Abstract
Background
Data is inconsistent and, for the most part, not sufficient to demonstrate the association between serum Prolactin (PRL) concentration within the physiologic range and the incidence rate of type 2 Diabetes Mellitus (DM) among men. Moreover, since both PRL and type 2 DM are associated with reproductive hormones, investigating these hormones might improve our understanding of how PRL might impose its effect on the incidence rate of type 2 DM.
Methods
For the present study, 652 eligible men aged 29–70 with a normal baseline PRL concentration were selected from the Tehran Lipid and Glucose Study (TLGS). Participants were sub-classified into three groups (tertiles) according to the serum concentration of PRL and were followed for 15.8 years. The incidence of type 2 DM and PRL, LH, FSH, testosterone, and AMH concentrations were measured. The effect of hormonal variables on the incidence of type 2 DM was estimated using the log-binomial model, adjusted for major confounding factors. The correlations between PRL and the indicators of glucose and lipid metabolism and other hormonal variables were also explored.
Results
In the unadjusted model, PRL was not significantly associated with the incidence rate of type 2 DM (RR = 0.98, 95% CI: 0.94 − 1.03). After adjusting for potential confounders, the inverse effect of AMH on the incidence rate of type 2 DM was the only significant association. The analyses also indicated a significant positive association between PRL and LH/FSH ratio (r = 0.1, P = 0.01).
Conclusion
No significant association was found between serum PRL concentrations within the physiologic range and the incidence rate of type 2 diabetes mellitus among middle-aged men. Men with higher concentrations of PRL within the physiologic range tended to show higher levels of LH and LH/FSH. AMH was the only variable significantly linked to the incidence rate of type 2 DM in men.
Similar content being viewed by others
Background
Prolactin (PRL) is a polypeptide pituitary hormone primarily known for its lactogenic role in mammals [1, 2]. PRL receptors are expressed in multiple organs and are involved in many physiologic functions, including osmoregulation, immune response, growth and development, brain function, reproduction, and metabolism [2,3,4]. According to preclinical studies, it is evident that serum PRL concentrations within the physiologic range contribute to maintaining normal glucose homeostasis in both sexes [5,6,7]. To elucidate, PRL enhances the proliferation of pancreatic beta cells, increases glucose-dependent insulin secretion, and prevents pancreatic islet apoptosis. As a result, serum PRL concentrations within the physiologic range might reduce the risk of developing type 2 Diabetes Mellitus (DM) [5,6,7]. In this context, it has been shown that higher than-normal serum concentrations of PRL (hyperprolactinemia) lead to insulin resistance and glucose intolerance [8, 9]. In addition, the symptomatic state of excess PRL that could be developed via hypothalamic-pituitary axis disorders or drugs -referred to as pathologic hyperprolactinemia- increases post-prandial insulin resistance. This process leads to increased gluconeogenesis together with lipolysis and impairment of peripheral glucose uptake [8,9,10,11]. Furthermore, hyperprolactinemia results in abnormal fatty acid metabolism and an aggravated inflammatory state, leading to increased food intake, weight gain, and insulin resistance [12,13,14,15]. Therefore, hyperprolactinemia (pathologic or not) might increase the risk of type 2 DM [9, 16]. As a result, PRL has contradictory effects on metabolism; while its concentrations within the physiologic range seem metabolically beneficial, its pathological concentrations have a detrimental effect on metabolism.
Several studies reported a significant inverse association between serum PRL concentration within the physiologic range and the risk of type 2 DM [17,18,19,20,21]. Nonetheless, the literature is inconsistent concerning the association between serum PRL concentrations within the physiologic range and the risk of type 2 DM among men, pointed out in a recent meta-analysis [22]. Although cross-sectional studies have reported a significant association between higher quartiles of serum PRL concentration within the physiologic range and lower risk of type 2 DM in both sexes [19, 20, 23], and large-scale longitudinal studies have demonstrated this association among women [17, 18], data is inconsistent and for the most part not sufficient to establish this association among men [18, 22, 23]. Another possible scenario contributing to this debate is that PRL concentrations within the physiologic range might have a sex-specific effect on glucose metabolism [24, 25]. On the one hand, previous research suggests an association between the risk of type 2 DM and reproductive hormones such as LH, FSH, testosterone, and AMH [26,27,28,29]. On the other hand, PRL appears to play a sex-specific role in reproduction and fertility alongside these hormones [30]. Thus, investigating the relationships between PRL and other reproductive hormones might help to explain why men and women have different interactions between PRL and type 2 DM. The paucity of studies properly equipped to answer these questions in the population of men prompted us to conduct a study on a dataset from a large long-term community-based cohort, the Tehran Lipid and Glucose Study (TLGS), to determine whether various concentrations of serum PRL within the physiologic range affect the incidence rate of type 2 DM among men, and to investigate the possibility of involvement of other reproductive hormones in the mechanisms at work.
