Abstract
Background
Enterococcus faecalis and Candida albicans are frequently found in persistent endodontic infection and could remain in dentinal tubules despite intracanal medication with calcium hydroxide (Ca(OH)2), a commonly used medication. Thus, an effective and safe antimicrobial medication against such refractory infection is necessary in endodontic retreatment, so we aimed to test the efficacy of chitosan paste against these microorganisms compared with Ca(OH)2 in root canals of extracted human teeth.
Methods
Thirty-six sterilized human root samples prepared from extracted premolars and upper maxillary incisors were infected with E. faecalis for 14 days, while 32 were infected with C. albicans for 48 h, for mature biofilm formation. The samples were assigned to 6 groups of intracanal medications: Group 1: no medication (negative control); Group 2: 20% Polyethylene glycol (PEG); Group 3: 20% Propylene glycol (PG); Group 4: Ca(OH)2; Group 5: Chitosan + PEG; and Group 6: Chitosan + PG. After 7 days, intracanal surface dentin was harvested using Protaper next, resuspended, serially diluted and spread on Brain–Heart-Infusion agar (for E. faecalis) and Yeast Extract-Peptone-Dextrose agar (for C. albicans) for colony count. Antimicrobial efficacy was determined as percentage of remaining colony forming unit (CFUs) relative to negative control and analyzed using One-way ANOVA and post-hoc Games-Howell test. The significance level was set at 0.05.
Results
For E. faecalis, chitosan + PG had significantly higher antibacterial activity than Ca(OH)2 (P = 0.039). Chitosan + PEG and chitosan + PG medication significantly reduced viable bacteria compared with negative control, PEG and PG (P = 0.001, 0.003, 0.024, respectively for chitosan + PEG; P = 0.002, 0.003, 0.014, respectively for chitosan + PG). For C.albicans, chitosan + PEG and chitosan + PG were not significantly different from Ca(OH)2. However, Chitosan + PEG and chitosan + PG, but not Ca(OH)2, showed a significantly lower level of remaining CFUs compared with negative control (P = 0.013 and 0.005, respectively).
Conclusion
Chitosan paste showed better efficacy in reducing viable E. faecalis biofilm when compared to Ca(OH)2 after 7-day intracanal medication in this in vitro root canal model. It could also significantly reduce viable C. albicans, but was not significantly different from Ca(OH)2.
Similar content being viewed by others
Background
A major factor in endodontic failure in root canal-treated teeth is persistent infection [1, 2]. Thus, it is critical to have effective disinfection of the root canal system. To eradicate microorganisms, intracanal medication is an important part of endodontic treatment that relies on the efficacy of antimicrobial agents [2]. Calcium hydroxide (Ca(OH)2) has been used as a routine intracanal medication. However, certain microorganisms are still frequently detected in failed endodontic treated teeth, such as Enterococcus faecalis and Candida albicans [3].
E. faecalis is a Gram positive cocci that can invade dentinal tubules, form biofilm, attach to collagen in serum, and suppress lymphocyte activity, which can protect them from destruction [4]. It also has a proton pump inhibitor mechanism to resist to a wide pH range, up to approximately pH 11.5 [5]. Thus, it can tolerate the alkalinity of Ca(OH)2, could remain after root canal obturation, and is frequently found in persistent infection [3, 6]. C. albicans is another microorganism that has been reported in persistent post-treatment apical periodontitis [7]. An important virulence factor of C. albicans is the ability to switch between blastospore and hyphal form. This enables it to invade host tissue and avoid phagocytosis by macrophages [8]. Thigmotropism allows C. albicans to penetrate into deep dentinal tubules [9]. C. albicans can form biofilm in 48 h [10]. It can survive in a wide range of pH, high alkaline environment and ecologically harsh conditions, which allow them to cause persistent infection [8].
