Abstract
Introduction
The aim of the present study was to explore and determine the association between BMI and socio-economic factors in Iran.
Methods
Adults aged 35 to 70 (n = 20,460) were included from Ardabil Non-Communicable Disease (ArNCD) cohort study. BMI was calculated as kg/m2. Principal Component Analysis (PCA) was used to determine the socio-economic quintiles. Multivariate linear regression was performed to analyze the association of BMI as dependent variable with explanatory variables, Additionally, decomposition analyzing conducted to identify factors that explained wealth-related inequality in obesity.
Results
The prevalence of overweight and obese people was 83.7% (41.4% overweight and 42.5% obese) wherein the highest frequency of obese people belonged to the age group of 45 to 49 years old (19.9%) and to the illiterate people (33.1%). The results of multivariate linear regression model showed that age, being female, marriage, lower education level, having chronic disease, alcohol use, and higher socioeconomic level positively associated with obesity. The results of the decomposition model showed that the most important variables affecting socioeconomic inequality in higher BMI level were socioeconomic status (75.8%), being women (5.6%), education level (− 4.1%), and having chronic disease (2.4%).
Conclusion
BMI showed significant association with socio-economic status, where richest people had significantly higher BMI than poorest group. Considering the direct role of high BMI in non-communicable diseases, new policies are needed to be developed and implemented by means of diet intervention and increased physical activity to control the BMI in the population of Iran.
Similar content being viewed by others
Introduction
Obesity is a major public health problem worldwide and its prevalence varies in different parts of the world and even in different groups [1]. Obesity was once common in high-income countries, however it is currently common in low-income countries [2]. The World Health Organization (WHO) estimates that globally obesity affects 500 million people and could be increased to one billion by 2030 [3].
Obesity is known as one of the main risk factors of type 2 diabetes, asthma, hypertension, stroke, coronary artery disease, cancer and related mortality, liver and gallbladder disease, sleep apnea, osteoarthritis, and gynecological diseases [4]. The health-care costs are also of concern. For instance, in the United States, total obesity-related expenditures account for 1.9% of GDP [5].
Obesity is generally caused by imbalanced intake and consumed calories. However, the cause of obesity is still unclear and is associated with a series of factors including genetics, health-related behaviors such as diet and physical activity, psychological, social, and economic factors [6, 7].
Despite widespread individual-level interventions, the obesity epidemic remains uncontrolled. Following this consensus, community-based approaches, which are opposed to the individual, can add to traditional individual interventions. In fact, large number of socio-demographic and socioeconomic indicators are associated with obesity [8].
Socio-economic inequalities in health are chiefly resulted from the socio-economic factors such as income, education, and employment status on health condition and also on account of the mediating factors such as destructive health behaviors and poor living conditions [9]. However, it should be pointed out that the nature of the relationship between obesity and socio-economic factors differs in developed and developing countries [10].
In developed countries, as per various studies, obesity widely affects people with lower SES while families with higher SES follow healthy diets. However, low-income families often choose more energetic foods to provide higher energy at lower cost. On this basis, the causes of obesity should be considered beyond individual factors in order for interventions for successful prevention and control of obesity [11].
Since recognizing the factors affecting obesity in the communities can lead to better formulation of obesity prevention and control policies, the assessment of socio-economic causes of obesity in Iran is of great importance.
Methods
Study setting and sample
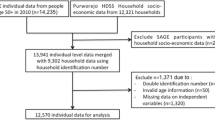
This population-based cross-sectional study was conducted in Ardabil (the capital of Ardabil province) in the northwest of Iran. Ardabil has a population of approximately 610,000 people [12]. This study uses data extracted from the Prospective Epidemiological Research Studies in IrAN (PERSIAN) [13], which was conducted to develop the context needed to modify health-care policies in the field of Non-communicable diseases (NCDs). The PERSIAN cohort is a cohort sample of various sites across Iran. Ardabil Non-Communicable Disease (ArNCD) cohort study is one of the 18 geographically distinct study areas of PERSIAN cohort study.