Methods
Study population
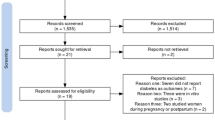
The sample for the present study was selected from the male participants of the Tehran Lipid and Glucose Study (TLGS). TLGS is an ongoing large-scale community-based multi-center cohort study initiated in the late 1990s to assess the incidence, prevalence, and risk factors of non-communicable diseases (NCDs) and metabolic disturbances among 3–69 years old residents of a district in Tehran, Iran, using a multistage stratified cluster random sampling technique. From the start, the participants have been followed up in visits three years apart, undergoing complete medical history and anthropometric data acquisition, blood sampling for biochemical tests of serum glucose and lipids, and outcome measurements. Further details of TLGS have been published elsewhere [31].
Selection criteria
For the present study, we selected all men aged 29–70 who participated in phase 1 of TLGS and had their serum PRL concentration measured. At baseline, all men who had a previous diagnosis of diabetes mellitus (n = 99) or serum PRL concentration of more than 20 ng/ml (n = 50) were excluded from the study, as well as participants who failed to attend any follow-up sessions (n = 27). Any participant taking medications known to elevate serum PRL concentration, such as first and second-generation antipsychotics, cyclic antidepressants, antihypertensives, antihistamines, and antiemetics like Metoclopramide, anyone with persistent headaches that could be suspicious of pituitary adenoma or hypothalamus tumor, cases of chronic renal failure or macroprolactinemia, cases of chest-wall injuries, those taking medications known to alter metabolic parameters, such as insulin, sulfonylurea and thiazolidinediones, beta-blockers and calcium-channel blockers, psychotropic and anti-seizure drugs, lipid-lowering drugs and corticosteroids were all excluded, which left us with a total of 652 eligible healthy men.
The protocol of the present study was designed according to the principles of the Helsinki declaration and was approved by the Ethics committee of the Research Institute for Endocrine Sciences (IR.SBMU.ENDOCRINE.REC.1400.082). Informed written consent was obtained from each participant after providing them with complete descriptions of the study. STROBE reporting guidelines for observational studies were used to design and report the present study.
Clinical, anthropometric, and laboratory measurements
Details of the measurements have been previously published [31]. Briefly, at baseline and each follow-up session, participants filled out a standard questionnaire regarding their complete medical and family history with the help of two trained physicians. Moreover, they underwent a brief physical examination, including a measurement of their anthropometrics such as weight, standing height, waist circumference (WC), hip circumference (HC), and wrist circumference (WrC). Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2), and waist-to-hip ratio (WHR) was calculated by dividing WC (cm) by HC (cm).
Venous blood samples were taken without excessive venepuncture stress from participants in the morning after 12–14 h of overnight fasting and 2–3 h after waking up, centrifuged for 30–45 min, and stored in -80 °C ultra-freezers until further testing. Fasting plasma glucose (FPG) was measured with the Glucose oxidase technique (Glucose kit, Pars Azmun, Tehran, Iran) in enzymatic colorimetric method, with inter- and intra-assay coefficients of variations (CV) of 2.2% both. A 2-h postprandial glucose test with 75 g glucose was administered for participants who did not use any glucose-lowering medications. Total cholesterol (TC), triglyceride (TG), and high-density lipoprotein (HDL) cholesterol concentrations were measured using an enzymatic colorimetric test (Pars Azmun kit, Tehran, Iran). Low-density lipoprotein (LDL) cholesterol was calculated using the Friedwald formula [32]. Measurement of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and PRL were based on Immunoradiometric assay (IRMA) using a gamma counter (Izotop, Budapest, Hungary, gamma counter: Dream Gamma- 10, Goyang-si, Gyeonggi-do, South Korea). The intra- and inter-assay coefficients of variations (CVs) for LH, FSH and PRL were 2.9% and 3.0%, 1.3% and 1.4%, 2.5% and 2.6%, respectively, at the detection limit of 0.02 mIU/mL, 0.08 mIU/mL and 0.04 ng/mL, respectively. Total AMH concentration was assayed using enzyme immunoassay (EIA) (AMH Gen Π, Beckman Coulter, Inc. Ca, USA, Sunrise, Tecan Co. Salzburg, Austria), with intra- and inter-assay CVs of 3.1% and 3.2%, respectively, at the detection limit of 0.08 ng/ml. Total testosterone concentration was measured using EIA (DRG Instrument, Sunrise, Tecan Co. Salzburg, Austria, GmbH, Germany), with intra- and inter-assay CVs of 5.7% and 8.4%, respectively, at the detection limit of 0.002 ng/ml. All measurements were carried out at the laboratory of the Research Institute for Endocrine Sciences (RIES).
Definitions
The normal range of serum PRL concentration in an adult male is 3 to 13 ng/ml, which is lower than an adult female [33]. However, since various methods and kits are used to measure PRL, there is some variation in the ranges reported by different laboratories. Based on the detection methods used in our laboratories, the normal/physiologic range of serum PRL concentration was set from 3 to 20 ng/ml. Hyperprolactinemia is a condition where serum PRL concentration exceeds the upper limit of the normal range [34].
Type 2 diabetes mellitus (DM) was diagnosed in the participants who met at least one of the criteria of the American Diabetes Association’s definition of diabetes [35]: 2-h PCPG ≥ 11.1 mmol/L OR FPG ≥ 7 mmol/L OR using any anti-diabetic medication. Also, those with FPG < 5.05 mmol/L and missing data on the 2-hpp glucose test at follow-up were defined as non-diabetic [36]. In addition, they did not have any early symptoms of insulin deficiency, autoimmune-related disease, or any history of type 1 DM in a first-degree relative. Family history of type 2 DM was defined as having at least one first-degree relative diagnosed with type 2 DM.