Chitosan is a natural polysaccharide derived from deacetylation of chitin in crustacean shells. Chitosan has antimicrobial, antifungal properties and enhances wound healing [11]. Chitosan can interact with microbial outer cellular components, cell membrane, and cytoplasmic constituents, and could inhibit biofilm formation [12]. Chitosan also has high biocompatibility, low toxicity, and showed inhibitory effect on planktonic form and biofilm of E. faecalis and C. albicans [13, 14]; thus, it may be effective as an antimicrobial intracanal medication. Previously published studies have shown that certain derivatives of chitosan are effective against E. faecalis and common oral Candida species, including C. albicans [15,16,17]. In particular, it has been demonstrated that 1700 kDa and 2100 kDa chitosan are effective against E. faecalis, but they require a long contact time (over 1 h) [17]. Thus, we propose that these chitosan derivatives are promising to be developed into intracanal medication [17, 18].
In order to formulate chitosan into intracanal medication, Polyethylene glycol (PEG) and Propylene glycol (PG) can be used as vehicles to deliver intracanal medication through dentinal tubules and apical foramen [19]. In addition, a previous study suggested that propylene glycol have antibacterial effect on S. mutans, E. faecalis, and E. coli [20]. Thus, it may also contribute to antimicrobial activity of the medication. This study aimed to develop chitosan paste as intracanal medication and test its antimicrobial activity against E. faecalis and C. albicans in comparison with Ca(OH)2 in the root canals of extracted human teeth. The null hypothesis was that chitosan paste would not be different from Ca(OH)2 in terms of antimicrobial activity against E. faecalis and C. albicans.
Methods
This study was carried out in accordance with Declaration of Helsinki and the proposal was approved by "The Human Research Ethics Committee of the Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand" (No. 055/2020). Informed consent was waived because the donors of the extracted tooth samples were unidentifiable.
Root samples
Sixty-eight intact premolars and upper maxillary incisors with single straight root canal extracted for orthodontic and periodontitis reasons were collected. Teeth with caries, fractures, cracks or other defects detected by magnifying loupes were excluded. The tooth samples were prepared as described with minor modification [21, 22]. All extracted teeth were stored in 0.1% thymol (MU DENT, Mahidol university, Bangkok, Thailand) until prepared for the experiments [22]. All soft-tissue remnants on the surfaces, the crowns and the coronal third of roots were removed until each root was 15 mm long. The root canals were enlarged by using Protaper next size X4 (Dentsply Sirona, Ballaigues, Switzerland) with 300 RPM speed and 2 g cm torque in a rotary handpiece. The samples were irrigated with 3 ml of 2.5% sodium hypochlorite (NaOCl) (Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand) followed by 1 ml of 17% ethylenediaminetetraacetic acid (EDTA) (Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand) to remove organic and inorganic debris. All samples were irrigated with 5 ml of distilled water to remove any remaining prior irrigants, and autoclaved for 20 min at 121 °C. The external surfaces were sealed with nail vanish. The samples were divided into 2 groups, 36 were inoculated with E. faecalis and 32 were inoculated with C. albicans. We calculated sample size based on a previous report on the differences in viable bacterial count between calcium hydroxide and calcium hydroxide combined with chitosan nanoparticles [21] using n4studies application [23]. The calculated sample size was 2 samples per group at 80% power of test. Nevertheless, all experiments were performed three times, each with 1–2 samples/group, so the total sample size was 5–6/group.
Preparation of microbial culture
E. faecalis (ATCC 29212) was incubated in brain heart infusion (BHI) broth (Himedia, Mumbai, India) at 37 °C until log phase. C. albicans (ATCC 90028) was incubated in Yeast extract—peptone-dextrose broth (YPD; Oxoid, UK and HiMedia, India) at 30 °C until log phase. The microbial suspension was adjusted to optical density of 0.5 for E. faecalis and 0.1 for C. albicans at 600 nm for inoculation into the root canals.