The study participants included 20,525 adults between the ages of 35–70 years from both men and women, mainly Azari ethnicity, and whom living in the city of Ardabil, north-west of Iran. Based on PERSIAN cohort protocol, enrolled participants have to pass several steps including clinical test, anthropometric evaluation, medical, nutritional, and mental evaluation, etc. People with disability such as deaf, blind, palsy and people with mental disorders, mental retardation, and any psychiatric illness in the acute phase; were excluded from the study. The details of the sampling design can be found elsewhere [13]. Accounting for missing data, the final sample size of the study was 20,460 people.
Data and variables
Data gathering was conducted from May 2017 to February 2020. Trained interviewers administered the questionnaire. Obesity as the dependent variable of our study was assessed based on BMI (continuous). Weight and height of the participants were measured based on American National Institute of Health (NIH). To measure weight and height, 111 Saka standing hand scales and 431 Saka wall height gauges were used, respectively. To report obesity status, BMI was classified based on the American College of Cardiology and the American Heart Association category into four groups; BMI less than 18.5 labeled as underweight, BMI between 18.5 to < 25 as the healthy weight range (normal), BMI between 25.0 to < 30 was the overweight range, and BMI from 30.0 and higher was ranged as obese. This category is defined regardless of age range [14]. Age (categorized from under 40 to upper 65), sex (male/female), marital status (single/ married/ divorced/ Other), education status (illiterate/ primary/ tips/ diploma/ academic degree) and occupation status were the independent variable in this study. Data on the non-communicable diseases (cardiovascular disease, diabetes, hypertension, and other disease including stork, renal failure, Hepatitis (B /C), Epilepsy, Amnesia, MS, etc.) was extracted based on the individuals’ self-declaration, clinical tests results, and request to see their clinical records. In addition, the wealth index, as the socio-economic status of the participants, was calculated based on their self-reported wealth, and it was divided into five quintiles from 1st quintile as the poorest to 5th quintile as the richest groups.
This study used the Principal Component Analysis (PCA) technique [15] to estimate the socioeconomic status of the study participants. Filmer and Pritchett (2001) popularized the use of PCA for estimating wealth levels using asset indicators to replace income or consumption data [16]. The estimation of relative wealth using PCA is based on the first principal component. Formally, the wealth index for household i is the linear combination,
Where, \({\overline{x}}_k\) and sk are the mean and standard deviation of asset xk, and α represents the weight for each variable xk for the first principal component. By definition the first principal component variable across households or individuals has a mean of zero and a variance of λ, which corresponds to the largest eigenvalue of the correlation matrix of x. The first principal component or wealth index can take positive as well as negative values. Assets and housing characteristics (e.g. housing situation, number of bedrooms at home, family assets, etc.), education level, and job were the explanatory variables in the PCA. Based on the wealth score, samples were divided into five quintiles from the poorest to the richest (1st quintile as the poorest and 5th quintile as the richest) as socioeconomic status.
Statistical analysis
Statistical analyses were performed using the Stata 17 for Windows running on 64-bit versions of Windows 10 (College Station, Texas, USA). Descriptive statistics for obesity indices were calculated for both men and women. Differences in continuous variables between genders were tested by Student’s t test. Differences in binomial categorized variables between men and women were analyzed by Pearson’s χ 2 test including marital status (single/married/divorced/other), educated (illiterate/primary/tips/diploma/academic), diabetes (yes/no), hypertension (yes/no), cardiac ischemic (yes/no), and socioeconomic quintile (from poorest to richest in five quintiles).
Multivariate linear regression was performed to analyze the association of BMI as dependent variable with explanatory variables. Again, anthropometric indices for obesity were not tested together in the same regression model due to the high multicollinearity. All P values reported are two-tailed and P < 0·05 was considered as statistically significant.
The multiple linear regression model Matrix form writes for all n points simultaneously:
where
y = (y1;::; yn) ∈ℝn is the n × 1 response vector
X = [1n; x1;:; xp] ∈ℝn × (p + 1) is the n × (p + 1) design matrix
_ 1n is an n × 1 vector of ones
_ xj = (x1j;:::; xnj) ∈ℝn is j-th predictor vector n × 1
b = (b0; b1;:::; bp) ∈ℝn × (p + 1) is (p + 1) × 1 vector of coefficients
e = (e1;:::; en) ∈ℝn is the n × 1 error vector [17].
