Abstract
Background
Temporomandibular joint (TMJ) disc repositioning through open suturing (OSu) is a new disc repositioning method. Its result for adolescents with condylar resorption and dentofacial deformities combined with and without postoperative occlusal splints (POS) has not been well studied.
Objective
This study was to evaluate and compare the effects of OSu with and without POS in the treatment of TMJ anterior disc displacement without reduction (ADDwoR) in adolescent skeletal Class II malocclusion.
Methods
A total of 60 adolescents with bilateral ADDwoR were enrolled in this study. They were randomly allocated into two groups: OSu with and without POS. Magnetic resonance imaging (MRI) and lateral cephalometric radiographs were used to measure changes in condylar height and the degree of skeletal Class II malocclusion from before operation and at 12 months postoperatively. Changes in these indicators were compared within and between the two groups.
Results
After OSu, both groups exhibited significant improvements in condylar height and occlusion at the end of 12 months follow-up (P < 0.05). The group of OSu with POS had significantly more new bone formation (2.83 ± 0.75 mm vs. 1.42 ± 0.81 mm, P < 0.001) and improvement in dentofacial deformity than the group of OSu only (P < 0.05). The new bone height was significantly correlated with POS (P < 0.001), the changes of SNB (P = 0.018), overjet (P = 0.012), and Wits appraisal (P < 0.001).
Conclusion
These findings indicated that OSu can effectively stimulate condylar regeneration and improve skeletal Class II malocclusion in adolescents with bilateral ADDwoR. The results are better when combined with POS.
Trial registration
This trial was prospectively registered on the chictr.org.cn registry with ID: ChiCTR1900021821 on 11/03/2019
Similar content being viewed by others
Introduction
Temporomandibular joint (TMJ) anterior disc displacement (ADD) is one of the most prevalent TMJ disorders (TMD) in the population [1]. According to whether the disc can return to the normal position during mandibular movement, disc displacement is classified as ADD with reduction (ADDwR) or ADD without reduction (ADDwoR). During growth, ADD without treatment may cause condylar resorption and lead to a decrease in condylar height (CH), creating or worsening a dentofacial deformity [2,3,4,5,6]. According to Schellhas et al. and our previous studies, without treatment, unilateral ADD would cause mandibular deviation, while bilateral ADD would lead to skeletal Class II malocclusion demonstrated as mandibular retrognathia [2,3,4,5,6,7]. Conservative treatment often fails to prevent progressive condylar resorption [8,9,10], while disc repositioning (DR) by surgery could stimulate condylar regeneration, which was especially benefit for the correction of Class II malocclusion [3, 5, 6, 8, 11,12,13,14,15]. So far, there are 2 methods for DR [16,17,18]: suturing by arthroscopy or open suturing (OSu), and anchorage by a mini-screw anchor (MsA). Our previous study showed that OSu had more new bone formation than MsA in the treatment of adolescent ADDwoR [6].
After DR we found that the condyle moved anteriorly and inferiorly with increased joint space, which caused open bite in the molars. While after an average of 3 months postoperation, the condyle returned to its normal position [10, 19, 20]. We then used postoperative occlusal splint (POS) to maintain the open bite, so that the increased joint space after DR was benefit for condylar regeneration [15, 21]. In our previous studies, by magnetic resonance imaging (MRI) and cephalometric measurement, patients with POS after DR by MsA had more condylar new bone formation and improved dentofacial deformities when combined with orthodontic treatment than the one without POS [4, 13, 15].
Hence, we hypothesized that in adolescent skeletal Class II malocclusion with bilateral ADDwoR, DR by OSu with POS would stimulate more condylar bone regeneration and improve mandibular retrusion than surgery only. A randomized controlled trial was designed to evaluate this hypothesis.
Materials and methods
Study design
The trial was registered at the Chinese Clinical Trial Registry, a member of the World Health Organization international clinical trials registry (Registration Number: ChiCTR1900021821, Date: 11/03/2019). This study was approved by the Institutional Review Board of the Shanghai 9th People’s Hospital (JYLJ201805). All investigators participated in calibration meetings for standardizing the clinical trial protocol. It was conducted following ethical principles by the Declaration of Helsinki and good clinical practice guidelines. The flowchart for the CONSORT guidelines is presented in Fig. 1.
