Abstract
Background
There is conflicting evidence on the effect of vitamin D on glycemic control. Therefore, in the current meta-analyses, we aimed to assess the effect of vitamin D supplementation on the glycemic control of type 2 diabetes (T2D) patients.
Methods
We conducted a comprehensive search in electronic databases including; PubMed/Medline, Web of Science, Scopus, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), and NIH’s Clinical Trials Registry, from the inception of each database up to January first, 2021.
Results
A total of 46 randomized controlled trials (RCTs) consisting of 2164 intervention subjects and 2149 placebo controls were included in this meta-analysis. Pooled analyses for HbA1c showed a significant change between the intervention and placebo group, the weighted mean difference (WMD)(95% confidence interval(CI)) was -0.20%(-0.29, -0.11) with P < 0.001. Analyses for assessing changes in FPG found a significant reduction in the intervention group after vitamin D supplementation, the WMD (95%CI) was -5.02 mg/dl (-6.75,-3.28) with P < 0.001. The result of pooled analyses for HOMA-IR revealed a significant change between the intervention and control group, the WMD (95%CI) was -0.42(-0.76, -0.07) with P = 0.019. The subgroup analyses showed the most efficacy in a higher dose and short intervention period and in subjects with deficient vitamin D status.
Conclusion
Vitamin D supplementation might be beneficial for the reduction of FPG, HbA1c, and HOMA-IR in type 2 diabetes patients with deficient vitamin D status. This effect was especially prominent when vitamin D was given in large doses and for a short period of time albeit with substantial heterogeneity between studies and a probability of publication bias.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus is a serious public health concern and the global prevalence has continued to rise over the past three decades [1, 2]. Globally, type 2 diabetes is ranked as the ninth leading cause of mortality contributing to more than 1 million deaths yearly and with an estimated 462 million cases in 2017 [2]. Diabetes mellitus is a group of metabolic disorders characterized by long-term hyperglycemia resulting from defects in insulin action, insulin secretion, or both [3]. Being diagnosed with and managing diabetes often affects an individuals quality of life and is also the leading cause of significant morbidity and premature mortality, as well as a major risk factor for adverse complications such as blindness, stroke, heart attack, amputation, and kidney failure [4, 5]. Although therapies for type 2 diabetes have improved over the last few decades, new insights for the prevention and management of type 2 diabetes remain necessary due to the increased prevalence of the disease.
Over the past decade, vitamin D has gained substantial interest for potential extra skeletal outcomes in various disease conditions, including diabetes [6, 7]. Vitamin D has been hypothesized to exhibit anti-diabetic properties by regulating insulin secretion or insulin sensitivity, producing anti-inflammatory effects, and down-regulation of elevated parathyroid hormone levels, which impair insulin secretion [8,9,10,11]. However, while there has been research suggesting that vitamin D may play an important role in glucose homeostasis, the results are conflicting. Many cross-sectional studies have found that insufficient vitamin D status was associated with the development of type 2 diabetes, diabetic complications, obesity, and metabolic syndrome [12,13,14,15]. A meta-analysis of observational studies indicated that low serum vitamin D levels were relatively associated with the prevalence of type 2 diabetes or metabolic syndrome [16]. Furthermore, prospective cohort studies have revealed inverse associations between baseline serum 25-OH-vitamin D [25(OH)D] and future risk of type 2 diabetes, diabetic complications, hyperglycemia, and insulin resistance [17,18,19,20]. In contrast, a meta-analysis of four prospective cohort studies suggested that there was no association between vitamin D intake and type 2 diabetes [21]. Evidence-based on Genetic Mendelian randomization analysis in a large sample of European ancestry did not support a causal association between total 25(OH)D or 25(OH)D metabolites and risk of type 2 diabetes [22].
Previous intervention studies evaluating the effect of vitamin D supplementation on glycemic control have produced conflicting findings [23,24,25,26,27]. Many previous meta-analyses of intervention studies exploring the effect of vitamin D supplementation on glycemic control had methodological limitations and the findings revealed inconsistencies [28,29,30,31]. Discrepancies in the findings and methodological limitations of individual studies in the literature, in addition to inconsistencies in the results of previous meta-analyses warrant the need for a comprehensive meta-analysis evaluating these relationships. Contrary to previous meta-analyses, only studies with vitamin D supplementation were included to isolate the potential effect of vitamin D independently, while studies with co-supplementation were excluded. Furthermore, there is a need for an updated systematic review and meta-analysis due to the increased volume of new or eligible studies in the literature evaluating the relationship between vitamin D supplementation and glycemic control since the publication of the most recent previous review.
Therefore, the objective of the current systematic review and meta-analysis of randomized controlled trials (RCTs) was to examine the effect of vitamin D supplementation on glycemic control indicators including fasting plasma glucose (FPG), HbA1c, and homeostasis model assessment insulin resistance (HOMA-IR) in patients with type 2 diabetes.
Materials and method
The study was performed according to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement guideline [32]. Since the present study utilized data from previously published studies, no patient consent or ethical approval was required. The protocol of this study was registered to Prospero online database (ID: 327,944).
Data sources and searches
A comprehensive search of online electronic databases from the inception of each database until January 1st, 2021 was completed. The databases included PubMed/Medline, Web of Science, Scopus, Embase, and Cochrane Central Register of Controlled Trials (CENTRAL). NIH’s Clinical Trials Registry (www.clinicaltrials.gov) was searched for completed but unpublished studies. The title/abstract search strategy based on syntax and MeSH terms of the following keywords and terms was performed: [(vitamin D supplementation OR vitamin D OR vitamin D2 OR vitamin D3 OR cholecalciferol OR ergocalciferol OR alphacalcidol OR alfacalcidol OR paricalcitol OR doxercalciferol OR calcitriol OR 25-Hydroxyvitamin D OR vitamin D) AND (Diabete OR diabetes mellitus OR T2DM OR hyperglycemia OR hyperglycaemia OR glucose OR HbA1c OR glycated hemoglobin OR insulin resistance OR insulin sensitivity OR HOMA OR glucose homeostasis OR insulin secretion OR insulin OR beta cell function OR glycemic control OR glucose tolerance OR glucose metabolism OR fasting blood glucose OR FBS OR Diabetes Mellitus OR Glycated Hemoglobin A OR Insulin Resistance) AND (randomized controlled trial OR controlled clinical trial OR random OR clinical trial OR controlled trial OR RCT) NOT (review OR animal)].