Measuring and decomposing socioeconomic inequality in alcohol use
Multivariate logistic regression was used to describe the relationships between BMI and explanatory variables. The study examined the socioeconomic differences in BMI among participants using the Relative Concentration Index (RCI) and Concentration Curve (CC) [18]. We used the relative concentration index (RCI) to measure and decompose the socioeconomic inequality in BMI among Ardabil adults (35 to 70 years of age). In addition, we used Concentration Curve (CC) to investigate the socioeconomic inequality in BMI graphically. The CC plots the cumulative percentage of socioeconomic status ranked participants on the x-axis and the cumulative percentage of the health outcome (BMI in our case) on the y-axis. The curves deviation from the line of equality indicates the severity of inequality. The RCI is equivalent to twice the area between the perfect equality line (45-degree line) and the concentration curve [19]. RCI values range from − 1 to + 1. RCI is positive (negative) when the concentration curve lies below (above) the line of perfect equality. The RCI’s positive (negative) value indicated that the BMI value concentrated more among the richest (poorest) [18]. Following Wagstaff [20], RCI was separated by \(\frac{1}{1-\mu }\) for normalization. For this calculation, μ is assumed the measure of BMI. Eventually, the process of decomposition was used to classify the key determinants of the reported inequities of BMI [21].
where xk describes the explanatory variables discussed in the previous section. Thus the RCI for BMI has been decomposed as follows [22]:
Where RC is the relative concentration index for BMI, \({\overline{x}}_k\) the mean of xk determinants, Ck are the RC for explanatory variables, and \({x}_k\left(\frac{\beta_k{\overline{x}}_k}{\mu}\right){RC}_k\) is the elasticity of BMI in relation to the explanatory variable xk . \(\sum_k\left(\frac{\beta_k{\overline{x}}_k}{\mu}\right){RC}_k\) presents the contribution of the explanatory factor xk to the RC. The last term, \(\frac{AC_{\varepsilon }}{\mu }\), is the residual component. Since RCI normalised our calculation of inequality, we used the following theorem in the decomposition analysis [22].
Results
Out of 20,480 people in the study, 15,570 (76.1%) were overweight (25 < BMI ≤ 30) and obese (BMI > 30), where about 44.5% of them was obese and 31.6% of them was over weighted people. The highest frequency of obese people belonged to the age group of 45 to 49 years (47.92%). According to the results, women were more obese than men were and the prevalence of obesity was higher among married people than other groups. Moreover, the prevalence of obesity among illiterate people was higher than other educational groups (35.3%). In the case of the underlying diseases, the prevalence of obesity among people with diabetes, hypertension, and cardiovascular disease was 45.25, 51.94, and 47.21%, respectively (Table 1).
Figure 1 showed that there was significant difference between men and women in term of BMI classes, where the prevalence of overweight in men is higher than women and the prevalence of obesity in women is higher than man (p < 0.001).
Dispersion of men and women participating in the study by Body Mass Index (BMI) classes. There is a significant difference between women and men in terms of BMI, where the distribution of men is significantly higher than women is in the category of * = normal and ** = overweight groups and in contrast to the distribution of women is more than men is in the group of ## = obese people
The results of multivariate linear regression in Table 2 showed the relationship between obesity (higher level of BMI) and demographic/socio-economic factors. The multivariate linear regression model showed that the coefficient of determination (R Square) was equal to 0.397 and the coefficient of modification (Adjusted R Square) was equal to 0.396. The proximity of these two values indicated that the variables used in the model were able to work well and provided a good fit. Although, age was significantly associated with obesity, but its association decreased by increasing age and was not significant in group aged over 65 years (p = 0.836). Female gender was significantly associated with BMI (2.546, 95% CI: 2.691 to 2.40, p < 0.001). In addition, a significant and positive relationship was predicted between marital status and BMI in which married people were more obese than single group. According to the results, BMI was decreased in individuals with increased education level and there was a significant and inverse (negative) relationship between education and BMI (− 1.425, 95% CI: − 1.679 to − 1.170, p < 0.001). Furthermore, as per results, diabetes and hypertension were significantly associated with increased BMI so that people with diabetes and CVDs were less likely to be obese and overweight than people without chronic disease were. People with high blood pressure were likely to increase BMI and be overweight and obese. Smoking had significant correlation with lower BMI, in contrast, alcohol use positively correlated with high BMI. Additionally, there was a significant and positive relationship between socio-economic status and BMI wherein rich people had significantly higher BMI (6.204, 95% CI: 5.971 to 6.438, p < 0.001).
