Abstract
Background
Many Australian adults are not receiving timely or effective diabetes management to prevent or delay the onset of diabetes related complications. Integrated care, a worldwide trend in healthcare reform, aims to reduce the fragmented delivery of health services and improve outcomes. This study aimed to test whether a specialist-led integrated model of care provided to a small subset of patients in general practices leads to spillover clinical improvements in all patients of the practice with type 2 diabetes.
Methods
Seventy-two general practice sites (clusters) in New South Wales, Australia received the Diabetes Alliance intervention, creating a non-randomised open cohort stepped wedge trial. The intervention comprised of case conferencing, delivered directly to a small proportion of adults with type 2 diabetes (n = 1,072) of the general practice sites; as well as practice feedback, education and training. Spillover clinical improvements were assessed on all adults with type 2 diabetes within the general practice sites (n = 22,706), using practice level data recorded in the MedicineInsight electronic database, compared before and after the intervention. Outcome measures included frequency of diabetes screening tests in line with the Annual Cycle of Care, and clinical results for weight, blood pressure, HbA1c, lipids, and kidney function.
Results
Compared to before Diabetes Alliance, the odds of all practice patients receiving screening tests at or above the recommended intervals were significantly higher for all recommended tests after Diabetes Alliance (odds ratio range 1.41–4.45, p < 0.0001). Significant improvements in clinical outcomes were observed for weight (absolute mean difference: -1.38 kg), blood pressure (systolic − 1.12 mmHg, diastolic − 1.18 mmHg), HbA1c (-0.03% at the mean), total cholesterol (-0.11 mmol/L), and triglycerides (-0.02 mmol/L) (p < 0.05). There were small but significant declines in kidney function.
Conclusions
Integrated care delivered to a small subset of patients with type 2 diabetes across a large geographic region has spillover benefits that improve the process measures and clinical outcomes for all practice patients with type 2 diabetes.
Trial registration
ACTRN12622001438741; 10th November 2022, retrospectively registered: https://www.anzctr.org.au/ACTRN12622001438741.aspx.
Similar content being viewed by others
Background
Half a billion people are living with diabetes mellitus worldwide, with projections of a 50% increase by 2045 [1]. Type 2 diabetes constitutes approximately 90% of all cases of diabetes [1]. In Australia, type 2 diabetes is the 12th largest contributor to the burden of disease, affecting 5.3% of adults [2, 3]. However, 65% of cardiovascular deaths in Australia occur in people with diabetes or prediabetes [4]. The prevalence of type 2 diabetes is also substantially underdiagnosed [5], masking the true burden of disease [6].
For over a decade the International Diabetes Federation has recommended an annual review of type 2 diabetes control and complications, an agreed and updated diabetes care plan, and involvement of a multidisciplinary team in delivering that plan, centred around the person [7]. In Australia, the Annual Cycle of Care provides minimum standards for diabetes care, including routine tests and measurements (usually at six or 12 monthly intervals) to identify problems early with the intention of reducing diabetes-related complications [8]. Interventions that improve glycaemia, blood pressure, and lipids have been shown to reduce the risk of premature mortality and cardiovascular disease [9]. The Annual Cycle of Care is intended to be delivered by general practitioners (GP) and other diabetes specialists, based on recommendations outlined in the Management of type 2 diabetes: A handbook for general practice [10]. Sainsbury et al. (2018) have reviewed existing evidence to determine what proportion of people with diabetes in Australia receive the Annual Cycle of Care [9]. From the four identified studies, completion rates ranged from 0.9% in an Indigenous population to 37% over a 12 to 18-month period in non-Indigenous people [9]. Sainsbury et al. (2018) also identified 31 studies investigating the proportion of people meeting the HbA1c target of ≤ 7.0%, finding an overall mean of 53% (range 13–79%) [9]. These findings highlight the need for services that focus on better implementation of the minimum standards of care for diabetes, with evaluation of the clinical outcomes [11].