In addition, we hand-searched the reference lists of the included articles and previous reviews for additional relevant studies to help prevent missing any eligible studies. There were no restrictions on the date or language of publications. All eligible studies were included and duplicated citations were removed prior to screening using the Mendeley software.
Study selection
The inclusion criteria were: (1) RCT design, (2) adult population (age ≥ 18y), (3) population diagnosed with type 2 diabetes, (4) reported at least one glycemic control outcome (FBG or insulin or HbA1c or insulin resistance), (5) insulin resistance estimated by HOMA-IR; ((glucose, [mmol/L] × insulin [mU/L])/22.5) [33], (6) data reported as mean ± SD along with 95%CI,(7) the intervention group provided Vitamin D supplementation, while the control group provided placebo.
The exclusion criteria were: (1) letters, comments, short communications, meta-analyses, reviews, abstracts, or animal studies, (2) incomplete reporting of necessary data, (3) interventions with co-supplementation, (4) follow-up less than two months, (5) populations with type 1 diabetes, high-risk population of diabetes, pre-diabetic, gestational diabetes, post-partum diabetes, and diabetic nephropathy.
Data extraction and risk of bias assessment
Two reviewers (M.A.F, M.M) independently screened studies based on the inclusion and exclusion criteria. First, the title and abstract of all retrieved studies were screened to identify potentially relevant articles. Studies judged to be relevant were selected for full-text review. During the full-text screening, each article was analyzed by both reviewers which determined whether the article qualified for inclusion. Any conflicting decisions between reviewers to include a given study were resolved initially by consensus, but in case of no resolution, a third author (L.A) was consulted for the final decision. Additionally, if the data was not available or unclear in the published article, the author was contacted by e-mail to request the necessary data.
We evaluated the methodological quality of each included trial using the validated 6-item Cochrane risk of the bias assessment tool, 2009 [34]. Using this tool, each study was assigned a “high”, “some concerns” or “low” score for each of the following items: random sequence generation; allocation concealment; blinding of participants and personal; blinding of outcome assessment; incomplete outcome data and other sources of bias.
Required data from each eligible study were extracted by two independent investigators. The mean and standard deviation (SD) and corresponding 95% CIs for the effect of vitamin D supplementation on glycemic control were extracted from each study. Study information (authors, year, country, sample size), participants’ characteristics (gender, age, body mass index (BMI), vitamin D status), vitamin D supplementation characteristics (treatment, type, dose, and therapy duration), and results (baseline and post-intervention serum vitamin D, FBG, HbA1c, and HOMA-IR) were extracted. Serum vitamin D status was defined as deficient (serum 25(OH)D concentrations < 50 nmol/l), insufficient (50–75 nmol/l), and sufficient (> 75 nmol /l) [35].
Data synthesis and analysis
The STATA (version 13.0; College Station, Texas) software was used for all statistical analyses. We extracted data for continuous outcomes including the mean and SD change in FPG, HbA1c, and HOMA-IR with consideration of the 95% CI. A random-effects model (DerSimonian and Laird method) was used to estimate the pooled results. The Chi-square test and I2 statistic (%) were used to assess heterogeneity. The I2 index calculated as the proportion of total variation attributable to between-study variation was used to determine statistical heterogeneity between the studies. An I2 value of greater than 75% was considered substantial heterogeneity [36]. Subgroup analyses by continent, study type, BMI, vitamin D status, vitamin D dose, study duration, and supplementation type were performed using Cochran’s Q test and the I2 statistic to assess the possible sources of heterogeneity. Moreover, we assessed the publication bias using funnel plots and Egger’s regression test. Also, sensitivity analysis was performed to distinguish the extent to which summary estimates probably might be related to a particular study or group of studies. Data analyses were performed using Stata Software, version 14. P-values were reported as statistically significant at the < 0.05 level.
Result
Search results
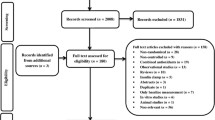
We identified 4452 articles in our initial search. After excluding duplicates and those that did not meet the inclusion criteria in the title and abstract screening, we identified 247 articles for full-text screening. After the full-text review, we excluded an additional 204 studies. A total of 43 papers were included in the current meta-analysis. Moreover, two additional studies were included after hand-searching the reference lists of the included papers [37, 38], and another study was included after receiving the full text of the paper by the author's email [39]. Among the 46 included studies, 35 reported an appropriate effect size for FPG, 42 for HbA1c, and 19 for HOMA-IR. A flow diagram of the study selection is presented in Fig. 1.
Study characteristics
Characteristics of the included studies are summarized in Table 1. 31 studies were conducted in Asia [24, 39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68], 9 in Europe [23, 27, 69,70,71,72,73,74], 3 in America [75,76,77], 1 in Africa [78], 1 in Australia [26] and 1 was conducted in 33 different countries [37]. A total of 4313 participants with type 2 diabetes were included in the current study, 2164 represented the intervention group and 2149 represented the control group. Across the included studies, the mean age of participants was 56.51 years and the mean BMI was 29.32. The baseline vitamin D status of 34 studies was classified as deficient, 6 studies as insufficient, 4 studies as sufficient and 2 studies did not report baseline vitamin D status. All studies included participants from both genders, except for one study with a population of only women [66]. The intervention ranged from 8 to 48 weeks in duration. Forty-two studies used oral vitamin D supplementation, while 4 studies used intramuscular (IM) vitamin D.
