Abstract
Background
Immediate loading has recently been introduced into unsplinted mandibular implant-retained overdentures for the management of edentulous patients due to their increasing demand on immediate aesthetics and function. However, there is still a scarcity of meta-analytical evidence on the efficacy of immediate loading compared to delayed loading in unsplinted mandibular implant-retained overdentures. The purpose of this study was to compare the marginal bone loss (MBL) around implants between immediate and delayed loading of unsplinted mandibular implant-retained overdentures.
Methods
Randomized controlled trials (RCTs), controlled clinical trials (CCTs), and cohort studies quantitatively comparing the MBL around implants between immediate loading protocol (ILP) and delayed loading protocol (DLP) of unsplinted mandibular overdentures were included. A systematic search was carried out in PubMed, EMBASE, and CENTRAL databases on December 02, 2020. “Grey” literature was also searched. A meta-analysis was conducted to compare the pooled MBL of two different loading protocols of unsplinted mandibular overdentures through weighted mean differences (WMDs) with 95% confidence intervals (95% CIs). The subgroup analysis was performed between different attachment types (i.e. Locator attachment vs. ball anchor). The risk of bias within and across studies were assessed using the Cochrane Collaboration’s tool, the Newcastle–Ottawa scale, and Egger’s test.
Results
Of 328 records, five RCTs and two cohort studies were included and evaluated, which totally contained 191 participants with 400 implants. The MBL of ILP group showed no significant difference with that of DLP group (WMD 0.04, CI − 0.13 to 0.21, P > .05). The subgroup analysis revealed similar results with Locator attachments or ball anchors (P > .05). Apart from one RCT (20%) with a high risk of bias, four RCTs (80%) showed a moderate risk of bias. Two prospective cohort studies were proved with acceptable quality. Seven included studies have reported 5.03% implant failure rate (10 of 199 implants) in ILP group and 1.00% failure rate (2 of 201 implants) in DLP group in total.
Conclusions
For unsplinted mandibular implant-retained overdentures, the MBL around implants after ILP seems comparable to that of implants after DLP. Immediate loading may be a promising alternative to delayed loading for the management of unsplinted mandibular implant-retained overdentures.
PROSPERO registration number: CRD42020159124.
Similar content being viewed by others
Background
The rehabilitation of edentulism has long been regarded as one of the main challenges for dentists. Conventional complete dentures may present some limitations such as insufficient retention and poor comfort, especially in the severely atrophic mandible [1]. With the wide application of osseointegrated implants, implant-retained overdentures have been introduced as a viable alternative to conventional complete dentures [2, 3]. In order to obtain adequate retention at a reasonable cost, the McGill Consensus Statement [4] recommended that the overdenture retained by two implants in anterior area of mandible could be the first-choice standard for edentulous patients. More recently, the York Consensus Statement [5] provided further clinical evidence that the use of no less than two implants could significantly enhance the retention of mandibular overdentures and the EAO consensus conference [6] also indicated that the oral health-related of life outcomes could be improved with overdentures retained by two or four implants. Little difference was observed between the average annual costs of overdentures retained by two implants and conventional complete dentures. Moreover, when unsplinted anchors are employed, the implant-retained overdentures could cost even less compared to their counterparts with splinted anchors [5]. Besides low costs, the unsplinted mandibular implant-retained overdentures display a low repair frequency and easy maintenance on isolated attachments, attracting more attention in the clinic [7]. Furthermore, the unsplinted overdentures provide good emergence profile and require simple oral hygiene practice in daily life [8]. Accordingly, unsplinted mandibular implant-retained overdentures with at least two implants have been frequently used in dental clinic [9,10,11].
Long-term outcomes of implant-retained overdentures are greatly affected by the longevity and functionality of the underlying implants, and the osseointegration is considered as the most important determinant of implant success [12]. To achieve osseointegration, Branemark et al. [13] suggested that sufficient healing time after implant insertion should be provided. Accordingly, a delayed loading protocol (DLP) was routinely performed, in which the prosthesis would be attached to the implants in the second stage after a healing period of three to six months [14, 15]. For a long time, it was assumed that enough healing time of DLP could not only decrease the risk of infection but also avoid the micromotion at the bone-implant interface that might lead to the implant failure [13, 16, 17]. However, along with lots of researches on intraosseous implant materials and implant surface modification techniques during the last two decades, predictable osseointegration could be achieved with obviously reduced healing time [18]. More importantly, optimized implant geometry designs and improved surgical techniques significantly enhanced the initial stability of dental implants [19, 20]. Therefore, the necessity of long healing period was challenged and the change of loading protocol was required to address the increasing demands of patients on the immediate aesthetics and function [21, 22]. Consequently, immediate loading protocol (ILP), in which the implants could be put in function within seven days after their placement [23], has been introduced into clinical practice [24]. But the prognosis of implants restored with ILP is yet to be further evaluated, especially regarding the promising unsplinted mandibular implant-retained overdentures.
