Abstract
Background
Osteogenesis of lateral window sinus elevation surgery is the key to placement of the subsequent implant, excessive collapse of the sub-antral space may adversely affect long-term stability of implants. At present, few studies focus on the influence of the contact area of the sub-antral space on osteogenesis. This study evaluated whether the change in the contact area of the sub-antral space with maxillary sinus bone and the Schneiderian membrane can affect osteogenesis.
Methods
Cone beam computed tomography (CBCT) images were collected of patients requiring maxillary sinus floor elevation (residual bone height < 6 mm) for standard-length implant placement before surgery, after surgery, and at 6-month follow-up visits. The postoperative sub-antral space volume (V1) and surface area (S1), and the remaining volume after six months of healing (V2) were measured. Then, the contact area of sub-antral space with maxillary sinus bone (Sbc) and the Schneiderian membrane (Smc), the absorbed volume during healing (Va), and the percentage of remaining volume (V2%) and absorbed volume (Va%) were calculated. The correlation between anatomical parameters was analyzed using multiple linear regression.
Results
A total of 62 maxillary sinuses from 56 patients were augmented, of which 57 were considered for the final analysis (5 withdrew due to perforation). Multiple linear regression results demonstrated that Sbc was significantly positively correlated with Va (β coefficient = 0.141, p < 0.01) without correlation between Smc and Va (β coefficient = − 0.046, p = 0.470). There was a positive correlation between Sbc and V2% (β coefficient = 2.269, p < 0.05).
Conclusions
This study confirmed that the size of the Sbc in lateral window sinus elevation surgery affected osteogenesis after six months of healing. Clinicians should assess the sinus contour type preoperatively, then consider whether it is necessary to expand the range of the Schneiderian membrane elevation to avoid excessive collapse of the sub-antral space.
Trial registration: Chinese Clinical Trial Registry (ChiCTR), ChiCTR2200057924. Registered 22 March 2022–Retrospectively registered.
Similar content being viewed by others
Background
Lateral window sinus elevation surgery was first presented by Tatum in 1976 and then published by Boyne and James in 1980. It is an innovative method that can predictably increase the height available at the bone in the maxillary posterior tooth area to place a standard-length implant [1]. The best material for this surgery is autologous bone due to its excellent bone conduction, bone induction, and osteogenesis [2]. Although the new bone formation rate of autologous bone is significantly higher than that of other types of bone graft materials, it also has disadvantages, such as the need for a second surgical site, the limited amount, and low dimensional stability [3]. In particular, low dimensional stability means the absorption of graft materials and the collapse of the graft volume, which can significantly affect surgical outcomes [4, 5]. Therefore, new graft materials have been developed, including allografts and xenografts, and their applications in clinical treatment and scientific research have been studied in-depth [6,7,8,9]. Xenografts are widely used due to their high three-dimensional stability during healing after bone augmentation surgery [10, 11].
During the healing process after lateral window sinus elevation surgery, the two major biological behaviors affecting osteogenesis are extensive neoangiogenesis and the migration and colonization of osteoprogenitor cells from surrounding bone [12, 13]. The Schneiderian membrane and the maxillary sinus bone support this physiological process, but the Schneiderian membrane does not consistently significantly contribute to new bone formation [14]. Some animal experiments depict that the pluripotent mesenchymal cells of the Schneiderian membrane contribute to osteogenesis [15, 16], while other animal experiments suggested no obvious effect of the Schneiderian membrane on new bone formation. However, the effect of sinus bone on osteogenesis has been widely recognized in many studies [17, 18]. So how do the Schneiderian membrane and maxillary sinus bone affect those biological processes of osteogenesis after sinus augmentation? The size of Sbc and Smc may significantly impact osteogenesis since better bone formation was observed when the diameter of bone graft material particles decreased to give a larger contact area in an in vitro tissue engineering study [19]. In maxillary sinuses with different sinus widths, the contact area between the implant and sinus walls is larger in the narrow sinus, which promotes the vascular blood supply for bone formation [20]. Nevertheless, to date, there is little research focusing on the influence of Sbc and Smc on the osteogenic effect. Therefore, this prospective study aimed to determine how Sbc and Smc affect osteogenesis following lateral window sinus elevation surgery.
Methods
Study protocol
This prospective cohort study was reported according to the STROBE statement. All procedures were conducted according to the guidelines of the Declaration of Helsinki as revised in Fortaleza (2013) for human subject research. The study protocol was approved by the ethics committee of Stomatology Hospital, Shandong University, China (No. 20190107), and registered in the Clinical Trial Registry (ChiCTR2200057924). The patients provided written informed consent to participate in the trial and authorized the use of their data for the study purposes after being informed of the study protocol, treatment protocol, alternatives, and any potential dangers.