The Diabetes Alliance commenced in 2015, delivering an integrated model of care that provides access to tertiary specialist services within the general practice (or primary care) setting [12]. The Diabetes Alliance was initially piloted across 20 general practices within Hunter New England Local Health District (HNELHD), Australia [12] and has since been implemented on a larger scale involving 120 practices. While Diabetes Alliance has been shown to be effective in enhancing adherence to the Annual Cycle of Care and improving glycaemic control for those who receive the specialist-led case conferencing [12], the question remained whether the learning and knowledge from Diabetes Alliance was transferred and applied by the GPs to their other patients with diabetes, in epidemiological terms a spillover effect [13]. Therefore, this study aimed to evaluate the spillover effect of the Diabetes Alliance on diabetes care for patients with type 2 diabetes seen in the general practice setting.
Methods
Study design
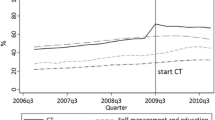
This is a non-randomised open cohort stepped-wedge trial comparing clinical and process outcomes before and after Diabetes Alliance (also referred to as the intervention). The trial was prospectively registered with the Australian New Zealand Clinical Trials Registry on 10/11/2022 (ACTRN12622001438741) [14]. Between 2015 and 2019 Diabetes Alliance was implemented in general practices in a staggered and ongoing basis. The pre and post intervention dates differ by practice, creating the stepped wedge design, where every practice switches from control to the intervention (once it had participated in the Diabetes Alliance), just not at the same point in time. Clustering for this study was at a site level, where each site may contain more than one general practice clinic and multiple practice clinicians, with or without Diabetes Alliance training. The data available was at the site level and could not distinguish individual clinics or GPs within each site. De-identified aggregate data were extracted from the NPS MedicineWise MedicineInsight program [15] and restricted for analysis purposes to 13 months prior to the first case conferencing at each site. Analysed data spans April 2014-May 2019 [16]. This study was conducted in accordance with the Declaration of Helsinki [17] and received ethics approval from the Hunter New England Human Research Ethics Committee (15/04/15/5.02). Written, informed consent was obtained from general practices and individually from patients who received the specialist-led case conferencing.
Recruitment
General practice recruitment for Diabetes Alliance occurred from April 2015 with patient outcomes data included up to May 2019. General practices were recruited via the Hunter New England and Central Coast Primary Health Network website, in their monthly newsletter and via expressions of interest. Recruitment also occurred during the Diabetes Alliance Masterclasses (education sessions) and through word of mouth.
Participants
For this study, data were extracted for patients 18 years and over with a recorded diagnosis of type 2 diabetes by their GP from practices enrolled in Diabetes Alliance. Data extracted at the practice level included all active patients, defined as 3 or more visits to the practice in the past 2 years, that received care for the management of type 2 diabetes. Participants who received the specialist-led case conferencing (n = 1072) were not able to be separated from general practice patients who did not (n = 21,634 patients), due to data aggregation. Simulation modelling (described as sensitivity analyses) was used to mimic the removal of the case conference participants from the spillover sample.
Integrated care intervention
Diabetes Alliance consists of three key activities: (i) case conferencing, (ii) practice feedback, and (iii) education and training.
(i) Case conferencing:
Patients enrolled directly in the Diabetes Alliance were provided a face-to-face specialist-led consultation of approximately 45 min duration, at their usual general practice. The case conferencing integrated the diabetes specialist team (endocrinologist, diabetes educator) with the general practice clinicians (GP and practice nurse). During the consultation, complications and comorbidities were reviewed, and a treatment plan was negotiated with the patient. Patients were reviewed by their GP and the diabetes specialist team 6 months after the initial case conference.
(ii) Practice feedback:
NPS MedicineWise utilised MedicineInsight data to produce a feedback report for each practice to monitor and evaluate practice-level clinical and process outcomes. The visiting endocrinologist and NPS MedicineWise facilitator discussed the feedback at each practice visit and assisted the practice staff to develop a plan for quality improvement. Practices received feedback reports every 6 months.
(iii) Education and training:
Endocrinologists provided 3 × 3 h face-to-face Masterclasses to GPs, registrars, and allied health staff in cycles every 3–4 months per year. Examples of topics included screening, diagnosis, and classification of diabetes, pathophysiology of type 2 diabetes, and medications. Diabetes Educators also provided a full day of education for practice nurses on similar topics.