The results related to socioeconomic inequality in BMI by gender in the study population are reported in Table 3 and Fig. 2. The estimated Cn was 0.054 (95% confidence interval [CI]:0.053–0.055) for the entire population, 0.050 (95% CI: 0.049–0.052) for men and 0.068 (95% CI: 0.066 to 0.070) for women. This estimation shows that higher BMI is more common among people with higher socioeconomic status. Socioeconomic inequality in obesity was significant for both men and women, but the severity of inequality among women was higher than men was. The concentration curves are also shown in Fig. 2. According to Fig. 2, BMI concentration curves for the study population, men and women are below the equality line, indicating that higher BMI is more common among wealthy people.
Table 4 shows the decomposition analysis results of inequality in BMI in the study population. The findings related to the final effects showed that old age and higher education level (academic degree) have negative relationship with obesity (higher BMI). There is also a direct (positive) relationship between higher BMI with other variables such as female gender, marital status, alcohol use, having chronic disease, and higher economic status. The results of the decomposition model showed that the most important variables affecting socioeconomic inequality in higher BMI level were socioeconomic status (75.8%), being women (5.6%), education level (− 4.1%), and having chronic disease (2.4%). The results suggested that 82.1% of socioeconomic-related inequality in higher BMI level were explained by variables included in the study and the remaining 17.9% was associated with the variables that were not included in our decomposition model.
Discussion
The present study aimed to quantify and decompose socioeconomic inequalities in adult obesity in north-west of Iran. Using 20,460 PERSIAN cohort data from Ardabil, Iran, we analyzed being overweight and obese in Iranian adults aged 35 to 70 years. Socio-economic status was measured in overweight and obese people from Ardabil. Our descriptive results showed that 76.1% were overweight and obese in the population. However, in Ardabil, 32.6% were overweight and 15.9% were obese in 2000 [23]. Najdafi et al. showed that the overall prevalence of obesity and overweight in Iranian adults (aged 35 years and older) were 40.76 and 30.43%, respectively [24]. The increase in the prevalence of obesity indicated some changes in lifestyle and socio-economic factors in the region. Similarly, the prevalence of obesity in the United States, a country with a high prevalence of obesity and overweight, more than a third of adults were obese in 2010 [25]. In the adult population in Spain, the prevalence of obesity was 22.9 [26]. The prevalence of obesity in Turkey was 33.2% in women and 18.2% in men [27].
The comparison of the findings of the present study with the similar studies shows that the prevalence of obesity and being overweight was higher compared to other countries. Since obesity results from complex interactions among genetic, behavioral, cultural, and environmental factors, the impact of all these factors should be considered for the prevalence of obesity and being overweight in Iran [28]. The highest rate of obesity in this study could be attribute to the study population, where we conducted study on adults aged 35 and above years old. Inoue et al. showed that the prevalence of obesity is higher among adults than young [29].
Similar to previous studies in Iran [24, 30], the results of the present study showed that women were more obese than men. In previous studies, a number of factors such as unemployment, depression, unhealthy eating patterns, sleep disorders and illiteracy, low SES, number of pregnancies and physical inactivity have been identified as risk factors of obesity in women [31]. Generally, Iranian women have less physical activity than men due to limited social conditions and the type of outdoor clothing or the limited number of suitable gyms and sport clubs. In addition, childbirth can also be another reason. Various studies showed that women with lower levels of education, lower employment status, and lower incomes were more likely to be obese.