Marginal bone loss (MBL), measured as the bone loss from the implant neck to the first bone-to-implant contact [25], is recognized as a crucial consideration for the attainment and maintenance of implant osseointegration [26]. In general, remodelling and resorption of peri-implant marginal bone could be observed after the implant surgery without bone augmentation technique. Therefore, MBL in the first year of loading was proposed as a criterion for implant success [27,28,29] and many studies have focused on the threshold between normal and pathological MBL. Papaspyridakos et al. [30] suggested that MBL of less than 1.5 mm in the first year was one of evaluation criteria for clinical implant success. Roos-Jansaker et al. [28] reported that MBL of less than 1.8 mm presented a reliable clinical outcome, while Naert et al. [31] believed that the maximal mean bone loss of 2.2 mm still indicated an acceptable long-term outcome. In spite of some discrepancies, MBL of 2 mm is wildly accepted as the maximum threshold of MBL in clinic situations, and is frequently used to evaluate the implant success as well as the extent of peri-implantitis [32, 33].
Several systematic reviews have focused on the effects of these two different loading protocols on MBL around implants in fixed and removable restorations [34, 35], while there was no meta-analytic review regarding the comparison between ILP and DLP in unsplinted mandibular overdentures. Some studies reported that implant-retained overdentures restored with ILP presented lower survival rates compared to those restored with DLP [36, 37], but others found that both ILP and DLP groups showed similar MBL with successful osseointegration [34, 38]. Therefore, it is still unknown whether ILP could provide acceptable MBL for the unsplinted mandibular implant-retained overdentures in the clinic.
Consequently, we quantitatively compared the effects of immediate and delayed loading protocols on MBL around implants for unsplinted mandibular implant-retained overdentures in this systematic review and meta-analysis, to inform dental practitioners about the selection of appropriate loading protocol for the long-term clinical success of restorations.
Methods
The present meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol was registered priori in the International Prospective Register of Systematic Reviews (PROSPERO) (www.crd.york.ac.uk/PROSPERO/) (registration number: CRD42020159124, Additional file 1, Details in Supplementary Information).
PICOS question
According to the recommendations of the Centre for Evidence-Based Medicine (University of Oxford, Oxford, UK), the PICOS (participants, interventions, comparisons, outcomes, and study designs) question was as follows: How is the effect on MBL around implants after ILP in the unsplinted mandibular implant-retained overdentures when compared to DLP?
Participants: edentulous patients restored with unsplinted mandibular implant-retained overdentures.
Intervention: ILP for unsplinted mandibular implant-retained overdentures.
Comparisons: DLP for unsplinted mandibular implant-retained overdentures.
Outcomes: MBL with a minimum follow-up of one year.
Study designs: randomized controlled trials (RCTs), controlled clinical trials (CCTs), and cohort studies.
Inclusion criteria
Based on the PICOS question, a study must fulfil the following inclusion criteria:
-
Clinical studies on human subjects only.
-
Studies with adults over 20 years of age who had mandibular edentulism restored by unsplinted implant-retained overdentures.
-
Studies with a minimum follow-up of 1 year.
-
Studies comparing the quantitative outcomes of MBL around implants in unsplinted mandibular implant-retained overdentures restored with ILP and DLP.
-
Studies with details of measuring techniques.
-
RCTs, CCTs, prospective and retrospective cohort studies.
-
Studies reported in English language only.
Exclusion criteria
In addition, if a study met any of the following exclusion criteria, it was excluded from the study:
-
Case reports, review papers.
-
Overdentures retained by a single implant only.
-
Diameter of implants narrower than 3 mm (mini-implant).
-
Duplicate studies based on the same patient cohorts.
-
Studies with sample size less than ten.
Information sources and literature search
The literature search was conducted independently by two independent assessors (W.L. and H.C.). Any disagreement was resolved by discussion between the two assessors. Three online electronic databases, including PubMed, EMBASE, and CENTRAL (Cochrane Library), were searched for relevant scientific reports published in the English language on December 02, 2020. No time filter was applied. The online search was conducted with the search strategy combining both the MeSH and free text words with high sensitivity and adaptation for the databases (Table 1). For the “grey” literature (e.g. unpublished and ongoing studies, conference abstracts, dissertation and thesis), the ClinicalTrials.gov, System for Information on Grey Literature in Europe (OpenGrey), National Technical Information Service (NTIS), and ProQuest Dissertation Abstracts, and Thesis databases were also searched. Furthermore, hand search was performed to identify the eligible reports based on the reference lists of related trials and reviews as a complement.
Study selection
After pooling the full search results from all database, literatures with repetitive contents were excluded. Two assessors (W.L. and H.C.) independently screened the titles and abstracts of studies, and irrelevant reports were discarded. Then the full-text evaluation of articles was carried out by the same two assessors to select reports that met all inclusion criteria as well as to exclude reports according to any of the exclusion criteria. Any disagreement about whether a study should be included was resolved by discussion or arbitrated by a third assessor (L.S.). In addition, the kappa statistic was used to measure agreement between the independent assessors.
Data collection and data items
The data were extracted from included reports and cross-checked by two assessors (W.L. and H.C.) independently. If there was a discrepancy on the data extraction during this process, the third assessor (L.S.) was consulted and an agreement was finally reached through a consensus discussion. A data collection form was developed a priori to record the extracted information. The following data were included: study, study design, total number of patients, age, edentulous region, number of implants (per patient), implant system, implant diameter, implant length, torque of implants, attachment type, comparison, number of patients in ILP/DLP, loading time of ILP/DLP, radiographic method, marginal bone loss, dropout (patient).
During the data extraction, it was found that one of the studies reported the mean and the standard deviation of vertical bone loss at four different sites (i.e. distal, labial, mesial, and lingual), while the other studies measured MBL at distal and mesial sites around the inserted implants. Thus, only the average values of MBL at distal and mesial sites in these studies were included in the following meta-analysis.