Infection of the root samples
Log phase culture (30 μl) of E. faecalis or C. albicans was inoculated into the root canals. For E. faecalis, BHI media was replenished every 48 h and the samples were incubated for 14 days for mature biofilm formation [24]. For C. albicans, the root samples were incubated for 48 h for mature biofilm formation [10]. All procedures were carried out in a biosafety cabinet (LabGard NuAire Inc, MN, USA).
Preparation of intracanal medications
The chitosan powder (1700 KDa, Marine Bio Resources, Samutsakhon, Thailand) was dissolved in 1% acetic acid (Merck KGaA, Darmstadt, Germany) at 20 mg/ml. The chitosan pastes were prepared by mixing 1 ml of chitosan solution (20 mg/ml) with 1 ml of Polyethylene glycol (PEG; Krungthepchemi, Bangkok, Thailand) or propylene glycol (PG; Krungthepchemi, Bangkok, Thailand), and 3 ml of distilled water. The final concentration of chitosan was 4 mg/ml in 20% PEG or PG. The pastes were sterilized by autoclave (Hirayama, Tokyo, Japan).
Ca(OH)2 intracanal medication was prepared by mixing 0.4 g of Ca(OH)2 powder (Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand) with 10 ml of distill water. The final concentration of Ca(OH)2 was 40 mg/ml.
Antimicrobial assessment
After the specified incubation period, an aliquot of the media from each sample was plated on solid media to check for microbial purity and viability. Root samples infected with E. faecalis and those with C. albicans were allocated to 6 groups and treated as follow Group 1: no medication (negative control), Group 2: 20% Polyethylene glycol (PEG), Group 3: 20% Propylene glycol (PG), Group 4: Ca(OH)2, Group 5: Chitosan + PEG, and Group 6: Chitosan + PG. Thirty μl of the assigned medication were applied into each root canal using a micropipette (Rainin Instrument Co., Oakland, CA, USA).The whole volume was delivered to ensure that the canal was filled. The root samples were incubated at 37ºC for E. faecalis and 30ºC for C. albicans in 24-well plates with covers for 7 days. After 7 days, the canals were washed with 3 ml of sterile distilled water and Protaper next size X4 was used at 300 RPM speed and 2 g cm torque to remove the medicament.
Dentin samples were harvested from root canal surfaces as previously described with minor modification [25] using Protaper next size X5 (Dentsply Sirona, Ballaigues, Switzerland) at 300 RPM speed and 2gcm torque and collected in 1 ml of phosphate buffered saline solution. After serial dilutions, 100 μl of each dilution were plated on BHI agar for E. faecalis and YPD agar for C. albicans, and incubated for 24 h at 37 °C for E. faecalis and 48 h at 30 °C for C. albicans. Colonies were counted and calculated into percentage of remaining viable microorganisms relative to the negative control. All experiments were performed in duplicates and repeated 3 times (except for the PEG and PG groups for C. albicans where only one sample/group was available for two of the experiments).
Statistical analysis
Shapiro–Wilk was used to test for normality of the data. Welch’s ANOVA was used to analyze the differences in percentage of remaining viable microorganisms after treatment among groups, followed by Games-Howell test for pairwise comparison. Data were analyzed using IBM SPSS Statistics for Windows, Version 22.0 (IBM, Armonk, New York, USA). A P value of < 0.05 was considered statistically significant.
Results
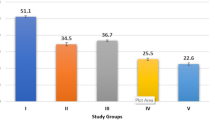
After 7 days of treatment with various medications, the remaining viable microorganisms in the root canals were examined by plate count. The results are shown in Fig. 1 for E. faecalis and Fig. 2 for C. albicans. For E. faecalis, the average percentage of remaining bacteria in both chitosan + PEG (9.68 ± 8.6%) and chitosan + PG (3.02 ± 2%) groups was significantly lower than that of the negative control (102.74 ± 26%), PEG (85.7 ± 25.3%) and PG (45.28 ± 17.9%) groups. (P = 0.001, 0.003, and 0.024, respectively for chitosan + PEG; P = 0.002, 0.003, and 0.014, respectively for chitosan + PG). In addition, the PG group showed a significantly lower remaining E. faecalis than the negative control (P = 0.015). Ca(OH)2 (46.38 ± 23.4%) also had a significantly lower level of remaining E. faecalis than the negative control group (P = 0.034). Chitosan + PG could reduce the bacteria to a level that is significantly lower than the Ca(OH)2 group (P = 0.039) but this was not significantly different for the chitosan + PEG group (P = 0.071).