This study showed that higher education contribute with lower level of BMI. Alaba et al. showed that educational attainment was a major contributor to obesity in South Africa [32]. Similarly, Hajizadeh et al. explained income and education level as demographic variables as main factors of income-related inequality in obesity in Canada [33]. Additionally, education defined as a key contributors to inequalities in obesity in Spain [34]. In Iran, studies showed that people with lower levels of education have been more obese than their counterparts with higher levels of education [35]. As found in this study, the prevalence of obesity was higher among illiterate people than in other educational groups. Qualifications, as a form of cultural capital, may have consequences for the extent to which social standards of attractiveness and health messages about diet and physical activity are adhered to, thus emphasizing weight-loss [36, 37].
Moreover, marital status had a positive contribution to obesity wherein married adults were more obese than single people did. This finding was consistent with the results of other studies in Iran [35, 38,39,40]. Various studies have suggested some changes in the lifestyle and post-marital nutrition patterns as an influencing factor in increased BMI in adults. Findings of Azadbakht et al. (2005) showed that the percentage of energy and fat intake was higher among married people compared to single people [41]. Also, Sartorius et al. (2015) reported that single people spend more time exercising than married people [42]. Being married was detected as an important counteracting factor for high BMI in Sweden [36].
This study showed that people with diabetes were less likely to be obese and overweight. As shown in various studies, people with diabetes suffer from impaired insulin sensitivity to transport glucose to the cells of organs. Consequently, glucose remains in blood. When glucose, the fuel needed by the body, does not reach the cells, it causes weight loss, and as a result, diabetes causes a person to lose weight. Moreover, taking diabetic medications can lead to weight-loss in diabetics [43].
In the present study, people with high blood pressure were more likely to be overweight and obese. As per similar literature, high blood pressure in obese people was 2 to 6 times higher than people who were not overweight [44, 45].
Several studies that conducted a comprehensive assessment, showed a complex and controversial picture of socioeconomic inequalities in obesity in developing and developed countries. There are various studies in developed countries showed that the prevalence of obesity was common among people with low socio-economic status [46]. In contrast, there are evidences showed that the highest socioeconomic groups had the lowest prevalence of obesity [47]. According to the decomposition analysis of obesity inequality in Sweden, income was the main driving force behind obesity inequality [36]. In developed countries, socioeconomic inequalities in adult obesity is pro-rich. This is because low-income people in developed countries often use unhealthy foods, which are high in fat, sugar, and are cheaper for abdominal satiety. However, in developing countries, food consumption and obesity, which is a symbol of well-being in society, increase the prevalence of obesity in people with high socio-economic status [47, 48]. From the evidence, in several countries (including Europe, the United States, Australia, and Canada) the diet is changing economically and socially where people in higher social and economic groups tend to diet. Staying on a healthier diet using more fruits, vegetables, and less fat is common in rich groups. This indicated a person’s income or economic capability to buy healthy foods, which are normally more expensive than low-value food items [33, 49].
On the other hand, the present study in Iran as a developing country showed that rich people had significantly higher BMI. In Ardabil, obesity was statistically pro-poor, where it was in line with the previous studies in Iran. In agreement with our findings, previous studies in Iran have shown that obesity is less common in people with low SES and it is pro-poor. For example, Najafi et al. reported a lower prevalence of obesity among poor people in a sample of Iranians [50]. Mohammadi et al. (2011) found that income was positively associated with obesity [51]. Some Overall, our findings showed that higher SES was disproportionately responsible for being overweight and obese. Accordingly, crosscutting measures appear to be taken to control and prevent overweight and obesity among higher socioeconomic groups. Eliminating social and economic inequalities in health outcomes is the key public policy priority. Powerful support of government and targeted programs are needed to combat the obesity epidemic, reduce inequality in physical activity, and prepare the community for the associated consequences in the future. Eating behaviors and lifestyles in childhood are often followed in their future life. Hence, effective intervention programs to promote healthy lifestyles not only help fighting the obesity epidemic, but also prevent other chronic diseases, reduce future health-care costs, and pave the way for a healthier nation.
The present study have had several advantages: the use of valid PERSIAN group data, which was obtained through determined and controlled methods and had a large sample size. In addition, individuals’ BMIs were obtained based on height and weight measurements at the Gastroenterology Research Center. Iranian society is not homogeneous and this can be clearly seen in the results of the study. It should be noted that the data on children and the population aged under 35 years old were excluded because children and age groups under 35 years were not included in the PERSIAN cohort sample population.