In our dataset, physical activity was measured using the Modifiable Activity Questionnaire (MAQ), including leisure time, job, and household activities. Appropriate physical activity was defined as more than 600 min of moderate physical activity within a week.
Statistical analysis
The present study has a power of 80% to detect 0.45% risk reduction in type 2 DM outcome, with a two-sided 5% significance level, and a sample size of 652 male participants. Continuous variables were checked for normal distribution using the one-sample Kolmogorov-Smirnoff test. Categorical variables were expressed as percentages, whereas continuous variables with normal distribution were expressed as mean ± standard deviation (SD), and non-normal distributed variables were expressed as median with interquartile range (IQR 25%– 75%). Participants were sub-classified into three groups according to the serum concentration of PRL. Characteristics of the participants at baseline and last follow-up were compared between the tertiles of PRL, by applying the ANOVA or chi-square test for continuous and categorical data, respectively. Last follow-up was considered a visit at which participants experienced either a DM outcome or the last follow-up in which they have been censored. Bonferroni post-hoc test after ANOVA was applied when an overall statistically significant difference in group means was observed. The Kruskal–Wallis test was applied to compare variables with skewed distribution. After a significant Kruskal–Wallis, Dunn test was used in order to make pairwise comparisons. Furthermore, the incidence rate ratio (IRR) of DM per 1000 persons as well as 95% confidence intervals were estimated in each tertile of PRL.
A scatter plot matrix was drawn, and Spearman’s correlation test was used to explore the correlation between PRL and LH, FSH, LH/FSH, testosterone, and AMH, as well as indicators of glucose and lipid metabolism at the baseline of the study. The effect of hormonal variables on binary type 2 DM outcome was estimated using the log-binomial model, which is a useful approach for computing relative risks [37]. Both unadjusted and adjusted models were fitted, and effect measures (relative risks [RRs]) were calculated with 95% confidence intervals. Based on the literature, potential confounding variables were considered to be age, BMI, smoking status, and family history of DM [22]. Moreover, to check if the effect of PRL on DM depends on the value of hormonal variables, an interaction term between PRL and each hormonal variable was added to the log-binomial model. The Cox regression model was applied to explore the effect of PRL on the age at the onset of diabetes, and hazard ratios were estimated. Statistical analyses were performed using the STATA software package (version 13; STATA Inc., College Station, TX, USA). The significance level was set at P < 0.05 and the confidence interval at 95%.
Results
The characteristics of the study participants at baseline and last follow-up according to their serum concentration of PRL are presented in Table 1. The mean follow-up was 15.8 years (IQR: 13.6 − 17.2). Of all participants, 112 men (17%) were diagnosed with type 2 DM in the course of the study. Age at DM onset was 58 (51 − 67), 56 (51 − 69), and 53.5 (47 − 63) years in the first, second and third PRL tertile, respectively (P = 0.2).
There was no significant difference in various parameters across tertiles of PRL except for LH and LH/FSH ratio. Men with PRL within tertile three, compared separately to those with PRL within tertile two and one, had higher LH concentrations and higher LH/FSH ratios (Table 1). Point estimates and confidence intervals for the incidence rate ratio (IRR) of DM per 1000 persons in tertile 1, 2, and 3 were 2.6 (95% CI 1.9–3.7), 3.3 (95% CI 2.5–4.5), and 2.5 (95% CI 1.7–3.6), respectively. Differences in IRRs of DM between tertiles were not statistically significant (P = 0.15).
The associations between PRL and other hormones, as well as indicators of glucose and lipid metabolism, are presented based on the baseline data in Fig. 1, indicating a slightly significant positive association between PRL and LH/FSH ratio (r = 0.1, P = 0.01). However, no significant relationship was found between PRL, other hormones, and the indicators of glucose and lipid metabolism.
Scatter plot matrix for the association of PRL with a LH, FSH, LH/FSH, Testosterone, and AMH, as well as b indicators of glucose and lipid metabolism. Note: Baseline data were used in this analysis. The significant correlation is shown with a star (*). Abbreviations: PRL, prolactin; LH, luteinizing hormone; FSH, follicle stimulating hormone; AMH, anti-mullerian hormone
Adjusted and unadjusted risk ratios as well as 95% confidence intervals for type 2 DM outcome, are presented in Table 2. In the unadjusted model, PRL was not associated with the incidence rate of type 2 DM (RR = 0.98, 95% CI: 0.94 − 1.03, P = 0.6), while there was a significant risk reduction in type 2 DM outcome for each unit increase in LH/FSH ratio (RR = 0.55, 95% CI: 0.35 − 0.89, P = 0.01), testosterone (RR = 0.87, 95% CI: 0.78 − 0.98, P = 0.02), and AMH (RR = 0.94, 95% CI: 0.91 − 0.98, P = 0.01). After adjusting for age, BMI, smoking status, and family history of DM, the only significant association that remained was the inverse effect of AMH on the incidence rate of type 2 DM (RR = 0.95, 95% CI: 0.91 − 0.99, P = 0.02).