Risk of bias in individual trials
The risk of bias in the included RCTs were evaluated by the Cochrane Collaboration’s tool (RevMan v5.3) [39]. According to the bias indices, three different levels including low, moderate, and high were used to classify the risk of bias within RCTs [40]. The Newcastle–Ottawa scale (NOS), as an ordinal star-rating scale, was employed for the assessment of methodological quality of non-RCTs. In NOS, a higher score represented a higher report quality of cohort study [41]. The assessments were carried out by two independent assessors (W.L. and J.Z.). Any disagreements were discussed and resolved until consensus was reached.
Summary measures and synthesis of results
Statistical analyses were performed via the RevMan (RevMan v5.3, Cochrane Collaboration) and Stata (Stata MP v14, StataCorp LP) software. To compare MBL of ILP group with DLP group, the weighted mean differences (WMDs) with 95% confidence intervals (95% CIs) for these continuous outcomes was calculated. The results were provided with a fixed-effect or random-effects model [42]. Statistical heterogeneity was measured by the Chi2 statistic and I2 statistic [40].
Risk of bias across studies
When there are at least 10 studies included in the present meta-analysis, tests for funnel plot asymmetry was drawn. Otherwise, Egger’s test was employed to assess the publication bias [40, 43].
Additional analyses
The subgroup analysis was carried out among different attachment types of unsplinted mandibular implant-retained overdentures including Locator attachments, ball anchors and magnetic attachments, in order to reveal whether the overall estimate effect would be influenced by different attachment types. Sensitivity analyses were performed by removing individual trials from the meta-analysis, to see whether the overall effect would be affected and thus to reveal the robustness of the results.
Results
Study selection
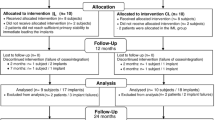
Six hundred and seventeen and six records were identified through database search and hand search respectively. Through removal of repetitive records and initial screening by titles and abstracts, 34 records remained. After full-text review, 27 studies were excluded as they did not meet the eligibility criteria and a total of seven articles were included for this review and meta-analysis (Fig. 1).
The kappa value for the inter-investigator agreement of initial screening by titles and abstracts was 0.96 and that of full-text evaluation was 0.91, both presented an “almost perfect” inter-agreement [44].
Study characteristics
Table 2 showed the characteristics of the included seven studies. All studies were published from 2007 to 2020, and 191 recruited participants with 400 implants were included all together. Among these seven studies, five (71%) were RCTs and two (29%) were prospective cohort studies. In six studies [45,46,47,48,49,50], overdentures in ILP groups were attached to the implants immediately after implantation, while in the other one study, the restorations in the ILP group were performed seven days after the surgery [51]. In DLP groups of all included studies [45,46,47,48,49,50,51], the healing time after implant surgery was no less than three months. Four studies [45,46,47,48] disclosed the specific ranges of inserting torque, and the other three studies [49,50,51] did not report the insertion torque. Moreover, Locator attachments were employed in three studies [45, 47, 48] and ball anchors were utilized in the other four literatures [46, 49,50,51]. In regard to “implants failed (at 12 months, implants)”, no implant failure was reported in ILP and DLP groups of three included studies [45, 46, 51]. Three studies [47,48,49] reported two implant failures occurring in ILP group and no implant failure in DLP group each. One study [50] revealed four implants failures in ILP group and two implant failures in DLP group. Thus, ILP group demonstrated a higher implant failure rate of 5.03% (10 of 199 implants), compared with 1.00% failure rate (2 of 201 implants) in DLP group.
Risk of bias within studies
Figure 2 illustrated the quality assessments and risk of bias of the included RCTs. Four RCTs [45, 46, 48, 49] were of unclear risk of bias while one study [47] included a high risk of bias. Two RCTs had a low risk of selection bias and three RCTs did not provide detailed information in terms of random sequence generation or allocation concealment. Only one RCT [47] (20%) reported a high risk of performance bias as only one experienced operator performed all the surgeries in ILP group and DLP group. Three studies [46,47,48], which did not provide enough information about the binding of outcome assessment, had an unclear risk of detection bias. All studies reported low risk of attrition bias with no missing data [45, 46, 49] or reasonable explanations for only one missing data [47, 48]. The reporting bias was classified at an unclear level in 80% of the trials [45, 46, 48, 49], for insufficient information was available to judge the risk level. These studies appeared to be free of other sources of bias. Table 3 presented the quality assessment results of two prospective cohort studies [50, 51]. The overall risk of bias was deemed to be low (seven stars) in the two cohort studies, and these studies were proved to be of an acceptable quality [41, 52, 53]. As the two studies did not report the derivation of the cohorts, it was unclear to judge the representativeness of their exposed cohorts. Though two subjects of one study [50] lost to follow up, the description of those lost was provided in detail and then the adequacy of follow up was considered with low risk of bias.
Quality assessment and risk of bias of the included RCTs assessed by review authors with the RevMan v.5.3 software: a risk of bias summary showing review authors' judgments about risk of bias items for each included RCT; b risk of bias graph showing review authors' judgments about each item's risk of bias presented as percentages for all included RCTs
Results of individual studies and synthesis of data
In this review, 191 patients with a follow-up of no less than 12 months were pooled for the synthesis of data and the meta-analysis result of seven studies was illustrated with the forest plot (Fig. 3). As a result of the comparison of MBL between ILP and DLP groups, a substantial heterogeneity [39] (P = 0.04, I2 = 55.06% > 50%) was found. Therefore, instead of the fixed-effect model, DerSimonian–Laird model as a random-effect model was applied according to the STATA technical bulletin and Cochrane handbook [40, 54]. No statistically significant difference of MBL was detected (WMD 0.04, CI − 0.13 to 0.21, P = 0.68) between ILP and DLP group.
