Abstract
Background
Lipid and glucose metabolism abnormalities are associated with nonalcoholic fatty liver disease (NAFLD). The triglyceride–glucose (TyG) index is a recently developed indicator that can identify individuals at risk for NAFLD. However, the applicability of the TyG index for identifying NAFLD in patients with type 2 diabetes mellitus (T2DM) is unclear. The aim of this study was to investigate the ability of the TyG index to identify individuals at risk for NAFLD in the T2DM population.
Methods
A total of 2280 participants with T2DM were recruited in this cross-sectional study. The TyG index was calculated, and NAFLD was diagnosed by ultrasonography. Binary logistic regression models were used to evaluate the association of the TyG index, glycemic parameters and lipid parameters with NAFLD.
Results
Logistic regression analysis showed that the TyG index was significantly associated with NAFLD in subjects with T2DM, the odds ratio (OR) were 3.27 (95% confidence interval [CI], 2.03–5.27; P < 0.001) for NAFLD in the highest TyG quartile after adjustment for known confounders. In stratified analysis, an elevated TyG index were more remarkably associated with NAFLD in younger patients (< 65 years; OR, 2.35; 95% CI, 1.83–3.02; P < 0.001), females (OR, 2.69; 95% CI, 1.67–4.32; P < 0.001), patients with BMI < 25 kg/m2 (OR, 2.80; 95% CI, 2.01–3.91; P < 0.0001), and with lower high-density lipoprotein cholesterol (< 1 mmol/L; OR, 2.76; 95% CI, 1.98–3.83; P < 0.001).
Conclusion
The TyG index is significantly associated with NAFLD and shows superior ability for identify NAFLD risk compared with other lipid and glycemic parameters in T2DM.
Similar content being viewed by others
Background
Nonalcoholic fatty liver disease (NAFLD) has emerged as a growing global public health concern and is the most common cause of chronic liver disease worldwide[1, 2]. NAFLD is also strongly associated with overweight/obesity, insulin resistance (IR), metabolic syndrome (MS), and type 2 diabetes mellitus (T2DM)[3, 4]. NAFLD is characterized by pathological ectopic fat accumulation accompanied by low-grade chronic inflammatory state in the liver[5]. Previous studies suggested that NAFLD increases the risk of developing T2DM; worsens glycemic and lipid control; and contributes to the pathogenesis of major chronic cardiometabolic complications, such as IR, dyslipidemia, MS and cardiovascular disease (CVD), especially in people with established T2DM[6, 7].
The recently developed triglyceride–glucose (TyG) index, which is easily calculated using fasting blood glucose (FBG) and triglyceride (TG) levels, is consider an ideal substitutional marker of IR in general population[8, 9]. Additionally, the TyG index is more suitable in determining IR than other surrogate indexes, such as the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR)[10, 11]. The TyG index was closely associated with BMI, total cholesterol (TC), TG, FBG, HbA1c levels, HOMA-IR, and increased incidence of MS and NAFLD[12, 13]. Furthermore, previous studies showed that glucose and lipid metabolism are closely associated with NAFLD. Lipotoxicity and glucotoxicity, which begin in hepatocyte exposure to high lipid and glucose levels, respectively, play vital roles in the development and subsequent progression of NAFLD[14]. Thus, the TyG index has been recommended as a simple and reliable indicator to identify individuals at risk for NAFLD[15, 16].
However, studies on the association between the TyG index and NAFLD and the comparison of the discriminative abilities of the TyG index, lipid parameters, and glycemic parameters for NAFLD risk, especially in patients with T2DM, are lacking[16]. Impairment of glucose and lipid metabolic pathways, which has been propelled by the prevalence of obesity and T2DM, is most likely behind the increase in NAFLD population. As the prevalence of NAFLD varies among subgroups of patients with obesity and diabetes, stratification of patients with diabetes might improve the diagnosis of NAFLD and prediction of its progression[17]. Therefore, our study aimed to characterize the relationship between the TyG index and NAFLD and compare the discriminative power of the TyG index, lipid parameters, and glycemic parameters in identifying the risk of NAFLD in patients with T2DM.
