Abstract
Objective
The aim of this review is to evaluate the different medicinal interventions available for the management of oral submucous fibrosis (OSF).
Materials and methods
We conducted a comprehensive electronic search on PubMed, Web of Science, and Cochrane Library databases for articles related to OSF patients treated with medications from December 2011 to September 2022. GRADE system was used to evaluate the evidence quality. The reporting of the systematic review is in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol. The main outcomes were the improvement of maximum mouth opening, burning sensation, cheek flexibility, and tongue protrusion.
Results
Twenty-nine randomized controlled trials (RCTs), five clinical trials (CCTs) were included, and the use of drugs for OSF treatment were evaluated. Drugs like steroids, hyaluronidase, pentoxifylline, lycopene, curcumin, dpirulina, aloe vera, omega3, oxitard, allicin, colchicine have been used. It was found that drugs with evidence high quality were salvia miltiorrhiza combined with triamcinolone acetonide, lycopene, pentoxifylline, curcumin, and aloe vera, and those with evidence moderate quality were allicin, colchicine, omega 3, and oxitard.
Conclusion
Based on the results of our comprehensive analysis, for long-term treatment, we found lycopene with low side effects, whereas for relieving the symptoms of severe burning sensation, aloe vera is the most effective. Although the recent review has made some progress, drug therapy for OSF remains unclear, and more high-quality RCTs are needed to identify better treatments for OSF.
Similar content being viewed by others
Introduction
Oral submucous fibrosis (OSF) is an insidious and chronic oral mucosal disease. It is a potentially malignant disorder of the oral mucosa with a malignant transformation rate of 4.2% [1]. The initial manifestation of OSF is inflammation, followed by loss of blood vessels and fibrosis visible, and blanching of the oral mucosa with a marble-like appearance [2]. The late stage of this disease shows dense fibrosis extending into the underlying muscles, fibrous bands in the buccal mucosa, lip, or palate leading to progressive restriction of maximum mouth opening (MMO), which can further cause problems with oral hygiene, speaking, and chewing [3, 4].
The etiology of OSF has not yet been fully elucidated but may be related to betel nut chewing, capsaicin, autoimmunity, allergies, genetic predisposition, and chronic vitamin and micronutrient deficiencies [5, 6]. The current mainstream view is that betel nut chewing is closely associated with the occurrence of OSF [7, 8]. Excessive use of betel nut, collagen synthesis increases and collagen degradation decreases, increased collagen cross-linking, and insufficient collagen phagocytosis and fibrokine action [9], this eventually leads to OSF. Moreover, the long-term use of betel nut can induce the production of free radicals and reactive oxygen species, leading to a high rate of oxidation/peroxidation of unsaturated fatty acids, which affects the essential components of cell membranes [10]. The study showed that the composition of betel nut products, the frequency and duration of betel nut consumption may all affect the malignant transformation rate of the disease [11] Currently, the treatment of OSF mainly includes physical therapy, hyperbaric oxygen therapy, drug therapy, and surgical treatment [12]. Drug therapy is the most common treatment, and available drug treatments include steroids, exogenous enzymes, multivitamins and micronutrients, peripheral vasodilators, human placental extracts, and other therapeutic agents. Although various treatments have been proposed for OSF over the past few decades, satisfactory results have not been achieved with most methods.
In 2012, Chole et al. [13] reviewed the literature on drug treatment for OSF to identify the role of various drugs in the treatment of OSF. In 2020, More et al. [14] summarized the clinical studies of OSF drugs in the past decade according to the mechanism of action of different drugs and targeted pathways, and discussed other potential drugs. With the emergence of new drugs for the treatment of OSF, we summarize the available pharmacological interventions for the treatment of OSF, describe the efficacy of contemporary and newly developed treatment modalities attempts to provide reference strategies for future research. Therefore, in this review, we collected relevant studies conducted in the past 10 years from 2012 to the present to systematically identify published randomized controlled trials (RCTs), clinical trials (CCTs) on various drugs for the treatment of OSF since December 2011 and update the literature with new clinical studies.
Materials and methods
This systematic review is in accordance with the PRISMA protocols and the protocol was registered in PROSPERO with the code CRD42023429093. The PICO (Population, Intervention, Comparison, Outcome) framework was used to guide the eligibility criteria of this review. P = Patients with OSF I = Any drugs with the aim to treat OSF, C = Other drug or placebo for OSF, O = improving symptoms of OSF, such as MMO, burning sensation (BS), cheek flexibility (CF), tongue protrusion (TP).
Search strategy
Detailed literature searches of PubMed, Web of Science, and Cochrane Library from December 2011 to September 2022 were conducted. In addition, we performed a manual search for other references in published reviews. The search strategy was based on the recommendations of the Oxford Centre for Evidence-Based Medicine and performed using subject headings, free-text terms for OSF, and relevant interventions to identify relevant RCTs, clinical trials, and meta-analyses. The detailed search strategy was (((“Oral Submucous Fibrosis“[Mesh]) OR ((submucous fibrosis) OR (submucous fibroses))) AND ((“randomized controlled trial*” OR “randomised controlled trial*” OR “randomized” OR “controlled trial”) OR (clinical trials))) AND ((“Drug Therapy“[Mesh]) OR (treatment) OR (therapy*) OR (management))
Screening and data extraction
Articles were independently screened and extracted by two authors (X. C. and H. X.). The included studies were identified from the databases and other sources according to the previously search strategy. Other sources were references of included studies identified from databases. The screening contents included: first, a rapid title screening was performed on all the retrieved studies and irrelevant studies were excluded. Second, detailed abstracts were screened according to the defined inclusion criteria of all relevant articles. Finally, the full texts of the included studies that met the criteria were read in detail. Any disagreements between the two independent screeners were resolved by discussion and referral with another more senior and experienced member of the review team (J. G.).