The trial was designed as a single-center, randomized, open-label, parallel-controlled clinical trial. Patients with bilateral ADDwoR and skeletal Class II malocclusion were recruited from the Department of Oral Surgery, Shanghai 9th People’s Hospital, from January 2019 to January 2021.
Sample-size calculation
According to our previous retrospective study of ADD with skeletal Class II malocclusion treatment by MsA with and without POS [4], the minimum difference in new bone height of the condyle was calculated for the sample size of this study by OSu with and without POS. 24 patients in each group were estimated as a minimum sample size to detect a clinically relevant difference, with a power of 80% and a statistical significance level of 0.05 (two-tailed). Allowing for a dropout rate of 20%, the total sample size was determined to be 60 patients.
Inclusion and exclusion criteria
The inclusion criteria were: (1) age between 12 and 20 years; (2) bilateral ADDwoR (Wilkes stage III to V) diagnosed by MRI; (3) skeletal Class II malocclusion with SNB < 78°and ANB > 4°measured by cephalometric films [22]. The exclusion criteria were: 1) history of TMJ surgical treatment and orthodontic treatment;2) history of developmental and/or systemic disorders such as autoimmune disease and rheumatoid arthritis that might affect craniofacial growth; 3) small condylar process or poor bone quality; (4) poorly formed articular disc length; (5) patients with malignant tumors and end-stage diseases; (6) pregnancy or lactation.
After the patients were screened, written informed consent to participate was obtained before enrolling them in the study.
Randomization
The patients were given an enrollment number (by H.Z.) in matched sealed envelopes that included group assignments based on block randomization (fixed block size of 4) by an independent statistician (S.C.) from the Biostatistics Office. Each patient was allocated into one of the following groups immediately before the operation:
Test group (OSu + POS group):
DR through OSu and POS.
Control group (OSu group):
DR through OSu.
TMJ MRI images, lateral cephalometric films, and dentition were obtained before the operation. The TRIOS3 oral scanner (3shape, Denmark) was used to record the dentition for POS fabrication and further orthodontic treatment by the orthodontist (Z.Y).
Surgical procedures
One senior surgeon (D.H.) performed DR by OSu under general anesthesia [18]. Through a small modified pre-auricular approach, the joint capsule was entered for disc repositioning. The disc was passively reduced after completely releasing the anterior attachment. Two horizontal sutures were placed at the border of the posterior band by a 20-gauged needle and a self-designed hook. The disc was sutured to the posterior articular capsule with 6 knots buried under the external auricular cartilage (Fig. 2).
Steps of disc repositioning by OSu (A-G) and suture instruments (H-I). A-B, exposure of the operative area through a small modified pre-auricular approach; C-G, suturing method; H, (a) exchangeable hooked thread lifter and (b) 20 gauge needle, (c) Tip of the hook lifter; I, suture thread, (a) guiding zone, (b) functional zone
POS fabrication
After operation, the condyle was moved forward and downward by the increased joint space, resulting in mandibular forward movement and posterior open bite [19]. An interocclusal wax registration was made to record this occlusion and sent to the orthodontist (Z.Y.) to design POS, so that new bone can be formed in the increased joint space and conducive to orthodontic treatment later. POS was fabricated by using polymethyl methacrylate material and provides complete coverage of the maxillary and mandibular dentition. Generally, the vertical dimension of the splint height is less than 2 mm. (Fig. 3). Patients were required to wear POS no less than 12 hours per day for 12 months [4].
MRI examination within one week after the operation was taken to assess the disc position. After 12 months, MRI and cephalometric films were taken for all patients to evaluate CH and jaw development. Patients were excluded if the discs were not properly repositioned or if they had relapsed. Adverse events of the DR and POS were monitored throughout the clinical trial period.