Methods
Study population
We included 2280 individuals with T2DM aged ≥ 18 years who had undergone liver ultrasonography. All patients included in this study were hospitalized at the First Affiliated Hospital of Zhengzhou University from January 2018 to December 2020. Subjects with previous histories of hepatic virus infections, autoimmune hepatic disease, other chronic hepatic diseases, alcohol consumption greater than 140 g/week in men and 70 g/week in women or liver cirrhosis by ultrasonography, as well as the participants without complete data on BMI, TG level, FBG level, or ultrasonic liver examination were excluded. According to the guidelines described by the Asia-Pacific Working Party, NAFLD was defined as presence of fatty liver. Fatty liver was determined by ultrasound scan, the presence of increased echogenicity of liver compared to renal cortex[18]. The study protocol was approved by the Ethical Committee of the First Affiliated Hospital of Zhengzhou University, and the requirement for informed consent was waived.
Anthropometric and biochemical measurements.
Demographics; medical history; and social habits, including smoking and drinking habits, were obtained via a self-reported questionnaire at the first visit. Height and body weight were measured, and BMI was calculated as weight divided by the square of the height (kg/m2). Obesity was defined according to the criteria of the Asia-Pacific region (BMI ≥ 25 kg/m2)[19]. Blood pressure was measured after at least 10 min of rest. Hypertension was defined as blood pressure ≥ 140/90 mmHg or the use of antihypertensive drugs. Blood samples were collected after overnight fasting and analyzed for biochemical parameters, such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), FBG, uric acid (UA), and serum lipids (including TG, TC, high-density lipoprotein cholesterol [HDL-C], and low-density lipoprotein cholesterol [LDL-C]). All measurements were determined by chemiluminescence on an auto-analyzer. Glycosylated hemoglobin (HbA1c) was measured by high-pressure liquid chromatography. The TyG index was calculated as ln [(TG (mg/dL) × FBG (mg/dL)) /2][9].
Abdominal ultrasonography.
Based on the guidelines proposed by the Asia-Pacific Working Party, NAFLD was diagnosed by the presence of fatty liver, and the presence of excessive alcohol intake (> 140 g/week for men, > 70 g/week for women) and history of hepatic viral infection and the utilization of steatogenic or hepatotoxic medicines were ruled out. Fatty liver was assessed semi-quantitatively by a professional operator using standard method as the presence or absence of hepatic steatosis by ultrasound scan and the presence of increased echo in the liver compared with the renal cortex[18].
Statistical analyses
Normality testing was conducted, and continuous variables were presented as median and interquartile range because of their skewed distribution, whereas categorical variables were presented as percentages. Differences between the participants with NAFLD and non-NAFLD were assessed using Mann–Whitney U test for continuous variables and chi-square test for categorical variables. Binary logistic regression analysis was conducted to assess the association of the TyG index with NFALD after adjustment for confounding factors. Odds ratios (OR) with 95% confidence intervals (CI) for the risk of NAFLD were calculated. The following regression models were applied: unadjusted in Model 0; adjusted for age and sex in Model 1; further adjusted for BMI in Model 2; further adjusted for hypertension, smoking status, drinking habits, duration of diabetes mellitus, and AST and ALT levels in Model 3; and further adjusted for HbA1C, FBG, UA, TC, and HDL-C levels in Model 4. Subgroup analyses of different glycemic and lipid parameters and their interactions were performed after adjustment by Model 3. P < 0.05 was considered statistically significant. All statistical analyses were performed by SPSS version 26.0.
Results
Main characteristics of the study population by NAFLD.
A total of 2280 patients with T2DM were included. Among which, 67% were male, and 1543 (67.7%) had NAFLD. Compared with the non-NAFLD group, participants in the NAFLD group had a higher BMI, higher frequency of smoking or drinking, higher mean systolic and diastolic BP, shorter diabetes duration, less favorable metabolic profile (FBG, UA, AST, ALT, GGT, TC, and TG), lower HDL-C level and AST/ALT ratio, and higher TyG index (Table 1).
Associations between the TyG index and NAFLD risk.