Quality assessment
The risk of bias assessment was conducted using the Cochrane risk of bias assessment tool [34] (Supplementary figure S1). Overall, 8 out of 46 included studies were considered as ‘high quality’ due to not being classified as high risk or unclear risk of bias on any of the assessment items. Among the remaining studies, 16 were considered as ‘moderate quality’ due to being classified as unclear risk of bias on ≤ 2 items, but not having any assessment items classified as high-risk. The remaining 22 studies were considered as ‘poor quality’ due to being classified as high-risk on any of the items or having > 2 items classified as an unclear risk of bias on the six domains. Allocation concealment, blinding of participants and personal and random sequence generation were the three most common sources of bias.
Meta-analysis
Vitamin D supplementation and FPG
Thirty-five studies representing a total of 3528 participants evaluated the effect of vitamin D supplementation on FPG. In the pooled analysis for FPG, a statistically significant difference between the intervention group and placebo group (WMD: -5.02 mg/dl (-0.28 mmol/L); 95%CI: -6.75 to -3.28 (-0.37 to -0.18 mmol/L), P < 0.00) was observed indicating an inverse effect of vitamin D on FBG (Fig. 2). However, there was evidence of significant heterogeneity between studies (I2 = 98.2%; P < 0.001).
Subgroup analyses revealed that continent, study type, vitamin D status, BMI, supplementation type, vitamin D dosage, and study duration explained the between-study heterogeneity. These analyses revealed a significant inverse effect of vitamin D supplementation on FPG in the majority of the study subgroups. The highest magnitude of differences were observed in subjects with deficient vitamin D status (WMD (95%CI): -7.37 mg/dl (-9.82, -4.92); P < 0.001) (Supplementary Table S1).
Based on the findings from the meta-regression, no effect of age on the effect sizes was found (regression coefficient = 0.04; 95%CI: -0.45, 0.55; P = 0.856).
Vitamin D supplementation and HbA1c
Forty-two studies representing a total of 4098 participants evaluated the effect of vitamin D supplementation on HbA1c. In the pooled analyses for HbA1c, a statistically significant difference between the intervention and control group (WMD (95%CI): -0.20% (-0.29, -0.11); P < 0.001) was observed indicating an inverse effect of vitamin D on HbA1c (Fig. 3). However, there was evidence of significant heterogeneity between studies (I2 = 98.2%; p < 0.001). In the subgroup analyses, we found that HbA1c was significantly lower in many of the subgroups including studies study populations from Asia, double-blind study designs, deficient serum vitamin D status, oral supplementation type, duration of ≤ 12 weeks, and a vitamin D dosage of > 2000 IU (Supplementary Table S2).
Based on the findings from the meta-regression, no effect of age on the effect sizes was found (regression coefficient = 0.005; 95%CI: -0.03, 0.05; P = 0.797).
Vitamin D supplementation and HOMA-IR
Nineteen studies representing a total of 1272 participants evaluated the effect of vitamin D supplementation on HOMA-IR level. In the pooled analyses for HOMA-IR, a statistically significant difference between the intervention and control group (WMD (95%CI): -0.42 (-0.76, -0.07); P = 0.019) was observed indicating an inverse effect of vitamin D on HOMA-IR (Fig. 4). Subgroup analyses revealed that HOMA-IR level decreased significantly in many subgroups including study populations from Asia, deficient serum vitamin D status, oral supplementation type, duration of ≤ 12 weeks, and vitamin D dose of > 2000 IU (Supplementary Table S3).
Based on the findings from the meta-regression, no effect of age on the effect sizes was found (regression coefficient = -0.006; 95%CI: -0.05, 0.03; P = 0.761).
Publication bias
The funnel plot for FPG appeared to be symmetric; but the Eggers test indicated that there was probability of publication bias (Supplementary Figure S2, Egger test = 0.024). The funnel plot for HbA1c appeared to be asymmetric (Supplementary Figure S3), but the Eggers test indicated that there was weak probability of publication bias (P = 0.402).
Similarly, there was no evidence of publication bias with HOMA-IR based on the results of the Eggers test (P = 0.842). However, the funnel plot for HOMA-IR appeared to be slightly asymmetric with a few studies falling beyond the funnel, which is consistent with the substantial heterogeneity observed among studies reporting HOMA-IR (Supplementary Figure S4).
Sensitivity analyses
In the sensitivity analyses, we did not find evidence that any particular study was the main source of heterogeneity.
Discussion
In the current systematic review and meta-analysis of RCTs, we found that vitamin D supplementation interventions resulted in a reduction in FPG, HbA1c, and HOMA-IR for individuals with type 2 diabetes. However, there was evidence of substantial heterogeneity. The heterogeneity appeared to be partially explained by diversity between study populations for serum vitamin D status, supplementation characteristics (dose and duration), BMIs, and ethnicity.
The FPG is a commonly used measure for the detection of short-term blood glucose [79]. HbA1c is a common measure of long-term blood glucose detection [79, 80]. In the current meta-analyses, we observed a statistically significant reduction of 5.02 mg/dl in FPG and a 0.20% reduction in HbA1c levels. However, it is important to consider that a reduction of < 0.50% in HbA1c is not considered clinically significant [81]. Findings suggest that high doses of vitamin D supplementation produced greater positive effects in vitamin D deficient, obese and Asian populations.