Conclusion
The results showed an extremely high prevalence of obesity and being overweight in the studied area in comparison to other developing and also developed countries. BMI as the index of obesity was positively correlated with gender, marital status, education level, having chronic disease (hypertension, diabetes, and CVDs), smoking, alcohol use, and socioeconomic status. After creating socio-economic level for the population, BMI had a greater association with socio-economic status where the richest people had significantly higher BMI and socioeconomic inequality in obesity was pro-poor in this study. Considering the direct role of high BMI in non-communicable diseases and high mortality rate and also the direct and significant role of high socio-economic level in increased BMI and obesity, specific policies are needed to be developed and implemented through diet intervention and increased physical activity to control the increase in BMI of rich people. In addition, organized supports from health system with other social and economic sectors could be an effective policy strategy for reducing socioeconomic inequalities in obesity in adults.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to PERSIAN cohort protocol (available at: https://persiancohort.com/) but are available from the corresponding author on reasonable request.
Abbreviations
- ArNCD:
-
Ardabil Non-communicable Disease
- BMI:
-
Body Mass Index
- SES:
-
Socio-Economic Status
- GDP:
-
Gross Domestic Product
- NCD:
-
Non-communicable diseases
- PERSIAN:
-
Prospective Epidemiological Research Studies in IrAN
- PCA:
-
Principal Component Analysis
- RCI:
-
Relative Concentration Index
- WHO:
-
World Health Organization
References
Agha M, Agha R. The rising prevalence of obesity: part a: impact on public health. Int J Surg Oncol. 2017;2(7):e17.
Organization WH. Overweight and obesity. 2020.
Breda J, Jewell J, Keller A. The importance of the world health organization sugar guidelines for dental health and obesity prevention. Caries Res. 2019;53(2):149–52.
Garg S, Maurer H, Reed K, Selagamsetty R. Diabetes and cancer: two diseases with obesity as a common risk factor. Diabetes Obes Metab. 2014;16(2):97–110.
Biener A, Cawley J, Meyerhoefer C. The High and Rising Costs of Obesity to the US Health Care System. J Gen Intern Med. 2017;32:6–8. https://doi.org/10.1007/s11606-016-3968-8.
Kyrou I, Randeva HS, Tsigos C, Kaltsas G, Weickert MO. Clinical problems caused by obesity. Endotext; 2018.
Medvedyuk S, Ali A, Raphael D. Ideology, obesity and the social determinants of health: a critical analysis of the obesity and health relationship. Crit Public Health. 2018;28(5):573–85.
Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–40.
Moghadam TZ, Zandian H, Pourfarzi F, Poustchi H. Environmental and economics-related factors of smoking among Iranian adults aged 35–70: a PERSIAN cohort–based cross-sectional study. Environ Sci Pollut Res. 2021;28(33):1-10.
Ball K, Crawford D. Socio-economic factors in obesity: a case of slim chance in a fat world? Asia Pac J Clin Nutr. 2006;15(Supplement):15–20.
Newton S, Braithwaite D, Akinyemiju TF. Socio-economic status over the life course and obesity: systematic review and meta-analysis. PLoS One. 2017;12(5):e0177151.
Statistical Center of Iran. Population and household of the country by province and sub-province Tehran. Iran: Statistical Center of Iran; 2017.
Poustchi H, Eghtesad S, Kamangar F, Etemadi A, Keshtkar A-A, Hekmatdoost A, et al. Prospective epidemiological research studies in Iran (the PERSIAN cohort study): rationale, objectives, and design. Am J Epidemiol. 2017;187(4):647–55.
Jensen M, Ryan D, Apovian C, Ard J, Comuzzie A, Donato K, et al. Obesity Society 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–38.
Kolenikov S, Angeles G. Socioeconomic status measurement with discrete proxy variables: is principal component analysis a reliable answer? Rev Income Wealth. 2009;55(1):128–65.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32.
Fox J. Applied regression analysis, linear models, and related methods: sage publications, Inc; 1997.
Wagstaff A, Paci P, Van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33(5):545–57.
Pulok MH, van Gool K, Hajizadeh M, Allin S, Hall J. Measuring horizontal inequity in healthcare utilisation: a review of methodological developments and debates. Eur J Health Econ. 2020;21(2):171–80.