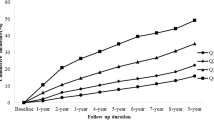
The prevalence of NAFLD remarkably increased with the increase in TyG level. Binary logistic regression was performed to examine whether TyG index is independently associated with NAFLD in patients with T2DM within four different models. The NAFLD risk significantly increased with the increasing TyG level, the OR were 5.0 in the highest TyG quartile (95% CI, 3.79–6.60; P < 0.001; Model 0). As presented in Table 2, the OR for NAFLD were higher with increasing TyG quartiles after adjusting for age, gender (4.24, 95% CI 3.20–5.63, P < 0.001 for trend; Model 1). In the highest TyG quartile, the OR were 3.02 (95% CI, 2.22–4.11; P < 0.001 for trend) for NAFLD after further adjustment for BMI (Model 2), and the OR were 2.90 (95% CI, 2.12–3.98; P < 0.001) for NAFLD after adjustment for Model 3. The associations persisted after additional adjustment in Model 4 (OR, 3.27; 95% CI, 2.03–5.27; P < 0.001). In addition, the prevalence of NAFLD in individuals with the highest TyG quartile was 86.3%, which showed a 1.73-fold increase compared with the prevalence in the lowest quartile (50%, Fig. 1).
Association of the TyG index, glycemic parameters, and lipid parameters with NAFLD.
Binary logistic regression models that separately consider each glycemic and lipid parameters as predictors of NAFLD were performed. Table 3 shows the OR and 95% CI of NAFLD with FBG, HbA1c, BMI, TC, TG, HDL-C, LDL-C, TyG index, TG/HDL-C ratio, and AST/ALT ratio in the total population within Model 3. As shown in Table 3, BMI (OR, 1.31; 95% CI, 1.26–1.35; P < 0.001), TC (OR, 1.13; 95% CI, 1.03–1.23; P = 0.009), TG (OR, 1.25; 95% CI, 1.15–1.34; P < 0.001), HDL-C (OR, 0.41; 95% CI, 0.29–0.57; P < 0.001), TyG index (OR, 1.82; 95% CI, 1.58–2.10; P < 0.001), TG/HDL-C (OR, 1.14; 95% CI, 1.08–1.20; P < 0.001), and AST/ALT ratio (OR, 0.68; 95% CI, 0.55–0.85; P < 0.001) were associated with NAFLD. However, FBG, HbA1C, and LDL-C levels had no association with NAFLD risk as observed in Model 3. Although the OR of HDL-C for NAFLD risk is higher in Model 3, the OR dramatically decreased after further adjustment in Model 4 (OR, 0.52; 95% CI, 0.32–0.84; P = 0.008). The OR of TyG stood out the most in comparison with the ORs of lipid and glycemic parameters, which indicates that TyG index can be a better discriminator of NAFLD.
Associations between the TyG index and NAFLD in subgroups of age, sex, BMI, HDL-C, and AST/ALT ratio.
Stratified analyses were conducted in different subgroups (age, sex, BMI, HDL-C, and AST/ALT ratio) to further validate the above results after adjustment for Model 4 as shown in Table 4. The results suggested that compared with participants with lower TyG, higher TyG levels were more remarkably associated with the risk of NAFLD in younger age (< 65 years; OR, 2.35; 95% CI, 1.83–3.02; P < 0.001), female (OR, 2.69; 95% CI, 1.67–4.32; P < 0.001), lower BMI (< 25 kg/m2; OR, 2.80; 95% CI, 2.01–3.91; P < 0.001), lower HDL-C (< 1 mmol/L; OR, 2.76; 95% CI, 1.98–3.83; P < 0.001), and higher AST/ALT ratio (≥ 0.9; OR, 2.63; 95% CI, 1.91–3.62; P < 0.001). However, no association between TyG index and NAFLD was observed in the older age subgroups (≥ 65 years; OR, 1.49; 95% CI, 0.65–3.39; P = 0.343). Additionally, in the subgroup analysis, the TyG index had interaction effects with age (P value for interaction = 0.043), BMI (P value for interaction < 0.001), HDL-C (P value for interaction < 0.001), and AST/ALT (P for interaction = 0.011) on NAFLD risk after adjusting for potential confounders (Model 4). The result indicates an excess risk due to the additive interaction.