The baseline vitamin D status of participants was an important factor contributing to observed glycemic control outcomes. We found significant reductions in FBG and HbA1c in patients with vitamin D deficiency, but not in patients with vitamin D insufficiency or sufficiency. Similarly, even though we found that 25(OH)D increased significantly in all subgroups receiving the intervention, the greatest improvement was observed in vitamin D deficient patients. This may be due to the excess vitamin D from supplementation being stored in adipose tissue in individuals with sufficient vitamin D status rather than producing a further increase in serum level. Another reasonable explanation may be the impact of large doses of vitamin D supplementation. We found that high doses increased the likelihood of correcting vitamin D deficiency or achieving favorable levels of serum 25(OH)D, confirmed by relatively higher 25(OH)D levels in the high dose subgroup (> 2000 IU) after receiving the intervention compared to the lower dose (≤ 2000 IU). In line with our findings, a meta-analysis by Chunhua Wu et al. found that vitamin D supplementation was associated with reduced FPG and HbA1c among patients with 25-hydroxyvitamin D (25(OH) D) deficiency at baseline [29].
The dosage and duration of vitamin D supplementation are other important contributors to glycemic control outcomes for patients with type 2 diabetes. High doses of vitamin D were found to improve glycemic control outcomes and was observed to be more efficient for correcting serum 25-hydroxyvitamin D level for subjects with vitamin D deficiency. The effect of the duration of vitamin D supplementation appeared to be more ambiguous amongst glycemic control outcomes. For example, we found a statistically significant reduction in FPG with both short-term (≤ 12 weeks) and long-term (> 12 weeks) vitamin D supplementation, however, the magnitude of reduction was greater with long-term (WMD: -6.74) than short-term (WMD: -2.37) supplementation. Comparatively, there was only evidence of a reduction in HbA1c and HOMA-IR outcomes with short-term (≤ 12 weeks) vitamin D supplementation.
Among different continents of study origin, vitamin D supplementation produced varying effects. The greatest reductions were observed among studies conducted in Asia and Europe, while studies conducted on other continents revealed no evidence of a difference. However, studies conducted in Asia represented the majority of the included RCTs for the meta-analysis and it is possible that this analysis had a greater power to detect a statistically significant difference compared to other continents that may not have had a sufficient number of studies. Therefore, insufficient evidence to differentiate between the continents of study origin should be considered when interpreting the findings from the subgroup analysis. Wang et al. explained the heterogeneous responses between Asians and the other groups by demonstrating that vitamin D-binding protein polymorphism was associated with increased susceptibility to T2D in Asians, but not in Caucasians [82]. Furthermore, it is relatively understood that typically between 50 to 90% of vitamin D in the body is due to the production in the skin and the remainder is from the diet. Previous studies have found that populations with darker skin color and cultural preferences toward less exposure to the sun, which matched the profile of Asians and especially Middle Easterners, were at a higher risk of vitamin D deficiency, which in turn, was associated with greater positive effects from supplementation [83, 84]. However, there were a limited number of studies included in the analysis that represented data from America, Africa, and Australia. Therefore, future investigations on the effect of vitamin D supplementation in these continents and populations are warranted.
HOMA-IR as proposed by Matthews et al. [33], is the most frequently employed technique as the index of insulin resistance (IR) and has proved to be a robust tool for the assessment of IR [85, 86]. The concept of IR is generally defined as the reduced biological action of insulin, such as inhibition of hepatic glucose production and insulin-mediated glucose disposal [87]. In the current meta-analysis, a significant reduction in HOMA-IR was found in the vitamin D intervention compared to the control group with the lowest between-study heterogeneity found for studies with a short-duration intervention (≤ 12 weeks) in the subgroup analysis. Similar to our findings, Hu Z et al. revealed that decreases in HOMA-IR and changes in insulin resulting from a vitamin D supplementation intervention were only observed in short-term follow-up studies and not in long-term studies [30]. It was hypothesized that this may be due to higher doses of vitamin D being provided in short-term interventions in comparison to doses provided in longer-term studies. Our findings are comparable to results from another meta-analysis by Xinyi Li et al. revealing an improvement in HOMA-IR for subjects in the vitamin D intervention group and subjects with baseline vitamin D deficiency [28].
We conducted a comprehensive systematic review and meta-analysis on a large number of RCTs that investigated the effect of vitamin D supplementation on glycemic control outcomes including FPG, HbA1c, and HOMA-IR. Part of the objective for this meta-analysis was to overcome methodological concerns present in previous meta-analyses, to provide updated findings, and transition from previous inconsistencies toward more conclusive results. However, potential limitations should be considered when interpreting our findings. Although we conducted a comprehensive search, appropriate publications being missed remains a possibility. The relatively short intervention durations, small sample sizes, and variations in intervention doses and durations of some studies, in addition to the moderate to substantial heterogeneity observed in some of our results, may limit our ability to determine the effects of vitamin D supplementation and draw meaningful conclusions. Finally, some of the included RCTs did not consider the effect of sun exposure, diet, and physical activity on the findings which may have directly influenced vitamin D status, or did not consider the consumption of antidiabetic medications that may have masked the benefits of vitamin D supplementation. Another factor that may pose a challenge to interpreting the study results related to many studies which did not provide enough details to allow accurate qualitative assessment of how each study handled randomization, allocation, blinding, and missing data.
Conclusion
The present meta-analysis found that vitamin D supplementation may be beneficial for the reduction of FPG, HbA1c, and HOMA-IR in patients with type 2 diabetes and deficient vitamin D status. This effect was especially prominent when vitamin D was given in large doses and for a short period of time albeit with substantial heterogeneity between studies and a probability of publication bias. In conclusion, this study is in agreement with previous findings on the potential of vitamin D supplementation along with other antidiabetic drugs to improve glycemic control and prevent diabetic complications.
Availability of data and materials
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- T2D:
-
Type 2 diabetes
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Hemoglobin A1c
- HOMA-IR:
-
Homeostasis model assessment – insulin resistance
- RCT:
-
Randomized controlled trials
- CI:
-
Confidence interval
- WMD:
-
Weighted mean difference
References
Waly MI, Essa MM, Ali Ajijbmr. The global burden of type 2 diabetes: a review. 2010;1(4):326–9.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, AlKaabi J, et al. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107.