Selection criteria
Any patient with missing teeth in the maxillary posterior area and requiring lateral window sinus elevation surgery to increase the available bone height to place a standard-length implant was eligible for inclusion. The inclusion criteria were: age > 18 years; edentulism in the maxillary premolar and molar region for at least three months; residual bone height (RBH) < 6 mm and residual bone crest width ≥ 6 mm in site(s) prepared for the implant placement; systemic condition sufficient to undergo surgery; willing to provide informed consent, good medical compliance, and be able to return to the hospital regularly. The exclusion criteria were: absolute contraindications for implant surgery or bone augmentation surgery [21]; smokers (≥ 10 cigarettes/day); pregnancy or lactation; uncontrolled systemic diseases (diabetes, hypertension, autoimmune diseases, etc.); undergoing head and neck radiotherapy or bisphosphate treatment; allergic to materials that they may be exposed to during the operation; uncontrolled periodontal disease, dental pulp disease or other oral diseases; suffering from maxillary sinusitis (thickness of the Schneiderian membrane > 2 mm, sinus effusion, and sinus density increased) [22,23,24]; previous implant or bone augmentation surgery at the surgical site; the Schneiderian membrane perforation during the operation.
Pre-surgical phase
Comprehensive medical history collection and clinical examination were conducted for the patients included in this study. The oral examination included a periodontal and endodontic examination and CBCT evaluation of the health status of the sinus and the residual bone quantity at the planned implant site. The patients were divided into two groups according to the RBH based on expert consensus and ITI treatment guide of bone augmentation surgery [25, 26]: group A (3 mm ≤ RBH < 6 mm): simultaneous implant group, and group B (RBH < 3 mm): delayed implant group (Table 1).
Surgical procedure
Antibiotics (cefixime, metronidazole) were administered 0.5 h before the operation to prevent infection, and the mouths were rinsed with compound chlorhexidine mouthwash three times for 30 s. Concentrated growth factor (CGF) was prepared as instructed 10 min before surgery [27]. Under local anesthesia, a mid-crestal incision and two buccal releasing incisions were made, and the full-thickness flap was lifted to expose the buccal bone wall of the sinus. After removing the lateral wall, the Schneiderian membrane was carefully and evenly elevated with manual instruments until the sub-antral space reached the preset size. After checking the integrity of the Schneiderian membrane by visual inspection and the Valsalva maneuver, two to four CGF membranes were inserted into the sub-antral space, the mixture of red blood cells/platelets, and deproteinized bovine bone matrix (Bio-Oss®, Geistlich AG, Switzerland) was then grafted. A gelatin sponge was used to stop bleeding if necessary. A resorbable bovine collagen membrane (Bio-Gide®, Geistlich AG, Switzerland) was secured with pins to cover the lateral antrostomy. The patients in group A received 10–12 mm long implants (Straumann AG, Switzerland), and the flap was sutured with non-absorbable surgical sutures (Fig. 1). Postoperative CBCT images were taken immediately. Each patient was given antibiotics (Cefixime, metronidazole) for three days, gargled with compound chlorhexidine for one week, and given acetaminophen if necessary. The precautions after the operation were explained, and patients were informed to remove the sutures ten days later. The healing status of the patients was checked monthly.
After six months of healing, patients returned to the hospital for CBCT images to evaluate recovery. Patients in group B received 10–12 mm long implants (Straumann AG, Switzerland). The patients in both groups continued to fix superstructure restoration. The CBCT images collected from each patient included T0 (preoperative), T1 (immediately after operation), and T2 (six months after operation).
Radiographic measurements
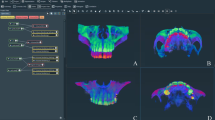
The data were analyzed by three independent surveyors using image processing software (Mimics Medical version 21.0). After confirming that there were no size errors, the sub-antral space was divided to check the coronal, axial, and sagittal planes for deviation before the 3D reconstruction of the model (Fig. 2). Automatically calculate the basic data of sub-antral space according to those models, including the postoperative volume (V1), remaining volume after six months of healing (V2) and surface area at T1 (S1). The sub-antral space at T1 was divided into two parts according to the contact relationship with the maxillary sinus bone wall and the Schneiderian membrane (Fig. 3); the surface area was automatically calculated as Sb (surface area of the sub-antral space in contact with bone) and Sm (surface area of the sub-antral space in contact with the Schneiderian membrane) respectively. The Sj was defined as the surface area of an imaginary plane, which divides the sub-antral space into upper and lower parts; the upper part contacts the Schneiderian membrane, while the lower part contacts the sinus bone (Sj is only used as the transition value for calculating Sbc and Smc, and how the imaginary plane divides the sub-antral space does not affect the calculation of subsequent values). The surface area of the removed lateral bone wall was defined as Sr. For group A, the volume of the implant entering the sub-antral space should be subtracted when calculating V1 and V2, and the cross-sectional area of the implant should be subtracted when calculating Sbc. The surface areas and their relationships are illustrated in Fig. 4.