Discussion
Although most studies explored the relationship between the TyG index and NAFLD risk, these studies focused on the general population[15, 20, 21]. Our present study focused on the associations of the TyG index, glycemic parameters, and lipid parameters with NAFLD in a T2DM population. This cross-sectional study observed a strong and positive association between the TyG index and NAFLD risk after adjustment for potential confounders. HDL-C, TG, BMI, ALT, and AST/ALT ratio were also associated with NAFLD risk but inferior to the TyG index. Further stratification analysis showed that females, patients with lesser BMI (< 25 kg/m2), younger age (< 65 years), and lower HDL-C level (< 1 mmol/L) have higher NAFLD risks when the TyG index is high. Therefore, based on the above observations, the TyG index can be used as an effective predictor of NAFLD risk in T2DM population.
NAFLD is closely associated with obesity and MS and characterized by excessive lipid accumulation in the liver tissue, which leads to hepatic IR[5, 22]. Furthermore, the hepatic IR subsequently leads to the overproduction of FBG and low-density lipoprotein. Lipotoxicity and glucotoxicity play central roles in the development and progression of NAFLD[14]. Our results showed that individuals with NAFLD had considerably higher BMI, FBG, TC, and TG levels than those without NAFLD. IR is a crucial pathophysiological mechanism of MS, which is a metabolic risk factor associated with an increased risk for T2DM and NAFLD[6, 23]. IR identification is deemed helpful to stratify and support the personalized treatment of patients with NAFLD. The TyG index combined with TG and FBG levels has been proposed as an effective substitute for IR[9]. A recent cross-sectional survey showed that the TyG index is significantly associated with hypertension, and shows the superior discriminative ability for hypertension compared with lipid parameters and glycemic parameters[24]. The TyG index is applied in assessing the value of TG and FBG because of the two parameters are intensively related. Hypertriglyceridemia is the most prevalent abnormalities in patients with T2DM, and its association with the risk of CVDs (including hypertension and NAFLD) has been clearly demonstrated. In line with previous study, the present study demonstrated the associations of BMI, TC, TG, HDL-C, and TyG with NAFLD risk, however, the association of the TyG index with NAFLD was stronger than those of lipid or glycemic parameters. Thus, the TyG index is a better indicator for identifying NAFLD risk compared with other lipid and glycemic parameters in patients with T2DM.
Studies on the interaction between BMI and HDL-C, sex, or age in NAFLD are limited. The interaction between HDL-C, age and TyG index might be due to the prevalence of low HDL-C in younger groups[25]. Thus, our study demonstrated that female, younger age (< 65 years), and low HDL-C level (< 1 mmol/L) are associated with higher NAFLD risks when the TyG index is higher. The effect of hormone levels on glucose, lipid metabolism and IR, might account for this discrepancies in different sexes and thus requires further explore[26, 27]. Although the LDL-C level was considered to be the most crucial lipid risk factor and therapeutic goal for CVDs[28], however, there was no significant association of LDL-C with the risk of NAFLD in the present study. Furthermore, when HDL-C and TC were adjusted in Model 4, the TyG index was still remarkably associated with NAFLD risk in our study. The precise mechanism of the association between TyG index and NAFLD has not been fully elucidated, but it is thought to involved IR, endothelial dysfunction, systemic inflammation, glucose and lipid metabolism disorders[29].
In our present study, we examined the association of the TyG index, glycemic parameters, and lipid parameters with NAFLD. Obviously, in all participants, the OR of TyG stood out the most in comparison with the ORs of other lipid and glycemic parameters, which indicates that the TyG index might be superior to other glycemic or lipid parameters in associating NAFLD risk. The TyG index is applied in evaluating the levels of FBG and TG in T2DM population due to the two parameters are closely interrelated. High TG levels remains one of the most prevalent abnormalities in T2DM patients, and its association with increased risk of NAFLD has been fully demonstrated[30]. This study revealed that the TyG index helps to identify potential risks of NAFLD in individuals who would otherwise be neglected. Thus, clinicians should be put their attention to individuals with high FBG and TG levels.
Serum ALT level is commonly used as a surrogate indicator for evaluating liver function in various liver diseases, and ALT seems to be closely associated with steatohepatitis[31, 32]. Furthermore, ALT has high specificity for liver injury and is considered as a cardiometabolic risk factor associated with IR, MS, and CVD[33, 34]. In accordance with prior studies, our findings showed that only 18.8% of individuals with NAFLD had increased ALT levels (≥ 40 U/L)[35, 36]. This result implicated that elevated ALT is probably inadequate to evaluate the NAFLD risk of individuals with T2DM. Thus, more sensitive biomarkers for predict the risk of NAFLD are needed. Furthermore, our data demonstrated that the diagnostic accuracy of the TyG index was superior to those of ALT and AST/ALT ratio in identifying NAFLD risk in patients with T2DM.