Outcomes
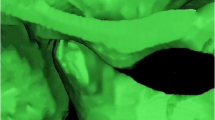
The primary outcome was condylar height measured by MRI (1.5-Tesla imager, Signa; General Electric, Milwaukee, WI, USA). Sagittal images with closed- and open-mouth positions and coronal images of the condyle were acquired for evaluation of disc position, condylar bone status and height [23, 24]. Images with the largest section of the condyle were selected, and the condylar height was determined based on the three-circle method [3]. E-Ruler measurement software was used to obtain parameter values with an accuracy of 0.01 mm (Fig. 4). Condylar height measurements before and at 12 months after operation were obtained. The positions of the generated new bone shown as double contour images were recorded as anterior, superior and posterior parts of the condyle.
The secondary outcome was the degree of skeletal Class II malocclusion measured by lateral cephalometric films, including the following variables: ∠SNA, ∠SNB, ∠ANB, incisor overjet, Wits appraisal, Y-Axis angle, Pog’-G’ (Pog’, pogonion of soft tissue; G’, a plane perpendicular to Frankfort horizontal plane through glabella), Sn-G’ (Sn, subnasale), U1-SN and, U1-L1. Shanghai Ninth People’s Hospital standard cephalometric analysis was used under Dolphin 11.5 software (Dolphin Imaging, Chatsworth, CA, USA) for measurement before operation and at 12-month follow-up (Fig. 5).
To guarantee the accuracy, MRIs and cephalometric radiographs were blindly evaluated by 2 clinicians (J.S & H.Z) twice at a 2-week interval. The average value of the 2 clinicians was calculated for comparison. If a statistical difference by a paired t-test was discovered (P < 0.05) in the 2 data sets, experts in TMJ or orthodontists were required to repeat the measurements.
Statistical analysis
Two TMJs of each patient were included in the analysis. The analyses applied the intention-to-treat (ITT) principle by analyzing all available data from all randomized patients according to their treatment allocation. Continuous variables with normal distribution were presented as mean ± standard deviation (SD); non-normal variables were reported as median (interquartile range). Differences in changes in condylar heights, maxillofacial sagittal mandibular position, and occlusal relationship at pre-operation and 12 months post-operative were analyzed by paired t-tests. Student t-test (for continuous variables) or Chi-Squared test (for qualitative variables) were used for comparing the differences in the above indicators between the two groups. Pearson test (when the variables were normally distributed) and Spearman correlation test (when the variables were not normally distributed) were used to evaluate the correlation between the height of condylar new bone with POS and changes of the skeletal Class II malocclusion. P < 0.05 was considered statistically significant. IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA) was utilized to analyze all data.
Results
One patient in the control group and one in the test group were lost because of Covid-19 outbreak, they refused to come for follow-up, so the trial procedures were completed with 58 patients (n = 29 in the test and control groups, respectively). At baseline, the mean age of the patients was 16.48 ± 2.45 years, 50 were females and 10 were males, and there were no statistical significances between the two groups in these or other baseline characteristics (P < 0.05, Table 1). None of the patients showed any side effects beyond the normal range for surgical procedures.
After DR, MRI showed that all discs were repositioned. In the OSu group, the condylar height increased from 19.11 ± 3.83 mm preoperatively to 20.52 ± 3.80 mm at the 12-month follow-up, with a mean increase of 1.42 ± 0.81 mm (P < 0.001). Among them, 46.6% of joints (27/58) had cap-shaped new bone formation in the anterior, superior, and posterior parts of the condyle. 89.7% joints (52/58) had new bone formation in any position. ∠SNB increased 0.65 ± 0.64° (P < 0.001), and other parameters decreased including incisal overjet (1.16 ± 1.03 mm, P < 0.001), ∠ANB (0.54 ± 1.18°, P = 0.020), Wits appraisal (0.55 ± 1.68 mm, P = 0.091), Y-axis angle (0.09 ± 1.26 °, P = 0.694), and Pog’-G’ (0.74 ± 1.86 mm, P = 0.040, Table 2).