Volume and surface area analysis was performed using Mimics. A “Green mask” of the sub-antral space was created as the region of interest. A–C: the coronal, axial and sagittal planes of sub-antral space. D: A 3-dimensional model, including sub-antral space (green), bone tissue around maxillary sinus (yellow) and some nearby teeth (white)
Contact area analysis using Mimics. A Sub-antral space was divided into two parts according to its contact relationship with maxillary sinus bone wall and the Schneiderian membrane, (a) the Schneiderian membrane, the red line marks its lower boundary, (b) maxillary sinus bone. B The sub-antral space that in contact with the Schneiderian membrane (c). C the sub-antral space that in contact with maxillary sinus bone (d)
Contact relationship between sub-antral space and surrounding tissue. Smc: the contact area of sub-antral space with schneiderian membrane. Sr: the surface area of the removed lateral bone wall. Sbc: the contact area of sub-antral space with maxillary sinus bone. Sj: the surface area of an imaginary plane, which divides the sub-antral space into upper and lower parts, the upper part contacts the Schneiderian membrane, while the lower part contacts the sinus bone
Numeral calculations
Some of the values used in the statistical analysis were calculated according to the following formulas:
Predictor and outcome variables
The null hypothesis in this prospective research was that the change in the contact area of the sub-antral space with bone and the Schneiderian membrane does not affect osteogenesis. The primary predictor variables are the contact area of sub-antral space with bone (Sbc) and the Schneiderian membrane (Smc).
Primary outcome measure: the absorbed volume of the sub-antral space (Va).
Secondary outcome measures: the remaining volume of the sub-antral space (V2); percentage of the absorbed volume (Va%); percentage of the remaining volume (V2%); the occurrence of any complications.
Statistical analysis
Data were collected by an independent investigator and analyzed using statistical software (IBM SPSS Statistics for Windows, Version 26.0, IBM Corp.). The intraclass correlation coefficient (ICC) was used to compare the reproducibility between the three surveyors. The Shapiro–Wilk test was used to evaluate the existence of normal distribution, the assumptions required to apply the parameter test are met by all parameters. Descriptive statistics were fully recorded, including mean and standard deviation. Independent sample t-tests were performed to evaluate the difference between Va, V2, Va%, and V2% in groups A and B. Multiple linear regression analysis was performed to study the influence of Va, V2, Va%, and V2%, respectively, and the independent factors were V1, Sbc, and Smc. Durbin-Watson test was used to evaluate the independence of samples, with R-squared values as a goodness-of-fit measure. A p-value < 0.5 was considered statistically significant.
Results
Study population and clinical results
The study initially included 62 maxillary sinuses from 56 patients, all of whom underwent lateral window sinus elevation surgery in the Department of Oral Implantology, Stomatology Hospital, Shandong University, Jinan, China, from January 2019 to August 2021. The surgeries were performed by three experienced implantologists. Due to the different sizes of the Schneiderian membrane perforations during surgery, five patients withdrew from the study, and after perforation repair, those patients did not suffer serious complications during the follow-up period of at least one year. Ultimately, 57 maxillary sinuses from 51 patients (25 males; 26 females; mean age 51.8 ± 11.9; age range 22–74 years) were analyzed: 33 cases in group A (simultaneous implant) and 24 in group B (delayed implant). During the follow-up period of 7–38 months, all implants functioned normally, without complications or adverse events during the intraoperative, postoperative, and follow-up phases.
Radiographic measurements
The mean measured values of the three surveyors were analyzed and were highly consistent (ICC > 0.830). Table 2 presents the volume of sub-antral space in groups A and B immediately after the operation and after six months of healing, showing no significant difference in bone formation between the two groups. Therefore, in the subsequent analysis, the two data groups were combined into one group.
