Abstract
Background
Low-grade inflammation plays a role in the pathogenesis of metabolic syndrome (MetS), and measuring levels of inflammatory molecules, such as high-sensitivity C-reactive protein (hs-CRP), may indicate Mets progression. Serum uric acid (SUA) has also been identified as an independent risk factor for MetS. This study aimed to investigate the association between MetS components and levels of serum hs-CRP and SUA using representative and reliable data for the Korean population.
Methods
This study used the data of the Korea National Health and Nutrition Examination Survey 2016–2018, a cross-sectional and nationally representative survey performed by the Korean Centers for Disease Control and Prevention.
Results
We analysed the data of 13,454 individuals. High hs-CRP levels were observed in 1,164 (8.7%) subjects while 3,296 (24.5%) subjects had high SUA levels. Moreover, hs-CRP was negatively correlated with serum high-density lipoprotein (HDL) (OR, 1.703; 95% CI, 1.431–2.027). When stratified by sex, this trend remained, but the correlation was stronger in women than in men. Furthermore, high SUA levels were significantly associated with hypertension (HTN) (OR, 1.399; 95% CI, 1.210–1.616), hypertriglyceridemia (OR, 1.735; 95% CI, 1.486–2.026), and low HDL (OR, 1.257; 95% CI, 1.106–1.429), but not with diabetes mellitus (DM) (OR, 0.478; 95% CI, 0.382–0.597). When grouped by sex, this trend remained, however, all MetS components were found to be more prevalent in women with high SUA.
Conclusions
Our findings showed that low HDL was more prevalent in subjects with high hs-CRP, and high SUA levels were observed in subjects with HTN, hypertriglyceridemia, and low HDL. However, the prevalence of high SUA was lower in diabetic subjects.
Similar content being viewed by others
Background
Metabolic syndrome (MetS) is a cluster of metabolic abnormalities that include abdominal obesity with high waist circumference (WC), increased blood pressure (BP), increased fasting blood glucose (FBG) and triglyceride (TG) levels, and decreased high-density lipoprotein (HDL) cholesterol levels [1,2,3]. These abnormalities are the well-known classical risk factors for type 2 diabetes mellitus (DM) and cardiovascular diseases (CVDs) [2, 3]. Worldwide, the prevalence of MetS has rapidly increased over the past several decades, and it is estimated that about one-quarter of adults have MetS, although its prevalence differs in different geographical regions [4,5,6,7,8,9]. Thus, it is crucial to identify early risk factors for MetS that could ultimately help in preventing abnormal conditions leading to chronic diseases.
Previous studies suggest that MetS is a chronic condition with low-grade inflammation and is influenced by the interaction between genetic and environmental factors [10, 11]. Although the precise role of inflammation in MetS pathogenesis remains unknown, the rate of disease progression could be indirectly estimated by measuring the circulating levels of inflammatory molecules such as high-sensitivity C-reactive protein (hs-CRP) [10, 11]. Mirhafez et al. reported that serum hs-CRP level increases in a step-wise manner with the increase in the number of MetS components [1]. Similar association was observed in another study conducted by Wang et al. [12].
Increased level of serum uric acid (SUA), the end product of purine metabolism, is considered as one of the independent risk factors for MetS [13,14,15]. High SUA levels might contribute to the development of MetS by enhancing the levels of circulatory inflammatory molecules, such as hs-CRP, and increasing the erythrocyte sedimentation rate by activating nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB), a protein complex that plays a role in the transcription of several cytokines and inflammatory molecules [14]. Thus, it is possible to predict the development of hypertension, obesity, and DM by monitoring the levels of serum hs-CRP and SUA.
The independent risk factors of hs-CRP and SUA levels may have a significant impact on evaluating the prevalence of MetS components in both men and women. Moreover, research has shown that there is a correlation between BMI and the increase in SUA and hs-CRP levels in adults [13, 16]. Nevertheless, there have been limited investigations into these relationships among Korean adults. Hence, the aim of this study was to explore the associations between the levels of hs-CRP and SUA and the prevalence of MetS components among Korean adults, categorized by sex and BMI subgroups, using representative and reliable data for the Korean population.
Methods
Study population
This study used data from the seventh Korea National Health and Nutrition Examination Survey (KNHANES VII) conducted during 2016–2018 by the Korean Centers for Disease Control and Prevention (KCDC). The KNHANES data were obtained annually from randomly selected 3840 individuals of 192 regions in Korea using a stratified multi-stage probability sampling design. The KNHANES included a health interview, health examination, and a nutrition survey. The data were collected through household interviews, and standardized physical examinations were conducted at mobile examination centers. All survey procedures were approved by the institutional review board of the KCDC, and written informed consent was obtained from all participants before initiating the surveys. All study participants were aged ≥ 19 years. Individuals with data on WC, BP, FBG, TG, HDL, hs-CRP, and SUA were included in our study. Finally, 13,454 out of 24,269 adults were eligible for this study (Fig. 1).