In the OSu with POS group, the condylar height increased from 19.00 ± 3.65 mm preoperatively to 21.83 ± 3.85 mm at a 12-month follow-up, with a mean increase of 2.83 ± 0.75 mm (P < 0.001). Among them, 74.1% of joints (43/58) had cap-shaped osteogenesis. 100% joints (58/58) had new bone formation in any position. ∠SNB increased 1.83 ± 1.19° (P < 0.001), and other parameters decreased including the incisal overjet (2.04 ± 1.71 mm, P < 0.001),∠ANB (1.40 ± 1.30°, P < 0.001), Wits appraisal (2.43 ± 1.94, P < 0.001), Y-axis angle (1.55 ± 2.30°, P = 0.001), and Pog’-G’ (2.36 ± 3.59 mm, P = 0.001, Table 2; Figs. 6 and 7).
Female, 12years old, in the OSu + POS group. A, D, Preoperative facial photo; B, E, 12 months postoperative photo; C, F, photo after orthodontics treatment; G, preoperative overjet; H, 12 months postoperative overjet; I, overjet after orthodontic treatment; J, preoperative cephalometric film; K, 12 months postoperative cephalometric film; L, cephalometric film after orthodontic treatment; M, pre- (red outline) and 12 months postoperative (blue outline) cephalometric measurement showed improved mandibular retrusion
MRI of patient in Fig. 5. A, B, anteriorly displaced disc (red arrows), and discontinuous bone cortex of right & left condyles before operation; C, D, cap-shaped regenerated bone (red dashed line) after 12 months post operation
There was no statistical difference in SNA, U1-SN, Sn-G’, L1-MP and U1-L1 between the two groups before and after treatment (P > 0.05, Table 3). OSu with POS group had significantly more regenerated condylar new bone height (P < 0.001), higher osteogenesis rates (100.0% vs 89.7%, χ2 test, P = 0.036) and cap-shaped new bone formation rates(74.1% vs 44.8%, χ2 test, P = 0.001), more increased SNB (P < 0.001), more decreased overjet (P = 0.020), ANB (P = 0.011), Wits appraisal (P < 0.001), Y-axis angle (P = 0.004), and Pog’-G’ (P = 0.038) than OSu only group (Tables 3 and 4).
The correlation analysis showed that the height of condylar new bone was significantly correlated with wearing POS (r = 0.542, P < 0.001) and changes of mandibular position (△SNB, r = 0.311, P = 0.018; △overjet, r=-0.393, P = 0.002; △Wits appraisal, r=-0.498, P < 0.001, Table 5).
Discussion
The prevalence of ADD was observed to be three times higher during adolescence compared to other stages of life [25]. Roh et al. used MRI and reported that the incidence of condylar resorption was four times higher in patients with ADDwoR than in the general population [26]. When ADD happened in adolescents, condylar growth may be affected because of exceeding physiological loading. Many research have shown that adolescent ADDwoR and dentofacial deformities were closely connected [27,28,29]. Our previous studies by MRI follow-up also showed that condylar height decreased without treatment in adolescent patients with ADDwoR [2,3,4, 6, 13]. Mandibular deviation or retrusion was aggravated when ADD occurred unilaterally [3, 5] or bilaterally [4, 6, 11]. Functional appliances are usually used to correct patients with retrognathic mandibles [30,31,32]. However, it is noneffective for Class II malocclusion adolescents with bilateral ADDwoR and may increase the risk of condyle resorption thus exacerbate dentofacial deformities [4, 10]. Whether articular disc reduction by surgery can control or prevent condylar bone resorption, promote bone regeneration, and eventually obtain a stable joint has become the focus of many scholars.