Wagstaff A. The concentration index of a binary outcome revisited. Health Econ. 2011;20:1155–60.
Wagstaff A, Doorslaer vE, Watanabe N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in. Vietnam: The World Bank; 2001.
Monteiro CN, Beenackers MA, Goldbaum M, de Azevedo Barros MB, Gianini RJ, Cesar CLG, et al. Socioeconomic inequalities in dental health services in Sao Paulo, Brazil, 2003–2008. BMC Health Serv Res. 2016;16(1):683.
Sadeghi-Bazargani H, Jafarzadeh H, Fallah M, Hekmat S, Bashiri J, Hosseingolizadeh G, et al. Risk factor investigation for cardiovascular health through WHO STEPS approach in Ardabil, Iran. Vasc Health Risk Manag. 2011;7:417.
Najafi F, Soltani S, Karami Matin B, Kazemi Karyani A, Rezaei S, Soofi M, et al. Socioeconomic-related inequalities in overweight and obesity: findings from the PERSIAN cohort study. BMC Public Health. 2020;20(1):1–13.
Rosenthal RJ, Morton J, Brethauer S, Mattar S, De Maria E, Benz JK, et al. Obesity in America. Surg Obes Relat Dis. 2017;13(10):1643–50.
Gutiérrez-Fisac J, Guallar-Castillón P, León-Muñoz L, Graciani A, Banegas J, Rodríguez-Artalejo F. Prevalence of general and abdominal obesity in the adult population of Spain, 2008–2010: the ENRICA study. Obes Rev. 2012;13(4):388–92.
Ural D, Kılıçkap M, Göksülük H, Karaaslan D, Kayıkçıoğlu M, Özer N, et al. Data on prevalence of obesity and waist circumference in Turkey: systematic review, meta-analysis and meta regression of epidemiological studies on cardiovascular risk factors. Turk Kardiyol Dern Ars. 2018;46(7):577–90.
Ayatollahi S, Ghoreshizadeh Z. Prevalence of obesity and overweight among adults in Iran. Obes Rev. 2010;11(5):335–7.
Inoue Y, Qin B, Poti J, Sokol R, Gordon-Larsen P. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. 2018;7(4):276–88.
Mehboudi MB, Raeisi A, Najaf F, Mosadeghzadeh S, Nabipour I, Darabi H, et al. The incidence and prevalence of obesity and overweight in adults during 2003 to 2009 in Bushehr Province-The Persian Gulf healthy heart study. ISMJ. 2015;18(2):409–20.
Audrain-McGovern J, Benowitz N. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. 2011;90(1):164–8.
Alaba O, Chola L. Socioeconomic inequalities in adult obesity prevalence in South Africa: a decomposition analysis. Int J Environ Res Public Health. 2014;11(3):3387–406.
Hajizadeh M, Karen Campbell M, Sarma S. Socioeconomic inequalities in adult obesity risk in Canada: trends and decomposition analyses. Eur J Health Econ. 2014;15(2):203–21.
Costa-Font J, Gil J. What lies behind socio-economic inequalities in obesity in Spain? A decomposition approach. Food Policy. 2008;33(1):61–73.
Moghimi-Dehkordi B, Safaee A, Vahedi M, Pourhoseingholi A, Pourhoseingholi M, Ashtari S, et al. Overweight and obesity and related factors in urban Iranian population aged between 20 to 84 years. Ann Med Health Sci Res. 2013;3(2):171–6.
Devaux M, Sassi F, Church J, Cecchini M, Borgonovi F. Exploring the relationship between education and obesity. OECD J Econ Stud. 2011;2011(1):1–40.
Baum CL II, Ruhm CJ. Age, socioeconomic status and obesity growth. J Health Econ. 2009;28(3):635–48.
Bakhshi E, Eshraghian MR, Mohammad K, Foroushani AR, Zeraati H, Fotouhi A, et al. Sociodemographic and smoking associated with obesity in adult women in Iran: results from the National Health Survey. J Public Health. 2008;30(4):429–35.
Karimbeiki R, Safavi M, Feizi A, Abbasi B, Nikpour M. The relationship between dietary diversity score and obesity in Tehranian adults: a case-control study. Iran J Endocrinol Metab. 2016;18(4):260–9.