Definition of metabolic syndrome components
Serum levels of glucose, TG, and HDL cholesterol were measured after 8- or 12-hour fasting period. The hexokinase UV method with the Hitachi Automatic Analyzer (Hitachi, Japan) and Pureauto S GLU reagent (Sekisui, Japan) was used to measure glucose levels. TG levels were measured using the enzymatic method with the Hitachi Automatic Analyzer (Hitachi, Japan) and Pureauto S TG-N reagent (Sekisui, Japan). HDL cholesterol levels were measured with the Cholestest N HDL reagent (Sekisui, Japan) and homogeneous enzymatic colorimetric method using the Hitachi Automatic Analyzer (Hitachi, Japan). Normal fasting glucose level was considered as < 100 mg/dL, impaired fasting glucose or prediabetes was considered if the fasting glucose level was 100–125 mg/dL, and DM was considered if fasting glucose was ≥ 126 mg/dL [17]. Individuals with DM who were receiving antihyperglycemic agents and/or insulin, regardless of the fasting glucose level, were also included in the DM group. Hypertriglyceridemia was defined as fasting TG level ≥ 200 mg/dL, and individuals were assigned to high or very high groups according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) guidelines [2, 18]. This decision was made to better reflect the actual clinical setting and to better capture the increased risk of cardiovascular diseases such as heart attacks and strokes. In addition, this decision was made based on the assumption that using this threshold would demonstrate a more significant association between hs-CRP, SUA, and high triglyceride levels. Low HDL cholesterol level was defined as < 40 mg/dL for men and < 50 mg/dL for women [18].
BP measurements were performed on the right arm of the participants seated for at least 5 min using a standard mercury sphygmomanometer. Three measurements were performed for all participants at 5-minute intervals, and the average of the second and third measurements was used in the analysis. Hypertension (HTN) was defined as systolic blood pressure (SBP) ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, or use of antihypertensive medications independently of BP [19].
WC measurement was taken to the nearest 0.1 cm in a horizontal plane at the midpoint between the iliac crest and the lower rib. High WC was defined as ≥ 90 cm for men and ≥ 85 cm for women according to the criteria for abdominal obesity defined by the Korean Society for the Study of Obesity [20].
Hs-CRP and SUA measurements
Hs-CRP levels were measured by immunoturbidimetry using the Cobas analyzer (Roche, Germany) and the Cardiac C-Reactive Protein High Sensitivity reagent (Roche, Germany) (detection range 0.1–20 mg/L). High and low hs-CRP levels were defined as ≥ 3.0 mg/L and < 3.0 mg/dL, respectively [1]. SUA was measured by colorimetric method using uricase and Uric acid reagent (Eiken, Japan) on a Hitachi Automatic Analyzer (Hitachi, Japan) (lower detection limit 1.0 mg/dL). High and low SUA levels were defined as ≥ 6 mg/dL and < 6 mg/dL, respectively [10].
Other variables
Information on age, sex, socioeconomic variables (i.e., household income and educational level), and lifestyle variables (i.e., smoking, alcohol consumption, and physical activity) were collected from all participants using a self-reported questionnaire. The average monthly household income was categorized into four groups: low, lower middle, higher middle, and high. Educational level was categorized into four groups: elementary school graduation or lower, middle school graduation, high school graduation, and college graduation or higher. Non-smokers were defined as individuals who had never smoked in their lifetime, past-smokers as those who had smoked in the past but did not smoke at the time of conducting the survey, and current smokers as those who continued smoking daily or often at the time of conducting the survey. Alcohol consumption was dichotomized into zero and non-zero consumption. Physical activity during work, transport, and leisure time was estimated based on the total time spent in physical activity per week and the intensity of the physical activity. The following criteria regarding physical activity for health were recommended to achieve ≥ 600 MET-min/week: at least 150 min/week of moderate-intensity physical activity, 75 min/week of vigorous-intensity physical activity, or an equivalent combination of moderate- and vigorous-intensity physical activity.
Body weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively, with participants wearing light indoor clothing without shoes. BMI was calculated by dividing weight (in kilograms) by the square of height (in meters) (kg/m2). Underweight status was defined as BMI < 18.5 kg/m2, normoweight as BMI between ≥ 18.5 kg/m2 and < 25.0 kg/m2, overweight as BMI between ≥ 25.0 kg/m2 and < 30.0 kg/m2, and obese as BMI ≥ 30.0 kg/m2 [21].
Statistical analysis
All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). We applied the complex sampling design and sampling weights while analyzing the KNHANES data in order to provide a national prevalence estimate. A P-value < 0.05 was considered statistically significant. The subjects included in the analysis were divided into groups based on hs-CRP and SUA levels. Subgroup analyses were performed according to sex and BMI. The chi-square test was used to analyzed categorical variables (represented as frequency and percentage (%)), whereas the independent t-test was used to analyze continuous variables (represented as mean ± standard error). Multivariate logistic regression analysis was performed to assess the impact of hs-CRP and SUA (using low hs-CRP and low SUA as the reference groups) on the prevalence of MetS components by sex and BMI (< 25.0 kg/m2 and ≥ 25.0 kg/m2) subgroups. Results of the regression analysis are presented as odds ratios (ORs) with 95% confidence intervals (CIs).