Wolford et al. and our previous studies showed that DR could alleviate condylar bone resorption and encourage bone regeneration, especially in adolescents [8, 29]. Currently, there are two methods for DR: suturing by arthroscopy or open incision and anchorage by MsA. From the 1990s, many scholars attempted to use arthroscopic techniques to treat TMJ ADD, but the success rate was not high [26, 33]. In 2001, Wolford proposed implanting Mitek anchors into the condyle to fix the displaced articular disc [34]. Yang modified the technique with a self-designed MsA for easy reimplantation and retied the sutures [16]. The MRI follow-up studies showed that 10 months and 2 years stability was 98.6% and 95.3%, respectively [23, 35]. In a 5-year follow-up study, 89% of the discs were stable by MRI evaluation [36]. For patients with small condyles such as idiopathic condylar resorption and osteoporosis, it is difficult to implant the MsA. The dissection around the condyle may also affect the blood supply and increase the risk of condylar resorption [15]. In 2012, Yang reported an arthroscopic suturing method with self-designed instruments [17] that provided stable disc repositioning of 95.3% in 749 discs after 24-month follow up [37]. Although arthroscopic suturing method modified by Yang [17] without anchor implantation is suitable for hypoplastic condyles, the heavy equipment including arthroscope, light source, monitor and coblation device and difficult technique limit its wide application. Therefore, He et al. [18] proposed OSu technique by using the same self-designed hook of Yang’s arthroscopic surgery. It is easier to perform especially for the one with hyperplastic posterior bands or perforation [18]. Compared with MsA, OSu does not involve the insertion of anchor nails, the growth of the condyle may have the least mutual influence on surgical performance. Our previous study of 84 adolescents with ADD and Class II skeletal malocclusion, showed that OSu produced more condylar new bone formation and incisor overjet reduction than MsA [6]. A 1-year follow up study in 104 ADD adolescents from 10 to 18 years also showed that, through MRI image and cephalometric films, DR by OSu could promote condylar regeneration and alleviate maxillofacial deformity [11]. In this study, we determined the age of the participants according to the adolescence definition of World Health Organization (the second decade of life, 10–19 years of age). Although our sample population ranged wide from 12 to 20 years and most of them were women who ended growth after 15 years old [5, 6, 20, 38], at 1 year follow-up after DR, the condylar height increased significantly with improved dentofacial deformity. So it is the DR surgery that simulated condylar regeneration especially in adolescents who had strong tissue repair ability. By post-operative orthodontic treatment, orthognathic surgery may be avoided.
Another factor that affects postoperative condylar new bone formation is the application of POS. After DR, the condyle moved forward and downward, with the increasing of the superior and posterior joint space, resulting in posterior open bites. Without any interventions, the condyle returned to its normal position an average of 3 months after surgery [19]. Using POS can maintain this enlarged joint space, thus promoting new bone formation. It had been suggested that exceeding physiological loading could disrupt joint lubrication, leading to temporary hypoxia and consequently fibrocartilage destruction [39, 40]. So, wearing POS helps protect the new fragile bone from absorption under stressful conditions. Our previous studies showed that after DR by either arthroscopy or open surgery with POS, CH and dentofacial deformity improved more than without POS [4,5,6, 15]. We found that new bone remodeling generally occurs around 3 months after DR, with a peak around 6 months. Compared with OSu only, POS group had significantly more condylar new bone formation (2.83 ± 0.75 mm vs. 1.42 ± 0.81 mm) and a higher rate of cap-shaped osteogenesis (74.1% vs. 44.8%). Furthermore, the amount of condylar new bone was significantly correlated with POS and changes of the skeletal Class II malocclusion. In this study, orthodontic treatment began 1 year after DR for further malocclusion correction. The increased CH benefited orthodontic treatment especially in OSu with POS group.
It is debatable whether a patient will benefit from early open joint operations or whether a diverse variety of conservative nonsurgical methods should be considered before deciding on open joint surgery [41]. According to Gonçalves et al., a period of symptoms within 4 years provides the best predictor of outcomes in TMJ disc surgery [42]. Nitzan and Marmary [43] discovered that the endurance of symptoms had a detrimental impact on articular function. Our previous research has shown that ADD without intervention causes condylar resorption and may cause or accelerate dentofacial deformity in adolescent patients with and without TMJ symptoms. Under a comprehensive consideration, ADD should be treated as early as possible rather than as an end-stage disease later. Early surgery, particularly in adolescents during the growth spurt, should be conducted as soon as feasible to restore the condylar development potential, hopefully reducing the chance of future orthognathic surgery for mandibular retraction. Larger sample size is needed to determine whether DR by OSu and POS with further orthodontic treatment can avoid future orthognathic surgery.
Conclusion
This randomized controlled trial demonstrated that DR by OSu with POS can stimulate more condylar new bone formation in adolescents than OSu only, which can better improve skeletal Class II malocclusion.
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary information files (Additional file 1).