Outcomes
Outcomes for this study include compliance with the frequency of diabetes tests. The Annual Cycle of Care recommends that body weight, waist, body mass index (BMI), and blood pressure are monitored every 6 months; HbA1c every 6–12 months; and total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides, albumin-to-creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) every 12 months [3]. Clinical outcomes include weight, waist, BMI, blood pressure, HbA1c, total cholesterol, LDL, HDL, triglycerides, ACR, creatinine, and eGFR.
Statistical analysis
Baseline characteristics were summarised as mean and standard deviation for continuous variables; frequency and percentage for categorical variables. Logistic mixed models were used to test whether the intervention was associated with compliance (yes/no) with test intervals before and after Diabetes Alliance for each outcome, with a random effect for patient within each site to account for the repeated measures of participants and the clustering within sites. The before Diabetes Alliance period began 13 months prior to the start of the intervention at each site, through to 1 month prior (12 months). The after Diabetes Alliance period began 6 months after the last intervention at each site, and lasted 6 months (or 12 months for tests that were only required annually). Linear mixed models were used to test for difference in clinical results (continuous) before and after Diabetes Alliance, with a random effect for patient within site. For outcomes where the residuals violated the assumption of normality, log-transformations were performed, and then results were back-transformed to their original scale. For the mixed models, the mean test value at each stage is reported, along with a p-value for the test of the difference between pre and post mean values.
Estimated glomerular filtration rate could not be adequately modelled in either its original or log transformed form and was therefore categorised and analysed using an ordinal mixed model, with patient within site effects. Odds ratio (OR) and 95% confidence interval (CI) are reported, where the OR represents the odds of scoring a higher eGFR category, where < 15 mL/min/1.73m2 is the lowest category, and > 60 mL/min/1.73m2 is the highest category (i.e. higher scores indicate better kidney function).
Chi-squared tests were used to assess changes in systolic blood pressure, HbA1c, and LDL cholesterol categories before and after Diabetes Alliance for a subset of patients who had repeated measures, i.e. test values in both the pre and post intervention periods.
Sensitivity analyses were conducted to investigate whether study results reflected spillover effects or if they were driven by the small proportion (< 5%) of patients that received specialist-led case conferencing. Patient-level data was not available, however the number of patients receiving case conferencing at each site was known. Therefore, simulation modelling was used, where a random sample from each site was taken, sampling the number of participants in the spillover: total number for that site minus the number receiving case conferencing at that site. This was performed 200 times until the results converged. The logistic mixed models for HbA1c only (screening tests and clinical result) were then run on each dataset with the mean odds ratio and estimated proportions pre and post reported. Effect estimates were compared to the main analyses. All statistical analyses were performed using Statistical Analysis System (SAS) software (version 9.4; SAS Institute, Cary, North Carolina, United States) and assumed a 5% significance level.
Results
Seventy-two sites, with a total of 22,706 patients with type 2 diabetes were included in the current analyses (Fig. 1). Overall, 1,072 out of 22,706 (4.7%) patients from practices enrolled in Diabetes Alliance directly participated in case conferencing. Characteristics of the patients at included sites are summarised in Table 1. Mean age was 67.7 (±13.5) years and 45% were female. Characteristics of the sample with data at 6 and 12 months post intervention are provided in Supplementary Table 1, Additional File 1 and show negligible differences.
Frequency of testing
Following Diabetes Alliance, compliance with the recommended testing intervals increased for all 12 clinical outcomes (p < 0.0001, Table 2). The largest increases were seen in compliance with measurement of waist circumference (OR 4.45), HbA1c (OR 3.05), BMI (OR 2.45), and weight (OR 2.29).
Clinical results
Overall, the clinical results showed small but significant improvements after Diabetes Alliance across most of the results, including weight, BMI, systolic and diastolic blood pressure, HbA1c, total cholesterol, LDL cholesterol, and triglycerides (Table 3). There was no difference in waist circumference, and HDL cholesterol reduction was of borderline significance (p = 0.05). Urine ACR and creatinine both increased following Diabetes Alliance (Table 3), and there was a reduced odds having an eGFR > 60 after Diabetes Alliance: OR 0.57, 95% CI. 0.52 to 0.63 (p < 0.001). Observed eGFR categories before and after Diabetes Alliance are presented in Supplementary Table 2, Additional File 1.