Finally, an interaction term between PRL and other hormonal variables was checked in the log-binomial model, which had no significant results (not shown). The hazard ratio obtained by the Cox regression analysis for exploring the effect of PRL on the age at the onset of diabetes was close to the RRs obtained from log-binomial models (not shown).
Discussion
The present large-scale community-based cohort study with a long follow-up found no significant association between the incidence rate of type 2 DM and serum PRL concentrations within the physiologic range among middle-aged men. Our study also indicated an inverse association between AMH, testosterone, and LH/FSH ratio with the incidence rate of type 2 DM, which except for the former, were no longer significant after adjustment for the major confounding factors, including age, BMI, smoking status, and family history of DM. In addition, the group of men with PRL within the highest tertile of the physiologic range tended to show higher concentrations of LH and LH/FSH ratio, besides the finding that PRL was weakly correlated with LH/FSH ratio.
Previous cross-sectional studies conducted in Germany and China reported that higher quartiles of PRL concentration within the physiologic range were associated with a lower prevalence of type 2 DM among both sexes [19, 20]. Another cross-sectional study on Indian individuals reported that this association was only observed in women and not in men [23]. Previous longitudinal studies that included more than 4000 American and Chinese individuals also reported that serum PRL concentrations within the physiologic range were not associated with the risk of type 2 DM among men [18, 38], which is consistent with the results of the present study. It is important to note that the population-based prospective studies investigating this association among men are scarce [22], which necessitates more studies to reach a more reliable conclusion.
PRL is associated with glucose metabolism [3, 39], which might be explained through several routes. First, PRL improves insulin sensitivity by enhancing pancreatic β cell proliferation, preventing their apoptosis, and increasing insulin secretion [5,6,7, 40]. Second, PRL is involved in the reproduction and fertility [30]. LH and FSH [27], testosterone [26], and AMH [28, 29] are associated with obesity, metabolic syndrome, and type 2 DM in both sexes. Moreover, the signaling of insulin receptors in the brain is suggested to be crucial to the functional integrity of the hypothalamic-pituitary–gonadal axis, implying that a link might exist between the state of insulin resistance and this axis [41]. One study by Juneja et al. conducted on male rats found that LH suppression leads to PRL rise in a chain of events, causing a surge in testosterone [42]. After a few hours, testosterone concentrations decrease, resulting in PRL suppression, followed by a surge in LH. Testosterone suppression indirectly induces the release of PRL from the pituitary. It might be inappropriate to extrapolate the findings of an animal study to humans. However, PRL and testosterone's feedback mechanism might be an evolutionarily conserved phenomenon that ensures the circadian release of PRL, which is crucial to maintaining male fertility and libido [42, 43]. Finally, PRL is involved in the regulation of lipid metabolism. Adipose tissue not only expresses PRL receptors but also secretes PRL [15, 44]. PRL reduces lipogenesis [45] and regulates the release of adiponectin and interleukin-6 (IL-6) into the adipose tissue [46, 47]. It is important to note that, although the associations between PRL, reproductive hormones, and lipid metabolism have been investigated by a few studies, it is still not clear whether the possible association between PRL and the risk of developing type 2 DM could be influenced by the regulatory effect of PRL on the other reproductive hormones, its role in the lipid metabolism, or both.
Longitudinal studies on women have found that PRL within the physiologic range is associated with the incidence rate of type 2 DM. Based on our knowledge, this was not demonstrated among men. Our prospective analyses have not indicated the abovementioned association among men, which contrasts the findings of the previous studies among women [17, 18, 38]. This issue might be due to the sex-dependent nature of the multiple mechanisms involving PRL, reproductive hormones, and adipose tissue metabolism. For instance, a sex-dependent association exists between androgens and the incidence rate of type 2 DM [48, 49]. In contrast to women, testosterone is negatively correlated with the incidence rate of type 2 DM in men. Moreover, based on the mentioned study on male rats, lower testosterone concentrations accompany higher concentrations of PRL [42]. Therefore, it can be hypothesized that lower testosterone might dilute the protective effect of higher PRL concentrations within the physiologic range on glucose metabolism among men. This might explain the lack of a prospective association between PRL concentrations within the physiologic range and the incidence rate of type 2 DM among men. On the other hand, besides the fact that PRL is involved in adipose tissue metabolism [15, 44], adipose tissue distribution is different between the sexes. For instance, visceral adipose tissue (VAT) makes up to 20% of total adipose tissue in men, compared to just 6% in women [50]. In VAT, PRL has a dose-dependent inhibitory effect on the release of IL-6. As PRL concentrations increase within the physiologic range, IL-6 release into the tissue decrease [15], leading to an inflammatory state that might aggravate insulin resistance [51]. This phenomenon is more prominent in men due to the difference in VAT volume between men and women. Another proportion of adipose tissue, called subcutaneous adipose tissues (SAT), constitutes a greater proportion of total adipose tissue in women [50]. In SAT, PRL inhibits lipolysis by down-regulating lipoprotein lipase [52], resulting in a possible favorable metabolic effect by promoting insulin sensitivity and decreasing insulin resistance [53]. In addition, adiponectin is produced in SAT, and its baseline concentration is significantly higher in women [50]. When PRL concentrations are low within the physiologic range, adiponectin production is down-regulated [54], which causes an inflammatory state that might increase insulin resistance and decrease insulin sensitivity [51]. Since women have more SAT volume than men, the metabolically favorable regulatory effect of upper-limit concentrations of PRL on lipoprotein lipase and adiponectin might be more prominent in them [51, 53, 54]. Although we are unable to verify these hypotheses due to our lack of data on women and discussed adiposity-related factors, future studies might benefit from these novel perspectives.