For C. albicans, both chitosan + PEG (24.77 ± 20.5%) and chitosan + PG (7.57 ± 14.6%) groups harbored significantly lower remaining viable C.albicans compared with the negative control (105.40 ± 36.5%) (P = 0.013 and 0.005, respectively). However, they were not significantly different from PEG (122.06 ± 71.7%) and PG (95.36 ± 64.8%) groups (P = 0.292, and 0.441, respectively for chitosan + PEG; P = 0.206 and 0.293, respectively for chitosan + PG). In contrast, PEG, PG, and Ca(OH)2 (41.19 ± 38.1%) were not significantly different from the negative control (P = 0.997, 1.00, and 0.106, respectively).
Discussion
In this study, we showed that 1700 kDa chitosan (4 mg/ml) paste has good antimicrobial efficacy against E. faecalis and C. albicans biofilm in human root canals, especially chitosan + PG paste, which showed significantly higher efficacy than calcium hydroxide against E. faecalis. The results suggest that chitosan paste is a promising candidate to be further developed into an antimicrobial intracanal medication, particularly in cases with persistent E. faecalis infection.
Microbiological investigations found a complex community of bacteria and fungi in root canal treated teeth with persistent infection/chronic apical periodontitis [1, 3]. This suggests that previous endodontic treatment could not efficiently control these microorganisms. Mechanical instrumentation using larger size rotary instruments may help to remove bacteria and fungi in the root canals, but it cannot completely eradicate microbes in complex root canal structures and excessive instrumentation weakens root dentin [26,27,28,29]. Thus, effective antimicrobial intracanal medication can overcome the limitations of instrumentation to reduce microorganisms in complex anatomy of the root canals. Ca(OH)2 has been used as routine intracanal medication, but it was not effective against E. faecalis and C. albicans [30,31,32]. Several studies have identified E. faecalis and C. albicans as important microorganisms using culture-dependent and molecular techniques [3, 33, 34]. For example, a recent study used culture-dependent methods and showed that the most prevalent microorganisms in root canal treated teeth was E. faecalis (36.6%) and followed by C. albicans (20%) [3]. Studies using PCR detected E. faecalis at a prevalence of up to 77%, and C. albicans up to 35%, of failed root-filled teeth [33, 34]. Although E. faecalis was not the most abundant bacteria detected by metagenomic studies, it was observed at a greater frequency or proportion in secondary apical periodontitis than primary infection [35, 36]. Thus, persistence of these microorganisms in the root canals are problematic for endodontic treatment and effective antimicrobial agent against E. faecalis and C. albicans in root canals is clearly needed [32, 37, 38].
Our group has previously shown that 1700 kDa chitosan and 2100 kDa chitosan could effectively kill E. faecalis at an MBC of 2 mg/ml [17]. However, it needed a long contact time of over 10 min, so it is likely more effective when applied as a root-canal medication rather than as an irrigant. In addition, we also showed that these chitosan derivatives has a minimum fungicidal concentration against C. albicans at 4 mg/ml [16]. Thus, in this study, we formulated 4 mg/ml of 1700 KDa chitosan in 0.2% acetic acid into a paste for application as an antimicrobial intracanal medication. We used 20% PEG or PG to confer good flowability for easy handling and enhance penetration into dentinal tubules.