For log-transformed outcomes, absolute differences were also calculated (Table 3), but these values only hold at the mean, and the results are multiplicative, meaning at higher values the differences are greater and at lower values these differences are smaller. For a HbA1c of 10%, we expect the change to be 10 × 0.996 = 9.96%, i.e. a reduction in HbA1c of 0.04% after the Diabetes Alliance intervention. With a mean weight of 90.19 kg before Diabetes Alliance and 88.81 kg after, there was an absolute improvement at the mean of -1.38 kg. With a mean of 6.84% for HbA1c before the Diabetes Alliance and 6.81% after the intervention, there was an absolute improvement of -0.03% for HbA1c at the mean, and − 0.04% at a HbA1c of 10% (10 × 0.996 = 9.96; a change of -0.04%).
Changes in clinical results categories for subset with repeated measures
For the subset of patients with test results both before and after the Diabetes Alliance intervention, significant changes in clinical categories were observed for blood pressure, HbA1c, and LDL-cholesterol (Fig. 2, Supplementary Table 3, Additional File 1). Whilst most patients did not change category, a higher proportion of patients moved down to the lowest category (i.e. met the clinical target) in systolic blood pressure, HbA1c, and LDL-cholesterol, than moved up to the highest. For blood pressure (n = 9360, 41% of total sample), 18% moved down to ≤ 130 mm Hg systolic blood pressure after Diabetes Alliance, whereas only 12% moved up to > 130 mm Hg systolic blood pressure. For HbA1c (n = 5989, 26% of total sample), 18% moved down to a lower HbA1c category (< 7%, 7 to ≤ 8%, or 8 to ≤ 9%) after the intervention while 17% moved up (7 to ≤ 8%, 8 to ≤ 9%, or > 9%). For LDL-cholesterol (n = 3715, 16% of total sample), 13% of patients moved down to < 2mmol/L after Diabetes Alliance, and only 7% moved up to ≥ 2mmol/L.
Sensitivity analysis
Results from the simulation models indicated very slightly attenuated effect estimates for HbA1c. Patients were 2.29 (2.31, 2.65) times more likely to have their HbA1c levels measured at 6 months after Diabetes Alliance. This is lower than the estimate from the main analysis [3.05 (2.85–3.27)], but still significantly greater than 1. The proportion of patients that received 6 monthly HbA1c tests was 0.27 (0.26, 0.28) before the program and 0.48 (0.47, 0.49) after Diabetes Alliance. These proportions are also close to the point estimates of 0.24 and 0.48 from the main analysis. The mean test value in the pre period of 6.83% (95% CI 6.82–6.84%) and 6.81% (95% CI 6.80–6.82%) in the post period are also very similar to the values from the main analysis (6.84% and 6.81%, respectively), suggesting the presence of a spillover effect is robust.
Discussion
Overall, the Diabetes Alliance integrated model of care was associated with significant improvements in the frequency of diabetes screening tests, and small but significant improvement in clinical outcomes including weight, BMI, blood pressure, blood lipid profiles and glycaemic control across up to 22,706 general practice patients with type 2 diabetes. The learnings from the specialist-led case conferencing delivered to a small proportion of patients, accompanied by other capability building activities, spilled over to the wider cohort of general patients receiving usual care without direct involvement from the specialist team. These results are in keeping with previous small pilot studies [18, 19] and prospective controlled trials [20,21,22], and have now been confirmed at scale across a broad geographic footprint.
