Abstract
Background
Parathyroid carcinoma is a rare disease with a frequency of 0.005% of all malignancies [1, 2]. Various aspects of its pathogenesis, diagnosis, and treatment remain poorly understood. Furthermore, cases with secondary hyperparathyroidism are fewer. In this case report, we describe a case of left parathyroid carcinoma with secondary hyperparathyroidism.
Case presentation
The patient was a 54-year-old woman who had been on hemodialysis since the age of 40 years. At 53 years of age, her calcium levels were high, and she was diagnosed with drug-resistant secondary hyperparathyroidism and was referred to our hospital for surgical treatment. Blood tests revealed calcium levels of 11.4 mg/dL and intact parathyroid hormone (PTH) levels of 1007 pg/mL. Neck ultrasonography revealed a 22-mm large round hypoechoic mass, partially indistinct margins, and D/W ratio > 1 at the left thyroid lobe. Computed tomography scans revealed a 20-mm nodule at the left thyroid lobe. No enlarged lymph nodes or distant metastases were noted. 99mTc-hexakis-2-methoxyisobutylisonitrile scintigraphy revealed an accumulation at the superior pole of the left thyroid lobe. Laryngeal endoscopy revealed paralysis of the left vocal cord, signifying recurrent nerve palsy due to parathyroid carcinoma. Based on these results, a diagnosis of secondary hyperparathyroidism and suspected left parathyroid carcinoma was made, and the patient underwent surgery. Pathology results revealed hyperplasia in the right upper and lower parathyroid glands. The left upper parathyroid gland showed capsular and venous invasion, and the diagnosis was left parathyroid carcinoma. At 4 months post-surgery, calcium levels improved to 8.7 mg/dL and intact PTH levels to 20 pg/mL, with no signs of recurrence.
Conclusions
We report a case of left parathyroid carcinoma associated with secondary hyperparathyroidism. Concomitant secondary hyperparathyroidism may cause mild hypercalcemia compared to parathyroid carcinoma alone due to the added modification of dialysis. Although our patient also presented with mild hypercalcemia, a D/W ratio > 1 on preoperative echocardiography and presence of recurrent nerve palsy on laryngoscopy led to the suspicion and treatment of parathyroid carcinoma preoperatively.
Similar content being viewed by others
Background
Parathyroid carcinoma is a rare disease with a frequency of 0.005% of all malignancies [1, 2]. Various aspects of its pathogenesis, diagnosis, and treatment remain poorly understood. Parathyroid carcinoma typically presents as a nodule and should therefore be differentiated from parathyroid adenoma, parathyroid or thyroglossal cyst, multinodular goiter, thyroiditis, thyroid adenoma and carcinomas [3]. Although puncture aspiration cytology or needle biopsy of a tumor is an important diagnostic test, if the tumor is parathyroid carcinoma, those tests are contraindicated, as they cause spread of cancer cells when the capsule is damaged. Hypercalcemia is an important finding in the diagnosis of parathyroid carcinoma, serum calcium levels are > 12 mg/dL or more than 3-4 mg/dL above the upper limit of normal range. However, very rare cases of secondary parathyroid function should be noted, as they are modified by dialysis. In this case report, we describe a case of left parathyroid carcinoma with secondary hyperparathyroidism.
Case presentation
Patient characteristics
The case was a 54-year-old woman, referred to our department for hypercalcemia. Her past medical history included chronic renal failure (maintenance dialysis), hypertension, and hyperuricemia. No significant family history was noted. The patient had been on hemodialysis since the age of 40 years. In April 2020 (at the age of 53 years), poor control of blood calcium levels was observed, and high-dose maxacalcitol was commenced in October 2020, but no improvement was observed. In December 2020, she was referred to her previous doctor with a diagnosis of drug-resistant secondary hyperparathyroidism and was referred to our hospital for close examination and treatment.
On admission, the patient had a height of 155.0 cm, weight of 56.7 kg, body mass index of 23.6 kg/m2, and no palpable mass in the neck. Her blood test results are presented in Table 1. High creatinine (8.73 mg/dL), calcium (11.4 mg/dL), phosphorus (9.2 mg/dL), and intact parathyroid hormone (PTH) levels (1007 pg/mL) were observed. Neck ultrasonography revealed a hypoechoic mass measuring 30.3 × 23.7x21.8 mm in size with irregular and partly indistinct margins, D(23.7)/W(21.8) ratio > 1, and abundant blood flow at the dorsal surface of the left thyroid lobe, outside the capsule (Fig. 1). A 10-mm large well-defined hypoechoic mass was observed at the dorsal surface of the right thyroid lobe, outside the capsule.
