Kilner and Von Langenbeck palatoplasties. Cleft Palate J. 1976;13:319–29.
da Silva Filho OG, Rosa LA, Lauris Rde C. Influence of isolated cleft palate and palatoplasty on the face. J Appl Oral Sci. 2007;15(3):199–208.
Corthouts P, Boels F, Van de Casteele E, Nadjmi N. Effects of various surgical protocols on maxillofacial growth in patients with unilateral cleft lip and palate: a systematic review. Plastic and Aesthetic Research. 2020;7:46.
Bichara LM, Araújo RC, Flores-Mir C, Normando D. Impact of primary palatoplasty on the maxillomandibular sagittal relationship in patients with unilateral cleft lip and palate: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2015;44(1):50–6.
Ebin LE, Zam NM, Othman SA. Cephalometric analysis of Malay children with and without unilateral cleft lip and palate. Aust Orthod J. 2010;26(2):165–70.
Farronato G, Kairyte L, Giannini L, Galbiati G, Maspero C. How various surgical protocols of the unilateral cleft lip and palate influence the facial growth and possible orthodontic problems? Which is the best timing of lip, palate and alveolus repair? literature review. Stomatologija. 2014;16(2):53–60.
Acknowledgements
The authors would like to thank Dr. Essam Ahmed Al-Moraissi for his consultation and assistance in accomplishing this study.
Funding
This work was supported by the National Natural Science Foundation of China grant to B. Shi (81974147).
Author information
Authors and Affiliations
Contributions
S.A.E, J.Y and W.S.A contributed to data collection, interpretation of data, designing the study and writing the original manuscript. H.Y. prepared figures. All other authors have critically revised the manuscript and approved the final one before its submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Ethical Scientific Board and Research Subject Review Board of Sichuan University (No. WCHS-CRSE-2023–113-R2-P). and has been conducted by the guidelines of the Declaration of Helsinki. Each of their parents had given informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. Cranial Base measurements; Anterior cranial base length (S-N, Sella-Nasion); Posterior cranial base length (S-Ba, Sella- Basion); Cranial base angle (S-N-Ba, Sella-Nasion-Basion angle). Figure S2. Maxilla measurements; Maxillary Length (Co-A, condylion - A point); Anterior Upper Facial Height (N-ANS, Nasion- anterior nasal spine); Posterior Upper Facial Height (S- PNS, Sella - posterior nasal spine); Sagittal Maxillary Position (SNA, Sella-Nasion- A point angle), and Maxillary Anteroposterior Inclination (SN-PP, Sella-Nasion line- palatal plane angle). Figure S3. Mandible measurements; Mandibular Length (Co-Gn, condylion- Gnathion); Corpus (Body) Length (Go-Gn, gonion -Gnathion); Ramus Height (Ar-Go, articular- gonion); Mandibular sagittal Position (SNB, Sella-Nasion- B point angle); Total Anterior Facial Height (N-Me, Nasion- mention); Lower Anterior Facial Height (ANS-Me, anterior nasal spine -mention), Posterior Total Facial Height (S-Go, Sella- gonion) and Mandibular Anteroposterior Inclination (MP – SN, mandibular plane- Sella Nasion line angle). Figure S4. Intermaxillary relation measurements; Maxillo-mandibular differences (Co-Gn - Co-A, condylion- Gnathion- condylion - articular); Sagittal intermaxillary relationship (ANB, A point -Nasion - B point angle) and Palatal plane - mandibular plane (PP-MP,) angle. Figure S5. Occlusion measurements; Occlusal plane to anterior cranial base angle (OP-SN, Occlusal plane- Sella Nasion line angle); Occlusal Plane to Frankfort horizontal plane angle (OP-FH) angle, and Occlusal plane to mandibular plane (OP-MP) angle.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elayah, S.A., Yin, J., Al-Gumaei, W.S. et al. A comparison of maxillofacial growth in Chinese children with isolated cleft palate treated with two different palatoplasty techniques without relaxing incisions: a preliminary study. BMC Oral Health 23, 914 (2023). https://doi.org/10.1186/s12903-023-03588-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03588-6