Our results showed that chitosan paste could eliminate more E. faecalis than negative control and carrier controls. Chitosan + PG showed greater antibacterial effect against E. faecalis biofilm than PG, and also greater than Ca(OH)2. Although E. faecalis could resist to Ca(OH)2 by a proton pump mechanism, our result showed that Ca(OH)2 was better at reducing viable E. faecalis than no medication [30]. Since PG could also reduce E. faecalis compared with negative control, the combined effect of both chitosan and PG may explain why chitosan + PG is the most effective in this experiment. Chitosan is positively charged and binds the negatively charged microbial cell membrane, while PG can help intracanal medication to penetrate deeper in dentinal tubules and it also has germicidal activity [20, 39, 40]. Similarly, chitosan-propolis nanoparticles was shown to be effective at eliminating E. faecalis biofilm after 7 days of medication [18]. Thus, chitosan is a promising alternative option for intracanal medication, either alone or in combination with other active ingredients, especially in infection where E. faecalis and/or C. albicans infection may play important roles. We also found that chitosan paste was effective against C. albicans biofilm as both chitosan groups had significantly less remaining viable C. albicans than the negative control. We could not detect significant differences among other groups, likely due to the wide variations in the CFU results. For C.albicans, Ca(OH)2 was not significantly different from the negative control group. Our results suggest that Ca(OH)2 is more effective against E. faecalis than C. albicans. This is concordant with a report by Ercan and colleagues [41].
Microorganisms in biofilm are more tolerant to antimicrobial agents, and this is the form found in the root canals [8, 42]. Thus, we simulated such biofilm condition in this study using extracted human root specimens inoculated with E. faecalis and with C. albicans, and allowed sufficient time for mature biofilm formation and penetration in dentinal tubules, i.e., 14 days for E. faecalis and 48 h for C. albicans, according to previous reports [10, 42, 43]. In addition, we collected dentin shavings to evaluate remaining viable microorganisms. In contrast to sample collections by irrigation or using paper points, this method allowed us to examine bacteria that invaded into dentinal tubules that may not have direct contact with intracanal medication if it does not penetrate well into dentinal tubules [44]. Our results showed that chitosan paste could significantly reduce viability of both E. faecalis and C. albicans in this root canal biofilm model. Thus, it has a great advantage over antibiotics medication, which are effective only against bacteria, but not fungi, and may also lead to tooth discoloration [45]. Nevertheless, this in vitro model used single-species biofilm, unlike in vivo conditions where multiple species coexist in a community. Therefore, further studies on multi-species biofilm and clinical trials should be performed in order to develop chitosan paste for future clinical applications. In addition, in this study, the effects of the medication were examined at 7-day after medication. This may be a limitation because previous studies suggested that a longer period of medication may be required [46]. However, a previous study showed that the antimicrobial activity of Ca(OH)2 after 7 day and 14-day medication was not significantly different [47] and another study showed that pH of Ca(OH)2 already increased after 7 days [48]. Nevertheless, further research on optimizing the length of medication time will be required.
Conclusion
In this root-canal biofilm model, chitosan paste showed better efficacy in reducing viable E. faecalis biofilm when compared to Ca(OH)2 after 7-day intracanal medication in this in vitro root canal model. It also significantly reduced viable C. albicans, but was not significantly different from Ca(OH)2. Therefore, it could be developed into an effective antimicrobial intracanal medication".
Availability of data and materials
The data analyzed in the present study are available in Additional file 1.
Abbreviations
- Ca(OH)2 :
-
Calcium hydroxide
- E. faecalis :
-
Enterococcus faecalis
- C. albicans :
-
Candida albicans
- PEG:
-
Polyethylene glycol
- PG:
-
Propylene glycol
- ANOVA:
-
Analysis of variance
References
Nair PN, Sjogren U, Krey G, Kahnberg KE, Sundqvist G. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. J Endod. 1990;16(12):580–8.
Lin LM, Skribner JE, Gaengler P. Factors associated with endodontic treatment failures. J Endod. 1992;18(12):625–7.