As displayed in Table 3, linear regression analysis indicated a significant positive correlation between V1 and Va (p < 0.001). Table 4 illustrates the linear regression results for the contact area (Sbc and Smc) and Va, revealing a significant positive correlation between Sbc and Va (p = 0.002) but no correlation between Smc and Va (p = 0.470). This suggests that Sbc is more likely than Smc to affect Va; thus, we focused on Sbc in the following analysis. Table 5 depicts that Sbc and V2 are significantly positively correlated (p < 0.001).
Tables 6 and 7 displays the linear regression results of volume percentage (Va% and V2%) and Sbc, indicating a significantly positive correlation between Sbc and V2% and a significantly negative correlation between Sbc and Va%. Since the sum of Va% and V2% is 1, the two tables are equal except for the opposite β coefficient value.
Discussion
The success of maxillary sinus floor elevation was due to the effect of new bone formation, which is influenced by anatomical morphology, bone graft substitutes, surgical methods, etc. In the process of new bone formation, extensive neovascularization, migration, and colonization of bone progenitor cells are two key biological steps of postoperative healing. The neovascular network and osteoprogenitor cells may come from the bone or sinus membrane in contact with the graft materials. This signifies that the size of the contact area is likely to affect osteogenesis; however, this is little literature regarding its impact, how it affects, and the specific impact relationship.
This study evaluated the effect of Sbc and Smc on Va, showing that the graft material is in contact with the maxillary sinus bone, the more it will be absorbed, and for every 1 cm2 increase in the contact area, the absorbed volume increases by 0.141 cm3. During the healing process, the sub-antral space volume reduction is mainly due to the absorption of the contents, which in addition to the bone substitute, contains CGF, blood, and air (Fig. 5), but the metabolism rate of these contents is much faster than that of the bone substitute. Therefore, when the Sbc is larger, these contents will be absorbed faster, and the Schneiderian membrane does not participate in this absorption process, which indicates that the contribution of bone to the absorption of these contents is much greater than that of the Schneiderian membrane. Although the bone material will also be absorbed during the healing, since Bio-oss is a long-term degradation material that is difficult to be absorbed [28], it can exist in the body for a long time [29], so the volume of this part is negligible. Second, the reduction of sub-antral space volume is also related to the collapse of the three-dimensional structure of bone material, which may be affected by the negative pressure generated by the absorption of contents within the gaps of bone material particles, and the process is associated with the extra pressure on the Schneiderian membrane [5, 30], which is unavoidable due to respiration [31]. However, no effect of Smc on Va was observed in this study, so the effect of pressure from breathing on collapse may be much greater than that of Smc.
This study analyzed the effect of Sbc on V2, showing that there is a considerable positive association between Sbc and V2, illustrating the relationship between Sbc and the osteogenic effect. The larger Sbc can preserve more bone graft after six months of healing. This argument resembles the one mentioned in the previous paragraph that "the larger the Sbc, the greater the amount of absorbed graft material", which is the correlationship between volume and area. However, there is often a strong inherent correlation between the volume and area values of sub-antral space; in other words, the larger the volume, the larger the area, and vice versa. So, the significant positive correlation between Sbc and V2 may not fully explain the influence of Sbc on osteogenesis. Therefore, ratios were used instead of numerical values to represent the osteogenic effect to avoid the influence of the strong correlation between volume and area on the results. Sbc was significantly positively correlated with V2% and significantly negatively correlated with Va%, and when Sbc increased by 1 cm2, V2% increased by 2.27%. This indicates that the larger the Sbc, the higher the volume of graft material maintained, and the more new bone can be obtained. The possible reason for this, as mentioned earlier, is that a larger contact area leads to more osteoprogenitor cell migration, as well as a wider range of neovascularization.
Significant correlation of Sbc with V2% and Va% has important implications for clinical and research work. Clinicians not only need to consider the patient factors (systemic condition, oral condition, maxillary sinus anatomy, etc.), select the appropriate type of graft material and dosage, but appropriately increase the contact area of the graft material with the sinus wall and sinus floor during the operation when faced with a patient who may require sinus bone augmentation to gain more neogenetic bone. In the light of the classification of maxillary sinus contours [32], in the narrow tapered maxillary sinus, the proper elevation of the maxillary sinus membrane and filling of graft materials can achieve a large contact area between the sub-antral space and the bone, resulting in a good osteogenic effect (Fig. 6A). However, in the square maxillary sinus, especially at sites that require delayed implantation, the traditional sinus membrane elevation range often cannot obtain a sufficient Sbc, so it is necessary to consider continuing to elevate the sinus membrane (Fig. 6B); otherwise, the bone height after six months of healing may be lower than expected. In square maxillary sinuses where simultaneous implantation can be performed, an implant may assist in maintaining the volume of the sub-antral space [33], but this was not supported in other studies [34,35,36]. As a result, if the scope of the elevated sinus membrane is not excessive in the square maxillary sinus, it may lead to less periapical bone in the implant at the follow-up visit after six months or even the implant in direct contact with the Schneiderian membrane (Fig. 7), which may damage the sinus membrane, leading to perforation [37] and affect the long-term survival of the implant [38]. It should be noted that in the process of increasing Sbc by elevating the membrane, for those maxillary sinuses with an acute angle between the sinus walls or sinus septa and obvious vessels are present, it is also vital to control the angle and strength of the surgical instruments to avoid bleeding and perforation of the Schneiderian membrane [39], or consider using hydraulic pressure [40,41,42]. For researchers, Sbc should be considered as one of the variables when studying the factors influencing osteogenesis of the maxillary sinus lifting surgery, and its value should be recorded and inserted into statistical models or controlled as an irrelevant variable when studying other influencing factors.