Inclusion criteria
1)Type of study: RCT, CCT were included; 2) Subjects: patients diagnosed with OSF according to pathological diagnosis or clinical manifestations, regardless of gender and race; 3) Intervention: the experimental group was treated with drugs; 4) The study was conducted from December 2011 to September 2022; 5) Studies were reported in English only.
Exclusion criteria
(1) incomplete data (2) full text not available (3) Studies with unclear evaluation criteria; (4) Cannot be obtained Bureau index data, literature with incomplete data and wrong data.
Quality assessment
In this review, quality was assessed independently and in duplicate by two independent reviewers using a standardized critical appraisal method for quality evaluation. The quality of RCTs was assessed using the Cochrane Risk of Bias tool, and CCTs were assessed using the tool of ROBINS. Overall, a study was judged to have a high risk of bias if at least one domain of bias was judged to be high risk. The quality of the findings generated by our review was classified as high, moderate, low, or very low in accordance with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system [15]. It was judged by two authors (X. C. and H. X.) and checked by another author (J. G.).
Data assessment
The data synthesis results were organized and summarized in tabular form, and the effectiveness of different drugs in the treatment of OSF were evaluated. The evaluation of BS, MMO, CF and TP were included.
Results
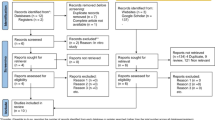
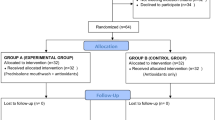
Figure 1 shows the process of the literature search. The database search yielded a total of 270 studies, and the manual search yielded 9 studies. After eliminating duplicate studies, 117 studies were selected for further title and abstract screening. After screening, 68 studies were excluded as they did not meet the inclusion criteria. The remaining 49 studies were selected for full-text screening, and among the 49 studies, 34 met the criteria and were accepted. These 34 studies included 29 RCTs, 5 CCTs, a total of 2136 patients were included in the study. Four studies reported the use of steroids, it mainly includes medium-acting (triamcinolone acetonide) and long-acting (dexamethasone and betamethasone) steroid. Three reported the use of hyaluronidase. Four studies reported the use of peripheral vasodilators, including isoxsuprine and pentoxifylline. The use of antioxidants was also found to be very common: three studies reported the use of spirulina, seven studies reported the use of curcumin, and six studies reported the use of lycopene, these antioxidants were mainly used as capsules, tablets, and gels. One study used salvianolic acid B, a substance extracted from salvianolic miltiorrhiza, which is a common hemorheological agent and has the effect of promoting blood circulation and removing blood stasis. In addition, other drugs such as omega 3, allicin, colchicine, and oxitard were used to treat OSF. Oxitard capsules contains the extracts of Mangifera indica, Withania somnifera, Daucus carota, Glycyrrhiza glabra, Vitis vinifera, powders of Emblica officinalis and Yashada bhasma, and oils of Triticum sativum, these components all have anti-inflammatory effects. Table 1 presents the results of all the included studies. The included studies were all published between 2011 and 2022 and mainly reported data from Asia including China and India. The minimum duration of the intervention was 1.5 months and the maximum duration was 10 months. More than 70% of the studies presented outcomes of BS, 94% of the studies presented outcomes of MMO. Other outcomes included CF, TP, ulceration improved, blanching of oral mucosa, fibrotic bands improved, ankyloglossia improved, color of mucosa, VAS with spicy food. The results shows that drugs with evidence high quality were salvia miltiorrhiza injection (SMI) combined with triamcinolone acetonide, lycopene, pentoxifylline, curcumin, and aloe vera, and those with evidence moderate quality were allicin, colchicine, omega 3, and oxitard.
Risk of bias in RCT
An analysis of the risk of bias in RCTs found that two studies [16, 17] were rated as having a high risk of bias due to the open-label approach used during the trial, which influenced both objective and subjective outcomes. The remaining studies included all had moderate risk scores for bias. The parameters that led to bias were: no mention of randomization in detail, lack of assignment hiding and blind procedures, and use of open labels for trials. Only 7 studies [18,19,20,21,22,23,24] mentioned the details of random sequence production, 3 studies [19, 22, 25] used allocation concealment, and only 12 studies [18, 19, 21, 22, 24, 26,27,28,29,30,31,32] used blind methods. The results were shown in Fig. 2.
Risk of bias in CCT
The risk of bias score in 5 CCTs [33,34,35,36,37] was high, which was due to the lack of control for confounding factors, and the bias in measurement and outcome reporting. Considering that the 5 studies did not achieve serious bias and had some reference value, these 5 clinical trials were included in the review for analysis. The results were shown in Fig. 3.
Side-effects
No significant serious side effects were found among the included drugs. In one study, the use of oxitard capsules caused mild abdominal discomfort, and in another study, patients reported mild pain from intralesial injections of dexamethasone [38]. In one study, it was suggested that high-dose isoxsuprine may cause side effects such as facial flushing, high-dose tachycardia, and hypotension, the study used normal dosing, so no related side effects occurred [39]. Mild adverse effects can also occur when curcumin is not used properly, it can cause indigestion, abdominal pain, abdominal distension, dizziness, and other minor adverse reactions. Therefore, more attention should be paid to its adverse reactions to ensure that curcumin is effective and safe for the treatment of OSF.
Discussion
OSF is a chronic disease, and betel nut is the main pathogenic factor. In addition, smoking, nutritional deficiencies, genetic and immune processes are other potential factors. The pathogenesis of OSF and the various interventions that work against different pathogenesis are shown in Fig. 4. The treatment of OSF is difficult, and the current treatment methods are mainly aimed at relieving the signs and symptoms of the disease. Usually, OSF is treated with drugs in the early stages, followed by physical therapy in severe cases and surgery in the late or advanced stages. Many studies have shown that a combination of drugs, including steroids, enzymes, antioxidants, multivitamins, and minerals, can alleviate the signs and symptoms of OSF; however, these studies lacked solid evidence or the sample size was too small to be representative, and related drug therapy trials have been disappointing. Therefore, it is fairly challenging to compare or even combine their effects in a scientifically meaningful manner. Therefore, our article reviewed RCTs and clinical trials for a better assessment of the available evidence.