Abbreviations
- ADDwoR:
-
Anterior disc displacement without reduction
- ADDwR:
-
Anterior disc displacement with reduction
- CH:
-
Condylar height
- DR:
-
Disc repositioning
- ITT:
-
Intention-to-treat
- MRI:
-
Magnetic resonance imaging
- MsA:
-
Mini-screw anchor
- OSu:
-
Open suturing
- POS:
-
Postoperative splints
- SD:
-
Standard deviation
- TMD:
-
Temporomandibular joint disorders
- TMJ:
-
Temporomandibular joint
References
Hosgor H. The relationship between temporomandibular joint effusion and pain in patients with internal derangement. J Cranio-Maxillofacial Surg. 2019;47(6):940–4.
Zhuo Z, Cai X, Xie Q. Is anterior disc displacement without reduction associated with temporomandibular joint condylar height in juvenile patients younger than 20 years? J Oral Maxillofac Surg. 2015;73(5):843–9.
Xie Q, Yang C, He D, Cai X, Ma Z, Shen Y, et al. Will unilateral temporomandibular joint anterior disc displacement in teenagers lead to asymmetry of condyle and mandible? A longitudinal study. J Craniomaxillofac Surg. 2016;44(5):590–6.
Zhu H, He D, Yang Z, Song X, Ellis E. The effect of disc repositioning and post-operative functional splint for the treatment of anterior disc displacement in juvenile patients with class II malocclusion. J Craniomaxillofac Surg. 2019;47(1):66–72.
Liu Z, Xie Q, Yang C, Chen M, Bai G, Abdelrehem A. The effect of arthroscopic disc repositioning on facial growth in juvenile patients with unilateral anterior disc displacement. J Craniomaxillofac Surg. 2020;48(8):765–71.
Zhu H, He D, Yang Z, Lu C, Zhao J, Yang C. The Effect of Condylar Regeneration after different disc repositioning Surgeries in adolescents with skeletal class II malocclusion. J Oral Maxillofac Surg. 2021;79(9):1851–61.
Schellhas KP, Pollei SR, Wilkes CH. Pediatric internal derangements of the temporomandibular joint: effect on facial development. Am J Orthod Dentofacial Orthop. 1993;104(1):51–9.
Wolford LM, Cardenas L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999;116(6):667–77.
Fang B. [Relationship between the mandibular hypoplasia and temporomandibular joint internal derangement in adolescents with skeletal class II malocclusion]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2017;52(3):152–6.
Shen P, Liu X, Xie Q, Zhang S, Yang C. The Effect evaluation of functional Appliance used for class II patients with Temporomandibular Joint Anterior Disc Displacement. J Craniofac Surg. 2019;30(1):e15–7.
Wang X, Mao Y, Chen X, Zhen J, Zhang S. Radiologic outcomes of temporomandibular joint disk repositioning by suturing through an open incision in adolescent patients with anterior disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;S2212-4403(22)01117-8.
Yuan M, Shen P, Yang C. [Impact of temporomandibular joint arthroscopic discopexy on condylar growth in adolescents: a retrospective cohort study]. Chinese journal of stomatology [Internet]. 2021 Sep 2 [cited 2022 Oct 8];56(2). Available from: https://pubmed.ncbi.nlm.nih.gov/33557499/
Liu Z, Xie Q, Yang C, Chen M, Bai G, Shen P, et al. Functional orthodontics after arthroscopic disk repositioning in adolescent anterior disk displacement with mandibular retrusion. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;130(4):357–62.
Cai XY, Yang C, Jin JM, Song H. Condylar remodelling following arthroscopic disc repositioning of TMJ in teenage patients: a longitudinal magnetic resonance imaging study. China J Oral Maxillofac Surg. 2012;10(4):322–7.
Zhu H, Yang Z, He D, Hu N, Cheng Z. The effect of TMJ disk repositioning by suturing through open incision on adolescent mandibular asymmetry with and without a functional orthodontic appliance. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131(4):405–14.