Results
We retrospectively analysed the data of 13,454 subjects. Low and high hs-CRP levels were observed in 12,290 (91.3%) and 1,164 (8.7%) subjects, respectively. Moreover, low and high SUA levels were observed in 10,158 (75.5%) and 3,296 (24.5%) subjects, respectively. The characteristics of the participants are summarized in Table 1. Compared to subjects with low hs-CRP, the prevalence of high WC (46.16% vs. 27.69%), HTN (36.30% vs. 27.57%), prediabetes (25.14% vs. 22.87%), DM (16.10% vs. 10.18%), hypertriglyceridemia (18.18% vs. 15.48%), and low HDL (47.35% vs. 30.08%) was higher in those with high hs-CRP. Similarly, compared to subjects with low SUA, the prevalence of high WC (40.41% vs. 24.98%), HTN (33.91% vs. 26.17%), prediabetes (28.98% vs. 20.80%), hypertriglyceridemia (26.92% vs. 11.45%), and low HDL (32.10% vs. 31.31%) was higher in those with high SUA. However, the prevalence of DM was lower in subjects with high SUA compared to those with low SUA (8.87% vs. 11.36%).
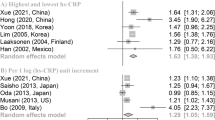
To determine the association between hs-CRP levels and MetS components, we performed logistic regression analysis, and the results are presented in Table 2. A significant negative correlation was observed between HDL and hs-CRP (OR, 1.703; 95% CI, 1.431–2.027). In subjects with BMI < 25 kg/m2, the OR of high hs-CRP for low HDL was higher than that for low hs-CRP. In subjects with BMI ≥ 25 kg/m2, the OR of high hs-CRP as a risk determinant factor for low HDL was higher than that of low hs-CRP. However, the OR in subjects with BMI < 25 kg/m2 was relatively higher than that in their counterparts. High WC was significantly associated with hs-CRP only in subjects with BMI ≥ 25 kg/m2. When stratified by sex, similar trends were observed.
Furthermore, logistic regression analysis was performed to determine the association between SUA levels and MetS components, and the results are summarized in Table 3. A high SUA level was found to be an independent risk factor for HTN (OR, 1.399; 95% CI, 1.210–1.616), hypertriglyceridemia (OR, 1.735; 95% CI, 1.486–2.026), and low HDL (OR, 1.257; 95% CI, 1.106–1.429), but not for DM (OR, 0.478; 95% CI, 0.382–0.597). The ORs of high SUA for prediabetes and high WC were similar to those for low SUA. Similar trends were observed when the subjects were stratified by BMI (< 25 kg/m2 vs. ≥25 kg/m2).
Finally, logistic regression analysis was implemented to estimate the association between SUA levels and MetS components for men and women separately, and the findings are presented in Table 3. In the subgroup analyses for men, the ORs of high SUA for HTN (OR, 1.272; 95% CI, 1.081–1.497), hypertriglyceridemia (OR, 1.735; 95% CI, 1.452–2.074), and low HDL (OR, 1.171; 95% CI, 1.002–1.368) were higher than those of low SUA. However, the ORs of high SUA for DM (OR, 0.339; 95% CI, 0.268–0.429) and prediabetes (OR, 0.845; 95% CI, 0.725–0.984) were lower than those of low SUA. No significant association was observed between SUA levels and WC. In men, these trends remained even after stratification according to BMI. In the subgroup analyses for women, the association between SUA and each MetS component was comparatively stronger than that in men. The ORs of high SUA for HTN (OR, 1.906; 95% CI, 1.443–2.517), DM (OR, 1.512; 95% CI, 1.081–2.114), prediabetes (OR, 1.431; 95% CI, 1.100-1.861), hypertriglyceridemia (OR, 1.752; 95% CI, 1.331–2.305), low HDL (OR, 1.483; 95% CI, 1.189–1.850), and high WC (OR, 1.598; 95% CI, 1.145–2.230) were higher than those of low SUA. In particular, a significant association between high SUA levels and DM risk was observed only among women.
Discussion
Herein, we investigated the association of hs-CRP and SUA levels with MetS components in Korean adults aged 19 years and above using the reliable and representative KNHANES VII data. Our results showed that low HDL was more prevalent in subjects with high hs-CRP levels. This trend remained even when individuals were grouped by sex and BMI; however, the association was stronger in women than in men. Moreover, the prevalence of high SUA was higher in subjects with HTN, hypertriglyceridemia, and low HDL; however, it was lower in those with DM. When grouped by sex, this trend was still observed in men, but all MetS components were found to be more prevalent in women with high SUA. These results suggest that hs-CRP and SUA could be used as potential biomarkers for identifying individuals at high risk for MetS and cardiometabolic diseases.