Steroids
Owing to their immunosuppressive and anti-inflammatory properties, steroids are widely used to treat OSF. In terms of immunosuppression, steroids can activate sensitized lymphocytes against specific antigens to release soluble factors. In terms of their anti-inflammatory effects, steroids can inhibit the proliferation of inflammatory factors and increase the apoptosis of inflammatory cells. Several glucocorticoids, such as short-acting (hydrocortisone), medium-acting (triamcinolone), and long-acting (dexamethasone and betamethasone), have been used for the treatment of OSF [40]. In the early stage, steroids can effectively improve MMO and BS; however, they do not improve the abnormal accumulation of fibrotic tissue [33]. Therefore, steroids alone cannot completely improve the quality of life of patients with OSF. Two studies from Yadav et al. [23] and Anuradha et al. [36] showed that dexamethasone combined with hyaluronic acid was superior to curcumin and aloe vera in improving BS and MMO, respectively. Datarkar et al. [18] showed that prednisolone mouthwash was superior to antioxidant capsules only in improving MMO, but was inferior to antioxidant capsules in relieving BS and ulcers. Systemic corticosteroids are rarely used in the treatment of OSF and usually administered as intrafocal injections or mouthwashes [41]. Overall, steroids can alleviate the signs and symptoms of OSF and can be used in combination with other medications as adjunctive therapy.
Salvia miltiorrhiza
SMI has an excellent antifibrotic activity in vitro. Salvianolic acid B (SA-B) is the important active compound of SMI, it can inhibit collagen accumulation and procollagen gene transcription by targeting the mitogen-activated protein kinase/extracellular signal-regulated kinase pathway, Akt pathway and transforming growth factor /Smad pathway [42]. Jiang et al. [43] compared the efficacy of SA-B combined with triamcinolone acetonide in the treatment of OSF. The SA-B group achieved better improvement in the MMO and BS. A meta-analysis by Guo et al. [44] concluded that in combination with steroids, SMI can effectively improve the subjective symptoms of MMO and BS in patients with OSF and reduce the area of oral mucosal lesions without causing adverse reactions.
Enzymes
Hyaluronidase was originally found in bacteria and widely distributed in nature. It can break down hyaluronic acid (an important component of the extracellular matrix), which reduces the viscosity of intracellular cement and collagen formation. A significant feature of OSF is the massive abnormal deposition of collagen fibers and reduced fibrinolysis [45]. Exogenous enzyme hyaluronidase can target MMP-1 or MMP-2 to destroy abnormal fibrotic tissue, thereby alleviating or curing OSF [46, 47]. Study of Beenakumary et al. showed that hyaluronidase combination with dexamethasone injection was superior to lycopene in improving MMO [41]. Johny et al. [34] showed that LycoRed along with hyaluronidase intralesional injection had 92.8% partial response and 7.2% complete response in improving BS. However, LycoRed alone only achieved a partial response. Hyaluronidase could effectively improve MMO and reduce mucosal tightness, compensating for the lack of effect of steroids in improving the abnormal accumulation of fibrotic tissue; therefore, the two drugs are often used in combination [27]. A meta-analysis by Guo et al. [48] showed that hyaluronidase combined with steroids showed a significantly better effect than placebo in alleviating the BS and improving the MMO in OSF and was as effective as control drugs (such as aloe vera, pentoxifylline, and lycopene).
Peripheral vasodilators
A potential cause of OSF is the progressive loss of diseased mucosal blood vessels, which can lead to epithelial atrophy [49]. Therefore, vasodilators are considered effective for the treatment of OSF. Pentoxifylline (PTX), a trisubstituted methylxanthine derivative, is used as a vasodilator and is effective in the treatment of diseases caused by chronic peripheral arterial occlusion [50]. As mucosal ischemia and the resulting epithelial atrophy may be factors in the pathogenesis of OSF, PTX can be therapeutic owing to its ability to relax and dilate blood vessels, ensuring increased blood supply to the ischemic tissue and enabling nutritional and therapeutic drugs to reach the affected tissue [51]. Isoxsuprine is a phenylalanine derivative of epinephrine and a β-adrenoreceptor agonist that causes an overall increase in the cytosolic calcium concentration, stimulating the production and release of several endothelium-derived vasodilators [52]. In a clinical trial, isoxsuprine plus physical therapy was superior to placebo plus physical therapy in reducing BS, but there was no difference in improving MMO [39]. Sadakshara et al. [28] showed that oral pentoxifylline 400 mg thrice daily was superior to dexamethasone combine with hyaluronidase in improving MMO. Prabhu et al. [53] and Mehrotra et al [29] suggest that oral pentoxifylline was effective in improving BS and fibrotic band. A meta-analysis by Liu et al. [54] showed that PTX is an effective treatment as it can not only increase MMO of patients with OSF but also relieve BS in the mouth. High-dose isoxsuprine may cause facial flushing, high-dose tachycardia, hypotension and other side effects, which can be effectively prevented under normal use doses. Thus, 400 mg twice daily PTX is well tolerated and is expected to become more effective over time.
Antioxidants
One of the pathogenic mechanisms of betel nut is the production of reactive oxygen species, free radicals, and peroxidase to destroy the cellular structure. Based on this hypothesis, several studies have tested various natural or synthetic antioxidants and reported that using them can improve the condition of betel nut damage to the mouth. The mechanism of action of antioxidants is to inhibit ROS production by targeting JAK, MAPK, PI3K and other pathways, and can also inhibit inflammatory response by targeting pro-inflammatory mediators, such as NF-κB, ROS, COX-2, IL-1, IL-2, TGF-β, growth factors, apoptotic proteins, receptors and various kinases [55, 56]. Natural antioxidants include lycopene, aloe vera, curcumin, and spirulina.