In addition, this study corroborates the conclusions of previous studies that V1 is significantly positively correlated with Va, which means the more graft material, the more it is absorbed [43]. Simultaneous and delayed implant placement results in similar bone augmentation in line with two separate studies with a short-term follow-up of four months after loading and a long-term follow-up of 24 months after surgery [34, 35]. Thus, the choice of implant timing for patients who need sinus floor lift surgery does not affect the osteogenic effect, so clinicians should choose simultaneous or delayed implant methods based on bone mineral density and the overall cortical bone thickness [44].
This study confirmed that bone formation is affected by the contact area between the sub-antral space and surrounding bone after lateral window sinus elevation surgery. Moreover, the contact area between the sub-antral space and the Schneiderian membrane has no effect; thus, it is possible to reject the null hypothesis. However, this study has some limitations, such as the time point at which CBCT images were collected (6 months after surgery) only provides information on prognosis in the short term, and images at follow-up visits may be needed to confirm these results [45]. Furthermore, only one bone graft material (Bio-oss) was used in this study, so the applicability of the findings to other materials needs to be investigated. Lastly, similar to other studies, only imaging methods were used to analyze the effect of contact area on osteogenesis [39, 46], and it is better to use histological studies to further verify the results [47]. Further larger, longer-term studies are required to confirm these results.
Conclusions
This study confirmed that the size of Sbc in lateral window sinus elevation surgery affects osteogenesis after six months of healing, as Sbc is positively correlated with V2%. Therefore, clinicians should assess the sinus contour type preoperatively to consider whether the range of the sinus membrane elevation should be expanded and the amount of bone graft material increased to avoid excessive collapse of the sub-antral space.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CBCT:
-
Cone beam computed tomograph
- V1 :
-
Postoperative sub-antral space’s volume
- CGF:
-
Concentrated growth factor
- S1 :
-
Postoperative sub-antral space’s surface area
- V2 :
-
Remaining volume after 6 months of healing
- Sbc :
-
Contact area of sub-antral space with maxillary sinus bone
- Smc :
-
Contact area of sub-antral space with schneiderian membrane
- Sj :
-
The surface area of an imaginary plane, which divides the sub-antral space into upper and lower parts, the upper part contacts the Schneiderian membrane, while the lower part contacts the sinus bone
- Sb :
-
Surface area of the part in contact with bone
- Sm :
-
Surface area of the sub-antral space in contact with the Schneiderian membrane
- Sr :
-
Surface area of the removed lateral bone wall
- Va :
-
Absorbed volume during healing
- V2%:
-
Percentage of remaining volume
- Va%:
-
Percentage of absorbed volume
- RBH:
-
Residual bone height
- T0 :
-
Preoperative
- T1 :
-
Immediately after operation
- T2 :
-
6 Months after operation
References
Raghoebar GM, Onclin P, Boven GC, Vissink A, Meijer HJA. Long-term effectiveness of maxillary sinus floor augmentation: a systematic review and meta-analysis. J Clin Periodontol. 2019;46:307–18. https://doi.org/10.1111/jcpe.13055.
Corbella S, Taschieri S, Weinstein R, Del Fabbro M. Histomorphometric outcomes after lateral sinus floor elevation procedure: a systematic review of the literature and meta-analysis. Clin Oral Implant Res. 2016;27:1106–22. https://doi.org/10.1111/clr.12702.
Danesh-Sani SA, Engebretson SP, Janal MN. Histomorphometric results of different grafting materials and effect of healing time on bone maturation after sinus floor augmentation: a systematic review and meta-analysis. J Periodontal Res. 2017;52:301–12. https://doi.org/10.1111/jre.12402.