Imaging findings
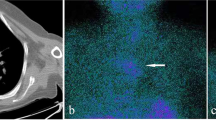
Cervical computer tomography (CT) scan revealed a 20-mm nodule at the dorsal surface of the left thyroid lobe and a 10-mm enlarged parathyroid gland at the dorsal surface of the right thyroid lobe. 99mTc-hexakis-2-methoxyisobutylisonitrile scintigraphy revealed an accumulation at the upper pole of the left thyroid gland (Fig. 2). Laryngeal endoscopy revealed paralysis of the left vocal cord (median fixation).
Treatment plan
Based on the test results, we suspected secondary hyperparathyroidism with left parathyroid carcinoma, leading us to perform total parathyroidectomy, peritracheal lymph node dissection, combined thyroidectomy, left recurrent nerve resection and reconstruction (left recurrent nerve – ansa cervicalis), and autograft of the parathyroid to right upper arm in February 2021 (Fig. 3).
Surgical findings
The left upper parathyroid tumor was located 10 mm centrally from the left recurrent nerve and invading inwards circumferentially. We thus excised the left thyroid lobe, including the recurrent nerve, and reconnected it with the ansa cervicalis with two stitches of 6–0 Proline(Johnson & Johnson, City of New Brunswick, USA) and Beriplast(CSL Behring, King of Prussia, USA).
Postoperative course
The anterior cervical drain was removed at postoperative day (POD) 2, and the patient was discharged at POD 3 without complications.
Pathology results
Macroscopic pathology analysis revealed a left thyroid lobe measuring 59 × 30 × 20 mm, including a milky white substantial mass measuring 18 × 13 × 18 mm in the upper pole. The left lower parathyroid gland was normal (Fig. 4a). We were unable to measure the left parathyroid due to cancer invasion. The right upper and lower parathyroid glands were 15 × 12 × 7 mm and 7 × 7 × 7 mm in size and weighed 450 mg and 90 mg, respectively.
Pathological specimens. a (macro): Left thyroid lobe including a milky white substantial mass measuring 18 × 13 × 18 mm in the upper pole. b (hematoxylin & eosin [HE] stain): Large round nucleus, fenestrated-to-dense growth of principal cells with pale acidophilic cytoplasm, and a fibrous capsule covering the mass. Acidophilic cells with acidophilic cytoplasm proliferating in a fenestrated-to-dense manner are observed. c (Elastin van Gieson [EVG] stain): EVG stain showed some venous invasion
Microscopic pathology analysis revealed that the left upper mass consisted of a large round nucleus, fenestrated to dense growth of principal cells with pale acidophilic cytoplasm, and a fibrous capsule covering the mass. We observed acidophilic cells with acidophilic cytoplasm proliferating in a fenestrated to dense manner (Fig. 4b). Some parts of the lesion appeared to proliferate beyond the fibrous capsule. Elastin van Gieson staining revealed venous infiltration in some areas, suggesting vascular invasion (Fig. 4c); therefore, the diagnosis was parathyroid carcinoma. No lymph node metastasis was observed(0/1). The other parathyroid glands exhibited nodular proliferation of principal cells and eosinophilic cells forming a fenestrated to follicular structure. No obvious normal rim was noted at the specimen margins. The diagnosis was hyperplasia of the right upper and lower parathyroid gland.
Postoperative outpatient course
At 1 month postoperatively, calcium and iPTH levels were 9.5 mg/dL and 15 pg/mL, respectively, with no subsequent increase. At 25 months postsurgery, no apparent evidence of recurrence was observed. Table 2 shows pre and postoperative calcium and iPTH levels.