Lycopene
Lycopene is a carotenoid found in vegetables and red fruits such as tomatoes, watermelon, and papaya [57]. Lycopene is a carotenoid with strong antioxidant properties because of its high singlet oxygen quenching ability and the ability to quench other free radicals in vitro; it also has antioxidant properties [57]. Many studies have shown that lycopene can prevent and treat diseases, such as oral diseases, heart failure and tumors, through anti-inflammatory, antioxidant and anti-proliferative activities [58,59,60]. Karemore et al [26]. showed that compared with the placebo group, the lycopene group had significantly improved MMO, significantly reduced para-epithelial collagen deposition and chronic inflammatory infiltration after treatment. Saran et al [25]. showed that the lycopene group was superior to the curcumin group in improving MMO. In a study by Piyush et al. [19], lycopene showed superior therapeutic effects in terms of MMO, BS, CF, and TP in 90 patients. In addition, a meta-analysis by Guo et al. [61] showed that lycopene was more effective than placebo in improving the MMO of patients with OSF. Compared with control patients who received drugs such as aloe vera gel, curcumin, spirulina, and betamethasone, patients with OSF showed significantly improved MMO after 1, 2, and 3 months of lycopene treatment, with no significant effect on BS, tongue process, or lesion-related pain. Therefore, lycopene is a promising antioxidant for the treatment of patients with OSF, especially for improving MMO.
Spirulina
Spirulina is a blue-green alga with abundant vitamins (A and B12), minerals, carotenoids, and phycocyanin, it is considered as superfood by the WHO. It imparts the antioxidant effect by increasing IL-2 concentration and decreasing IL-6 concentration [62]. Due to its antioxidant, anti-inflammatory, and immunomodulating properties, spirulina has shown promising results in the management of OSF. Shetty et al. [35] reported that spirulina can effectively improve MMO and BS in patients with OSF. Studies by Mulk et al. [63] showed that spirulina was more effective in improving MMO than pentoxifylline. In a RCT from Patil et al. [64] show that spirulina was superior to aloe vera gel in improving MMO.
Aloe vera
Aloe vera is an ancient plant with a variety of pharmacological effects and has long been used as a medicine to treat many diseases without any reported side effects [65, 66]. Aloe vera is a rich source of vitamins, enzymes, minerals, and sugars, vitamins include antioxidant vitamins A, C, and E, which help neutralize free radicals and act as antioxidants. [62]. Enzymes in aloe vera help reduce inflammation, and polysaccharides promote wound healing and exhibit anti-inflammatory, anticancer, immunomodulatory, and gastric protective properties that explain their role in treating OSF. Nerkar et al. [17] reported that compared with curcumin gel, aloe vera was more effective in improving BS and MMO. Alam et al. [30] showed that the combination of aloe vera after medical or surgical treatment was more effective in improving both BS and TP than either medical or surgical treatment alone. Bohr et al. [31] showed that daily use of aloe vera gel was superior to weekly injections of hydrocortisone acetate and hyaluronidase in improving BS, MMO, TP, and CF. Two other trials from Singh et al. and Sudarshan et al. [32, 67] showed that aloe vera was superior to antioxidant capsules in improving MMO, TP, BS, and CF. A meta-analysis conducted by Al-Maweri et al. [68] showed that compared with other drugs, aloe vera was well tolerated, had few side effects, and was significantly better in reducing BS in the short-term treatment; however, differences in its long-term treatment effects and improvements in MMO, TP, and CF were not significant. Thus, short-term treatment with aloe vera can effectively improve the oral BS in patients with OSF. Therefore, topical application of aloe vera can be a convenient, economical and effective treatment for OSF without any side effects, it is a very safe therapeutic drug.
Curcumin
Curcumin is a polyphenolic compound extracted from the rhizome of curcuma longa and tuber tubers of Zingiberaceae, it is widely used as an antioxidant in many diseases. It interacts with thioredoxin reductase to induce reactive oxygen species (ROS) and inhibit the action of nicotinamide adenine dinucleotide phosphate oxidase, which is responsible for the generation of ROS, thus playing an antioxidant role [69]. In this review, in the study of Chandrashekar et al. [20] Curcumin gel and Curcumin mucoadhesive patch were more effective in improving BS, MMO, TP and CF. In the study by Pipalia et al. [21] curcumin plus black pepper was more effective in improving BS and MMO than nigella sativa. In the study by Rai et al. [22] curcumin tablet (containing curcumin 300 mg and piperine 5 mg) was more effective than ordinary antioxidants in improving BS, MMO and TP. In addition, Lanjekar et al. [70] evaluated the efficacy of curcumin in patients with OSF and found that curcumin showed better improvement in MMO and color of oral mucosa compared with triamcinolone acetonide and hyaluronidase mucoadhesive semisolid gel, better results were obtained when the two drugs were used in combination. Therefore, a combination of curcumin, triamcinolone acetonide, and hyaluronidase is recommended as hyaluronidase facilitates deeper administration of curcumin and triamcinolone acetonide, which have synergistic effects between each other. A meta-analysis by Guo et al. [71] showed that compared with placebo, oral curcumin significantly improved the symptoms of MMO and BS. Compared with lycopene and other drugs, curcumin was less effective in improving MMO after 1 month of treatment, and the improvement of BS after 3 months of treatment was better than that in the control group. Therefore, curcumin can be used as an effective treatment for OSF.