Zhang S, Liu X, Yang C, Cai X, Chen M, Haddad MS, et al. New arthroscopic disc repositioning and suturing technique for treating internal derangement of the temporomandibular joint: part II–magnetic resonance imaging evaluation. J Oral Maxillofac Surg. 2010;68(8):1813–7.
Yang C, Cai XY, Chen MJ, Zhang SY. New arthroscopic disc repositioning and suturing technique for treating an anteriorly displaced disc of the temporomandibular joint: part I–technique introduction. Int J Oral Maxillofac Surg. 2012;41(9):1058–63.
He D, Yang C, Zhu H, Ellis E. Temporomandibular Joint Disc Repositioning by suturing through Open Incision: a technical note. J Oral Maxillofac Surg. 2018;76(5):948–54.
Chen X, Qiu Y, Zhang S, Zheng J, Yang C. Changes of the condylar position after modified disk repositioning: a retrospective study based on magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;129(1):14–20.
Hu YK, Abdelrehem A, Yang C, Cai XY, Xie QY, Sah MK. Changes in temporomandibular joint spaces after arthroscopic disc repositioning: a self-control study. Sci Rep. 2017;7:45513.
Ma Z, Xie Q, Yang C, Zhang S, Shen Y, Abdelrehem A. Can anterior repositioning splint effectively treat temporomandibular joint disc displacement? Sci Rep. 2019;9(1):534.
Burhan AS, Nawaya FR. Dentoskeletal effects of the bite-jumping Appliance and the twin-block Appliance in the treatment of skeletal class II malocclusion: a randomized controlled trial. Eur J Orthod. 2015;37(3):330–7.
Zhou Q, Zhu H, He D, Yang C, Song X, Ellis E. Modified Temporomandibular Joint Disc Repositioning with Mini-screw Anchor: Part II-Stability evaluation by magnetic resonance imaging. J Oral Maxillofac Surg. 2019;77(2):273–9.
Sun Q, Dong MJ, Tao XF, da Jiang M, Yang C. Selection and application of coils in temporomandibular joint MRI. Dentomaxillofac Radiol. 2020;49(3):20190002.
Isberg A, Hägglund M, Paesani D. The effect of age and gender on the onset of symptomatic temporomandibular joint disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(3):252–7.
Roh HS, Kim W, Kim YK, Lee JY. Relationships between disk displacement, joint effusion, and degenerative changes of the TMJ in TMD patients based on MRI findings. J Craniomaxillofac Surg. 2012;40(3):283–6.
Lei J, Yap AUJ, Liu MQ, Fu KY. Condylar repair and regeneration in adolescents/young adults with early-stage degenerative temporomandibular joint disease: a randomised controlled study. J Oral Rehabil. 2019;46(8):704–14.
Shen P, Zhang D, Abdelrehem A, Jin S, Luo Y, Yang C. Association between sexual maturation and anterior disc displacement of temporomandibular joint in adolescents aged 13–14 years. Clin Oral Investig. 2022.
Zhang X, Sun J, He D. Review of the studies on the relationship and treatment of anterior disc displacement and dentofacial deformity in adolescents. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology [Internet]. 2022 [cited 2022 Sep 5]; Available from: https://www.sciencedirect.com/science/article/pii/S2212440322010860
Ruf S, Pancherz H. Temporomandibular joint remodeling in adolescents and young adults during Herbst treatment: a prospective longitudinal magnetic resonance imaging and cephalometric radiographic investigation. Am J Orthod Dentofac Orthop. 1999;115(6):607–18.
Ruf S, Baltromejus S, Pancherz H. Effective condylar growth and Chin position changes in activator treatment: a cephalometric roentgenographic study. Angle Orthod. 2001;71(1):4–11.
Yildirim E, Karacay S, Erkan M. Condylar response to functional therapy with twin-block as shown by cone-beam computed tomography. Angle Orthod. 2014;84(6):1018–25.
Pirttiniemi P, Peltomäki T, Müller L, Luder HU. Abnormal mandibular growth and the condylar cartilage. Eur J Orthod. 2009;31(1):1–11.
Mehra P, Wolford LM. The Mitek mini anchor for TMJ disc repositioning: surgical technique and results. Int J Oral Maxillofac Surg. 2001;30(6):497–503.