American Diabetes Association; Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2004;27(suppl_1): s5–s10.
Lotfy M, Adeghate J, Kalasz H, Singh J, Adeghate E. Chronic complications of diabetes mellitus: a mini review. Curr Diabetes Rev. 2017;13(1):3–10.
Ramtahal R, Khan C, Maharaj-Khan K, Nallamothu S, Hinds A, Dhanoo A, et al. Prevalence of self-reported sleep duration and sleep habits in type 2 diabetes patients in South Trinidad. J Epidemiol Glob Health. 2015;5(4):S35–43.
Bikle D. Nonclassic actions of vitamin D. J Clin Endocrinol Metab. 2009;94(1):26–34.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–81.
Borissova AM, Tankova T, Kirilov G, Dakovska L, Kovacheva R. The effect of vitamin D3 on insulin secretion and peripheral insulin sensitivity in type 2 diabetic patients. Int J Clin Pract. 2003;57(4):258–61.
Pitocco D, Crinò A, Di Stasio E, Manfrini S, Guglielmi C, Spera S, et al. The effects of calcitriol and nicotinamide on residual pancreatic beta-cell function in patients with recent-onset Type 1 diabetes (IMDIAB XI). Diabet Med. 2006;23(8):920–3.
Mitri J, Pittas AG. Vitamin D and diabetes. Endocrinol Metab Clin North Am. 2014;43(1):205–32.
Fadda GZ, Akmal M, Lipson LG, Massry SG. Direct effect of parathyroid hormone on insulin secretion from pancreatic islets. Am J Physiol. 1990;258(6 Pt 1):E975–84.
Xiao Y, Wei L, Xiong X, Yang M, Sun L. Association between vitamin D status and diabetic complications in patients with type 2 diabetes mellitus: a cross-sectional study in Hunan China. Front Endocrinol. 2020;11: 564738.
Butler AE, Dargham SR, Latif A, Mokhtar HR, Robay A, Chidiac OM, et al. Association of vitamin D(3) and its metabolites in patients with and without type 2 diabetes and their relationship to diabetes complications. Ther Adv Chronic Dis. 2020;11:2040622320924159.
Dai J, Yu M, Chen H, Chai Y. Association between serum 25-OH-vitamin D and diabetic foot ulcer in patients with type 2 diabetes. Front Nutr. 2020;7:109.
Gulseth HL, Gjelstad IM, Birkeland KI, Drevon CA. Vitamin D and the metabolic syndrome. Curr Vasc Pharmacol. 2013;11(6):968–84.
Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92(6):2017–29.
Wang L, Liu X, Hou J, Wei D, Liu P, Fan K, et al. Serum Vitamin D Affected Type 2 Diabetes though Altering Lipid Profile and Modified the Effects of Testosterone on Diabetes Status. Nutrients. 2020;13(1):90.
Ahmed LHM, Butler AE, Dargham SR, Latif A, Robay A, Chidiac OM, et al. Association of vitamin D(2) and D(3) with type 2 diabetes complications. BMC Endocr Disord. 2020;20(1):65.
Mattila C, Knekt P, Männistö S, Rissanen H, Laaksonen MA, Montonen J, et al. Serum 25-hydroxyvitamin D concentration and subsequent risk of type 2 diabetes. Diabetes Care. 2007;30(10):2569–70.
Forouhi NG, Luan J, Cooper A, Boucher BJ, Wareham NJ. Baseline serum 25-hydroxy vitamin d is predictive of future glycemic status and insulin resistance: the medical research council Ely prospective study 1990–2000. Diabetes. 2008;57(10):2619–25.
Zhao LM, Tian XQ, Ge JP, Xu YC. Vitamin D intake and type 2 diabetes risk: a meta-analysis of prospective cohort studies. Afr Health Sci. 2013;13(4):1130–8.
Zheng JS, Luan J, Sofianopoulou E, Sharp SJ, Day FR, Imamura F, et al. The association between circulating 25-hydroxyvitamin D metabolites and type 2 diabetes in European populations: a meta-analysis and Mendelian randomisation analysis. PLoS medicine. 17(10):e1003394.
Gulseth HL, Wium C, Angel K, Eriksen EF, Birkeland KI. Effects of vitamin D supplementation on insulin sensitivity and insulin secretion in subjects with Type 2 diabetes and vitamin D deficiency: a randomized controlled trial. Diabetes Care. 2017;40(7):872–8.
Safarpour P, Daneshi-Maskooni M, Vafa M, Nourbakhsh M, Janani L, Maddah M, et al. Vitamin D supplementation improves SIRT1, Irisin, and glucose indices in overweight or obese type 2 diabetic patients: a double-blind randomized placebo-controlled clinical trial. BMC family practice. 2020;21(1):26.
Baziar N, Jafarian K, Shadman Z, Qorbani M, Nikoo MK, Abd Mishani MJIRCMJ. Effect of therapeutic dose of vitamin D on serum adiponectin and glycemia in vitamin D-insufficient or deficient type 2 diabetic patients. 2014;16(9).
Elkassaby S, Harrison LC, Mazzitelli N, Wentworth JM, Colman PG, Spelman T, et al. A randomised controlled trial of high dose vitamin D in recent-onset type 2 diabetes. Diabetes Res Clin Pract. 2014;106(3):576–82.
Krul-Poel YH, Westra S, ten Boekel E, ter Wee MM, van Schoor NM, van Wijland H, et al. Effect of vitamin D supplementation on glycemic control in patients with type 2 diabetes (SUNNY trial): a randomized placebo-controlled trial. Diabetes Care. 2015;38(8):1420–6.
Li X, Liu Y, Zheng Y, Wang P, Zhang Y. The effect of vitamin D supplementation on glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Nutrients. 2018;10(3):375.