Risk of bias across studies
Because the limited number of included studies (n < 10), the publication bias assessment was conducted with Egger’s test in the current meta-analysis. The result of Egger’s test indicated that no significant bias could be found among seven included studies (P > 0.05). Nevertheless, this evaluation of risk of publication bias should be considered as a reference only owing to the limited quantity of articles.
Additional analysis
According to the different attachments applied in these studies, two subgroups (i.e. Locator attachment vs. ball anchor) were set. Figure 4 showed the comparison of average MBL in the subgroups respectively. In either the Locator attachments (three trials, WMD − 0.08, CI − 0.50 to 0.34, P > 0.05) or the ball anchors (four trials, WMD 0.05, CI − 0.15 to 0.25, P > 0.05) subgroup, no significant difference was detected between ILP and DLP. In the sensitivity analyses, one single study was deleted from the overall pooled analysis each time and it was found that the exclusion of individual studies did not show any influence on the overall MBL (Fig. 5). Moreover, with the omission of two prospective studies, there was still no significant difference between ILP and DLP groups (WMD − 0.02, CI − 0.23 to 0.19, P > 0.05).
Discussion
The present systematic review was based on the results from five RCTs and two non-RCTs with a total of 191 patients. The meta-analysis was conducted to compare the MBL around inserted implants of unsplinted mandibular overdentures between ILP and DLP groups, and the result did not reveal any significant difference (P > 0.05). Further, the subgroup analysis showed similar results about the MBL between the two different loading protocols in either the Locator attachments or the ball anchors subgroup (P > 0.05), suggesting that different attachment types employed in the included studies did not result in any difference on the result of meta-analysis, and might not be the source of cross-study heterogeneity. Additionally, in both ILP and DLP groups of these included studies, the average MBL surrounding implants of unsplinted implant-retained overdentures were lower than 2 mm, indicating that the results were all clinically acceptable as far as MBL was concerned [32].
Several studies reported that the initial healing of implants with immediately loaded mandibular overdentures might be impaired by the resultant restoration movement, immediate abutment connection, and early contact with oral microbial plaque [55,56,57]. However, the present meta-analysis reported no detectable difference in the MBL around immediately loaded implants compared to the DLP group, which is also in line with the evidence from some previous systematic reviews [34, 58]. This may be attributed to the early mechanical strain and a lack of the second-stage surgery in ILP [59,60,61]. Mechanical loading from the overdentures in ILP might act as a stimulator to alveolar bone formation and then lead to high bone fractions [61]. The early mechanical strain in the bone-to-implant contact surface was found to have a positive effect on the initial phase of bone healing [59, 60]. Moreover, second-stage surgical operations could bring additional trauma and damage tissues, leading to marginal bone loss [62, 63]. DLP with a second-stage surgery might be accompanied by the loss of underlying bone around implants compared with ILP [64]. Noticeably, Sanz-Sanchez et al. [25] and Kern et al. [65] synthesised both the fixed implant-supported and removal implant-retained restorations and reported that the ILP group presented an even less MBL compared to DLP group. This result may due to the combined discussion of fixed implant-supported and removal implant-retained restorations. The early mechanical strain from fixed dentures is usually much higher than that from removable restorations, thus the positive effect of immediate loading on MBL [61] is supposed to be more obvious.
Besides different loading protocols, marginal bone level could also be influenced by some factors such as implant primary stability and alveolar bone condition. In seven included studies, the effect of these factors on the MBL has been carefully controlled. The insertion torque value and implant stability quotient (ISQ) in these studies revealed clinically acceptable micromotion of implants [18, 66], and all implants sites of included cases were the alveolar bone of anterior mandible which was considered with the highest bone density compared to the alveolar bone of other oral regions [67]. Therefore, the primary stability, as an essential prerequisite for implant success, met the implant loading requirement for both ILP and DLP.
In this review, the early loading protocol, in which implants were put in function between one week and two months after placement [23], was not discussed, for this loading protocol could not reduce healing time significantly compared with ILP, whereas would increase the period with low masticate efficiency, and is seldom applied on the implant-retained overdentures in the clinic.
Apart from MBL around implants, the dropouts of patients as well as the implant failures were reported in these included studies. Patient dropouts commonly occur in long-term studies, due to death, illness, leaving the city, or many other reasons, it was considered as a quality index of RCT rather than a parameter of clinical outcomes, while the implant failure is commonly recognized as a key index for prognosis of implant treatment [68]. Therefore, in the current meta-analysis, only the data of implant failure was extracted from the included studies. MBL is triggered by multiple factors, such as gender, age, bone density, and type of connection. And the definition of implant failure requires the assessment of these features of each implant and patient [69]. Hence, given the crucial role of MBL in the prognosis of long-term implant failure, all possible efforts should be employed to decrease the MBL around implants and build a strict follow-up maintenance program. In this meta-analysis, the MBL at the first year of loading was chosen as the main outcome and the early implant failures of included studies occurring in the first 12 months were also reported (Table 2). Since three included studies [49,50,51] here did not report specific values of inserted torque in the implant surgery which had an obvious impact on the early survival rate of implants [70], a robust conclusion about implant success could not be drawn in this review. Therefore, this index was not taken into consideration in this present meta-analysis.