Increased testing does not automatically translate to better healthcare; however, statistically significant improvements in most of the clinical results were observed for all patients with type 2 diabetes across the general practice sites who had received the Diabetes Alliance intervention. If sustained, these improvements should translate into reduced morbidity and mortality at the population level. Results indicated that Diabetes Alliance was associated with a reduction in HbA1c even at the mean value of 6.84%, which is within recommendations, noting that slightly higher reductions occurred at higher HbA1C values. While the spillover benefits were modest when each clinical outcome was considered separately, the combination of clinical benefits (i.e. improved weight, blood pressure, lipids and glycaemic control) is likely to be synergistic and significant at a population level. A simulation study demonstrated that reductions in HbA1c levels by as little as 0.1%, up to 0.8% (in 0.1% increments), in a Swedish population with type 1 diabetes reduced the incidence of microvascular complications, improved life expectancy and quality of life over a 50-year time horizon, illustrating the importance of early improvement in glycaemic control, even if modest [23]. While glucose control remains a major focus in the management of patients with type 2 diabetes [24], the synergistic effects of improved blood pressure, blood lipids, and HbA1c likely confers the greatest benefit for reducing cardiovascular disease risk [25]. Diabetes Alliance is a real-world intervention that takes into consideration the “prevention paradox”, where a large number of individuals with less risk creates more cases in absolute terms than a small number of individuals with higher risk [26] The spillover effect show here is on all patients, the majority of whom had no interaction with the Diabetes Alliance program directly. The integrated care model specifically aims to enhance general practitioners capability in managing diabetes so the emphasis is on small but sustained improvements in the majority of patients, rather than the minority who are seen during specialist-led case conferencing or in hospital. The aim is to shift the distribution curve for a large sample, toward a favourable outcome, which has been demonstrated by the findings of this study.
The clinical results for ACR, creatinine, and eGFR observed in this study are consistent with kidney function declining over time for patients with type 2 diabetes; slowing the rate of decline represents improvement. The rate of kidney function decline has been studied recently in a cohort of 32,492 adult patients with type 2 diabetes (mean age 66.3 years, 52.6% male) predominantly located in Germany [27]. Over three years, 31% of patients had an eGFR slope of -12 mL/min/1.73m2 or more, and the proportion of patients with an eGFR < 30 mL/min/1.73m2 more than doubled [27]. Rates of chronic kidney disease in the Hunter New England region are high by Australian standards, identified as one of the top 20 hot spots contributing to the national burden of kidney disease [28]. The increase in urine ACR and creatinine in our study likely reflects the increased screening following Diabetes Alliance, noting creatinine/eGFR had more than twice the odds of being tested after Diabetes Alliance as it did before the intervention. Some reduction in eGFR may also be the result of an increased initiation of angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs) and sodium-glucose co-transporter-2 (SGLT2) inhibitors, where kidney function shows an initial decline with medication commencement but nephroprotective effects over time [29].
This study has evaluated the real-world spillover effect of an integrated model of care that has been implemented at scale across one Australian local health district. The nonrandomised pragmatic trial included a large sample of patients with type 2 diabetes from general practices using data from MedicineInsight, a national database. The analyses on the subset of patients with repeated measures looking at changes in clinical categories is at risk of selection bias and results need replication in other studies to be generalisable. We were also not able to identify the 4.7% of patients who had directly received case conferencing and exclude them to define a clean spillover sample. Instead, we ran simulation models for HbA1c to mimic patient removal and findings remained significant and consistent with the main analyses. Another limitation is the inability to quantify the extent of Diabetes Alliance intervention received by each site. General Practices vary considerably in size, both in number of GPs and patients with type 2 diabetes. Inclusion of sites with a mix of GPs who had and had not engaged with one or more Diabetes Alliance intervention activities, would likely bias our results towards the null, meaning the true effect estimates would be greater if restricted to GPs (and their spillover patient group) who had actively participated. Future evaluation of the Diabetes Alliance also aims to include a parallel control group; however, this was not feasible at the time of these analyses.
Conclusions
Although Diabetes Alliance was associated with significant improvements in the frequency of screening tests and clinical results across a large cohort, it is unclear if these effects are maintained over the longer-term and what impact they may have on reducing micro- and macrovascular complications. Hence, further research and evaluation is needed to determine the health, societal, and economic impacts from this real-world, integrated model of care for diabetes.
Data availability
The author confirms that all data generated or analysed during this study are included in this published article and Additional File 1.
Abbreviations
- ACR:
-
Albumin-to-Creatinine Ratio
- ACE:
-
Angiotensin-Converting Enzyme
- ARBs:
-
Angiotensin II Receptor Blockers
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- eGFR:
-
Estimated Glomerular Filtration Rate
- GP:
-
General Practitioners
- HDL:
-
High-Density Lipoprotein
- HNELHD:
-
Hunter New England Local Health District
- LDL:
-
Low-Density Lipoprotein (LDL)
- OR:
-
Odds Ratio
- SAS:
-
Statistical Analysis System
- SGLT2:
-
Sodium-Glucose Co-Transporter-2
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843.