In the investigations regarding the role of reproductive hormones, the present study found that the incidence rate of type 2 DM in men was inversely associated with AMH concentration in both unadjusted and adjusted models. Previous research has also suggested that lower AMH concentrations in men are associated with conditions that increase the risk of type 2 DM, including metabolic syndrome and insulin resistance [28, 29]. Moreover, based on several meta-analyses, testosterone concentrations are inversely associated with the risk of developing type 2 DM in men [48, 55, 56], the findings of which were confirmed solely in the unadjusted model of the current study. This might be due to the methodologic variations of the studies included in the meta-analyses. Including studies that measured free testosterone [55], investigating only hypogonadal men [56], using a limited number and relatively modest size of studies included [56], and lack of adjustment for confounders such as the family history of DM and smoking status [48, 55, 56] are the major aspects that might partly explain the contradiction between their results and ours. However, in a recent cohort study conducted on a sample of 673 middle-aged Chinese men, Li et al. [57] reported that in an adjusted model that also included smoking status, the odds of incident type 2 DM were not increased in different quartiles of total testosterone. The authors also reported the same results for LH and FSH, which agrees with our findings. However, an inverse association between the incidence rate of type 2 DM and concentrations of LH and FSH in males has been suggested by other studies [58, 59]. In addition, testosterone which is negatively associated with the risk of developing type 2 DM, is positively associated with LH and FSH concentrations in men [60], further contributing to the idea. Another study was conducted on knockout mice lacking neural insulin receptors to mimic the state of insulin resistance and found a significant reduction in LH concentrations in both sexes [41]. The authors concluded that the means to maintain the normal function of the hypothalamic-pituitary–gonadal axis is through regulating LH concentration. This indicates that type 2 DM might be associated with a lower LH/FSH ratio, explaining the significant inverse association between the incidence rate of type 2 DM and the LH/FSH ratio found in the unadjusted model of the present study. In addition, the LH/FSH ratio was positively correlated with PRL concentrations within the physiologic range in our study. This correlation might be justified by the observation made in the experimental study by Juneja et al., in which the stimulation of PRL pituitary release is preceded by a surge in LH among male rats [42]. Of note, the association between LH and higher PRL concentration which suggests a decrease in dopaminergic tone was also reported in our recent study [61].
This study has benefited from a prospective community-based design with a large sample of middle-aged men followed for more than 15 years. Another strength of this study arises from investigating the association between PRL and other reproductive hormones possibly involved in the mechanisms of glucose metabolism among men, including LH, FSH, testosterone, and AMH, which was lacking in the literature. There are also some limitations in this study worth mentioning. First, for women of the Tehran Lipid and Glucose Study, we lacked the required data to explore the associations between PRL, type 2 DM, and hormonal variables. Such data would enable us to compare these associations between the sexes with evidential accuracy. Second, a single measurement of PRL concentration was performed for each participant, which may not be the most reliable option, considering it is affected by factors like physical activity and stress. However, based on the guidelines for population-based studies, a single measurement is usually enough if the aim is overall assessment [62]. In addition, all proceedings were taken into account to make that single measurement as accurate as possible, which is mentioned in the methods section. Third, macroprolactin screening was not performed in asymptomatic men with serum PRL concentrations above the physiologic range. However, it should be noted that most current guidelines recommend a case-finding approach rather than a systematic screening for macroprolactinemia [63]. Fourth, testosterone was measured in the form of total testosterone (TT), consisting of bound plus free testosterone (FT). FT, as the bioavailable form of testosterone, yields more accurate results compared to TT. However, due to its standard equilibrium dialysis method’s complexity and its unharmonized assays, measuring FT is challenging in clinical laboratories [57]. In addition, faulty models of the bond between testosterone and sex-hormone binding globulin were used to derive FT calculating algorithms [64]. Finally, the markers of adiposity were not measured in this study, which could further shed light on the sex-specific association between PRL and t the incidence rate of type 2 DM. To better understand the mechanism underlying the effect of PRL on metabolism in various situations, further comprehensive studies, including assessment of different influential factors and adiposity factors with long enough follow-up, are recommended.
Conclusions
In a large-scale community-based cohort study, no significant association was found between serum prolactin concentrations within the physiologic range and the incidence rate of type 2 diabetes mellitus among middle-aged men. There was a tendency for men with higher concentrations of PRL within the physiologic range to show higher levels of LH and LH/FSH. These factors, along with FSH and testosterone, do not appear to be linked to type 2 DM in men. Higher AMH, however, was linked to a lower risk of developing type 2 DM in them.
Availability of Data and Materials
The datasets generated during and analyzed during the current study are not publicly available due to it being part of a large-scale cohort study called the Tehran Lipid and Glucose Study (TLGS), but are available from the corresponding author on reasonable request.