Discussion and conclusions
Parathyroid carcinoma is a rare disease, accounting for only 0.005% of all cancers and 0.3–5.6% of primary hyperparathyroidism. Various aspects of its pathogenesis, diagnosis, and treatment remain poorly understood [1, 2]. Moreover, puncture aspiration cytology and needle biopsy are contraindicated, as they cause spread of cancer cells when the capsule is damaged, rendering it difficult to make a definitive diagnosis before surgery. Characteristic clinical findings include palpation of neck mass (sensitivity of 50% and specificity of 100%), generalized fibrous osteitis (sensitivity of 50% and specificity of 38%), and serum calcium levels > 12 mg/dL (sensitivity of 83% and specificity of 69%) [4,5,6,7,8,9]. Other findings suggestive of parathyroid carcinoma include the D/W ratio on neck ultrasonography and invasion of the thyroid gland and recurrent nerve [8]. In the case reported herein, none of the aforementioned clinical features was present. Although the D/W ratio was > 1, and recurrent nerve palsy was observed, we were able to remove the tumor without exposing it by suspecting parathyroid carcinoma preoperatively.
With regard to pathological diagnosis, parathyroid carcinoma is often grayish-white, hard, and has a gross irregular shape. The four histological diagnosis criteria proposed by Schantz and Castleman are (1) formation of a thick fibrous capsule within the tumor, (2) fenestrated arrangement of tumor cells, (3) nuclear fission image, and (4) capsular or vascular invasion [10]. However, as the first three features are also observed in adenomas, it is difficult to differentiate parathyroid adenomas from carcinomas based solely on histopathological findings [11]. To distinguish parathyroid adenomas and carcinomas, blood test findings may be useful. In parathyroid carcinoma, serum calcium levels are > 12 mg/dL or more than 3–4 mg/dL above the upper limit of normal range. In contrast, in parathyroid adenoma, calcium levels are only 1 mg/dL above the upper limit. Serum PTH levels also differ between parathyroid carcinomas and parathyroid adenomas. In parathyroid carcinoma, serum PTH levels are 3–10 times the upper limit of normal range, whereas in parathyroid adenoma, serum PTH levels are rarely more than twice the upper limit of normal range [12]. In this case, the serum calcium level was not above 12 mg/dl, partly due to hemodialysis.
Only 37 cases of parathyroid carcinoma associated with secondary hyperparathyroidism have been reported in the English literature since Berland et al.’s report in 1982 [13]. The 37 cases are summarized in Table 3 [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. The mean age of the patients was 50.5 years. Of these cases, 18 were men and 18 were women (one has no gender indicated in the text), indicating approximately equal sex distribution. Regarding the three clinical features listed above, only one case (no other description) presented with a palpable neck mass, 17 cases (65.4%) exhibited symptoms suggestive of fibrotic osteitis, and 25 cases (80.6%) presented with serum calcium levels > 12 mg/dL. PTH levels were high in 29 patients (100%), although measurement methods differed in some cases. In patients with parathyroid carcinoma associated with secondary hyperparathyroidism undergoing dialysis, the characteristic clinical findings observed only in parathyroid carcinoma do not necessarily apply due to the additional modifications caused by dialysis.
Table 4 presents a comparison of the age, sex ratio, serum calcium level, PTH level, and presence of bone lesions in patients with and without secondary hyperparathyroidism [47,48,49]. No obvious differences were noted in age, sex ratio, PTH level, or presence of bone lesions between groups. Serum calcium levels were lower in patients with than in those without secondary hyperparathyroidism, presumably due to the removal of calcium by hemodialysis. In addition, hypercalcemia is also observed in 20–30% of patients with malignancies other than parathyroid carcinoma, caused by the release of PTHrP(parathyroid hormone-related peptide) [50]. For these reasons, imaging tests are crucial when parathyroid carcinoma is suspected. In many cases, CT scans were performed for uncontrolled hypercalcemia, and large nodules were observed around the thyroid gland, leading to surgical resection. However, it is difficult to distinguish between an adenoma and cancer based on the size of the parathyroid gland on CT. In several cases, a malignant tumor was observed in the postoperative pathology results after a preoperative diagnosis of secondary hyperparathyroidism only. If parathyroid carcinoma is not suspected preoperatively, it may be disseminated as described above. Therefore, we were able to resect the tumors while considering the risk of dissemination.