MBL was employed as the only criterion to evaluate the therapeutic effects of immediate and delayed loading protocols in this study. However, this parameter indeed has its drawback. The raw MBL data at 1-year post-loading is a static index and it could only present the status of peri-implant tissue at one single time point, thus the reliability of MBL is controversial. Accordingly, the rate of MBL as a new index was proposed by Galindo-Moreno et al. recently [69]. As remodelling of marginal bone is a dynamic process, the rate of MBL is calculated in millimetre/month (mm/m) and could change over time [69, 71]. Galindo-Moreno et al. [69] found that the progression of MBL tends to be higher and the risk of implant failure could be significantly increased when the rates of MBL was higher than 0.44 mm at six months post-loading. The new index may better help dentists predict future bone changes in the early stage and then establish a strict maintenance recall for patients. Meanwhile, a more definite evaluation of clinical outcomes between these two different loading protocols could be carried out in a short observation time rather than a minimum follow-up of one year. Thus, the rate of MBL might be a more suitable criterion for implant success in the clinic.
This was the first study to systemically evaluate the MBL of immediate loading compared to delayed loading in unsplinted mandibular implant-retained overdentures. The protocol of this study was registered in PROSPERO in advance and performed strictly in accordance with PRISMA guidelines. Apart from online search, manual search was performed based on the references of selected studies and related reviews, in order to discover qualified trials which might not be included in the databases. Therefore, compared with individual studies, it is a more convincing clinical suggestion of loading protocol selection of unspinted mandibular implant-retained overdentures to practitioners. However, there are some limitations of this study. The implant number and implant system in the included studies had not achieved complete consistency, which might cause the considerable heterogeneity in the meta-analysis. Additionally, only seven clinical trials were included and two of them were prospective cohort studies. Due to the limited number of the trials, the results of this study might lack sufficient evidence. Moreover, although the result of meta-analysis after removing two included prospective studies [50, 51] remained the same, the validity of analysis might also be slightly compromised since no randomization of participant allocation could be employed in cohort studies. Thus, further high-quality, well-designed RCTs with large sample size are required to appraise the efficacy of different loading protocols on MBL around implants in unsplinted mandibular implant-retained overdentures.
Conclusions
Based on the results of this systematic review and meta-analysis, the MBL around implants restored with ILP showed no significant difference with that of implants restored with DLP for unsplinted mandibular implant-retained overdentures. The subgroup analysis suggested that either the Locator attachments or the ball anchors employed in the included studies would not result in any difference on the result of meta-analysis. However, considerable heterogeneity was observed across the included studies. Also, the limited number of trails and no randomization of participant allocation in the included cohort studies might compromise the validity of analysis. Further high-quality RCTs with robust study design and large sample size are needed to strengthen the evidence base and identify the effect of immediate and delayed loading protocols on MBL around implants in unsplinted mandibular implant-retained overdentures.
Availability of data and materials
We declared that the datasets used and/or analyzed in the manuscript, including all relevant raw data, are available from the corresponding author on reasonable request.
Abbreviations
- MBL:
-
Marginal bone loss
- RCTs:
-
Randomized controlled trials
- CCTs:
-
Controlled clinical trials
- ILP:
-
Immediate loading protocol
- DLP:
-
Delayed loading protocol
- WMDs:
-
Weighted mean differences
- CIs:
-
Confidence intervals
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- PICOS:
-
Participants, interventions, comparisons, outcomes, and study designs
- NOS:
-
Newcastle–Ottawa scale
- ISQ:
-
Implant stability quotient
References
Geckili O, Bilhan H, Mumcu E, Dayan C, Yabul A, Tuncer N. Comparison of patient satisfaction, quality of life, and bite force between elderly edentulous patients wearing mandibular two implant-supported overdentures and conventional complete dentures after 4 years. Spec Care Dentist. 2012;32(4):136–41. https://doi.org/10.1111/j.1754-4505.2012.00258.x.
Hobkirk JA, Abdel-Latif HH, Howlett J, Welfare R, Moles DR. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-stabilized complete mandibular dentures: a case-control study (part 2). Int J Prosthodont. 2009;22(1):13–9.
Hasegawa T, Kawabata S, Takeda D, Iwata E, Saito I, Arimoto S, et al. Survival of Brånemark System Mk III implants and analysis of risk factors associated with implant failure. Int J Oral Maxillofac Surg. 2017;46(2):267–73. https://doi.org/10.1016/j.ijom.2016.10.014.
Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, et al. The McGill consensus statement on overdentures. Montreal, Quebec Canada. Int J Prosthodont. 2002;15(4):413–4.
Thomason JM, Feine J, Exley C, Moynihan P, Müller F, Naert I, et al. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients—the York Consensus Statement. Br Dent J. 2009;207(4):185–6. https://doi.org/10.1038/sj.bdj.2009.728.
Beikler T, Flemmig TF. EAO consensus conference: economic evaluation of implant-supported prostheses. Clin Oral Implants Res. 2015;26(Suppl 11):57–63. https://doi.org/10.1111/clr.12630.