Abbreviations
- PRL:
-
Prolactin
- DM:
-
Diabetes Mellitus
- LH:
-
Luteinizing hormone
- FSH:
-
Follicle-stimulating hormone
- AMH:
-
Anti-mullerian hormone
- NCDs:
-
Non-communicable diseases
- WC:
-
Waist circumference
- HC:
-
Hip circumference
- WrC:
-
Wrist circumference
- BMI:
-
Body mass index
- WHR:
-
Waist-to-hip ratio
- FPG:
-
Fasting plasma glucose
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- IL-6:
-
Interleukin-6
- VAT:
-
Visceral adipose tissue
- SAT:
-
Subcutaneous adipose tissue
- FT:
-
Free testosterone
References
Riddle O, Bates RW, Dykshorn SW. THE PREPARATION, IDENTIFICATION AND ASSAY OF PROLACTIN—A HORMONE OF THE ANTERIOR PITUITARY. Am J Physiol-Leg Cont. 1933;105(1):191–216.
Ben-Jonathan N, Hugo ER, Brandebourg TD, LaPensee CR. Focus on prolactin as a metabolic hormone. Trends Endocrinol Metab. 2006;17(3):110–6.
Freeman ME, Kanyicska B, Lerant A, Nagy G. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523–631.
Bernard V, Young J, Chanson P, Binart N. New insights in prolactin: pathological implications. Nat Rev Endocrinol. 2015;11(5):265–75.
Fleenor DE, Freemark M. Prolactin induction of insulin gene transcription: roles of glucose and signal transducer and activator of transcription 5. Endocrinology. 2001;142(7):2805–10.
Freemark M, Avril I, Fleenor D, Driscoll P, Petro A, Opara E, et al. Targeted deletion of the PRL receptor: effects on islet development, insulin production, and glucose tolerance. Endocrinology. 2002;143(4):1378–85.
Labriola L, Montor WR, Krogh K, Lojudice FH, Genzini T, Goldberg AC, et al. Beneficial effects of prolactin and laminin on human pancreatic islet-cell cultures. Mol Cell Endocrinol. 2007;263(1–2):120–33.
Tuzcu A, Yalaki S, Arikan S, Gokalp D, Bahcec M, Tuzcu S. Evaluation of insulin sensitivity in hyperprolactinemic subjects by euglycemic hyperinsulinemic clamp technique. Pituitary. 2009;12(4):330–4.
dos Santos Silva CM, Barbosa FR, Lima GA, Warszawski L, Fontes R, Domingues RC, et al. BMI and metabolic profile in patients with prolactinoma before and after treatment with dopamine agonists. Obesity (Silver Spring). 2011;19(4):800–5.
Doknic M, Pekic S, Zarkovic M, Medic-Stojanoska M, Dieguez C, Casanueva F, et al. Dopaminergic tone and obesity: an insight from prolactinomas treated with bromocriptine. Eur J Endocrinol. 2002;147(1):77–84.
Serri O, Li L, Mamputu JC, Beauchamp MC, Maingrette F, Renier G. The influences of hyperprolactinemia and obesity on cardiovascular risk markers: effects of cabergoline therapy. Clin Endocrinol (Oxf). 2006;64(4):366–70.
Zhang XZ, Imachi H, Lyu JY, Fukunaga K, Sato S, Ibata T, et al. Prolactin regulatory element-binding protein is involved in suppression of the adiponectin gene in vivo. J Endocrinol Invest. 2017;40(4):437–45.
Nilsson L, Binart N, Bohlooly YM, Bramnert M, Egecioglu E, Kindblom J, et al. Prolactin and growth hormone regulate adiponectin secretion and receptor expression in adipose tissue. Biochem Biophys Res Commun. 2005;331(4):1120–6.
Pala NA, Laway BA, Misgar RA, Shah ZA, Gojwari TA, Dar TA. Profile of leptin, adiponectin, and body fat in patients with hyperprolactinemia: Response to treatment with cabergoline. Indian J Endocrinol Metab. 2016;20(2):177–81.
Hugo ER, Brandebourg TD, Comstock CE, Gersin KS, Sussman JJ, Ben-Jonathan N. LS14: a novel human adipocyte cell line that produces prolactin. Endocrinology. 2006;147(1):306–13.
Byatt JC, Staten NR, Salsgiver WJ, Kostelc JG, Collier RJ. Stimulation of food intake and weight gain in mature female rats by bovine prolactin and bovine growth hormone. Am J Physiol. 1993;264(6 Pt 1):E986–92.
Li J, Rice MS, Huang T, Hankinson SE, Clevenger CV, Hu FB, et al. Circulating prolactin concentrations and risk of type 2 diabetes in US women. Diabetologia. 2018;61(12):2549–60.
Wang T, Xu Y, Xu M, Ning G, Lu J, Dai M, et al. Circulating Prolactin and Risk of Type 2 Diabetes: A Prospective Study. Am J Epidemiol. 2016;184(4):295–301.
Balbach L, Wallaschofski H, Völzke H, Nauck M, Dörr M, Haring R. Serum prolactin concentrations as risk factor of metabolic syndrome or type 2 diabetes? BMC Endocr Disord. 2013;13:12.