Pourhajibagher M, Ghorbanzadeh R, Bahador A. Culture-dependent approaches to explore the prevalence of root canal pathogens from endodontic infections. Braz Oral Res. 2017;31:e108.
Love RM. Enterococcus faecalis–a mechanism for its role in endodontic failure. Int Endod J. 2001;34(5):399–405.
Molander A, Reit C, Dahlen G. The antimicrobial effect of calcium hydroxide in root canals pretreated with 5% iodine potassium iodide. Endod Dent Traumatol. 1999;15(5):205–9.
Rocas IN, Siqueira JF Jr, Santos KR. Association of Enterococcus faecalis with different forms of periradicular diseases. J Endod. 2004;30(5):315–20.
Waltimo TM, Sen BH, Meurman JH, Orstavik D, Haapasalo MP. Yeasts in apical periodontitis. Crit Rev Oral Biol Med. 2003;14(2):128–37.
Siqueira JF Jr, Sen BH. Fungi in endodontic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(5):632–41.
Chua EG, Parolia A, Ahlawat P, Pau A, Amalraj FD. Antifungal effectiveness of various intracanal medicaments against Candida albicans: an ex-vivo study. BMC Oral Health. 2014;14:53.
Tyagi SP, Sinha DJ, Garg P, Singh UP, Mishra CC, Nagpal R. Comparison of antimicrobial efficacy of propolis, Morinda citrifolia, Azadirachta indica (Neem) and 5% sodium hypochlorite on Candida albicans biofilm formed on tooth substrate: an in-vitro study. J Conserv Dent. 2013;16(6):532–5.
Ballal N, Kundabala M, Bhat K, Acharya S, Ballal M, Kumar R, Prakash P. Susceptibility of Candida albicans and Enterococcus faecalis to Chitosan, Chlorhexidine gluconate and their combination in vitro. Aust Endod J. 2009;35(1):29–33.
Raafat D, Sahl HG. Chitosan and its antimicrobial potential: a critical literature survey. Microb Biotechnol. 2009;2(2):186–201.
Wang N, Ji Y, Zhu Y, Wu X, Mei L, Zhang H, Deng J, Wang S. Antibacterial effect of chitosan and its derivative on Enterococcus faecalis associated with endodontic infection. Exp Ther Med. 2020;19(6):3805–13.
Pu Y, Liu A, Zheng Y, Ye B. In vitro damage of Candida albicans biofilms by chitosan. Exp Ther Med. 2014;8(3):929–34.
Namangkalakul W, Benjavongkulchai S, Pochana T, Promchai A, Satitviboon W, Howattanapanich S, Phuprasong R, Ungvijanpunya N, Supakanjanakanti D, Chaitrakoonthong T, et al. Activity of chitosan antifungal denture adhesive against common Candida species and Candida albicans adherence on denture base acrylic resin. J Prosthet Dent. 2020;123(1):181 e181-181 e187.
Srimaneepong V, Thanamee T, Wattanasirmkit K, Muangsawat S, Matangkasombut O. Efficacy of low-molecular weight chitosan against Candida albicans biofilm on polymethyl methacrylate resin. Aust Dent J. 2021;66:262–9.
Supotngarmkul A, Panichuttra A, Ratisoontorn C, Nawachinda M, Matangkasombut O. Antibacterial property of chitosan against E. faecalis standard strain and clinical isolates. Dent Mater J. 2020;39:456–63.
Parolia A, Kumar H, Ramamurthy S, Davamani F, Pau A. Effectiveness of chitosan-propolis nanoparticle against Enterococcus faecalis biofilms in the root canal. BMC Oral Health. 2020;20(1):339.
Cruz EV, Kota K, Huque J, Iwaku M, Hoshino E. Penetration of propylene glycol into dentine. Int Endod J. 2002;35(4):330–6.