Increased hs-CRP levels in individuals with possible MetS could be explained based on the prevalence of low HDL and high WC [22,23,24,25]. The inverse relationship between hs-CRP and HDL levels in healthy individuals and those with MetS has been reported in several studies, suggesting that low HDL could be the main independent determinant for high hs-CRP that favors inflammation [22, 24, 25]. Another study reported that the overall prevalence of low HDL was approximately 1.703 times higher in subjects with high hs-CRP than those with low hs-CRP. Interestingly, higher prevalence of high hs-CRP was observed in women than in men. This sex-associated difference might be due to differences in the hormonal profile and total body adipose tissue between men and women [22, 26]. In women, estrogen might be involved in the inflammatory process [22], and compared to men, women generally have a higher percentage of total body adipose tissue, which is known to secretes several proinflammatory cytokines, such as tumor necrosis factor (TNF)-α, leptin, and adiponectin [26, 27]. Additionally, previous studies have shown that CRP gene expression and levels are increased from adipose tissue of MetS subjects, suggesting the significant association between increased hs-CRP levels and high WC [28, 29].
In this study, compared to overweight and obese subjects (BMI ≥ 25 kg/m2), normal-weight subjects (BMI < 25 kg/m2) showed a more significant negative correlation between HDL and hs-CRP in both men and women. This might be explained partially by the fact that individuals with normal weight obesity (NWO), which is defined as a state of normal weight (BMI < 25 kg/m2) but increased body fat percentage, are at a high risk for cardiovascular disorders [30]. The NWO phenotype is more prevalent in Asians compared to Westerners [31, 32]. Previous studies showed that Asians not only have a high percentage of body fat but also a relatively high prevalence of at least one risk factor for cardiovascular disorders even at a low BMI [32]. Specifically, over 30% of the general Korean population might be classified as having NWO even if a lower cut-off (BMI < 23 kg/m2 for the Asian cut-off point) is applied [33]. Individuals with the NWO phenotype are likely to have increased levels of adipocyte-derived proinflammatory cytokines due to increased body fat mass [30, 34]. In people with NWO, excessive body fat could affect the levels of HDL and TG through various mechanisms, such as alteration of the lipolysis process [30, 35]. Free fatty acid (FFA) and very low-density lipoprotein-triglyceride (VLDL-TG) complex are synthesized by the adipose tissue, and increased lysis of TG leads to increased levels of FFA, which eventually prevents the action of the enzyme lipoprotein lipase and increases the production of VLDL and TG in the liver [30, 36]. Increase in FFA, TG, and VLDL-TG levels can further promote the activity of cholesteryl ester transfer protein, leading to increased synthesis of TG-rich HDL particles, which are easily cleared and degraded, thereby lowering HDL levels [30, 36].
Our results showed that the overall prevalence rate of high SUA was higher in subjects with hypertriglyceridemia but not in those with high WC, a surrogate marker of central obesity. Our results are consistent with those of previous studies [37, 38]. A cross-sectional study in Peru reported that high SUA levels are positively associated with hypertriglyceridemia but not with central obesity [37]. Another longitudinal study in China reported that individuals with higher triglyceride levels are more likely to develop hyperuricemia than those with low triglyceride levels [38]. The association between high SUA and hypertriglyceridemia can be indirectly proved by urate-lowering therapy, which improves serum cholesterol and triglyceride levels [39]. Moreover, this association between high SUA and hypertriglyceridemia could be explained to some extent by alterations in the metabolism of lipids, especially triglycerides, through the activation of mitochondrial NADPH oxidase and inhibition of AMPK and AKT2 [37, 40]. Thus, although central obesity is a significant risk factor for the development of cardiometabolic diseases and MetS, our results suggest that hypertriglyceridemia due to high SUA precedes obesity. Interestingly, differences in the sex-specific association between high SUA levels and hypertriglyceridemia were not observed in this study.
Consistent with previous studies, we observed significantly higher SUA levels in men than in women, which might be due to the urate-lowering effects of estrogen in women [41,42,43]. However, it has been shown that the association between high SUA and various diseases including HTN is stronger in women than in men, which suggests that SUA plays a sex-specific role in the progression of cardiometabolic diseases [41, 44]. This sensitivity of women towards SUA may be partially explained by the positive association between mean platelet volume and SUA levels, which is observed only in women [41, 45]. Mean platelet volume as a determinant of platelet activation and is correlated with several cardiometabolic diseases including HTN [41, 46,47,48]. We observed that the overall prevalence rate of high SUA is higher in subjects with HTN. Specifically, the relationship between high SUA and HTN was found to be stronger in women than in men. These results are contrary with those of previous studies. A study from Japan reported that high SUA is strongly associated with HTN in men, but not in women [49]. Conversely, another study from China found that high SUA is positively correlated with HTN in men, whereas a negative correlation was observed in women [50].