Wang T, Lu J, Xu Y, Li M, Sun J, Zhang J, et al. Circulating prolactin associates with diabetes and impaired glucose regulation: a population-based study. Diabetes Care. 2013;36(7):1974–80.
Macotela Y, Triebel J, Clapp C. Time for a New Perspective on Prolactin in Metabolism. Trends Endocrinol Metab. 2020;31(4):276–86.
Faria de Castro L, Alves Dos Santos Á, Augusto Casulari L, Ansaneli Naves L, Amorim Amato A. Association between variations of physiological prolactin serum levels and the risk of type 2 diabetes: A systematic review and meta-analysis. Diabetes Res Clin Pract. 2020;166:108247.
Chahar C, Chahar K, Ankit BS, Gadhwal A, Agrawal RP. Association of Serum Prolactin Level with Impaired Glucose Regulation and Diabetes. J Assoc Physicians India. 2017;65(3):34–9.
Ben-Jonathan N, LaPensee CR, LaPensee EW. What can we learn from rodents about prolactin in humans? Endocr Rev. 2008;29(1):1–41.
Reis FM, Reis AM, Coimbra CC. Effects of hyperprolactinaemia on glucose tolerance and insulin release in male and female rats. J Endocrinol. 1997;153(3):423–8.
Gyawali P, Martin SA, Heilbronn LK, Vincent AD, Taylor AW, Adams RJT, et al. The role of sex hormone-binding globulin (SHBG), testosterone, and other sex steroids, on the development of type 2 diabetes in a cohort of community-dwelling middle-aged to elderly men. Acta Diabetol. 2018;55(8):861–72.
Stefanska A, Cembrowska P, Kubacka J, Kuligowska-Prusinska M, Sypniewska G. Gonadotropins and Their Association with the Risk of Prediabetes and Type 2 Diabetes in Middle-Aged Postmenopausal Women. Dis Markers. 2019;2019:2384069.
Robeva R, Tomova A, Kirilov G, Kumanov P. Anti-Mullerian hormone and inhibin B levels reflect altered Sertoli cell function in men with metabolic syndrome. Andrologia. 2012;44(Suppl 1):329–34.
Buyukinan M, Atar M, Pirgon O, Kurku H, Erdem SS, Deniz I. Anti-Mullerian Hormone and Inhibin B Levels in Obese Boys; Relations with Cardiovascular Risk Factors. Exp Clin Endocrinol Diabetes. 2018;126(8):528–33.
Auriemma RS, Del Vecchio G, Scairati R, Pirchio R, Liccardi A, Verde N, et al. The Interplay Between Prolactin and Reproductive System: Focus on Uterine Pathophysiology. Front Endocrinol (Lausanne). 2020;11:594370.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Diagnostic and laboratory tests. In: KD Pagana, PTJ, Pagana TN. Mosby's diagnostic and laboratory test reference. 15th ed. Missouri: Mosby; 2020. p. 734–5.
Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(2):273–88.
Association AD. Standards of Medical Care in Diabetes—2013. Diabetes Care. 2013;36(Supplement 1):S11–66.
Bozorgmanesh M, Hadaegh F, Saadat N, Azizi F. Fasting glucose cutoff point: where does the risk terminate? Tehran lipid and glucose study. Acta Diabetol. 2012;49(5):341–8.
McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–3.
Therkelsen KE, Abraham TM, Pedley A, Massaro JM, Sutherland P, Hoffmann U, Fox CS. Association between prolactin and incidence of cardiovascular risk factors in the Framingham heart study. J Am Heart Assoc. 2016;5(2):e002640.
Nagano M, Kelly PA. Tissue distribution and regulation of rat prolactin receptor gene expression. Quantitative analysis by polymerase chain reaction. J Biol Chem. 1994;269(18):13337–45.
Terra LF, Garay-Malpartida MH, Wailemann RA, Sogayar MC, Labriola L. Recombinant human prolactin promotes human beta cell survival via inhibition of extrinsic and intrinsic apoptosis pathways. Diabetologia. 2011;54(6):1388–97.
Bruning JC, Gautam D, Burks DJ, Gillette J, Schubert M, Orban PC, et al. Role of brain insulin receptor in control of body weight and reproduction. Science. 2000;289(5487):2122–5.
Juneja HS, Karanth S, Dutt A, Parte P, Meherjee P. Diurnal variations and temporal coupling of bioactive and immunoactive luteinizing hormone, prolactin, testosterone and 17-beta-estradiol in adult men. Horm Res. 1991;35(3–4):89–94.
Gill-Sharma MK. Prolactin and male fertility: the long and short feedback regulation. Int J Endocrinol. 2009;2009:687259.
Ben-Jonathan N, Hugo E. Prolactin (PRL) in adipose tissue: regulation and functions. Adv Exp Med Biol. 2015;846:1–35.
Barber MC, Clegg RA, Finley E, Vernon RG, Flint DJ. The role of growth hormone, prolactin and insulin-like growth factors in the regulation of rat mammary gland and adipose tissue metabolism during lactation. J Endocrinol. 1992;135(2):195–202.
Kobayashi K. Adipokines: therapeutic targets for metabolic syndrome. Curr Drug Targets. 2005;6(4):525–9.