In conclusion, we report a very rare case of left parathyroid carcinoma associated with secondary hyperparathyroidism. D/W ratio > 1 on preoperative echocardiography and presence of recurrent nerve palsy on laryngoscopy led to the suspicion and treatment of parathyroid carcinoma preoperatively.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- POD:
-
Postoperative day
- PTH:
-
Parathyroid hormone
References
Rahbari R, Kebebew E. Parathyroid tumors. In: Cancer: Principles and Practice of Oncology. 9th ed. DeVita VT Jr, Lawrence TS, Rosenberg SA, editors. Lippincott Williams & Wilkins; 2011. p. 1473–9.
Hundahl SA, Fleming ID, Fremgen AM, Menck HR. Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985-1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1999;86:538–44.
Francesk M, Fatima A. Thyroid Adenoma. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
Levin KE, Galante M, Clark OH. Parathyroid carcinoma versus parathyroid adenoma in patients with profound hypercalcemia. Surgery. 1987;101:649–60.
Stojadinovic A, Hoos A, Nissan A, Dudas ME, Cordon-Cardo C, Shaha AR, et al. Parathyroid neoplasms: clinical, histopathological, and tissue microarray-based molecular analysis. Hum Pathol. 2003;34:54–64.
Lumachi F, Ermani M, Marino F, Poletti A, Basso SM, Iacobone M, et al. Relationship of AgNOR counts and nuclear DNA content to survival in patients with parathyroid carcinoma. Endocr Relat Cancer. 2004;11:563–9.
Mann GN, Trombetti A, Garcia A. Less is (usually) more: when is amputation appropriate for treatment of extremity soft tissue sarcoma? Ann Surg Oncol. 2005;12:1–2.
Hara H, Igarashi A, Yano Y, Yashiro T, Ueno E, Aiyoshi Y, et al. Ultrasonographic features of parathyroid carcinoma. Endocr J. 2001;48:213–7.
Okamoto T, Ohara T, Fujimoto Y. Preoperative diagnosis of epithelioid body cancer: quantitative evaluation of preoperative information. Endocr Surg. 1991;8:401–5.
Schantz A, Castleman B. Parathyroid carcinoma. A study of 70 cases. Cancer. 1973 31 600-5.
Agarwal G, Prasad KK, Kar DK, Krishnani N, Pandey R, Mishra SK. Indian primary hyperparathyroidism patients with parathyroid carcinoma do not differ in clinicoinvestigative characteristics from those with benign parathyroid pathology. World J Surg. 2006;30(5):732–42.
Salcuni AS, Cetani F, Guarnieri V, Nicastro V, Romagnoli E, Martino D, et al. Parathyroid carcinoma. Best Pract Res Clin Endocrinol Metab. 2018;32:877889.
Berland Y, Olmer M, Lebreuil G, Grisoli J. Parathyroid carcinoma, adenoma and hyperplasia in a case of chronic renal insufficiency on dialysis. Clin Nephrol. 1982;18:154–8.
Anderson BJ, Samaan NA, Vassilopoulou-Sellin R, Ordonez NG, Hickey RC. Parathyroid carcinoma: features and difficulties in diagnosis and management. Surgery. 1983;94:906–15.
Ireland JP, Fleming SJ, Levison DA, Cattell WR, Baker LR. Parathyroid carcinoma associated with chronic renal failure and previous radiotherapy to the neck. J Clin Pathol. 1985;38:1114–8. https://doi.org/10.1136/jcp.38.10.1114.
Sherlock DJ, Newman J, Holl-Allen RT. Parathyroid carcinoma presenting as tertiary hyperparathyroidism. Postgrad Med J. 1985;61:243–4.
Krishna GG, Mendez M, Levy B, Ritchie W, Marks A, Narins RG. Parathyroid carcinoma in a chronic hemodialysis patient. Nephron. 1989;52:194–5.
Kodama M, Ikegami M, Imanishi M, Uemura T, Takada M, Kohri K, et al. Parathyroid carcinoma in a case of chronic renal failure on dialysis. Urol Int. 1989;44:110–2.
Iwamoto N, Yamazaki S, Fukuda T, Kondo M, Yamamoto N, Ono T, et al. Two cases of parathyroid carcinoma in patients on long-term hemodialysis. Nephron. 1990;55:429–31.
Rademaker P, Meijer S, Oosterhuis JW, Vermey A, Zwierstra R, vd Hem G, et al. Successful surgical treatment of parathyroid carcinoma in two haemodialysis patients. Nephrol Dial Transplant. 1990;5:545–8.