Kleis WK, Kämmerer PW, Hartmann S, Al-Nawas B, Wagner W. A comparison of three different attachment systems for mandibular two-implant overdentures: one-year report. Clin Implant Dent Relat Res. 2010;12(3):209–18. https://doi.org/10.1111/j.1708-8208.2009.00154.x.
de Souza Batista VE, Verri FR, Lemos CAA, Cruz RS, Oliveira HFF, Gomes JML, et al. Should the restoration of adjacent implants be splinted or nonsplinted? A systematic review and meta-analysis. J Prosthet Dent. 2019;121(1):41–51. https://doi.org/10.1016/j.prosdent.2018.03.004.
Carlsson GE, Kronström M, de Baat C, Cune M, Davis D, Garefis P, et al. A survey of the use of mandibular implant overdentures in 10 countries. Int J Prosthodont. 2004;17(2):211–7.
Naert I, Alsaadi G, Quirynen M. Prosthetic aspects and patient satisfaction with two-implant-retained mandibular overdentures: a 10-year randomized clinical study. Int J Prosthodont. 2004;17(4):401–10.
Timmerman R, Stoker GT, Wismeijer D, Oosterveld P, Vermeeren JI, van Waas MA. An eight-year follow-up to a randomized clinical trial of participant satisfaction with three types of mandibular implant-retained overdentures. J Dent Res. 2004;83(8):630–3. https://doi.org/10.1177/154405910408300809.
Albrektsson T, Jacobsson M. Bone–metal interface in osseointegration. J Prosthet Dent. 1987;57(5):597–607. https://doi.org/10.1016/0022-3913(87)90344-1.
Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lundkvist S, Rockler B. Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials. 1983;4(1):25–8. https://doi.org/10.1016/0142-9612(83)90065-0.
Schatzker J, Horne JG, Sumner-Smith G. The effect of movement on the holding power of screws in bone. Clin Orthop Relat Res. 1975;111:257–62. https://doi.org/10.1097/00003086-197509000-00032.
Cochran DL, Morton D, Weber HP. Consensus statements and recommended clinical procedures regarding loading protocols for endosseous dental implants. Int J Oral Maxillofac Implants. 2004;19(Suppl):109–13.
Chiapasco M, Gatti C. Implant-retained mandibular overdentures with immediate loading: a 3- to 8-year prospective study on 328 implants. Clin Implant Dent Relat Res. 2003;5(1):29–38. https://doi.org/10.1111/j.1708-8208.2003.tb00179.x.
Roberts WE, Smith RK, Zilberman Y, Mozsary PG, Smith RS. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984;86(2):95–111. https://doi.org/10.1016/0002-9416(84)90301-4.
Cannizzaro G, Leone M, Esposito M. Immediate functional loading of implants placed with flapless surgery in the edentulous maxilla: 1-year follow-up of a single cohort study. Int J Oral Maxillofac Implants. 2007;22(1):87–95.
Akkocaoglu M, Uysal S, Tekdemir I, Akca K, Cehreli MC. Implant design and intraosseous stability of immediately placed implants: a human cadaver study. Clin Oral Implants Res. 2005;16(2):202–9. https://doi.org/10.1111/j.1600-0501.2004.01099.x.
Fanuscu MI, Chang TL, Akça K. Effect of surgical techniques on primary implant stability and peri-implant bone. J Oral Maxillofac Surg. 2007;65(12):2487–91. https://doi.org/10.1016/j.joms.2007.04.017.
Borges TF, Mendes FA, de Oliveira TR, Gomes VL, do Prado CJ, das Neves FD. Mandibular overdentures with immediate loading: satisfaction and quality of life. Int J Prosthodont. 2011;24(6):534–9.
Erkapers M, Ekstrand K, Baer RA, Toljanic JA, Thor A. Patient satisfaction following dental implant treatment with immediate loading in the edentulous atrophic maxilla. Int J Oral Maxillofac Implants. 2011;26(2):356–64.
Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22(6):893–904.
Goiato MC, Bannwart LC, Pesqueira AA, Santos DM, Haddad MF, Santos MR, et al. Immediate loading of overdentures: systematic review. Oral Maxillofac Surg. 2014;18(3):259–64. https://doi.org/10.1007/s10006-013-0421-6.
Sanz-Sánchez I, Sanz-Martín I, Figuero E, Sanz M. Clinical efficacy of immediate implant loading protocols compared to conventional loading depending on the type of the restoration: a systematic review. Clin Oral Implants Res. 2015;26(8):964–82. https://doi.org/10.1111/clr.12428.
Zarb GA, Albrektsson T. Consensus report: towards optimized treatment outcomes for dental implants. J Prosthet Dent. 1998;80(6):641. https://doi.org/10.1016/s0022-3913(98)70048-4.
Koutsonikos A. Implants: success and failure—a literature review. Ann R Australas Coll Dent Surg. 1998;14:75–80.
Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part II: presence of peri-implant lesions. J Clin Periodontol. 2006;33(4):290–5. https://doi.org/10.1111/j.1600-051X.2006.00906.x.
Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546–9. https://doi.org/10.1902/jop.2000.71.4.546.
Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012;91(3):242–8. https://doi.org/10.1177/0022034511431252.
Naert I, Duyck J, Hosny M, Jacobs R, Quirynen M, van Steenberghe D. Evaluation of factors influencing the marginal bone stability around implants in the treatment of partial edentulism. Clin Implant Dent Relat Res. 2001;3(1):30–8. https://doi.org/10.1111/j.1708-8208.2001.tb00126.x.
Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, et al. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008;17(1):5–15. https://doi.org/10.1097/ID.0b013e3181676059.
Kline R, Hoar JE, Beck GH, Hazen R, Resnik RR, Crawford EA. A prospective multicenter clinical investigation of a bone quality-based dental implant system. Implant Dent. 2002;11(3):224–34. https://doi.org/10.1097/00008505-200207000-00006.
Esposito M, Grusovin MG, Maghaireh H, Worthington HV. Cochrane Database Syst Rev. 2013;3:Cd003878. https://doi.org/10.1002/14651858.CD003878.pub5.
Chen J, Cai M, Yang J, Aldhohrah T, Wang Y. Immediate versus early or conventional loading dental implants with fixed prostheses: a systematic review and meta-analysis of randomized controlled clinical trials. J Prosthet Dent. 2019;122(6):516–36. https://doi.org/10.1016/j.prosdent.2019.05.013.
van Steenberghe D, Molly L, Jacobs R, Vandekerckhove B, Quirynen M, Naert I. The immediate rehabilitation by means of a ready-made final fixed prosthesis in the edentulous mandible: a 1-year follow-up study on 50 consecutive patients. Clin Oral Implants Res. 2004;15(3):360–5. https://doi.org/10.1111/j.1600-0501.2004.01069.x.
De Bruyn H, Raes S, Ostman PO, Cosyn J. Immediate loading in partially and completely edentulous jaws: a review of the literature with clinical guidelines. Periodontol 2000. 2014;66(1):153–87. https://doi.org/10.1111/prd.12040.
Chrcanovic BR, Albrektsson T, Wennerberg A. Immediately loaded non-submerged versus delayed loaded submerged dental implants: a meta-analysis. Int J Oral Maxillofac Surg. 2015;44(4):493–506. https://doi.org/10.1016/j.ijom.2014.11.011.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011. https://doi.org/10.1136/bmj.d5928.
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ and Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated August 2019). Cochrane. 2019.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Borenstein M, Hedges L, Higgins JPT, Rothstein HR. Fixed-effect versus random-effects models. In: Borenstein M, Hedges LV, Higgins JPT, Rothstein HR, editors. Introduction to meta-analysis. Hoboken: Wiley; 2009. p. 77–86. https://doi.org/10.1002/9780470743386.ch13.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Kutkut A, Rezk M, Zephyr D, Dawson D, Frazer R, Al-Sabbagh M. Immediate loading of unsplinted implant retained mandibular overdenture: a randomized controlled clinical study. J Oral Implantol. 2019;45(5):378–89. https://doi.org/10.1563/aaid-joi-D-18-00202.
Aunmeungtong W, Kumchai T, Strietzel FP, Reichart PA, Khongkhunthian P. Comparative clinical study of conventional dental implants and mini dental implants for mandibular overdentures: a randomized clinical trial. Clin Implant Dent Relat Res. 2017;19(2):328–40. https://doi.org/10.1111/cid.12461.
Schincaglia GP, Rubin S, Thacker S, Dhingra A, Trombelli L, Ioannidou E. Marginal bone response around immediate- and delayed-loading implants supporting a locator-retained mandibular overdenture: a randomized controlled study. Int J Oral Maxillofac Implants. 2016;31(2):448–58. https://doi.org/10.11607/jomi.4118.
Elsyad MA, Elsaih EA, Khairallah AS. Marginal bone resorption around immediate and delayed loaded implants supporting a locator-retained mandibular overdenture. A 1-year randomised controlled trial. J Oral Rehabil. 2014;41(8):608–18. https://doi.org/10.1111/joor.12182.
Elsyad MA, Al-Mahdy YF, Fouad MM. Marginal bone loss adjacent to conventional and immediate loaded two implants supporting a ball-retained mandibular overdenture: a 3-year randomized clinical trial. Clin Oral Implants Res. 2012;23(4):496–503. https://doi.org/10.1111/j.1600-0501.2011.02173.x.
De Smet E, Duyck J, Vander Sloten J, Jacobs R, Naert I. Timing of loading–immediate, early, or delayed–in the outcome of implants in the edentulous mandible: a prospective clinical trial. Int J Oral Maxillofac Implants. 2007;22(4):580–94.
Turkyilmaz I, Tozum TF, Fuhrmann DM, Tumer C. Seven-year follow-up results of TiUnite implants supporting mandibular overdentures: early versus delayed loading. Clin Implant Dent Relat Res. 2012;14(Suppl 1):e83-90. https://doi.org/10.1111/j.1708-8208.2011.00365.x.
Aziz O, Constantinides V, Tekkis PP, Athanasiou T, Purkayastha S, Paraskeva P, et al. Laparoscopic versus open surgery for rectal cancer: a meta-analysis. Ann Surg Oncol. 2006;13(3):413–24. https://doi.org/10.1245/aso.2006.05.045.
Wei Y, Xu G, Zhang G, Wen C, Anwar F, Wang S, et al. Antigenic evolution of H9N2 chicken influenza viruses isolated in China during 2009–2013 and selection of a candidate vaccine strain with broad cross-reactivity. Vet Microbiol. 2016;182:1–7. https://doi.org/10.1016/j.vetmic.2015.10.031.
Newton HJ. sbe24. metan—an alternative meta-analysis command. Stata Technical Bulletin, p. 4–14. 1998.