Guerre-Millo M. Adipose tissue and adipokines: for better or worse. Diabetes Metab. 2004;30(1):13–9.
Ding EL, Song Y, Malik VS, Liu S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2006;295(11):1288–99.
Yao QM, Wang B, An XF, Zhang JA, Ding L. Testosterone level and risk of type 2 diabetes in men: a systematic review and meta-analysis. Endocr Connect. 2018;7(1):220–31.
Lafontan M, Berlan M. Do regional differences in adipocyte biology provide new pathophysiological insights? Trends Pharmacol Sci. 2003;24(6):276–83.
Vettor R, Milan G, Rossato M, Federspil G. Review article: adipocytokines and insulin resistance. Aliment Pharmacol Ther. 2005;22(Suppl 2):3–10.
LaPensee CR, Horseman ND, Tso P, Brandebourg TD, Hugo ER, Ben-Jonathan N. The prolactin-deficient mouse has an unaltered metabolic phenotype. Endocrinology. 2006;147(10):4638–45.
Morigny P, Houssier M, Mouisel E, Langin D. Adipocyte lipolysis and insulin resistance. Biochimie. 2016;125:259–66.
Brandebourg T, Hugo E, Ben-Jonathan N. Adipocyte prolactin: regulation of release and putative functions. Diabetes Obes Metab. 2007;9(4):464–76.
Corona G, Monami M, Rastrelli G, Aversa A, Sforza A, Lenzi A, et al. Type 2 diabetes mellitus and testosterone: a meta-analysis study. Int J Androl. 2011;34(6 Pt 1):528–40.
Grossmann M, Hoermann R, Wittert G, Yeap BB. Effects of testosterone treatment on glucose metabolism and symptoms in men with type 2 diabetes and the metabolic syndrome: a systematic review and meta-analysis of randomized controlled clinical trials. Clin Endocrinol (Oxf). 2015;83(3):344–51.
Li N, Huang C, Lan B, Lin D, Wang C, You L, et al. Association of gonadal hormones and sex hormone binding globulin with risk of diabetes: A cohort study in middle-aged and elderly Chinese males. Int J Clin Pract. 2021;75(5):e14008.
Basu AK, Singhania P, Bandyopadhyay R, Biswas K, Santra S, Singh S, et al. Late onset hypogonadism in type 2 diabetic and nondiabetic male: a comparative study. J Indian Med Assoc. 2012;110(8):573–5.
Zheng R, Cao L, Cao W, Chu X, Hu Y, Zhang H, et al. Risk Factors for Hypogonadism in Male Patients with Type 2 Diabetes. J Diabetes Res. 2016;2016:5162167.
Dhindsa S, Prabhakar S, Sethi M, Bandyopadhyay A, Chaudhuri A, Dandona P. Frequent occurrence of hypogonadotropic hypogonadism in type 2 diabetes. J Clin Endocrinol Metab. 2004;89(11):5462–8.
Mahboobifard F, Rahmati M, Amiri M, Azizi F, Ramezani TF. To what extent does polycystic ovary syndrome influence the cut-off value of prolactin? Findings of a community-based study. Adv Med Sci. 2022;67(1):79–86.
Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006;65(2):265–73.
Samson SL, Hamrahian AH, Ezzat S, Neuroendocrine A, Pituitary Scientific C, American College of E. American Association of Clinical Endocrinologists, American College of Endocrinology Disease State Clinical Review: Clinical Relevance of Macroprolactin in the Absence or Presence of True Hyperprolactinemia. Endocr Pract. 2015;21(12):1427–35.
Keevil BG, Adaway J. Assessment of free testosterone concentration. J Steroid Biochem Mol Biol. 2019;190:207–11.
Acknowledgements
The authors wish to acknowledge the study participants, the staff at the Tehran Lipid and Glucose Study, and the personnel of the Research Institute for Endocrine Sciences. The authors also appreciate Shahid Beheshti University of Medical Sciences for supporting this study.
Funding
This study was funded by Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Author information
Authors and Affiliations
Contributions
N.A. contributes in study design, execution, manuscript drafting, and critical discussion; M.F. contributes in study design, execution, manuscript drafting, and critical discussion; R.M. contributes in study design, execution, and analysis; F.F contributes in data collection, data cleaning, execution, and manuscript drafting; R.E contributes in study design and manuscript drafting; A.F contributes in study design, execution, and critical discussion; R.T.F. contributes in study design, execution, analysis, manuscript drafting, and critical discussion.
All authors have approved the final article.
Corresponding author
Ethics declarations
Ethics approval and consent to participation
The protocol of the present study was designed according to the principles of the Helsinki declaration and was approved by the Ethics committee of the Research Institute for Endocrine Sciences (IR.SBMU.ENDOCRINE.REC.1400.082). Informed written consent was obtained from each participant after providing them with complete descriptions of the study.
Consent for publication
Not applicable.
Competing Interests
Not applicable.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Niknam, A., Mahboobifard, F., Rahmati, M. et al. The effects of different physiologic concentrations of prolactin in association with reproductive hormones on the incidence of type 2 diabetes mellitus in men: Tehran Lipid and Glucose Study. BMC Endocr Disord 22, 302 (2022). https://doi.org/10.1186/s12902-022-01225-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01225-x