Wu C, Qiu S, Zhu X, Li L. Vitamin D supplementation and glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Metabolism. 2017;73:67–76.
Hu Z, Chen J, Sun X, Wang L, Wang A. Efficacy of vitamin D supplementation on glycemic control in type 2 diabetes patients: a meta-analysis of interventional studies. Medicine. 2019;98(14): e14970.
Lee CJ, Iyer G, Liu Y, Kalyani RR, Bamba N, Ligon CB, et al. The effect of vitamin D supplementation on glucose metabolism in type 2 diabetes mellitus: a systematic review and meta-analysis of intervention studies. J Diabetes Complications. 2017;31(7):1115–26.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-34.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner RJD. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed). 2011;343: d5928.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327(7414):557–60.
Punthakee Z, Bosch J, Dagenais G, Diaz R, Holman R, Probstfield J, Ramachandran A, Riddle M, Rydén LE, Zinman B, Afzal R, Yusuf S, Gerstein H. TIDE Trial Investigators. Design, history and results of the Thiazolidinedione Intervention with vitamin D Evaluation (TIDE) randomised controlled trial. Diabetologia. 2012;55(1):36–45.
Maggi S, Siviero P, Brocco E, Albertin M, Romanato G. Crepaldi GJAd. Vitamin D deficiency, serum leptin and osteoprotegerin levels in older diabetic patients: an input to new research avenues. 2014;51(3):461–9.
Shahriari S, Eftekhari MH, Jeddi M. The effect of vitamin D supplementation in overweight or obese type 2 diabetic patients with vitamin D deficiency and dyslipidemia. Int J Nutr Sci. 2018;3(4):185–91.
Shaseb E, Tohidi M, Abbasinazari M, Khalili D, Talasaz AH, Omrani H, et al. The effect of a single dose of vitamin D on glycemic status and C-reactive protein levels in type 2 diabetic patients with ischemic heart disease: a randomized clinical trial. Acta Diabetol. 2016;53(4):575–82.
Farrokhian A, Raygan F, Bahmani F, Talari HR, Esfandiari R, Esmaillzadeh A, et al. Long-term vitamin D supplementation affects metabolic status in vitamin D-deficient type 2 diabetic patients with coronary artery disease. J Nutr. 2017;147(3):384–9.
Khan DM, Jamil A, Randhawa FA, Butt NF, Malik U. Efficacy of oral vitamin D on glycated haemoglobin (HbA1c) in type 2 diabetics having vitamin D deficiency - a randomized controlled trial. J Pak Med Assoc. 2018;68(5):694–7.
Ghavamzadeh S, Mobasseri M, Mahdavi R. The effect of vitamin D supplementation on adiposity, blood glycated hemoglobin, serum leptin and tumor necrosis factor-α in Type 2 diabetic patients. Int J Prev Med. 2014;5(9):1091–8.
Sadiya A, Ahmed SM, Carlsson M, Tesfa Y, George M, Ali SH, et al. Vitamin D supplementation in obese type 2 diabetes subjects in Ajman, UAE: a randomized controlled double-blinded clinical trial. Eur J Clin Nutr. 2015;69(6):707–11.
Dalan R, Liew H, Assam PN, Chan ES, Siddiqui FJ, Tan AW, et al. A randomised controlled trial evaluating the impact of targeted vitamin D supplementation on endothelial function in type 2 diabetes mellitus: The DIMENSION trial. Diab Vasc Dis Res. 2016;13(3):192–200.
Momeni A, Mirhosseini M, Kabiri M, Kheiri S. Effect of vitamin D on proteinuria in type 2 diabetic patients. J Nephropathol. 2017;6(1):10–4.
Omidian M, Djalali M, Javanbakht MH, Eshraghian MR, Abshirini M, Omidian P, et al. Effects of vitamin D supplementation on advanced glycation end products signaling pathway in T2DM patients: a randomized, placebo-controlled, double blind clinical trial. Diabetol Metab Syndr. 2019;11:86.
Rad EY, Attar MJH, Koohdani F, Saboor-Yaraghi AA, Eshraghian MR, Javanbakht MH, et al. Effect of vitamin D supplementation on thioredoxin binding protein 2 gene expression in patients with diabetes type 2. Curr Top Nutraceutical Res. 2015;13(1):55–9.
Eftekhari MH, Akbarzadeh M, Dabbaghmanesh MH, Hasanzadeh J. Impact of treatment with oral calcitriol on glucose indices in type 2 diabetes mellitus patients. Asia Pac J Clin Nutr. 2011;20(4):521–6.
Ryu O-H, Chung W, Lee S, Hong K-S, Choi M-G, Yoo HJ. The effect of high-dose vitamin D supplementation on insulin resistance and arterial stiffness in patients with type 2 diabetes. Korean J Intern Med. 2014;29(5):620–9.
Agarwal C, Marwah S, Kulshrestha B, Anubhuti. Effect of Vitamin D Replacement Therapy on Glycaemic Control in Type 2 Diabetic Mellitus Patients. J Clin Diagn Res. 2017;11(12):OC40-3.
Heshmat R, Tabatabaei-Malazy O, Abbaszadeh-Ahranjani S, Shahbazi S, Khooshehchin G, Bandarian F, et al. Effect of vitamin D on insulin resistance and anthropometric parameters in Type 2 diabetes; a randomized double-blind clinical trial. Daru. 2012;20(1):10.
Shaheen A, Khawer F, Ijaz S. A randomized control trial to determine the orally taken vitamin-D glycated hemoglobin among patients of T2DM. Indo Am J Pharm Scie. 2019;6(5):9308–14.
Upreti V, Maitri V, Dhull P, Handa A, Prakash MS, Behl A. Effect of oral vitamin D supplementation on glycemic control in patients with type 2 diabetes mellitus with coexisting hypovitaminosis D: a parellel group placebo controlled randomized controlled pilot study. Diabetes & metabolic syndrome. 2018;12(4):509–12.