Tominaga Y, Numano M, Uchida K, Sato K, Asano H, Haba T, et al. Lung metastasis from parathyroid carcinoma causing recurrent renal hyperparathyroidism in a hemodialysis patient: report of a case. Surg Today. 1995;25:984–6.
Miki H, Sumitomo M, Inoue H, Kita S, Monden Y. Parathyroid carcinoma in patients with chronic renal failure on maintenance hemodialysis. Surgery. 1966;120:897–901.
Liou MJ, Lin JD, Huang MJ, Huang JY, Hsueh C, Jeng LB. Parathyroid carcinoma with postoperative prolonged hypocalcemia in a patient with chronic renal failure. J Formos Med Assoc. 1996;95:337–41.
Tseng CC, Huang JJ, Wang MC, Lan RR, Sung JM, Chen FF. Parathyroid carcinoma with multiple lung metastases. Nephrol Dial Transplant. 1999;14:449–51.
Takami H, Kameyama K, Nagakubo I. Parathyroid carcinoma in a patient receiving long-term hemodialysis. Surgery. 1999;125:239–40.
Jayawardene S, Owen WJ, Goldsmith DJ. Parathyroid carcinoma in a dialysis patient. Am J Kidney Dis. 2000;36:E26.
Kuji T, Kitamura H, Yasuda G, Umemura S, Kimura T, Shimizu S, et al. Different pathological findings in each of four parathyroid glands in a long-standing hemodialysis patient. Clin Nephrol. 2000;54:413–7.
Zivaljevic V, Krgovic K, Tatic S, Havelka M, Dimitrijevic Z, Diklic A, et al. Parathyroid cancer in a hemodialysis patient: a case report. Tumori. 2002;88:430–2.
Srouji IA, Resouly IA, Cree IA. Case of thymic parathyroid carcinoma in a hemodialysis patient: application of tumor chemosensitivity testing. J Laryngol Otol. 2004;118:162–4.
Khan MW, Worcester EM, Straus FH, Khan S, Staszak V, Kaplan EL. Parathyroid carcinoma in secondary and tertiary hyperparathyroidism1. J Am Coll Surg. 2004;199:312–9. https://doi.org/10.1016/j.jamcollsurg.2004.04.014.
Bossola M, Tazza L, Ferrante A, Giungi S, Carbone A, Gui D, et al. Parathyroid carcinoma in a chronic hemodialysis patient: case report and review of the literature. Tumori. 2005;91:558–62.
Babar-Craig H, Quaglia A, Stearns M. Parathyroid carcinoma: a report of two cases and a concise review and update of the literature. J Laryngol Otol. 2005;119:577–80. https://doi.org/10.1258/0022215054352261.
Falvo L, Catania A, Palermo S, Sorrenti S, Bonifazi AP, De Stefano M, et al. Bilateral synchronous parathyroid carcinoma in a patient on long-term hemodialysis: presentation of a rare clinical case and review literature. Int Surg. 2005;90:18–22.
Tkaczyk M, Czupryniak A, Nowicki M. Ectopic mediastinal parathyroid carcinoma as a cause of dialysis-dependent renal failure. Hemodial Int. 2007;11:398–402. https://doi.org/10.1111/j.1542-4758.2007.00207.x.
Diaconescu MR, Glod M, Costea I, Grigorovici M, Covic A, Diaconescu S. Surgical management of renal hyperparathyroidism: a preliminary series report. Chirurgia (Bucur). 2011;106:51–7.
Nasrallah MP, Fraker DL, Livolsi VA. Parathyroid carcinoma in the setting of tertiary hyperparathyroidism after renal transplant. Endocr Pathol. 2014;25:433–5. https://doi.org/10.1007/s12022-014-9336-5.
Kim BS, Ryu HS, Kang KH, Park SJ. Parathyroid carcinoma in tertiary hyperparathyroidism. Asian J Surg. 2016;39:255–9. https://doi.org/10.1016/j.asjsur.2013.01.007.
Pappa A, Hackman T. Simultaneous incidental parathyroid carcinoma and intrathyroid parathyroid gland in suspected renal failure induced hyperparathyroidism. Surg J (N Y). 2017;3:e23–4. https://doi.org/10.1055/s-0037-1599072.