Obesity leads to the development of MS and comorbidities, including hypertension, hyperlipidemia, IR, NAFLD, T2DM, and CVD[37, 38]. Obesity seems to play a crucial role in the initial development and progression of NAFLD[3, 39]. Previous studies found that NAFLD prevalence increases almost linearly with BMI, whereas obesity is independently related to NAFLD irrespective of other metabolic factors[40]. Another study showed that the association of TyG and NAFLD risk was significantly stronger in non-obese subjects than that in obese ones[20]. Thus, the predictive power of TyG index for NAFLD risk was partially affected by BMI of the individuals. Interestingly, our present study also demonstrated that the OR of NAFLD dramatically decreased after adjustment for BMI in Model 2 (OR, 4.24 vs. 3.02). Furthermore, subgroup analysis indicated that the relationship between the TyG index and NAFLD risk was significantly stronger in non-obese subjects than in obese ones (OR, 2.80 vs. 1.86). Previous study demonstrated that subjects who are of normal weight but metabolically unhealthy have a higher risk of fatty liver and CVD, compared to normal weight and metabolically healthy population. The existence of a distinct fat distribution and lipodystrophy in these population may be account for the potential mechanism[41, 42]. Therefore, these results suggested that BMI is an important factor that affects the efficacy of the TyG index in identifying individuals with NAFLD risk[43].
Nevertheless, several limitations should be noted in the present study. First, the NAFLD diagnosis was only based on ultrasonography rather than liver biopsy. The accuracy and sensitivity of NAFLD diagnosis may not be absolutely reliable. However, ultrasound examination for the diagnosis of NAFLD is a preferable and accessible imaging method in clinical practice[44]. Furthermore, our study population included only T2DM patients. The conclusion may not be applicable to the general population. Therefore, identifying the causal relationship between the TyG index and NAFLD in larger and more various population is necessary.
Conclusion
The results of present study revealed a remarkable association between the TyG index and NAFLD in patients with T2DM, and the TyG index is superior to HbA1c, FBG, AST/ALT ratio, and other lipid parameters in determining NAFLD risk. Therefore, we suggest that the TyG index could be a more efficient, useful, and simple indicator for the screening and management of NAFLD in T2DM population.
Data availability
The datasets in the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALT:
-
Alanine transferase
- AST:
-
Aspartate transferase
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- CI:
-
Confidence interval
- DBP:
-
Diastolic blood pressure
- eGFR:
-
Estimated glomerular filtration rate
- FBG:
-
Fasting plasma glucose
- GGT:
-
Gamma-glutamyl transferase
- HbA1c:
-
Glycosylated hemoglobin
- HDL-C:
-
High-density lipoprotein cholesterol
- IR:
-
Insulin resistance
- LDL-C:
-
Low-density lipoprotein cholesterol
- MS:
-
Metabolic syndrome
- NAFLD:
-
Non-alcoholic fatty liver disease
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- TyG:
-
Triglyceride and glucose index
- T2DM:
-
Type 2 diabetes mellitus
- UA:
-
Uric acid
References
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, George J, Bugianesi E. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20.
Zhou J, Zhou F, Wang W, Zhang XJ, Ji YX, Zhang P, She ZG, Zhu L, Cai J, Li H. Epidemiological Features of NAFLD From 1999 to 2018 in China. Hepatology. 2020;71:1851–64.
Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism. 2019;92:82–97.
Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, Fujii H, Wu Y, Kam LY, Ji F, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–98.
Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24:908–22.
Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017;14:32–42.
Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69:1691–705.
Lee SB, Ahn CW, Lee BK, Kang S, Nam JS, You JH, Kim MJ, Kim MK, Park JS. Association between triglyceride glucose index and arterial stiffness in Korean adults. Cardiovasc Diabetol. 2018;17:41.
Hong S, Han K, Park CY. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study. BMC Med. 2020;18:361.
Brito ADM, Hermsdorff HHM, Filgueiras MS, Suhett LG, Vieira-Ribeiro SA, Franceschini S, Novaes JF. Predictive capacity of triglyceride-glucose (TyG) index for insulin resistance and cardiometabolic risk in children and adolescents: a systematic review. Crit Rev Food Sci Nutr. 2021;61:2783–92.