Dadrass A, Mohamadzadeh Salamat K, Hamidi K, Azizbeigi K. Anti-inflammatory effects of vitamin D and resistance training in men with type 2 diabetes mellitus and vitamin D deficiency: a randomized, double-blinded, placebo-controlled clinical trial. J Diabetes Metab Disord. 2019;18(2):323–31.
Baziar N, Jafarian K, Shadman Z, Qorbani M, KhoshniatNikoo M, Abd Mishani M. Effect of therapeutic dose of vitamin d on serum adiponectin and glycemia in vitamin d-insufficient or deficient type 2 diabetic patients. Iran Red Crescent Med J. 2014;16(9):e21458.
Nasri H, Behradmanesh S, Maghsoudi AR, Ahmadi A, Nasri P, Rafieian-Kopaei M. Efficacy of supplementary vitamin D on improvement of glycemic parameters in patients with type 2 diabetes mellitus; a randomized double blind clinical trial. J Renal Inj Prev. 2014;3(1):31–4.
Breslavsky A, Frand J, Matas Z, Boaz M, Barnea Z, Shargorodsky M. Effect of high doses of vitamin D on arterial properties, adiponectin, leptin and glucose homeostasis in type 2 diabetic patients. Clinical nutrition (Edinburgh, Scotland). 2013;32(6):970–5.
El Hajj C, Walrand S, Helou M, Yammine K. Effect of vitamin D supplementation on inflammatory markers in non-obese lebanese patients with type 2 diabetes: a randomized controlled trial. Nutrients. 2020;12(7):2033.
Mirzavandi F, Babaie S, Rahimpour S, Razmpoosh E, Talenezhad N, Aghaei Zarch SM, et al. The effect of high dose of intramuscular vitamin D supplement injections on depression in patients with type 2 diabetes and vitamin D deficiency: a randomized controlled clinical trial. Obe Med. 17:100192.
Imanparast F, Javaheri J, Kamankesh F, Rafiei F, Salehi A, Mollaaliakbari Z, Rezaei F, Rahimi A, Abbasi E. The effects of chromium and vitamin D3 co-supplementation on insulin resistance and tumor necrosis factor-alpha in type 2 diabetes: a randomized placebo-controlled trial. Appl Physiol Nutr Metab. 2020;45(5):471–7.
Razzaghi R, Pourbagheri H, Momen-Heravi M, Bahmani F, Shadi J, Soleimani Z, et al. The effects of vitamin D supplementation on wound healing and metabolic status in patients with diabetic foot ulcer: a randomized, double-blind, placebo-controlled trial. J Diabetes Complications. 2017;31(4):766–72.
Parekh D, Sarathi V, Shivane VK, Bandgar TR, Menon PS, Shah NSJEP. Pilot study to evaluate the effect of short-term improvement in vitamin D status on glucose tolerance in patients with type 2 diabetes mellitus. Endocr Pract. 2010;16(4):600–8.
Al-Sofiani ME, Jammah A, Racz M, Khawaja RA, Hasanato R, El-Fawal HAN, et al. Effect of vitamin D supplementation on glucose control and inflammatory response in type II diabetes: a double blind, randomized clinical trial. Int J Endocrinol Metab. 2015;13(1):e22604.
Muley A, Iyer UJIJoPHR, Development. Impact of vitamin D supplementation on anthropometric, glycemic and lipemic profile in subjects with type 2 diabetes: a randomized control trial. 2019;10(9).
Kim JH, Lee JM, Chang SA. Effects of vitamin D supplement on arterial stiffness in patients with type 2 diabetes mellitus and vitamin D deficiency. Diabetologia. 2014;57(1):S526–7.
Alzahrani MK. The effect of vitamin D3 supplementation on glycemic control in type 2 diabetic patients having suboptimal vitamin d level, in an open-label, randomized controlled trial. Endocrine Reviews. 2012;33(3).
Bhosle DS, Mubeen MF. Evaluation of Effect of Vitamin D Supplementation on Glycemic Control in Patients of Type 2 Diabetes Mellitus. J Diabetes Metab. 2018;9(806):2.
Kampmann U, Mosekilde L, Juhl C, Moller N, Christensen B, Rejnmark L, et al. Effects of 12 weeks high dose vitamin D3 treatment on insulin sensitivity, beta cell function, and metabolic markers in patients with type 2 diabetes and vitamin D insufficiency - a double-blind, randomized, placebo-controlled trial. Metabolism. 2014;63(9):1115–24.
Witham MD, Dove FJ, Dryburgh M, Sugden JA, Morris AD, Struthers AD. The effect of different doses of vitamin D(3) on markers of vascular health in patients with type 2 diabetes: a randomised controlled trial. Diabetologia. 2010;53(10):2112–9.
Barengolts E, Kouser A, Kukreja SC, Eisenberg Y, Ciubotaru I, Manickam B. High dose vitamin D supplementation for 12 months improves insulin sensitivity and glucose disposition indices in African American men with hypovitaminosis D and Dysglycemia: Results of the D-Vitamin Intervention in Veteran Administration (DIVA) randomize. Endocr Rev. 2014;35(3, S).
Sugden JA, Davies JI, Witham MD, Morris AD, Struthers AD. Vitamin D improves endothelial function in patients with Type 2 diabetes mellitus and low vitamin D levels. Diabet Med. 2008;25(3):320-5.
Jehle S, Lardi A, Felix B, Hulter HN, Stettler C, Krapf R. Effect of large doses of parenteral vitamin D on glycaemic control and calcium/phosphate metabolism in patients with stable type 2 diabetes mellitus: A randomised, placebo-controlled, prospective pilot study. Swiss Med Wkly. 2014;144:w13942.