Australian Institute of Health and Welfare (AIHW). Australian Burden of Disease Study: impact and causes of illness and death in Australia 2015—Summary report. Canberra, ACT 2019.
Australian Institute of Health and Welfare (AIHW). Prevalence of self-reported type 2 diabetes, among persons aged 18 and over, 2017–18. Canberra, ACT AIHW; 2020.
Baker IDI, Heart and Diabetes Institute. Diabetes: the silent pandemic and its impact on Australia. 2012.
Bagheri N, McRae I, Konings P, Butler D, Douglas K, Del Fante P, et al. Undiagnosed diabetes from cross-sectional GP practice data: an approach to identify communities with high likelihood of undiagnosed diabetes. BMJ Open. 2014;4(7):e005305.
Diabetes Australia. About diabetes 2022 [ https://www.diabetesaustralia.com.au/about-diabetes
Clinical Guidelines Task Force. Global Guideline for Type 2 Diabetes. https://www.iapb.org/wp-content/uploads/Global-Guideline-for-Type-2-Diabetes-IDF-2012.pdf: International Diabetes Federation; 2012.
Factsheet. Your diabetes annual cycle of care. In: National Diabetes Services Scheme (NDSS), editor. https://www.ndss.com.au/wp-content/uploads/fact-sheets/fact-sheet-your-diabetes-annual-cycle-of-care.pdf2021.
Sainsbury E, Shi Y, Flack J, Colagiuri S. Burden of diabetes in Australia: it’s time for more action - preliminary report. 2018.
The Royal Australian College of General Practitioners (RACGP). Management of type 2 diabetes: A handbook for general practice. In: RACGP, editor. East Melbourne; VIC2020.
Arah OA, Roset B, Delnoij DM, Klazinga NS, Stronks K. Associations between technical quality of diabetes care and patient experience. Health Expect. 2013;16(4):e136–45.
Acharya S, Philcox AN, Parsons M, Suthers B, Luu J, Lynch M et al. Hunter and New England Diabetes Alliance: innovative and integrated diabetes care delivery in general practice. Aust J Prim Health. 2019.
Benjamin-Chung J, Arnold BF, Berger D, Luby SP, Miguel E, Colford JM Jr, et al. Spillover effects in epidemiology: parameters, study designs and methodological considerations. Int J Epidemiol. 2017;47(1):332–47.
Australian New Zealand Clinical Trials Registry (ANZCTR). Diabetes Alliance: effectiveness of Adult Diabetes Integrated Care Delivered in General Practice on Testing and clinical outcomes (ACTRN12622001438741). Sydney: NSW ANZCTR; 2022.
Busingye D, Gianacas C, Pollack A, Chidwick K, Merrifield A, Norman S, et al. Data Resource Profile: MedicineInsight, an Australian national primary health care database. Int J Epidemiol. 2019;48(6):1741–h.
National Statistical Service. A guide for data integration projects involving Commonwealth data for statistical and research purposes: the separation principle Canberra. ACT Australian Government; 2014.
Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Grimmer-Somers K, Dolesj W, Atkinson J. Enhanced primary care pilot program benefits type II diabetes patients. Aust Health Rev. 2010;34(1):18–24.
Meyerowitz-Katz G, Bramwell S, Jayaballa R, Bishay R, Corless I, Ravi S, et al. Effectiveness of joint specialist case conferences for building general practice capacity to enhance diabetes care: a pilot study in Western Sydney, Australia. J Integr Care. 2018;26(3):199–210.
Zhang J, Donald M, Baxter KA, Ware RS, Burridge L, Russell AW, et al. Impact of an integrated model of care on potentially preventable hospitalizations for people with type 2 diabetes mellitus. Diabet Med. 2015;32(7):872–80.
Russell AW, Donald M, Borg SJ, Zhang J, Burridge LH, Ware RS, et al. Clinical outcomes of an integrated primary-secondary model of care for individuals with complex type 2 diabetes: a non-inferiority randomised controlled trial. Diabetologia. 2019;62(1):41–52.