Other drugs
In addition to the abovementioned drugs, allicin, colchicine, omega 3, and oxitard have a certain effect on the treatment of OSF. There is evidence showing that allicin has important anti-inflammatory effects. Studies have shown that TNF-α is associated with the severity of OSF. First, allicin can reduce TNF-α protein and mRNA levels [72]. Second, allicin has antioxidant activity, which can reduce lipid peroxidation and scour hydroxyl radicals [73]. Finally, allicin can increase the expression of vascular endothelial growth factor and angiopoietin and decrease the expression of angiostatin, thereby promoting angiogenesis and accelerating self-repair [74]. Therefore, we attributed the possible therapeutic mechanism of allicin to its anti-inflammatory and antioxidant effects and the angiogenic ability of its breakdown products. One study showed that intralesional injection of allicin (1 mg) for 16 weeks can significantly improve MMO and BS compared with the control group [24]. Colchicine reduces collagen synthesis by disrupting microtubule formation and preventing the extrusion of collagen from fibroblasts [75]. Krishnamoorthy et al. [76] studied the effects of oral administration of 500 mg colchicine and intralesional injection of 0.5 ml hyaluronidase 1,500 IU in the management of OSF and found superior results with colchicine in ameliorating the symptoms of OSF. Omega 3 fatty acids are polyunsaturated essential fatty acids that humans cannot synthesize and must rely on dietary sources. They competitively inhibit the production of arachidonic acid metabolites through the cyclooxygenase and lipoxygenase pathways, thereby limiting tissue damage [77]. Studies have confirmed the inhibitory effect of omega 3 on the secretion of pro-fibrotic TGFβ1 and MMP-9 [78]. It can improve endogenous fibrinolysis and microcirculation by improving vasomotor function. Thus, it enhances vasodilatation and ameliorates the mucosal vessels that are significantly damaged by fibrosis in OSF. In their study, Raizada et al. [79] reported that omega 3 can be used as an adjunctive treatment option in patients with OSF to reduce subjective symptoms, and when combined with dexamethasone and hyaluronidase, omega 3 improved MMO, BS, and CF more effectively. Oxitard capsules are formulated using extracts of mango, morelle, carrot, licorice, grape, triglyceride powder, and wheat oil. These components have the effects of regulating immunity, antiinflammation, convergence and inhibition of BS, antioxidation, and wound healing, as well as certain curative effects on OSF for various reasons [38]. Santosh et al. [38] showed that oxitard capsules significantly improve MMO, TP, BS, pain associated with the lesion, and difficulty in swallowing and speech, with very few side effects.
In a network meta-analysis comparing the efficacy of different treatment interventions for OSF [80], most interventions were found to be superior to placebo in improving clinical symptoms, such as MMO and BS. Oxitard is superior to other interventions in improving MMO, aloe vera is superior in relieving BS, and lycopene has the lowest propensity for side effects and can be considered the best safety agent.
GRADE system was used to evaluate the evidence quality, and it was found that drugs with evidence high quality were SMI combined with triamcinolone acetonide, lycopene, pentoxifylline, curcumin, it is a good choice for the treatment of OSF.
This review had a few limitations, the first of which was the small sample size; only one clinical trial involved more than 150 people. Second, patients could only be verbally advised not to chew betel nuts during the trial. However, there was no effective means to monitor and confirm that all patients have eliminated the harmful habits and thus the results might be biased to some extent.
Conclusion
In conclusion, our findings found that steroids, hyaluronidase, pentoxifylline, antioxidants, omega 3, colicine, and allicin can alleviate the symptoms of OSF, for long-term treatment, lycopene is effective and has few side effects. Aloe vera is the most effective for relieving the symptoms of severe burning. Regardless of the number of treatment options available, abstaining from betel nut chewing is the best strategy to prevent OSF. Our review is intended only as a reference for clinical medication management, we hope that more high-quality meta-analyses, systematic reviews and multicenter RCTs with larger samples will provide more reference suggestions for the treatment of OSF in the future.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Muller S, Tilakaratne WM. Update from the 5th Edition of the World Health Organization classification of Head and Neck Tumors: Tumours of the oral cavity and Mobile Tongue. Head Neck Pathol. 2022;16(1):54–62.
Yang PY, Chen YT, Wang YH, Su NY, Yu HC, Chang YC. Malignant transformation of oral submucous fibrosis in Taiwan: a nationwide population-based retrospective cohort study. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2017;46(10):1040–5.
Rao NR, Villa A, More CB, Jayasinghe RD, Kerr AR, Johnson NW. Oral submucous fibrosis: a contemporary narrative review with a proposed inter-professional approach for an early diagnosis and clinical management. J Otolaryngol Head Neck Surg. 2020;49(1):3.
Sharma SR, Chavan S, Karjodkar FR, Sansare K, Bharathi S, Singh S. Correlation of clinical features in oral Submucous fibrosis: a 9-Year retrospective study. Ethiop J Health Sci. 2022;32(1):137–44.
Arakeri G, Rai KK, Hunasgi S, Merkx MAW, Gao S, Brennan PA. Oral submucous fibrosis: an update on current theories of pathogenesis. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2017;46(6):406–12.
Kumari P, Debta P, Dixit A. Oral potentially malignant Disorders: etiology, pathogenesis, and Transformation into oral Cancer. Front Pharmacol. 2022;13:825266.
Warnakulasuriya S, Chen THH. Areca nut and oral Cancer: evidence from studies conducted in humans. J Dent Res. 2022;101(10):1139–46.
Singh AG, Roy S, Oza S, Singhavi H, Chatterjee K, Chaturvedi P. A contemporary narrative review to guide molecular epidemiology of oral submucous fibrosis. Int J Mol Epidemiol Genet. 2021;12(4):61–70.
Ma RH, Tsai CC, Shieh TY. Increased lysyl oxidase activity in fibroblasts cultured from oral submucous fibrosis associated with betel nut chewing in Taiwan. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 1995;24(9):407–12.
Haque MF, Meghji S, Khitab U, Harris M. Oral submucous fibrosis patients have altered levels of cytokine production. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2000;29(3):123–8.
Murthy V, Mylonas P, Carey B, Yogarajah S, Farnell D, Addison O et al. Malignant Transformation rate of oral Submucous fibrosis: a systematic review and Meta-analysis. J Clin Med 2022, 11(7).
Vedeswari CP, Jayachandran S, Ganesan S. In vivo autofluorescence characteristics of pre- and post-treated oral submucous fibrosis: a pilot study. Indian J Dent Research: Official Publication Indian Soc Dent Res. 2009;20(3):261–7.