Jorde R, Figenschau Y. Supplementation with cholecalciferol does not improve glycaemic control in diabetic subjects with normal serum 25-hydroxyvitamin D levels. Eur J Nutr. 2009;48(6):349-54.
Angellotti E, D'Alessio D, Dawson-Hughes B, Chu Y, Nelson J, Hu P, Cohen RM, Pittas AG. Effect of vitamin D supplementation on cardiovascular risk in type 2 diabetes. Clin Nutr. 2019;38(5):2449–53.
Soric MM, Renner ET, Smith SR. Effect of daily vitamin D supplementation on HbA1c in patients with uncontrolled type 2 diabetes mellitus: a pilot study. J Diabetes. 2012;4(1):104–5.
Lo MC, Abushamat L, Mramba LK. Effect of treating vitamin D deficiency in uncontrolled type 2 diabetes: a randomized, placebo-controlled study. Am J Ther. 2019;26(4):e441–51.
Anyanwu AC, Fasanmade OA, Coker HAB, Ohwovoriole AE. Vitamin D supplementation improves insulin resistance in type 2 diabetes subjects in Lagos Nigeria. Afr J Diabetes Med. 2017;25(1):14–7.
Furusyo N, Koga T, Ai M, Otokozawa S, Kohzuma T, Ikezaki H, et al. Utility of glycated albumin for the diagnosis of diabetes mellitus in a Japanese population study: results from the Kyushu and Okinawa Population Study (KOPS). Diabetologia. 2011;54(12):3028–36.
Mittman N, Desiraju B, Fazil I, Kapupara H, Chattopadhyay J, Jani CM, et al. Serum fructosamine versus glycosylated hemoglobin as an index of glycemic control, hospitalization, and infection in diabetic hemodialysis patients. Kidney Int Suppl. 2010;117:S41–5.
Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, et al. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141(6):421–31.
Wang G, Li Y, Li L, Yu F, Cui L, Ba Y, et al. Association of the vitamin D binding protein polymorphisms with the risk of type 2 diabetes mellitus: a meta-analysis. BMJ Open. 2014;4(11): e005617.
Rajan S, Weishaar T, Keller B. Weight and skin colour as predictors of vitamin D status: results of an epidemiological investigation using nationally representative data. Public Health Nutr. 2017;20(10):1857–64.
Lips P. Worldwide status of vitamin D nutrition. J Steroid Biochem Mol Biol. 2010;121(1–2):297–300.
Mojiminiyi OA, Abdella NA. Effect of homeostasis model assessment computational method on the definition and associations of insulin resistance. Clin Chem Lab Med. 2010;48(11):1629–34.
Antuna-Puente B, Disse E, Rabasa-Lhoret R, Laville M, Capeau J, Bastard JP. How can we measure insulin sensitivity/resistance? Diabetes Metab. 2011;37(3):179–88.
Alebić M, Bulum T, Stojanović N, Duvnjak L. Definition of insulin resistance using the homeostasis model assessment (HOMA-IR) in IVF patients diagnosed with polycystic ovary syndrome (PCOS) according to the Rotterdam criteria. Endocrine. 2014;47(2):625–30.
Barchetta I, Del Ben M, Angelico F, Di Martino M, Fraioli A, La Torre G, Saulle R, Perri L, Morini S, Tiberti C, Bertoccini L, Cimini FA, Panimolle F, Catalano C, Baroni MG, Cavallo MG. No effects of oral vitamin D supplementation on non-alcoholic fatty liver disease in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled trial. BMC Med. 2016;14:92.
Yousefi Rad E, Djalali M, Koohdani F, Saboor-Yaraghi AA, Eshraghian MR, Javanbakht MH, Saboori S, Zarei M, Hosseinzadeh-Attar MJ. The Effects of Vitamin D Supplementation on Glucose Control and Insulin Resistance in Patients with Diabetes Type 2: A Randomized Clinical Trial Study. Iran J Public Health. 2014;43(12):1651-6.
Almoushawah AA, Almansour M, Alshahrani F, Rahman SU, Al-Zahrani A. A 3-month oral vitamin D supplementation marginally improves diastolic blood pressure in Saudi patients with type 2 diabetes mellitus. Int J Clin Exp Med. 2014;7(12):5421-8.
Acknowledgements
This work was supported by the Tehran University of Medical Science (TUMS), School of Nutrition and Dietetics (Grant No: 1400-1-130-51099).
Funding
This work was supported by the Tehran University of Medical Science (TUMS), School of Nutrition and Dietetics.
Author information
Authors and Affiliations
Contributions
MAF, ED, TTF, and LA: conceptualization and software; MAF and MM: resource and data curation; MAF and FZ: writing—original draft; ED: formal analysis; ED, LA and TTF: supervision and writing—review & editing. NB: revising, language checking and structural editing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work was supported by the Tehran University of Medical Science (TUMS), School of Nutrition and Dietetics (Grant No:1400–1-130–51099).
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest. The founding sponsor had no role in the design of the study; in the selection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Figure S1. Risk of bias assessment for included studies using the Cochrane Collaboration tool across six domains. Supplementary Table S1. Summary table of subgroup analyses; FPG changes. Supplementary Table S2. Summary table of subgroup analyses; HbA1c changes. Supplementary Table S3. Summary table of subgroup analyses; HOMA-IR changes. Supplementary Figure S2. Funnel plot for fasting plasma glucose. Supplementary Figure S3. Funnel plot for HbA1c. Supplementary Figure S4. Funnel plot for HOMA-IR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farahmand, M.A., Daneshzad, E., Fung, T.T. et al. What is the impact of vitamin D supplementation on glycemic control in people with type-2 diabetes: a systematic review and meta-analysis of randomized controlled trails. BMC Endocr Disord 23, 15 (2023). https://doi.org/10.1186/s12902-022-01209-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01209-x