Umanjec-Korac S, Wu G, Hassan B, Liu Y, Wismeijer D. A retrospective analysis of the resorption rate of deproteinized bovine bone as maxillary sinus graft material on cone beam computed tomography. Clin Oral Implant Res. 2014;25:781–5. https://doi.org/10.1111/clr.12174.
Zhang L, Si M, Shi J, Yang G, Shi Y. Evaluation of three-dimensional contraction of the volume of grafts after staged augmentation of the sinus floor, and an analysis of influential factors. Br J Oral Maxillofac Surg. 2019;57:323–9. https://doi.org/10.1016/j.bjoms.2019.03.006.
Danesh-Sani SA, Loomer PM, Wallace SS. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. Br J Oral Maxillofac Surg. 2016;54:724–30. https://doi.org/10.1016/j.bjoms.2016.05.008.
Khehra A, Levin L. Maxillary sinus augmentation procedures: a narrative clinical review. Quintessence Int. 2020;51:578–84. https://doi.org/10.3290/j.qi.a44632.
Al-Dajani M. Recent trends in sinus lift surgery and their clinical implications: recent trends in sinus lift surgery. Clin Implant Dent Relat Res. 2016;18:204–12. https://doi.org/10.1111/cid.12275.
Wang D, Tabassum A, Wu G, Deng L, Wismeijer D, Liu Y. Bone regeneration in critical-sized bone defect enhanced by introducing osteoinductivity to biphasic calcium phosphate granules. Clin Oral Implant Res. 2017;28:251–60. https://doi.org/10.1111/clr.12791.
Velasco-Ortega E, Valente NA, Iezzi G, Petrini M, Derchi G, Barone A. Maxillary sinus augmentation with three different biomaterials: Histological, histomorphometric, clinical, and patient-reported outcomes from a randomized controlled trial. Clin Implant Dent Relat Res. 2021;23:86–95. https://doi.org/10.1111/cid.12964.
Dumitrescu CR, Neacsu IA, Surdu VA, et al. Nano-hydroxyapatite vs. Xenografts: synthesis, characterization, and in vitro behavior. Nanomaterials. 2021;11:2289. https://doi.org/10.3390/nano11092289.
Carano RAD, Filvaroff EH. Angiogenesis and bone repair. Drug Discovery Today. 2003;8:980–9. https://doi.org/10.1016/S1359-6446(03)02866-6.
Busenlechner D, Huber CD, Vasak C, Dobsak A, Gruber R, Watzek G. Sinus augmentation analysis revised: the gradient of graft consolidation. Clin Oral Implant Res. 2009;20:1078–83. https://doi.org/10.1111/j.1600-0501.2009.01733.x.
Dragonas P, Katsaros T, Schiavo J, Galindo-Moreno P, Avila-Ortiz G. Osteogenic capacity of the sinus membrane following maxillary sinus augmentation procedures: a systematic review. Int J Oral Implantol. 2020;13:213–32.
Scala A, Botticelli D, Faeda RS, Garcia Rangel I Jr, de Oliveira JA, Lang NP. Lack of influence of the Schneiderian membrane in forming new bone apical to implants simultaneously installed with sinus floor elevation: an experimental study in monkeys. Clin Oral Implants Res. 2012;23:175–81. https://doi.org/10.1111/j.1600-0501.2011.02227.x.
Schweikert M, Botticelli D, de Oliveira JA, Scala A, Salata LA, Lang NP. Use of a titanium device in lateral sinus floor elevation: an experimental study in monkeys. Clin Oral Implant Res. 2012;23:100–5. https://doi.org/10.1111/j.1600-0501.2011.02200.x.
Costa MM, Botticelli D, Moses O, et al. Maxillary sinus augmentation using ceramic alloplastic granules or paste: an experimental study in rabbits. Dent J. 2021;9:65. https://doi.org/10.3390/dj9060065.
Stacchi C, Lombardi T, Ottonelli R, Berton F, Perinetti G, Traini T. New bone formation after transcrestal sinus floor elevation was influenced by sinus cavity dimensions: a prospective histologic and histomorphometric study. Clin Oral Implant Res. 2018;29:465–79. https://doi.org/10.1111/clr.13144.
Li S, Wang T, Hu J, et al. Effect of hydroxyapatite content and particle size on the mechanical behaviors and osteogenesis in vitro of polyetheretherketone–hydroxyapatite composite. Polym Compos. 2021;42:6512–22. https://doi.org/10.1002/pc.26317.