Chole RH, Gondivkar SM, Gadbail AR, Balsaraf S, Chaudhary S, Dhore SV, et al. Review of drug treatment of oral submucous fibrosis. Oral Oncol. 2012;48(5):393–8.
More CB, Jatti Patil D, Rao NR. Medicinal management of oral submucous fibrosis in the past decade- A systematic review. J oral Biology Craniofac Res. 2020;10(4):552–68.
Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380–2.
Raizada MK, Sable DM. Clinical Assessment of Efficacy of Omega 3 in oral Submucous Fibrosis Patients - A Randomized Controlled Trial. Asian Pac J cancer Prevention: APJCP. 2022;23(4):1185–92.
Nerkar Rajbhoj A, Kulkarni TM, Shete A, Shete M, Gore R, Sapkal R. A comparative study to evaluate efficacy of Curcumin and Aloe Vera Gel along with oral physiotherapy in the management of oral Submucous fibrosis: a Randomized Clinical Trial. Asian Pac J cancer Prevention: APJCP. 2021;22(S1):107–12.
Datarkar A, Akare A, Tayal S. Efficacy of Prednisolone Mouthwash in Management of Grade III oral Submucous fibrosis: a newer drug Regimen. J Oral Maxillofac Surg. 2020;19(4):532–8.
Piyush P, Mahajan A, Singh K, Ghosh S, Gupta S. Comparison of therapeutic response of lycopene and curcumin in oral submucous fibrosis: a randomized controlled trial. Oral Dis. 2019;25(1):73–9.
Chandrashekar A, Annigeri RG, Va U, Thimmasetty J. A clinicobiochemical evaluation of curcumin as gel and as buccal mucoadhesive patches in the management of oral submucous fibrosis. Oral Surg oral Med oral Pathol oral Radiol. 2021;131(4):428–34.
Pipalia PR, Annigeri RG, Mehta R. Clinicobiochemical evaluation of turmeric with black pepper and nigella sativa in management of oral submucous fibrosis-a double-blind, randomized preliminary study. Oral Surg oral Med oral Pathol oral Radiol. 2016;122(6):705–12.
Rai A, Kaur M, Gombra V, Hasan S, Kumar N. Comparative evaluation of curcumin and antioxidants in the management of oral submucous fibrosis. J Invest Clin Dent. 2019;10(4):e12464.
Yadav M, Aravinda K, Saxena VS, Srinivas K, Ratnakar P, Gupta J, et al. Comparison of curcumin with intralesional steroid injections in oral Submucous Fibrosis - A randomized, open-label interventional study. J oral Biology Craniofac Res. 2014;4(3):169–73.
Jiang X, Zhang Y, Li F, Zhu Y, Chen Y, Yang S, et al. Allicin as a possible adjunctive therapeutic drug for stage II oral submucous fibrosis: a preliminary clinical trial in a chinese cohort. Int J Oral Maxillofac Surg. 2015;44(12):1540–6.
Saran G, Umapathy D, Misra N, Channaiah SG, Singh P, Srivastava S, et al. A comparative study to evaluate the efficacy of lycopene and curcumin in oral submucous fibrosis patients: a randomized clinical trial. Indian J Dent Research: Official Publication Indian Soc Dent Res. 2018;29(3):303–12.
Karemore TV, Motwani M. Evaluation of the effect of newer antioxidant lycopene in the treatment of oral submucous fibrosis. Indian J Dent Research: Official Publication Indian Soc Dent Res. 2012;23(4):524–8.
Alora Veedu R, Balan A, Sankar SP. A randomized double-blind, multiple-arm trial comparing the efficacy of submucosal injections of hyaluronidase, dexamethasone, and combination of dexamethasone and hyaluronidase in the management of oral submucous fibrosis. Oral surgery, oral medicine, oral pathology and oral radiology 2015, 120(5):588–593.e581.
Sadaksharam J, Mahalingam S. Evaluation of oral Pentoxifylline in the management of oral Submucous fibrosis - an Ultrasonographic Study. Contemp Clin Dent. 2017;8(2):200–4.
Mehrotra R, Singh HP, Gupta SC, Singh M, Jain S. Pentoxifylline therapy in the management of oral submucous fibrosis. Asian Pac J cancer Prevention: APJCP. 2011;12(4):971–4.
Alam S, Ali I, Giri KY, Gokkulakrishnan S, Natu SS, Faisal M, et al. Efficacy of aloe vera gel as an adjuvant treatment of oral submucous fibrosis. Oral Surg oral Med oral Pathol oral Radiol. 2013;116(6):717–24.
Bohra A, Maheswari TNU, Harsh A, Garg A. Black Turmeric and Aloe Vera in the management of oral Submucous fibrosis: a prospective clinical study. Asian Pac J cancer Prevention: APJCP. 2021;22(12):3941–7.
Sudarshan R, Annigeri RG, Sree Vijayabala G. Aloe vera in the treatment for oral submucous fibrosis - a preliminary study. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2012;41(10):755–61.
Goel S, Ahmed J. A comparative study on efficacy of different treatment modalities of oral submucous fibrosis evaluated by clinical staging in population of Southern Rajasthan. J Cancer Res Ther. 2015;11(1):113–8.
Johny J, Bhagvandas SC, Mohan SP, Punathil S, Moyin S, Bhaskaran MK. Comparison of efficacy of Lycopene and Lycopene-Hyaluronidase combination in the treatment of oral Submucous Fibrosis. J Pharm Bioallied Sci. 2019;11(Suppl 2):260–S264.
Shetty P, Shenai P, Chatra L, Rao PK. Efficacy of spirulina as an antioxidant adjuvant to corticosteroid injection in management of oral submucous fibrosis. Indian J Dent Research: Official Publication Indian Soc Dent Res. 2013;24(3):347–50.
Anuradha A, Patil B, Asha VR. Evaluation of efficacy of aloe vera in the treatment of oral submucous fibrosis - a clinical study. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2017;46(1):50–5.