We observed that the overall prevalence of high SUA is lower in diabetic subjects, which is in line with the results of previous studies [51,52,53,54]. It has been reported that SUA levels are inversely correlated with DM in a representative sample of US adults [51]. This inverse correlation between SUA and DM was also reported in studies from Japan, India, and China [52,53,54]. This inverse correlation might be due to the uricosuric effect of glucose on uric acid. High glucose levels in diabetic individuals may prevent uric acid from being reabsorbed and enhance its excretion through the kidneys, thereby reducing the net concentration of SUA [55,56,57]. Another possible mechanism to explain the negative correlation between SUA and DM is related to the reduced antioxidant action of uric acid due to oxidative stress and increased free radical production in diabetic individuals [58,59,60]. It is possible that serum uric acid has a dual function in determining health outcomes, with the ultimate effects depending on the balance between these two functions [61]. At lower levels, serum uric acid can act as a powerful endogenous antioxidant with beneficial anti-oxidative effects [62, 63]. However, at higher levels, serum uric acid can act as a prooxidant on vascular cells and adipocytes [64], and promote the secretion of inflammatory mediators such as C-reactive protein and monocyte chemoattractant protein-1 [65, 66]. This suggests that at higher levels, its prooxidant function may outweigh its antioxidant function, leading to endocrine disorders.
Interestingly, when stratified by sex, the negative association between SUA and DM became stronger in men; however, a positive association was observed in women, which is similar to findings of some previous studies [67, 68]. A 5-year retrospective cohort study conducted in Korea reported a significant association between hyperuricemia and the risk for DM only in women but not in men [67]. Another retrospective longitudinal study conducted in Japan also reported similar association only in women [68]. These sex-associated differences might be to some extent due to differences in fat distribution and its role in regulating SUA levels between men and women. In women, low glucocorticoid receptor gene expression and low glucocorticoid-binding were observed in visceral preadipocytes compared to subcutaneous preadipocytes, which may lead to decreased visceral fat mass in women [69]. It has also been reported that subcutaneous-fat-type and visceral-fat-type obesity may be implicated in poor uric acid excretion and excess uric acid production, respectively [70]. Moreover, changes in the transport of uric acid in the kidney tubules may lead to insulin resistance or hyperinsulinemia in individuals with reduced uric acid excretion [71].
Our study has some limitations which have be considered when interpreting the results. The main limitation of our study is the cross-sectional study design, which makes it difficult to clearly determine the causality between hs-CRP, SUA, and MetS components. Second, almost all variables measured at a single time point were used to identify the effects of hs-CRP and SUA on the prevalence of each MetS component, which might negatively affect the data accuracy. Third, recall bias while collecting the sociodemographic characteristics cannot be ruled out due to the use of surveys. Finally, the overall prevalence of MetS components might have been underestimated since we included subjects without complete information on them. However, the data could be missing at random; thus, the exclusion process is unlikely to significantly affect the study findings.
Conclusion
Low HDL is more prevalent in individuals with high hs-CRP levels, and this association between HDL and hs-CRP is stronger in women than in men. Moreover, the prevalence of high SUA is more in people with HTN, hypertriglyceridemia, and low HDL; however, it is less in diabetic individuals. When grouped by sex, this trend is still observed in men, but all MetS components are more prevalent in women with high SUA.
Data Availability
The datasets used for this study are available from the corresponding author on reasonable request.
References
Mirhafez SR, Ebrahimi M, Saberi Karimian M, Avan A, Tayefi M, Heidari-Bakavoli A, et al. Serum high-sensitivity C-reactive protein as a biomarker in patients with metabolic syndrome: evidence-based study with 7284 subjects. Eur J Clin Nutr. 2016;70(11):1298–304.
Yang YM, Shin BC, Son C, Ha IH. An analysis of the associations between gender and metabolic syndrome components in korean adults: a national cross-sectional study. BMC Endocr Disord. 2019;19(1):67. https://doi.org/10.1186/s12902-019-0393-0.
Reddy P, Lent-Schochet D, Ramakrishnan N, McLaughlin M, Jialal I. Metabolic syndrome is an inflammatory disorder: a conspiracy between adipose tissue and phagocytes. Clin Chim Acta. 2019;496:35–44. https://doi.org/10.1016/j.cca.2019.06.019. Epub 2019 Jun 20.
Ranasinghe P, Mathangasinghe Y, Jayawardena R, Hills AP, Misra A. Prevalence and trends of metabolic syndrome among adults in the Asia-pacific region: a systematic review. BMC Public Health. 2017;17(1):101.
Song QB, Zhao Y, Liu YQ, Zhang J, Xin SJ, Dong GH. Sex difference in the prevalence of metabolic syndrome and cardiovascular-related risk factors in urban adults from 33 communities of China: the CHPSNE study. Diab Vasc Dis Res. 2015;12(3):189–98.
Li Y, Zhao L, Yu D, Wang Z, Ding G. Metabolic syndrome prevalence and its risk factors among adults in China: a nationally representative cross-sectional study. PLoS ONE. 2018;13(6):e0199293.
Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA. 2015;313(19):1973–4.
Lim S, Shin H, Song JH, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and nutrition examination survey for 1998–2007. Diabetes Care. 2011;34(6):1323–8.
Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and risk factors for metabolic syndrome in asian Indians: a community study from urban eastern India. J Cardiovasc Dis Res. 2012;3(3):204–11.
Sah SK, Khatiwada S, Pandey S, Kc R, Das BKL, Baral N, Lamsal M. Association of high-sensitivity C-reactive protein and uric acid with the metabolic syndrome components. Springerplus. 2016;5:269. https://doi.org/10.1186/s40064-016-1933-y. eCollection 2016.
Ma K, Jin X, Liang X, Zhao Q, Zhang X. Inflammatory mediators involved in the progression of the metabolic syndrome. Diabetes Metab Res Rev. 2012;28(5):388–94. https://doi.org/10.1002/dmrr.2291.
Wang L, Zheng B, Zhao H, Du P, Sun A, Hua K, et al. α-Adducin gene G614T polymorphisms in essential hypertension patients with high low density lipoprotein (LDL) levels. Indian J Med Res. 2014;139:273.
Foster C, Smith L, Alemzadeh R. Excess serum uric acid is associated with metabolic syndrome in obese adolescent patients. J Diabetes Metab Disord. 2020;19(1):535–43.
Spiga R, Marini MA, Mancuso E, Fatta CD, Fuoco A, Perticone F, et al. Uric acid is Associated with inflammatory biomarkers and induces inflammation Via activating the NF-κB signaling pathway in HepG2 cells. Arterioscler Thromb Vasc Biol. 2017;37(6):1241–9.
Cicero AFG, Fogacci F, Giovannini M, Grandi E, Rosticci M, D’Addato S, et al. Serum uric acid predicts incident metabolic syndrome in the elderly in an analysis of the Brisighella Heart Study. Sci Rep. 2018;8(1):11529. https://doi.org/10.1038/s41598-018-29955-w.
Hulsegge, Herber-Gast GCM, Spijkerman AMW, Susan H, Picavet J, van der Schouw YT, et al. Obesity and age-related changes in markers of oxidative stress and inflammation across four generations. Obes (Silver Spring). 2016;24(6):1389–96. https://doi.org/10.1002/oby.21515. Epub 2016 May 4.
American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes – 2018. Diabetes Care. 2018;41(Suppl 1):13–S27.
National cholesterol education program expert panel on. detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Available from: https://www.nhlbi.nih.gov/files/docs/guidelines/atp3xsum.pdf (accessed on January 10, 2022).
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in korean adults. Diabetes Res Clin Pract. 2007;75(1):72–80.
WHO Expert Consultation. Appropriate body-mass index for asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Garcia VP, Rocha HN, Sales AR, Rocha NG, da Nóbrega AC. Sex differences in high sensitivity C-Reactive protein in subjects with risk factors of metabolic syndrome. Arq Bras Cardiol. 2016;106(3):182–7.
Nakamura H, Ito H, Egami Y, Kaji Y, Maruyama T, Koike G, et al. Waist circumference is the main determinant of elevated C-reactive protein in metabolic syndrome. Diabetes Res Clin Pract. 2008;79(2):330–6.
Garcia-Lorda P, Bulló M, Balanzà R, Salas-Salvadó J. C-reactive protein, adiposity and cardiovascular risk factors in a Mediterranean population. Int J Obes (Lond). 2006;30(3):468–74.
Huang J, Parish R, Mansi I, Yu H, Kennen EM, Davis T, et al. Non-high-density lipoprotein cholesterol in patients with metabolic syndrome. J Investig Med. 2008;56(7):931–6.
Han TS, Sattar N, Williams K, Gonzalez-Villalpando C, Lean ME, Haffner SM. Prospective study of C-reactive protein in relation to the development of diabetes and metabolic syndrome in the Mexico City Diabetes Study. Diabetes Care. 2002;25(11):2016–21.
Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol. 2004;15(11):2792–800.
Bremer AA, Devaraj S, Afify A, Jialal I. Adipose tissue dysregulation in patients with metabolic syndrome. J Clin Endocrinol Metab. 2011;96(11):E1782–8. https://doi.org/10.1210/jc.2011-1577.
Ouchi N, Kihara S, Funahashi T, Nakamura T, Nishida M, Kumada M, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation. 2003;107(5):671–4. https://doi.org/10.1161/01.cir.0000055188.83694.b3.
Kim MH, Kim HN, Choi WS. The association between subclinical inflammation and abnormal glucose and lipid metabolisms in normal-weight korean individuals. Nutr Metab Cardiovasc Dis. 2018;28(11):1106–13.
Kapoor N, Furler J, Paul TV, Thomas N, Oldenburg B. Normal weight obesity: an underrecognized problem in individuals of south asian descent. Clin Ther. 2019;41(8):1638–42.
Wulan SN, Westerterp KR, Plasqui G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas. 2010;65(4):315–9.
Kim MK, Han K, Kwon HS, Song KH, Yim HW, Lee WC, et al. Normal weight obesity in korean adults. Clin Endocrinol (Oxf). 2014;80(2):214–20.