Mirr M, Skrypnik D, Bogdanski P, Owecki M. Newly proposed insulin resistance indexes called TyG-NC and TyG-NHtR show efficacy in diagnosing the metabolic syndrome. J Endocrinol Invest 2021.
Alizargar J, Bai CH, Hsieh NC, Wu SV. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc Diabetol. 2020;19:8.
Bullon-Vela V, Abete I, Tur JA, Konieczna J, Romaguera D, Pinto X, Corbella E, Martinez-Gonzalez MA, Sayon-Orea C, Toledo E, et al. Relationship of visceral adipose tissue with surrogate insulin resistance and liver markers in individuals with metabolic syndrome chronic complications. Ther Adv Endocrinol Metab. 2020;11:2042018820958298.
Mota M, Banini BA, Cazanave SC, Sanyal AJ. Molecular mechanisms of lipotoxicity and glucotoxicity in nonalcoholic fatty liver disease. Metabolism. 2016;65:1049–61.
Guo W, Lu J, Qin P, Li X, Zhu W, Wu J, Xu N, Zhang Q. The triglyceride-glucose index is associated with the severity of hepatic steatosis and the presence of liver fibrosis in non-alcoholic fatty liver disease: a cross-sectional study in Chinese adults. Lipids Health Dis. 2020;19:218.
Kitae A, Hashimoto Y, Hamaguchi M, Obora A, Kojima T, Fukui M. The Triglyceride and Glucose Index Is a Predictor of Incident Nonalcoholic Fatty Liver Disease: A Population-Based Cohort Study. Can J Gastroenterol Hepatol. 2019;2019:5121574.
Stefan N, Cusi K. A global view of the interplay between non-alcoholic fatty liver disease and diabetes. Lancet Diabetes Endocrinol. 2022;10:284–96.
Wong VW, Chan WK, Chitturi S, Chawla Y, Dan YY, Duseja A, Fan J, Goh KL, Hamaguchi M, Hashimoto E, et al. Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease guidelines 2017-Part 1: Definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33:70–85.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Li Y, Zheng R, Li J, Feng S, Wang L, Huang Z. Association between triglyceride glucose-body mass index and non-alcoholic fatty liver disease in the non-obese Chinese population with normal blood lipid levels: a secondary analysis based on a prospective cohort study. Lipids Health Dis. 2020;19:229.
Liu J, Guan L, Zhao M, Li Q, Song A, Gao L, Lin H, Zhao J. Association Between the Triglyceride-Glucose Index and Outcomes of Nonalcoholic Fatty Liver Disease: A Large-Scale Health Management Cohort Study. Diabetes Metab Syndr Obes. 2021;14:2829–39.
Yki-Jarvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2:901–10.
Mantovani A, Byrne CD, Bonora E, Targher G. Nonalcoholic Fatty Liver Disease and Risk of Incident Type 2 Diabetes: A Meta-analysis. Diabetes Care. 2018;41:372–82.
Zhu B, Wang J, Chen K, Yan W, Wang A, Wang W, Gao Z, Tang X, Yan L, Wan Q, et al. A high triglyceride glucose index is more closely associated with hypertension than lipid or glycemic parameters in elderly individuals: a cross-sectional survey from the Reaction Study. Cardiovasc Diabetol. 2020;19:112.
Yu Y, Xie K, Lou Q, Xia H, Wu D, Dai L, Hu C, Wang K, Shan S, Hu Y, Tang W. The achievement of comprehensive control targets among type 2 diabetes mellitus patients of different ages. Aging. 2020;12:14066–79.
Luo J, Chen Q, Shen T, Wang X, Fang W, Wu X, Yuan Z, Chen G, Ling W, Chen Y. Association of sex hormone-binding globulin with nonalcoholic fatty liver disease in Chinese adults. Nutr Metab (Lond). 2018;15:79.
Lonardo A, Nascimbeni F, Ballestri S, Fairweather D, Win S, Than TA, Abdelmalek MF, Suzuki A. Sex Differences in Nonalcoholic Fatty Liver Disease: State of the Art and Identification of Research Gaps. Hepatology. 2019;70:1457–69.