James L, Shetty A, Rishi D, Abraham M. Management of oral Submucous fibrosis with injection of hyaluronidase and dexamethasone in Grade III oral Submucous fibrosis: a retrospective study. J Int Oral Health. 2015;7(8):82–5.
Patil S, Santosh BS, Maheshwari S, Deoghare A, Chhugani S, Rajesh PR. Efficacy of oxitard capsules in the treatment of oral submucous fibrosis. J Cancer Res Ther. 2015;11(2):291–4.
Bhadage CJ, Umarji HR, Shah K, Välimaa H. Vasodilator isoxsuprine alleviates symptoms of oral submucous fibrosis. Clin Oral Invest. 2013;17(5):1375–82.
Lai DR, Chen HR, Lin LM, Huang YL, Tsai CC. Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10-year experience with 150 cases. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 1995;24(9):402–6.
Tp B, T AG, Varghese M, Raghavan R, Vm MN, Pius A. Evaluation of therapeutic efficacy of different treatment modalities in oral Submucous fibrosis: a comparative study. J Contemp Dent Pract. 2019;20(3):390–4.
Dai JP, Zhu DX, Sheng JT, Chen XX, Li WZ, Wang GF, et al. Inhibition of Tanshinone IIA, salvianolic acid A and salvianolic acid B on Areca nut extract-induced oral submucous fibrosis in vitro. Molecules. 2015;20(4):6794–807.
Jiang XW, Zhang Y, Yang SK, Zhang H, Lu K, Sun GL. Efficacy of salvianolic acid B combined with triamcinolone acetonide in the treatment of oral submucous fibrosis. Oral Surg oral Med oral Pathol oral Radiol. 2013;115(3):339–44.
Xie H, Guo J, Tan B, Wu H. Efficacy of Salvia miltiorrhiza injection combined with steroids in the treatment of oral submucous fibrosis: a meta-analysis of randomized controlled trials. Medicine. 2019;98(27):e16339.
Yang SF, Hsieh YS, Tsai CH, Chou MY, Chang YC. The upregulation of type I plasminogen activator inhibitor in oral submucous fibrosis. Oral Oncol. 2003;39(4):367–72.
Kakar PK, Puri RK, Venkatachalam VP. Oral submucous fibrosis–treatment with hyalase. J Laryngol Otol. 1985;99(1):57–9.
Ohno-Nakahara M, Honda K, Tanimoto K, Tanaka N, Doi T, Suzuki A, et al. Induction of CD44 and MMP expression by hyaluronidase treatment of articular chondrocytes. J Biochem. 2004;135(5):567–75.
Guo JC, Xie H, Mao S, Liang MN, Wu H. Efficacy of hyaluronidase combined with corticosteroids in treatment of oral submucous fibrosis: a meta-analysis of randomized controlled clinical trials. J Oral Pathol Med. 2020;49(4):311–9.
Kapoor R, Sansare K, Tamgadge S, Karjodkar F, Mehra A, Mishra I, et al. Epithelial atrophy, fibrosis and vascularity correlation with epithelial dysplasia in oral Submucous Fibrosis, a prospective study. J Microsc Ultrastruct. 2022;10(1):1–6.
Maksimovic ZV. [Prostacyclin and pentoxifylline in the treatment of patients with inoperable occlusions of the peripheral arteries of the lower extremities]. Srp Arh Celok Lek. 1999;127(7–8):249–53.
Rajendran R, Rani V, Shaikh S. Pentoxifylline therapy: a new adjunct in the treatment of oral submucous fibrosis. Indian J Dent Research: Official Publication Indian Soc Dent Res. 2006;17(4):190–8.
Erkert RS, Macallister CG. Isoxsuprine hydrochloride in the horse: a review. J Vet Pharmacol Ther. 2002;25(2):81–7.
Prabhu N, Rao SS, Kotrashetti SM, Baliga SD, Hallikerimath SR, Angadi PV, et al. Pentoxifylline in patients with oral submucous fibrosis-a randomized clinical trial. J Oral Maxillofac Surg. 2015;14(1):81–9.
Liu J, Chen F, Wei Z, Qiu M, Li Z, Dan H, et al. Evaluating the efficacy of pentoxifylline in the treatment of oral submucous fibrosis: a meta-analysis. Oral Dis. 2018;24(5):706–16.
Kunnumakkara AB, Bordoloi D, Padmavathi G, Monisha J, Roy NK, Prasad S, et al. Curcumin, the golden nutraceutical: multitargeting for multiple chronic diseases. Br J Pharmacol. 2017;174(11):1325–48.
Monisha J, Padmavathi G, Roy NK, Deka A, Bordoloi D, Anip A, et al. NF-kappaB blockers gifted by Mother Nature: Prospectives in Cancer Cell Chemosensitization. Curr Pharm Des. 2016;22(27):4173–200.
Mozos I, Stoian D, Caraba A, Malainer C, Horbanczuk JO, Atanasov AG. Lycopene and Vascular Health. Front Pharmacol. 2018;9:521.
Chen D, Huang C, Chen Z. A review for the pharmacological effect of lycopene in central nervous system disorders. Biomed Pharmacother. 2019;111:791–801.
Mein JR, Lian F, Wang XD. Biological activity of lycopene metabolites: implications for cancer prevention. Nutr Rev. 2008;66(12):667–83.
Zu K, Mucci L, Rosner BA, Clinton SK, Loda M, Stampfer MJ, et al. Dietary lycopene, angiogenesis, and prostate cancer: a prospective study in the prostate-specific antigen era. J Natl Cancer Inst. 2014;106(2):djt430.
Guo JC, Xie H, Wu H, Liang MN, EFFICACY OF LYCOPENE IN THE TREATMENT OF ORAL SUBMUCOUS FIBROSIS. : A META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS. J Evidence-Based Dent Pract 2020, 20(4).