Di Renzo L, Bigioni M, Del Gobbo V, Premrov MG, Barbini U, Di Lorenzo N, et al. Interleukin-1 (IL-1) receptor antagonist gene polymorphism in normal weight obese syndrome: relationship to body composition and IL-1 alpha and beta plasma levels. Pharmacol Res. 2007;55(2):131–8.
Jahangiri A, de Beer MC, Noffsinger V, Tannock LR, Ramaiah C, Webb NR, et al. HDL remodeling during the acute phase response. Arterioscler Thromb Vasc Biol. 2009;29(2):261–7.
Lewis GF, Uffelman KD, Szeto LW, Steiner G. Effects of acute hyperinsulinemia on VLDL triglyceride and VLDL apoB production in normal weight and obese individuals. Diabetes. 1993;42(6):833–42.
Galindo-Yllu BM, Rojas-Humpire R, Toro-Huamanchumo CJ, Gutierrez-Ajalcriña R, Soriano AN. Serum Uric Acid Is Associated with Metabolic Syndrome and Insulin Resistance among Health Personnel from Peru. J Nutr Metab. 2021; 2021:9933319. doi: https://doi.org/10.1155/2021/9933319. eCollection 2021.
Hou YL, Yang XL, Wang CX, Zhi LX, Yang MJ, You CG. Hypertriglyceridemia and hyperuricemia: a retrospective study of urban residents. Lipids Health Dis. 2019;18(1):81. https://doi.org/10.1186/s12944-019-1031-6.
Wu J, Zhang YP, Qu Y, Jie LG, Deng JX, Yu QH. Efficacy of uric acid-lowering therapy on hypercholesterolemia and hypertriglyceridemia in gouty patients. Int J Rheum Dis. 2019;22(8):1445–51.
King C, Lanaspa MA, Jensen T, Tolan DR, Sánchez-Lozada LG, Johnson RJ. Uric acid as a cause of the metabolic syndrome. Contrib Nephrol. 2018;192:88–102.
Mori K, Furuhashi M, Tanaka M, Higashiura Y, Koyama M, Hanawa N, et al. Serum uric acid level is associated with an increase in systolic blood pressure over time in female subjects: Linear mixed-effects model analyses. Hypertens Res. 2022;45(2):344–53.
Furuhashi M, Mori K, Tanaka M, Maeda T, Matsumoto M, Murase T, et al. Unexpected high plasma xanthine oxidoreductase activity in female subjects with low levels of uric acid. Endocr J. 2018;65:1083–92.
Yahyaoui R, Esteva I, Haro-Mora JJ, Almaraz MC, Morcillo S, Rojo-Martinez, et al. Effect of long-term administration of cross-sex hormone therapy on serum and urinary uric acid in transsexual persons. J Clin Endocrinol Metab. 2008;93:2230–3.
Nishio S, Maruyama Y, Sugano N, Hosoya T, Yokoo T, Kuriyama S. Gender interaction of uric acid in the development of hypertension. Clin Exp Hypertens. 2018;40:446–51.
Shimodaira M, Niwa T, Nakajima K, Kobayashi M, Hanyu N, Nakayama. Gender differences in the relationship between serum uric acid and mean platelet volume in a japanese general population. Platelets. 2014;25:202–6.
Korniluk A, Koper-Lenkiewicz OM, Kaminska J, Kemona H, Dymicka-Piekarska V. Mean platelet volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediators Inflamm. 2019;2019:9213074.
Coban E, Yazicioglu G, Berkant Avci A, Akcit F. The mean platelet volume in patients with essential and white coat hypertension. 2005;16:435–8.
Kaya MG, Yarlioglues M, Gunebakmaz O, Gunturk E, Inanc T, Dogan A, et al. Platelet activation and inflammatory respose in patients with non-dipper hypertension. Atheroscleosis. 2010;209:278–82.
Nagahama K, Inoue T, Kohagura K, Kinjo K, Ohya Y. Associations between serum uric acid levels and the incidence of hypertension and metabolic syndrome: a 4-year follow-up study of a large screened cohort in Okinawa, Japan. Hypertens Res. 2015;38(3):213–8.
Huang S, Liu X, Li H, Xu W, Jia H. Sex difference in the association of serum uric acid with metabolic syndrome and its components: a cross-sectional study in a chinese Yi population. Postgrad Med. 2017;129(8):828–33.
Bandaru P, Shankar A. Association between serum uric acid levels and diabetes Mellitus. Int J Endocrinol. 2011;2011:604715. https://doi.org/10.1155/2011/604715. Epub 2011 Nov 2.
Oda E, Kawai R, Sukumaran V, Watanabe K. Uric acid is positively associated with metabolic syndrome but negatively associated with diabetes in japanese men. Intern Med. 2009;48(20):1785–91.
Rabari K, Samadhiya A, Saha S, Sharma A, Atif Mirza A, Naithani M. A study to assess serum uric acid level and its association with glycemic parameters in individuals with prediabetes and diabetes mellitus a north indian tertiary care hospital. Yuva J Med Sci. 2018;4(2):12–8.