Nalawade TM, Bhat K, Sogi SH. Bactericidal activity of propylene glycol, glycerine, polyethylene glycol 400, and polyethylene glycol 1000 against selected microorganisms. J Int Soc Prev Community Dent. 2015;5(2):114–9.
Del Carpio-Perochena A, Kishen A, Felitti R, Bhagirath AY, Medapati MR, Lai C, Cunha RS. Antibacterial properties of chitosan nanoparticles and propolis associated with calcium hydroxide against single- and multispecies biofilms: an in vitro and in situ study. J Endod. 2017;43(8):1332–6.
Valera MC, Silva KC, Maekawa LE, Carvalho CA, Koga-Ito CY, Camargo CH, Lima RS. Antimicrobial activity of sodium hypochlorite associated with intracanal medication for Candida albicans and Enterococcus faecalis inoculated in root canals. J Appl Oral Sci. 2009;17(6):555–9.
Ngamjarus C. n4Studies: sample size calculation for an epidemiological study on a smart device. Siriraj Med J. 2016;68:160–70.
Taneja S, Kumar P, Malhotra K, Dhillon J. Antimicrobial effect of an oxazolidinone, lantibiotic and calcium hydroxide against Enterococcus faecalis biofilm: an in vitro study. Indian J Dent. 2015;6(4):190–4.
Attia DA, Farag AM, Afifib IK, Darrag AM. Antimicrobial effect of different intracanal medications on various microorganisms. Tanta Dent J. 2015;12(1):41–7.
Zelic K, Vukicevic A, Jovicic G, Aleksandrovic S, Filipovic N, Djuric M. Mechanical weakening of devitalized teeth: three-dimensional finite element analysis and prediction of tooth fracture. Int Endod J. 2015;48(9):850–63.
Usman N, Baumgartner JC, Marshall JG. Influence of instrument size on root canal debridement. J Endod. 2004;30(2):110–2.
Koprowicz A, Łęski M, Pawlicka H. Properties of mechanical endodontic instruments and the quality of the simulated canal preparation. Dent Med Probl. 2016;53(4):476–82.
Koprowicz A, Łęski M, Pawlicka HJD, Problems M. Properties of mechanical endodontic instruments and the quality of the simulated canal preparation. Dent Med Probl. 2016;53(4):476–82.
Evans M, Davies JK, Sundqvist G, Figdor D. Mechanisms involved in the resistance of Enterococcus faecalis to calcium hydroxide. Int Endod J. 2002;35(3):221–8.
Turk BT, Sen BH, Ozturk T. In vitro antimicrobial activity of calcium hydroxide mixed with different vehicles against Enterococcus faecalis and Candida albicans. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(2):297–301.
Joy Sinha D, Garg P, Verma A, Malik V, Maccune ER, Vasudeva A. Dentinal tubule disinfection with propolis & two extracts of Azadirachta indica against Candida albicans biofilm formed on tooth substrate. Open Dent J. 2015;9:369–74.
Poptani B, Sharaff M, Archana G, Parekh V. Detection of Enterococcus faecalis and Candida albicans in previously root-filled teeth in a population of Gujarat with polymerase chain reaction. Contemp Clin Dent. 2013;4(1):62–6.
Siqueira JF Jr, Rocas IN. Polymerase chain reaction-based analysis of microorganisms associated with failed endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(1):85–94.
Bouillaguet S, Manoil D, Girard M, Louis J, Gaia N, Leo S, Schrenzel J, Lazarevic V. Root microbiota in primary and secondary apical periodontitis. Front Microbiol. 2018;9:2374.
Keskin C, Demiryurek EO, Onuk EE. Pyrosequencing analysis of cryogenically ground samples from primary and secondary/persistent endodontic infections. J Endod. 2017;43(8):1309–16.
Waltimo TM, Orstavik D, Siren EK, Haapasalo MP. In vitro susceptibility of Candida albicans to four disinfectants and their combinations. Int Endod J. 1999;32(6):421–9.