Miranda MS, Cintra RG, Barros SB, Mancini Filho J. Antioxidant activity of the microalga Spirulina maxima. Braz J Med Biol Res. 1998;31(8):1075–9.
Mulk BS, Deshpande P, Velpula N, Chappidi V, Chintamaneni RL, Goyal S. Spirulina and pentoxyfilline - a novel approach for treatment of oral submucous fibrosis. J Clin Diagn Research: JCDR. 2013;7(12):3048–50.
Patil S, Al-Zarea BK, Maheshwari S, Sahu R. Comparative evaluation of natural antioxidants spirulina and aloe vera for the treatment of oral submucous fibrosis. J oral Biology Craniofac Res. 2015;5(1):11–5.
Ali S, Wahbi W. The efficacy of aloe vera in management of oral lichen planus: a systematic review and meta-analysis. Oral Dis. 2017;23(7):913–8.
Mangaiyarkarasi SP, Manigandan T, Elumalai M, Cholan PK, Kaur RP. Benefits of Aloe vera in dentistry. J Pharm Bioallied Sci. 2015;7(Suppl 1):255–9.
Singh N, Hebbale M, Mhapuskar A, Ul Nisa S, Thopte S, Singh S. Effectiveness of Aloe Vera and antioxidant along with physiotherapy in the management of oral Submucous Fibrosis. J Contemp Dent Pract. 2016;17(1):78–84.
Al-Maweri SA, Ashraf S, Lingam AS, Alqutaibi A, Abdulrab S, Alaizari N, et al. Aloe vera in treatment of oral submucous fibrosis: a systematic review and meta-analysis. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2019;48(2):99–107.
Ahmad T, Khan I, Rizvi MM, Saalim M, Manzoor N, Sultana A. An overview of effect of lycopene and curcumin in oral leukoplakia and oral submucous fibrosis. Natl J Maxillofacial Surg. 2021;12(3):316–23.
Lanjekar AB, Bhowate RR, Bakhle S, Narayane A, Pawar V, Gandagule R. Comparison of efficacy of topical curcumin gel with triamcinolone-hyaluronidase gel individually and in combination in the treatment of oral Submucous Fibrosis. J Contemp Dent Pract. 2020;21(1):83–90.
Guo JC, Xie H, Wu H, Tong TJ. [Efficacy of curcumin in the treatment of oral submucous fibrosis: a Meta-analysis]. Hua xi kou qiang yi xue za zhi = Huaxi kouqiang yixue zazhi = West. China J Stomatology. 2021;39(2):195–202.
Sodhi S, Sodhi JS, Khambete N, Kumar R, Marthala M, Sodhi NK. Expression of tumor necrosis factor alpha and its correlation with severity of oral submucous fibrosis: a case-control study. Oral Surg oral Med oral Pathol oral Radiol. 2014;117(6):704–8.
Borlinghaus J, Albrecht F, Gruhlke MC, Nwachukwu ID, Slusarenko AJ. Allicin: chemistry and biological properties. Molecules. 2014;19(8):12591–618.
Polhemus D, Kondo K, Bhushan S, Bir SC, Kevil CG, Murohara T, et al. Hydrogen sulfide attenuates cardiac dysfunction after heart failure via induction of angiogenesis. Circ Heart Fail. 2013;6(5):1077–86.
Li X, Wu H, Feng KW, Xu J, Wu S, Zhou ZZ, et al. Discovery of polymethoxyphenyl-pyridines bearing amino side chains as tubulin colchicine-binding site inhibitors. Bioorg Med Chem. 2022;73:117007.
Krishnamoorthy B, Khan M. Management of oral submucous fibrosis by two different drug regimens: a comparative study. Dent Res J. 2013;10(4):527–32.
El Khouli AM, El-Gendy EA. Efficacy of omega-3 in treatment of recurrent aphthous stomatitis and improvement of quality of life: a randomized, double-blind, placebo-controlled study. Oral surgery, oral medicine, oral pathology and oral radiology 2014, 117(2):191–196.
Gomaa AM, Abd El-Aziz EA. Omega-3 fatty acids decreases oxidative stress, tumor necrosis factor-alpha, and interleukin-1 beta in hyperthyroidism-induced hepatic dysfunction rat model. Pathophysiology. 2016;23(4):295–301.
Raizada MK, Sable DM, Chowdhery A, Chavan MS, Rajpurohit LS. Omega 3: a novel treatment agent in oral submucous fibrosis: a pilot study. J oral Pathol Medicine: Official Publication Int Association Oral Pathologists Am Acad Oral Pathol. 2017;46(6):439–42.
Gopinath D, Hui LM, Veettil SK, Nair AB, Maharajan MK. Comparative efficacy of interventions for the management of oral Submucous fibrosis: a systematic review and network Meta-analysis. J Personalized Med 2022, 12(8).
Acknowledgements
The authors gratefully acknowledge the financial supports by Natural Science Foundation of Hunan Province (No. 2021JJ70062); The Scientific Research Project of Hunan Health Commission (No. D202313048136); Chinese medicine research Project of Hunan Province (No. B2023048); Joint Fund Project of Hunan University of Chinese Medicine (No.2022XYLH120 and 2022XYLH134).
Funding
Natural Science Foundation of Hunan Province (No. 2021JJ70062); The Scientific Research Project of Hunan Health Commission (No.D202313048136); Chinese medicine research Project of Hunan Province(No.B2023048); Joint Fund Project of Hunan University of Chinese Medicine (No.2022XYLH120 and 2022XYLH134).
Author information
Authors and Affiliations
Contributions
Xueru Chen contributed to the data acquisition, interpretation and analysis, and manuscript writing; Jincai Guo contributed to the data acquisition and interpretation, data analysis, and critical revision of the manuscript; and Hui Xie contributed to the critical revision and approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, X., Xie, H. & Guo, J. Drug treatment for oral submucous fibrosis: an update. BMC Oral Health 23, 748 (2023). https://doi.org/10.1186/s12903-023-03488-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03488-9