Cheng X, Hu X, Wan S, Li X, Li Y, Deng F. Influence of lateral-medial sinus width on no-grafting inlay osteotome sinus augmentation outcomes. J Oral Maxillofac Surg. 2017;75:1644–55. https://doi.org/10.1016/j.joms.2017.03.010.
Hwang D, Wang H. Medical contraindications to implant therapy: part I: absolute contraindications. Implant Dent. 2006;15:353–60. https://doi.org/10.1097/01.id.0000247855.75691.03.
Shanbhag S, Karnik P, Shirke P, Shanbhag V. Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. J Endod. 2013;39:853–7. https://doi.org/10.1016/j.joen.2013.04.010.
Lu Y, Liu Z, Zhang L, et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod. 2012;38:1069–74. https://doi.org/10.1016/j.joen.2012.04.027.
Rak K, Newell J, Yakes W, Damiano M, Luethke J. Paranasal sinuses on MR images of the brain: significance of mucosal thickening. Am J Roentgenol. 1976;1991(156):381–4. https://doi.org/10.2214/ajr.156.2.1898819.
Fugui Z, Yucheng S, Lixin Q, et al. Expert consensus on the bone augmentation surgery for alveolar bone defects. J Prev Treat Stomatol Dis. 2022;30:229–36. https://doi.org/10.12016/j.issn.2096-1456.2022.04.001.
Scott RA. ITI treatment guide, volume 5: sinus floor elevation procedures. Br Dent J. 2012;212:512–512. https://doi.org/10.1038/sj.bdj.2012.462.
Chen H, Zhou L, Wu D, Zhang J, Zheng Y, Chen Y. Osteotome sinus floor elevation with concentrated growth factor and simultaneous implant placement with or without bone grafting: a retrospective study. Int J Oral Maxillofac Surg. 2022;51:1078–84. https://doi.org/10.1016/j.ijom.2021.10.010.
Guarnieri R, Belleggia F, DeVillier P, Testarelli L. Histologic and histomorphometric analysis of bone regeneration with bovine grafting material after 24 months of healing. A case report. J Funct Biomater. 2018;9:48. https://doi.org/10.3390/jfb9030048.
Traini T, Valentini P, Iezzi G, Piattelli A. A histologic and histomorphometric evaluation of anorganic bovine bone retrieved 9 years after a sinus augmentation procedure. J Periodontol. 1970;2007(78):955–61. https://doi.org/10.1902/jop.2007.060308.
Lim H, Kim S, Kim D, Herr Y, Chung J, Shin S. Factors affecting maxillary sinus pneumatization following posterior maxillary tooth extraction. J Periodontal Implant Sci. 2021;51:1–11. https://doi.org/10.5051/jpis.2007220361.
Asai S, Shimizu Y, Ooya K. Maxillary sinus augmentation model in rabbits: effect of occluded nasal ostium on new bone formation. Clin Oral Implant Res. 2002;13:405–9. https://doi.org/10.1034/j.1600-0501.2002.130409.x.
Niu L, Wang J, Yu H, Qiu L. New classification of maxillary sinus contours and its relation to sinus floor elevation surgery. Clin Implant Dent Relat Res. 2018;20:493–500. https://doi.org/10.1111/cid.12606.
Cricchio G, Sennerby L, Lundgren S. Sinus bone formation and implant survival after sinus membrane elevation and implant placement: a 1- to 6-year follow-up study. Clin Oral Implant Res. 2011;22:1200–12. https://doi.org/10.1111/j.1600-0501.2010.02096.x.
Yin L, Yu Z, Chen Z, et al. Analysis of bone height changes after maxillary sinus augmentation with simultaneous and delayed placement of dental implants: a clinical and radiographic study: bone height changes after maxillary sinus augmentation. J Prosthodont. 2016;25:440–5. https://doi.org/10.1111/jopr.12317.
Felice P, Pistilli R, Piattelli M, et al. 1-stage versus 2-stage lateral maxillary sinus lift procedures: 4-month post-loading results of a multicenter randomised controlled trial. Eur J Oral Implantol. 2013;6:153–65.
Mazzocco F, Lops D, Gobbato L, Lolato A, Romeo E, Del Fabbro M. Three-dimensional volume change of grafted bone in the maxillary sinus. Int J Oral Maxillofac Implants. 2014;29:178–84. https://doi.org/10.11607/jomi.3236.
Omori Y, Botticelli D, Ferri M, Delgado-Ruiz R, Balan VF, Xavier SP. Argon bioactivation of implants installed simultaneously to maxillary sinus lifting without graft. An experimental study in rabbits. Dent J. 2021;9:105. https://doi.org/10.3390/dj9090105.