Basrani B, Tjaderhane L, Santos JM, Pascon E, Grad H, Lawrence HP, Friedman S. Efficacy of chlorhexidine- and calcium hydroxide-containing medicaments against Enterococcus faecalis in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):618–24.
Olitzky I. Antimicrobial properties of a propylene glycol based topical therapeutic agent. J Pharm Sci. 1965;54(5):787–8.
Goy RC, Britto D, Assis OBJP. A review of the antimicrobial activity of chitosan. Polímer Ciênc Tecnol. 2009;19:241–7.
Ercan E, Dalli M, Dulgergil CT. In vitro assessment of the effectiveness of chlorhexidine gel and calcium hydroxide paste with chlorhexidine against Enterococcus faecalis and Candida albicans. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(2):e27-31.
Guerreiro-Tanomaru JM, de Faria-Junior NB, Duarte MA, Ordinola-Zapata R, Graeff MS, Tanomaru-Filho M. Comparative analysis of Enterococcus faecalis biofilm formation on different substrates. J Endod. 2013;39(3):346–50.
Dezhurko-Korol VA, Novozhilova NE, Makeeva IM, Arkhipova AY, Moisenovich MM, Akhmadishina LV, Lukashev AN, Semenov AM, Leontieva MR, Byakova SF. The influence of centrifugation and inoculation time on the number, distribution, and viability of intratubular bacteria and surface biofilm in deciduous and permanent bovine dentin. Arch Oral Biol. 2020;114: 104716.
Wen C, Yan L, Kong Y, Zhao J, Li Y, Jiang Q. The antibacterial efficacy of photon-initiated photoacoustic streaming in root canals with different diameters or tapers. BMC Oral Health. 2021;21(1):542.
Lenherr P, Allgayer N, Weiger R, Filippi A, Attin T, Krastl G. Tooth discoloration induced by endodontic materials: a laboratory study. Int Endod J. 2012;45(10):942–9.
Nerwich A, Figdor D, Messer HH. pH changes in root dentin over a 4-week period following root canal dressing with calcium hydroxide. J Endod. 1993;19(6):302–6.
Martinho FC, Gomes CC, Nascimento GG, Gomes APM, Leite FRM. Clinical comparison of the effectiveness of 7- and 14-day intracanal medications in root canal disinfection and inflammatory cytokines. Clin Oral Investig. 2018;22(1):523–30.
Mustafa M, Alaajam WH, Azeim AA, Alfayi NA, Alqobty RM, Alghannam S. Diffusion of calcium hydroxide through dentinal tubules of retreated root canals: an in vitro study. Eur J Dent. 2018;12(3):386–92.
Acknowledgements
This work was supported by Ratchadaphiseksomphot Endowment Fund (Center of Excellence on Oral Microbiology and Immunology). We would like to thank members of the Center of Excellence for their kind assistance.
Funding
This project was supported by Ratchadaphiseksomphot Endowment Fund (to Center of Excellence on Oral Microbiology and Immunology), Chulalongkorn University.
Author information
Authors and Affiliations
Contributions
PT, AP, CR and OM conceptualized and designed the experiments. CA provided suggestions on material selection and preparations. PT performed experiments under supervision of OM and AP. PT and OM analyzed data and wrote the manuscript. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with Declaration of Helsinki and the proposal was approved by "The Human Research Ethics Committee of the Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand" (No.055/2020). Informed consent was waived because the donors of the extracted tooth samples were unidentifiable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Percentage of remaining viable CFU of E. faecalis and C. albicans relative to control in 3 independent experiments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thienngern, P., Panichuttra, A., Ratisoontorn, C. et al. Efficacy of chitosan paste as intracanal medication against Enterococcus faecalis and Candida albicans biofilm compared with calcium hydroxide in an in vitro root canal infection model. BMC Oral Health 22, 354 (2022). https://doi.org/10.1186/s12903-022-02385-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02385-x