Pasdar Y, Darbandi M, Niazi P, Alghasi S, Roshanpour F. The prevalence and the affecting factors of obesity in women of Kermanshah. Jorjani Biomed J. 2015;3(1):82–97.
Azadbakht M, Shiva A. General obesity and central adiposity in a representative sample of Tehranian adults: prevalence and determinants. Int J Vitam Nutr Res. 2005;75(4):297–304.
Sartorius B, Veerman LJ, Manyema M, Chola L, Hofman K. Determinants of obesity and associated population attributability, South Africa: empirical evidence from a national panel survey, 2008-2012. PLoS One. 2015;10(6):e0130218.
Apolzan JW, Venditti EM, Edelstein SL, Knowler WC, Dabelea D, Boyko EJ, et al. Long-term weight loss with metformin or lifestyle intervention in the diabetes prevention program outcomes study. Ann Intern Med. 2019;170(10):682–90.
Shibao C, Gamboa A, Diedrich A, Ertl AC, Chen KY, Byrne DW, et al. Autonomic contribution to blood pressure and metabolism in obesity. Hypertension. 2007;49(1):27–33.
Dong Y, Jan C, Zou Z, Dong B, Wang Z, Yang Z, et al. Effect of overweight and obesity on high blood pressure in Chinese children and adolescents. Obesity. 2019;27(9):1503–12.
Reyes Matos U, Mesenburg MA, Victora CG. Socioeconomic inequalities in the prevalence of underweight, overweight, and obesity among women aged 20–49 in low-and middle-income countries. Int J Obes. 2020;44(3):609–16.
Hoebel J, Kuntz B, Kroll LE, Schienkiewitz A, Finger JD, Lange C, et al. Socioeconomic inequalities in the rise of adult obesity: a time-trend analysis of National Examination Data from Germany, 1990–2011. Obesity Facts. 2019;12(3):344–56.
Hayes A, Tan EJ, Killedar A, Lung T. Socioeconomic inequalities in obesity: modelling future trends in Australia. BMJ Open. 2019;9(3):e026525.
Seidell JC. Worldwide prevalence of obesity in adults. Handb Obes Epidemiol Etiol Physiopathol. 2014;1:47.
Najafi F, Pasdar Y, Hamzeh B, Rezaei S, Nazar MM, Soofi M. Measuring and decomposing socioeconomic inequalities in adult obesity in Western Iran. J Prev Med Public Health. 2018;51(6):289.
Mohammadi N, Shobeiri F, Khirollahi A. Frequency of over Wieght & Obesity of women in referents to medical and health centers in Hamadam City. Avicenna J Nurs Midwifery Care. 2011;19(2):36–46.
Acknowledgements
We would like to thank managers and staffs of the central office of PERSIAN Cohort Study, for helping us to conduct this study.
Funding
This project was financially supported by National Institute for Medical Research Development (NIMAD: 962249). This work was funded by the Ardabil University of Medical Sciences (ARUMS). The funder had no role in study design, data analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: FP and TZM. Acquisition of data: FD and FP. Analysis and interpretation of data: HZ & TZM. Drafting of the manuscript: TZM & HZ. Critical revision of the manuscript for important intellectual content: FP, SR, HZ & TM. Statistical analysis: HZ & SR. Administrative, technical, and material support: HZ, SR, & TZM. Study supervision: HZ & TZM. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All the experiment protocol for using human’s data was confirmed in accordance to guidelines of national/international/institutional or Declaration of Helsinki in the manuscript. The informed consent was obtained from all participants or their legal guardian(s). This study was approved by the ethical committee of Ardabil University of Medical Sciences (ARUMS) with code IR.ARUMS.REC.1399.610 The Ardabil PERSIAN cohort data was used where all participants signed the informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pourfarzi, F., Rezaei, S., Zahirian Moghadam, T. et al. The socio-economic inequality in body mass index: a PERSIAN cohort-based cross-sectional study on 20,000 Iranian adults. BMC Endocr Disord 22, 178 (2022). https://doi.org/10.1186/s12902-022-01096-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01096-2