Curto LS, Gervasi R, Caracciolo F, Innaro N. Parathyroid carcinoma presenting with chronic renal failure and single pulmonary metastasis: a case report. Int J Surg Case Rep. 2019;65:322–4. https://doi.org/10.1016/j.ijscr.2019.10.086.
Shen Y, Fei P. Refractory hypercalcemia due to an ectopic mediastinal parathyroid gland in a hemodialysis patient: a case report. BMC Nephrol. 2019;20:165. https://doi.org/10.1186/s12882-019-1363-5.
Won HR, Kang JY, Lee IH, Kim JM, Chang JW, Koo BS. Parathyroid carcinoma arising from auto-transplanted parathyroid tissue after total parathyroidectomy in chronic kidney disease patient: a case report. BMC Nephrol. 2019;20:414. https://doi.org/10.1186/s12882-019-1606-5.
Cappellacci F, Medas F, Canu GL, Lai ML, Conzo G, Erdas E, et al. Parathyroid carcinoma in the setting of tertiary hyperparathyroidism: case report and review of the literature. In: Case Rep Endocrinol. Boyanov, MA, et al., editor. 2020;2020:5710468.https://doi.org/10.1155/2020/5710468.
Malipedda S, Kamaleshwaran KK, Muthusamy D, Veerasamy M, Soundararajan AP, Jayaraj AV. Rare imaging findings of concomitant presence of multiple parathyroid adenomas and carcinoma in a chronic kidney disease patient with tertiary hyperparathyroidism detected on 99 m Tc-sestamibi single-photon-emission computed tomography/computed tomography scintigraphy. Indian J Nucl Med. 2020;35:333–5. https://doi.org/10.4103/ijnm.IJNM_100_20.
Kada S, Tanaka M, Yasoda A. Parathyroid carcinoma in a patient with secondary hyperparathyroidism and thyroid hemiagenesis: a case report and review of the literature. Ear Nose Throat J. 2021;1455613211036240. doi: https://doi.org/10.1177/01455613211036240.
Chen, Simei, Sui, Xin, Zhao, Bingxin, Liu, Zongjie, Dai, Xinpeng, Ding, Yang. A case report of secondary parathyroid adenomatous hyperplasia with carcinoma. Medicine 101(46):p e31362, November 18, 2022. https://doi.org/10.1097/MD.0000000000031362.
Petru R, Dragos G, Anca T, Mihai Z, Vlad P, Mircea B, Mircea L, Virgil P, Valentin G, Florian P, Valeriu S, Victor S. Parathyroid Cancer-A Rare Finding during Parathyroidectomy in High Volume Surgery Centre. Medicina. 2023;59(3):448. https://doi.org/10.3390/medicina59030448.
Yu Y, Wang Y, Wu Q, Zhao X, Liu D, Zhao Y, et al. Case report and systematic review: sarcomatoid parathyroid carcinoma-A rare, highly malignant subtype. Front Endocrinol. 2021;12:793718. https://doi.org/10.3389/fendo.2021.793718.
Lafferty FW. Primary hyperparathyroidism. Changing clinical spectrum, prevalence of hypertension, and discriminant analysis of laboratory tests. Arch Intern Med. 1981;141:1761–6.
Nikkilä MT, Saaristo JJ, Koivula TA. Clinical and biochemical features in primary hyperparathyroidism. Surgery. 1989;105:148–53.
Stewart AF. Clinical practice. Hypercalcemia associated with cancer. N Engl J Med. 2005;352:3739–379.
Acknowledgements
We would like to thank Dr Suganuma for useful discussions.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KY analyzed and interpreted the patient data regarding parathyroid carcinoma and secondary hyperparathyroidism. NS was the surgeon and major contributor in writing the manuscript. YR helped KY draft the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. The patient provided written informed consent for data collection.
Consent for publication
Written Informed consent was also obtained from the patient for publication of this case report. “I understand that the text and any pictures published in the article will be freely available on the internet and may be seen by the general public.”
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yokoyama, K., Suganuma, N. & Rino, Y. Left parathyroid carcinoma with secondary hyperparathyroidism: a case report. BMC Endocr Disord 23, 108 (2023). https://doi.org/10.1186/s12902-023-01370-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01370-x