Park W, Kang KL, Han J. Factors influencing long-term survival rates of implants placed simultaneously with lateral maxillary sinus floor augmentation: a 6- to 20-year retrospective study. Clin Oral Implant Res. 2019;30:977–88. https://doi.org/10.1111/clr.13505.
Testori T, Weinstein T, Taschieri S, Wallace SS. Risk factors in lateral window sinus elevation surgery. Periodontol. 2000;2019(81):91–123. https://doi.org/10.1111/prd.12286.
Ro JH, Moon JH, Cheon MC, Park CJ. Measurement of hydraulic pressure on the sinus membrane for safer control during transcrestal sinus lifting. Int J Oral Maxillofac Surg. 2021;50:1267–70. https://doi.org/10.1016/j.ijom.2021.02.003.
Lee J, Kim S, Shin S, Chung J, Herr Y, Lim H. Effectiveness of hydraulic pressure-assisted sinus augmentation in a rabbit sinus model: a preclinical study. Clin Oral Invest. 2021;2022(26):1581–91. https://doi.org/10.1007/s00784-021-04131-z.
Bhandari S, Thomas R, Kumar T, Shah R, Mehta DS. Maxillary sinus augmentation using hydraulic pressure by lateral approach and simultaneous implant placement: clinicoradiographic study. Implant Dent. 2019;28:514–9. https://doi.org/10.1097/ID.0000000000000911.
Pesce P, Menini M, Canullo L, et al. Radiographic and histomorphometric evaluation of biomaterials used for lateral sinus augmentation: a systematic review on the effect of residual bone height and vertical graft size on new bone formation and graft shrinkage. J Clin Med. 2021;10:4996. https://doi.org/10.3390/jcm10214996.
Rues S, Schmitter M, Kappel S, Sonntag R, Kretzer JP, Nadorf J. Effect of bone quality and quantity on the primary stability of dental implants in a simulated bicortical placement. Clin Oral Invest. 2020;2021(25):1265–72. https://doi.org/10.1007/s00784-020-03432-z.
Lundgren S, Johansson AS, Cricchio G, Lundgren S. Clinical outcome and factors determining new bone formation in lateral sinus membrane elevation with simultaneous implant placement without grafting material: a cross-sectional, 3–17 year follow-up study. Clin Implant Dent Relat Res. 2019;21:827–34. https://doi.org/10.1111/cid.12758.
Schwarz L, Schiebel V, Hof M, Ulm C, Watzek G, Pommer B. Risk factors of membrane perforation and postoperative complications in sinus floor elevation surgery: review of 407 augmentation procedures. J Oral Maxillofac Surg. 2015;73:1275–82. https://doi.org/10.1016/j.joms.2015.01.039.
Zhou W, Wang F, Magic M, Zhuang M, Sun J, Wu Y. The effect of anatomy on osteogenesis after maxillary sinus floor augmentation: a radiographic and histological analysis. Clin Oral Invest. 2021;25:5197–204. https://doi.org/10.1007/s00784-021-03827-6.
Acknowledgements
The authors wish to thank Department of Oral Implantology, Stomatology Hospital, Shandong University, Jinan, China for their precious help in the surgery and Imag acquisition.
Funding
This study was financed by Shandong Natural Science Foundation (ZR2021MH092).
Author information
Authors and Affiliations
Contributions
DS as corresponding author, gave the idea of research design and confirmed the final manuscript. XS as first author, did data collection, analysis and discussion, completed the first draft of the article. DZ, XX and XS evaluated and invited patients to participate in the research, completed the treatment process, and revised the first draft. ZZ, CJ, ZL, did some data collection and analysis. All the authors agreed with the accuracy of the content of this article, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were carried out in strict conformity with the guidelines of the Declaration of Helsinki as revised in Fortaleza (2013) for human subject research. The protocol of this study was approved by an ethics committee (Stomatology Hospital, Shandong University, China, No. 20190107) and registered in Clinical Trial Registry (ChiCTR2200057924, https://www.chictr.org.cn/edit.aspx?pid=153276&htm=4). The patients provided a written informed consent to participate in the trial and authorized the use of their data for the study's purposes after being thoroughly told about the study protocol, treatment protocol, alternatives, and any potential dangers.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
She, X., Zhang, D., Xu, X. et al. Influence of the contact area of the sub-antral space with sinus bone and the Schneiderian membrane on osteogenesis in lateral window sinus elevation surgery: a prospective experiment. BMC Oral Health 22, 650 (2022). https://doi.org/10.1186/s12903-022-02694-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02694-1