Alfadda SA, Attard NJ, David LA. Five-year clinical results of immediately loaded dental implants using mandibular overdentures. Int J Prosthodont. 2009;22(4):368–73.
Celik G, Uludag B. Photoelastic stress analysis of various retention mechanisms on 3-implant-retained mandibular overdentures. J Prosthet Dent. 2007;97(4):229–35. https://doi.org/10.1016/j.prosdent.2007.02.006.
Naert I, Gizani S, van Steenberghe D. Bone behavior around sleeping and non-sleeping implants retaining a mandibular hinging overdenture. Clin Oral Implants Res. 1999;10(2):149–54. https://doi.org/10.1034/j.1600-0501.1999.100209.x.
Helmy MHE, Alqutaibi AY, El-Ella AA, Shawky AF. Effect of implant loading protocols on failure and marginal bone loss with unsplinted two-implant-supported mandibular overdentures: systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2018;47(5):642–50. https://doi.org/10.1016/j.ijom.2017.10.018.
Qi MC, Zou SJ, Han LC, Zhou HX, Hu J. Expression of bone-related genes in bone marrow MSCs after cyclic mechanical strain: implications for distraction osteogenesis. Int J Oral Sci. 2009;1(3):143–50. https://doi.org/10.4248/ijos.09021.
Vandamme K, Naert I, Geris L, Sloten JV, Puers R, Duyck J. Histodynamics of bone tissue formation around immediately loaded cylindrical implants in the rabbit. Clin Oral Implants Res. 2007;18(4):471–80. https://doi.org/10.1111/j.1600-0501.2007.01339.x.
Duyck J, Slaets E, Sasaguri K, Vandamme K, Naert I. Effect of intermittent loading and surface roughness on peri-implant bone formation in a bone chamber model. J Clin Periodontol. 2007;34(11):998–1006. https://doi.org/10.1111/j.1600-051X.2007.01135.x.
Tal H, Artzi Z, Moses O, Nemcovsky CE, Kozlovsky A. Spontaneous early exposure of submerged endosseous implants resulting in crestal bone loss: a clinical evaluation between stage I and stage II surgery. Int J Oral Maxillofac Implants. 2001;16(4):514–21.
Randow K, Ericsson I, Nilner K, Petersson A, Glantz PO. Immediate functional loading of Brånemark dental implants. An 18-month clinical follow-up study. Clin Oral Implants Res. 1999;10(1):8–15. https://doi.org/10.1034/j.1600-0501.1999.100102.x.
Assad AS, Hassan SA, Shawky YM, Badawy MM. Clinical and radiographic evaluation of implant-retained mandibular overdentures with immediate loading. Implant Dent. 2007;16(2):212–23. https://doi.org/10.1097/ID.0b013e318065a95f.
Kern JS, Kern T, Wolfart S, Heussen N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res. 2016;27(2):174–95. https://doi.org/10.1111/clr.12531.
Nkenke E, Fenner M. Indications for immediate loading of implants and implant success. Clin Oral Implants Res. 2006;17(Suppl 2):19–34. https://doi.org/10.1111/j.1600-0501.2006.01348.x.
Li FB, Yu LY, Cai YD, Xie C. Jaw bone density assessments of implant sites using spiral CT and Simplant software. Shanghai Kou Qiang Yi Xue. 2009;18(1):52–5.
Salman A, Thacker S, Rubin S, Dhingra A, Ioannidou E, Schincaglia GP. Immediate versus delayed loading of mandibular implant-retained overdentures: a 60-month follow-up of a randomized clinical trial. J Clin Periodontol. 2019;46(8):863–71. https://doi.org/10.1111/jcpe.13153.
Galindo-Moreno P, León-Cano A, Ortega-Oller I, Monje A, O’Valle F, Catena A. Marginal bone loss as success criterion in implant dentistry: beyond 2 mm. Clin Oral Implants Res. 2015;26(4):e28–34. https://doi.org/10.1111/clr.12324.
Ntounis A, Petropoulou A. A technique for managing and accurate registration of periimplant soft tissues. J Prosthet Dent. 2010;104(4):276–9. https://doi.org/10.1016/s0022-3913(10)60139-4.
Acharya A, Leung MCT, Ng KT, Fan MHM, Fokas G, Mattheos N. Peri-implant marginal bone loss rate pre- and post-loading: an exploratory analysis of associated factors. Clin Oral Implants Res. 2019;30(5):410–9. https://doi.org/10.1111/clr.13424.
Acknowledgements
The authors thank Huidi Ren and Xin Zhang for their support and help during this study.
Funding
This study was supported by the National Natural Science Foundation of China (NSFC) [grant number 81970958]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
WL contributed to study planning, article selection, data collection, data analysis and interpretation, and writing and revising the manuscript. HC contributed to study planning, article selection, data collection, data analysis and interpretation, and writing and revising the manuscript. JZ contributed to data analysis such as risk of bias with studies, drafting and revising the manuscript. JW contributed to study planning, drafting and revising the manuscript. LS contributed to conception of the study, study planning, article selection, data interpretation, and revising the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. The PROSPERO protocol of this systematic review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, W., Cai, H., Zhang, J. et al. Effects of immediate and delayed loading protocols on marginal bone loss around implants in unsplinted mandibular implant-retained overdentures: a systematic review and meta-analysis. BMC Oral Health 21, 122 (2021). https://doi.org/10.1186/s12903-021-01486-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-021-01486-3