Nan H, Dong Y, Gao W, Tuomilehto J, Qiao Q. Diabetes associated with a low serum uric acid level in a general chinese population. Diabetes Res Clin Pract. 2007;76(1):68–74.
Tuomilehto J, Zimmet P, Wolf E, Taylor R, Ram P, King H. Plasma uric acid level and its association with diabetes mellitus and some biologic parameters in a biracial population of Fiji. Am J Epidemiol. 1988;127(2):321–36.
Herman JB, Medalie JH, Goldbourt U. Diabetes, prediabetes and uricaemia. Diabetologia. 1976;12(1):47–52.
Pavani CH, Mohanty S, Dharwadkar AA. Hypouricemia in type 2 diabetes mellitus without nephropathy: a case control study. Int J Clin Biochem Res. 2018;5(2):201–5.
Maritim AC, Sanders RA, Watkins JB 3. Diabetes, oxidative stress, and antioxidants: a review. J Biochem Mol Toxicol. 2003;17(1):24–38.
Palanduz S, Ademoğlu E, Gökkuşu C, Tamer S. Plasma antioxidants and type 2 diabetes mellitus. Res Commun Mol Pathol Pharmacol. 2001;109(5–6):309–18.
Memisoğullari R, Taysi S, Bakan E, Capoglu I. Antioxidant status and lipid peroxidation in type II diabetes mellitus. Cell Biochem Funct. 2003;21(3):291–6.
Wang T, Bi Y, Xu M, Huang Y, Xu Y, Li X, et al. Serum uric acid associates with the incidence of type 2 diabetes in a prospective cohort of middle-aged and elderly chinese. Endocrine. 2011;40(1):109–16. https://doi.org/10.1007/s12020-011-9449-2.
Glantzounis GK, Tsimoyiannis EC, Kappas AM, Galaris DA. Uric acid and oxidative stress. Curr Pharm Des. 2005;11:4145–51.
Waring WS. Uric acid: an important antioxidant in acute ischaemic stroke. QJM. 2002;95:691–3.
Suliman ME, Johnson RJ, García-López E, Qureshi AR, Molinaei H, Carrero JJ, et al. J-shaped mortality relationship for uric acid in CKD. Am J Kidney Dis. 2006;48(5):761–71. https://doi.org/10.1053/j.ajkd.2006.08.019.
Kang DH, Park SK, Lee IK, Johnson RJ. Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. J Am Soc Nephrol. 2005;16(12):3553–62. https://doi.org/10.1681/ASN.2005050572.
Kanellis J, Watanabe S, Li JH, Kang DH, Li P, Nakagawa T, et al. Uric acid stimulates monocyte chemoattractant protein-1 production in vascular smooth muscle cells via mitogen-activated protein kinase and cyclooxygenase-2. Hypertension. 2003;41(6):1287–93. https://doi.org/10.1161/01.HYP.0000072820.07472.3B.
Choi BG, Kim DJ, Baek MJ, Ryu YG, Kim SW, Lee MW, et al. Hyperuricaemia and development of type 2 diabetes mellitus in asian population. Clin Exp Pharmacol Physiol. 2018;45(6):499–506.
Yamada T, Fukatsu M, Suzuki S, Wada T, Joh T. Elevated serum uric acid predicts impaired fasting glucose and type 2 diabetes only among japanese women undergoing health checkups. Diabetes Metab. 2011;37(3):252–8.
Joyner JM, Hutley LJ, Cameron DP. Glucocorticoid receptors in human preadipocytes: regional and gender differences. J Endocrinol. 2000;166(1):145–52.
Matsuura F, Yamashita S, Nakamura T, Nishida M, Nozaki S, Funahashi T, et al. Effect of visceral fat accumulation on uric acid metabolism in male obese subjects: visceral fat obesity is linked more closely to overproduction of uric acid than subcutaneous fat obesity. Metabolism. 1998;47(8):929–33.
Quinones Galavan A, Natali A, Baldi S, Frascerra S, Sanna G, Ciociaro D, et al. Effect of insulin on uric acid excretion in humans. Am J Physiol. 1995;268:E1–5.
Acknowledgements
Not applicable.
Funding
This study was supported by research fund from Chosun University, 2021.
Author information
Authors and Affiliations
Contributions
Y.K.K. conceptualized and designed the study, interpreted the results, and drafted the original article. Y.M.Y. conceptualized and designed the study, obtained and analysed the data, interpreted the results, and critically revised the draft. Both authors have read and approved of the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional Review Board of Chosun University which waived the requirement for informed consent (IRB No. 2-1041055-AB-N-01-2022-07). All methods were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, Y.K., Yang, YM. An analysis of the associations of high-sensitivity C-reactive protein and uric acid with metabolic syndrome components in Korean adults by sex: a cross-sectional study using the Korea national health and nutrition examination survey 2016–2018. BMC Endocr Disord 23, 163 (2023). https://doi.org/10.1186/s12902-023-01417-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01417-z