Russell AW, Baxter KA, Askew DA, Tsai J, Ware RS, Jackson CL. Model of care for the management of complex type 2 diabetes managed in the community by primary care physicians with specialist support: an open controlled trial. Diabet Med. 2013;30(9):1112–21.
Jendle J, Ericsson Å, Hunt B, Valentine WJ, Pollock RF. Achieving good Glycemic Control Early after Onset of diabetes: a cost-effectiveness analysis in patients with type 1 diabetes in Sweden. Diabetes Therapy. 2018;9(1):87–99.
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the study of diabetes. Diabetes Care. 2015;38(1):140–9.
Wong ND, Zhao Y, Patel R, Patao C, Malik S, Bertoni AG, et al. Cardiovascular Risk factor targets and Cardiovascular Disease Event risk in diabetes: a Pooling Project of the atherosclerosis risk in communities Study, multi-ethnic study of atherosclerosis, and Jackson Heart Study. Diabetes Care. 2016;39(5):668–76.
Raza SA, Salemi JL, Zoorob RJ. Historical perspectives on prevention paradox: when the population moves as a whole. J Family Med Prim Care. 2018;7(6):1163–5.
Bramlage P, Lanzinger S, Hess E, Fahrner S, Heyer CHJ, Friebe M, et al. Renal function deterioration in adult patients with type-2 diabetes. BMC Nephrol. 2020;21(1):312.
Kidney Health Australia. Chronic Kidney Disease Hot Spots. https://kidney.org.au/uploads/resources/state-of-the-nation-kidney-health-week-2016-chronic-kidney-disease-hot-spots.pdf; 2016.
Bakris GL, Weir MR. Initial drops in glomerular filtration rate with certain drug classes retard kidney Disease Progression. Am J Nephrol. 2022;53(7):513–5.
Acknowledgements
We sincerely thank all patients who have directly or indirectly participated in Diabetes Alliance. We thank the Hunter New England Local Health District and Hunter New England and Central Coast Primary Health Network executive team for their sponsorship and support. We also thank Clare Delaney and Kendal Chidwick for their assistance with NPS MedicineWise data and drafting the manuscript, and all GPs, practice nurses, Primary Health Network support staff, diabetes educators, and endocrinologists who have overwhelmingly supported the development and roll out of this program.
Funding
This work is funded under an Alliance structure between the Hunter New England and Central Coast Primary Health Network and Hunter New England Local Health District. Funding for the program covers the costs of 1FTE Endocrinologist, 1FTE Diabetes Educator, 1FTE Program Manager, and 1 FTE Administrative officer. The Hunter New England and Central Coast Primary Health Network funded NPS MedicineWise to design, produce, and deliver feedback reports to participating practices and to utilise MedicineInsight data for evaluation of the integrated model of care. The Australian Government Department of Health and Aged Care.
Author information
Authors and Affiliations
Contributions
Conceptualisation, S.H.A., Data curation, M.E.P., L.L., C.J.O., Funding acquisition, S.H.A., M.E.P., J.R.A., A.J.H., Methodology, S.H.A., J.R.A., L.L., C.J.O., A.J.H., K.W., Project administration, M.E.P., M.J., J.L., A.N.P., K.W., C.W.R., D.J., T.Q., C.S., S.D., Data analysis and interpretation, S.H.A., L.L., C.J.O., J.R.A., A.J.H., K.W., Writing original draft, RMT., writing review and editing, all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All study methods were conducted in accordance with the Declaration of Helsinki. This study received ethics approval from the Hunter New England Human Research Ethics Committee (15/04/15/5.02). Written, informed consent was obtained from general practices and individually from patients who received the specialist-led case conferencing.
Consent for publication
Not applicable. The data presented is at a general practice level rather than reporting the specifics of an individual patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Acharya, S., Taylor, R., Parsons, M. et al. Spillover effects from a type 2 diabetes integrated model of care in 22,706 Australians: an open cohort stepped wedge trial. BMC Endocr Disord 24, 183 (2024). https://doi.org/10.1186/s12902-024-01692-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-024-01692-4