Michos ED, McEvoy JW, Blumenthal RS. Lipid Management for the Prevention of Atherosclerotic Cardiovascular Disease. N Engl J Med. 2019;381:1557–67.
Zhao J, Fan H, Wang T, Yu B, Mao S, Wang X, Zhang W, Wang L, Zhang Y, Ren Z, Liang B. TyG index is positively associated with risk of CHD and coronary atherosclerosis severity among NAFLD patients. Cardiovasc Diabetol. 2022;21:123.
Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, Yang H, Liu C, Kam LY, Tan XXE, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:739–52.
Newton KP, Lavine JE, Wilson L, Behling C, Vos MB, Molleston JP, Rosenthal P, Miloh T, Fishbein MH, Jain AK, et al. Alanine Aminotransferase and Gamma-Glutamyl Transpeptidase Predict Histologic Improvement in Pediatric Nonalcoholic Steatohepatitis. Hepatology. 2021;73:937–51.
Senior JR. Alanine aminotransferase: a clinical and regulatory tool for detecting liver injury-past, present, and future. Clin Pharmacol Ther. 2012;92:332–9.
Porter SA, Pedley A, Massaro JM, Vasan RS, Hoffmann U, Fox CS. Aminotransferase levels are associated with cardiometabolic risk above and beyond visceral fat and insulin resistance: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2013;33:139–46.
Zhao L, Cheng J, Chen Y, Li Q, Han B, Chen Y, Xia F, Chen C, Lin D, Yu X, et al. Serum alanine aminotransferase/aspartate aminotransferase ratio is one of the best markers of insulin resistance in the Chinese population. Nutr Metab (Lond). 2017;14:64.
Zhang S, Du T, Zhang J, Lu H, Lin X, Xie J, Yang Y, Yu X. The triglyceride and glucose index (TyG) is an effective biomarker to identify nonalcoholic fatty liver disease. Lipids Health Dis. 2017;16:15.
Zhang Y, He H, Zeng YP, Yang LD, Jia D, An ZM, Jia WG. Lipoprotein A, combined with alanine aminotransferase and aspartate aminotransferase, contributes to predicting the occurrence of NASH: a cross-sectional study. Lipids Health Dis. 2020;19:134.
Moore KJ, Shah R. Introduction to the Obesity, Metabolic Syndrome, and CVD Compendium. Circ Res. 2020;126:1475–6.
Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019;92:98–107.
Fan J, Luo S, Ye Y, Ju J, Zhang Z, Liu L, Yang J, Xia M. Prevalence and risk factors of metabolic associated fatty liver disease in the contemporary South China population. Nutr Metab (Lond). 2021;18:82.
Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, Chayama K, Saibara T, Jsg N. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47:586–95.
Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–27.
Stefan N, Schick F, Haring HU. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab. 2017;26:292–300.
Dai H, Xiang J, Hou Y, Xuan L, Wang T, Li M, Zhao Z, Xu Y, Lu J, Chen Y, et al. Fat mass to fat-free mass ratio and the risk of non-alcoholic fatty liver disease and fibrosis in non-obese and obese individuals. Nutr Metab (Lond). 2021;18:21.
Zhang B, Ding F, Chen T, Xia LH, Qian J, Lv GY. Ultrasound hepatic/renal ratio and hepatic attenuation rate for quantifying liver fat content. World J Gastroenterol. 2014;20:17985–92.
Acknowledgements
We would like to thank the participants in this study.
Funding
This study is supported by the National Natural Science Foundation of China (82000831).
Author information
Authors and Affiliations
Contributions
WL, YW, TFL, and SYL contributed to the conception and design of the study. WL, YW SYL, YQZ, FH, and ZL recruited the subjects and supervised the study. WL, YW, JD and EC analyzed the data. WL, EC, and YW wrote the initial draft of the paper. WL, YW, TFL, and SYL contributed to the writing, reviewing, and revising of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethical Committee of the First Affiliated Hospital of Zhengzhou University, and the requirement for informed consent was waived. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, W., Wang, Y., He, F. et al. Association between triglyceride–glucose index and nonalcoholic fatty liver disease in type 2 diabetes mellitus. BMC Endocr Disord 22, 261 (2022). https://doi.org/10.1186/s12902-022-01172-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01172-7