He D, Yang C, Zhang S, Wilson JJ. Modified temporomandibular joint disc repositioning with miniscrew anchor: part I–surgical technique. J Oral Maxillofac Surg. 2015;73(1):47e1–9.
Liu X, Zhou Z, Mao Y, Chen X, Zheng J, Yang C, et al. Temporomandibular joint anchorage surgery: a 5-year follow-up study. Sci Rep. 2019;9(1):19106.
Liu X, Zheng J, Cai X, Abdelrehem A, Yang C. Techniques of Yang’s arthroscopic discopexy for temporomandibular joint rotational anterior disc displacement. Int J Oral Maxillofac Surg. 2019;48(6):769–78.
Liu X, Shen P, Wang X, Zhang S, Zheng J, Yang C. A prognostic nomogram for postoperative bone remodeling in patients with ADDWoR. Sci Rep. 2018;8:4361.
Nitzan DW. The process of lubrication impairment and its involvement in temporomandibular joint disc displacement: a theoretical concept. J Oral Maxillofac Surg. 2001;59(1):36–45.
Betti BF, Everts V, Ket JCF, Tabeian H, Bakker AD, Langenbach GE, et al. Effect of mechanical loading on the metabolic activity of cells in the temporomandibular joint: a systematic review. Clin Oral Investig. 2018;22(1):57–67.
Puthukkudiyil JS, Bhutia O, Roychoudhury A, Bhatt K, Yadav R, Bhalla AS. Does Repositioning of Temporomandibular Joint Disc with Bone Anchors provide better clinical outcomes than conventional disc plication procedures for anterior disc displacements without reduction in patients refractory to nonsurgical treatments? J Oral Maxillofac Surg. 2020;78(12):2160–8.
Gonçalves JR, Cassano DS, Rezende L, Wolford LM. Disc repositioning: does it really work? Oral Maxillofac Surg Clin North Am. 2015;27(1):85–107.
Nitzan DW, Marmary Y. The anchored disc phenomenon: a proposed etiology for sudden-onset, severe, and persistent closed lock of the temporomandibular joint. J Oral Maxillofac Surg. 1997;55(8):797–803.
Acknowledgements
The authors thank the Dongmei He’s research staff and patients who participated in the trial. The authors also thank Mr. Sicheng Wu and Mr. Xin Nie (Biostatistics Office of Clinical Research Center, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China) for help with statistical analysis. The trial is registered at chictr.org.cn, ChiCTR1900021821. Full details of the trial protocol are available at Chictr.org.cn.
Funding
This work was supported by the Science and Technology Commission of Shanghai Municipality Science Research Project [20Y11903900, 20S31902500]; the National Natural Science Foundation of China [32071313, 82270996]; Cross-disciplinary Research Fund of Shanghai Ninth People’s Hospital, Shanghai JiaoTong university School of Medicine [JYJC202203].
Author information
Authors and Affiliations
Contributions
Conceptualization: ZY and DH; data curation: JS and HZ; formal analysis: JS; investigation: JS, HZ, CL and JZ; methodology: JS, HZ, CL, JZ, ZY and DH; supervision: XN and DH; validation: DH; visualization: JS; writing - original draft: JS and DH; writing - review & editing: DH. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The trial in the manuscript was registered at the Chinese Clinical Trial Registry, a member of the World Health Organization international clinical trials registry (Registry Number: ChiCTR1900021821; Registry Time: 03/11/2019). This study was approved by the ethics committee of Shanghai Ninth People’s Hospital affiliated with Shanghai Jiao Tong University, School of Medicine (Number: SH9H-2018-T88-2; Registry Time: 04/03/2019). All the methods in the trial were carried out in accordance with relevant guidelines and regulations. All participants permitted this study and signed an informed consent agreement. For participants that are minors, informed consent have been obtained from a parent and/or legal guardian.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, J., Zhu, H., Lu, C. et al. Temporomandibular joint disc repositioning and occlusal splint for adolescents with skeletal class II malocclusion: a single-center, randomized, open-label trial. BMC Oral Health 23, 694 (2023). https://doi.org/10.1186/s12903-023-03402-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03402-3