Abstract
Introduction
There is almost no published data on the assessment of self-management practice among adult type II diabetes patients in Ethiopia. Hence, we aim to assess the level of self-management practice for people with type II diabetes patients attending Adama Hospital Medical College, Ethiopia.
Method
The study was conducted from April 1 to August 30, 2021 in type II diabetes mellitus patients at Adama Hospital Medical College. The survey was performed using the diabetes mellitus self-Management questionnaire, which consists of four domains Physical activity, Physician contact, Medication adherence, glucose management and dietary management of the patients. The data was analyzed using Statistical Package for Social Science (SPSS) version 20.0. Descriptive statistics was performed. Fisher's Exact Test was used to determine the presence of association between adherence to self-care behavior and other variables. P-value less than 0.05 determines statistical significance.
Result
Majority (63.4%) of respondents do not perform self-monitoring of blood glucose (SMBG). Out of a total of 93 participants, 48 (51.6%) respondents adhered to insulin therapy. Sixty-two (66.7%) adhered to recommended diet management practice, 57 (61.3%) did not adhere to physical activity recommendations and 59 (63.5%) participants adhered to overall self-care practice (DMSQ).
Conclusion
Although the importance of self-care practices in the management of diabetes were recognized to be useful and effective for achieving glycemic control and preventing serious diabetes complications, our study found that most patients had not adhered to self-care practice especially in terms of SMBG and physical activity. Overall (DSMQ) adherence to self-care practice was optimal amongst type II diabetes patients in AHMC Chronic care unit.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is defined as a metabolic disorder of multiple etiologies characterized by chronic hyperglycemia with disturbance in carbohydrate, protein and fat metabolism resulting from defect in insulin secretion, insulin action or both. The World Health Organization has projected that in 2030 the global prevalence of DM in all age ranges wild becomes 4.4% or a total of 366 million diabetes patients. The Ethiopian diabetes association (EDA) estimated 2–3% prevalence in 2013 in Ethiopia [1,2,3]. Diabetes reduces both quality of life and life expectancy and imposes large economic burdens on individuals and on national health care systems directly or indirectly [4].
Acute and Long-term complications of diabetes can be reduced by following ongoing patient self-managements. Effective diabetes self-care can be achieved using the following actions: lifestyle modification, diet control, regular physical exercise, smoking cessation, weight reduction, self-blood glucose monitoring, medication adherence and foot care are effective treatments for improving diabetes consequences; so that self-care behavior adherence and patient education are the first steps in helping patients to better care and manage their disease [3,4,5,6,7]. About 95% of diabetes treatment depends on self-care behaviors regardless of the type of diabetes and similarly the patients and their families accomplish the self-care, hence diabetes patients must correct their behavior like adherence to prescribed medication, diet control, and changes to physical activity especially for older patients to prevent diabetes complications, which may be potentially lethal [8, 9]. Therefore, this study was aimed to identify personal perceptions of diabetes patients towards self-care behaviors.
Different studies done in different countries showed that Self-reported adherence to medication was low. A cross sectional study was done on physical activity and reported barriers to activity among type II diabetes patients in United Arab Emirates, Jimma University and Arba Minch (Ethiopia) and the result of the study showed that of the 390 patients recruited, only 25% reported an increase in their physical activity levels following the diagnosis of diabetes and only 3% reported physical activity levels that meet the recommended guidelines [10,11,12,13,14,15,16,17,18]. Since there is no research on diabetes self-care management practice in Adama, we hope that our study will provide better solutions for the patients, the health professionals, and the governmental and non-governmental health facilities.
Methods
Study area and sampling
The study was conducted from April 1 to August 30, 2021 in Adama Hospital medical college located in Adama Town. Adama is located at 99 km away from the capital city of Ethiopia, Addis Ababa, to the east. According to the central statistical agency report in 2007 E.C, the town has a total population of 341,796 (male 170,838 and female 170,953). The information from Adama town health Bureau shows that currently the town has 1 governmental Medical college hospital, 7 government health centers, 4 private Hospital, 94 private clinics with different level of which 17 special privet clinics, 4 Non-Governmental clinics and 108 drug store and Pharmacies. The college hospital, AHMC, has catchment population of about 5.2 million serving as referral hospital for all nearby district hospitals and the adjacent regions. Currently the hospital provides a service for 106 type II Diabetes patients. A cross-sectional study design was used and data was collected by using semi-structured questionnaire through face to face interview. Source populations were all type II diabetes who visited AHMC for diabetes follow-up care. Study subjects were those aged, 18 years and older diagnosed with type II diabetes who visited the hospital at the time of data collection period and fulfills eligibility criteria. Before starting the data collection, questionnaires were prepared in English and translated into Amharic and translated back into English to check its consistency. The Amharic versions were used for data collection after pretesting on 5% (9 patients) of the actual sample size in AHMC type II diabetes. One clinical pharmacy, one nurse for data collection and one medical doctor (MD) working in the hospital for supervision were given orientation before data collection. During the study period the effect of different factors affecting self-glucose management practice, dietary control practice, medication adherence practice, physical exercise practice, physician contact practice, and overall practice were assessed. Continuous follow up and supervision was made by the principal investigators throughout the data collection period. The data was analyzed by Statistical Package for Social Science (SPSS) version 20.0. Descriptive statistics was used for most variables; a Fischer Exact Analysis was employed to determine the presence of association between adherences to self-care behavior with other variables at P-value less than 0.05.
Sample size determination
Sample size was determined by using single population proportion.
n = (Z1-α/2)2 p (1–p)/d2 = (1.96)2*0.49(1–0.49)/ (0.05)2 = 384, Where: n = the required sample size.
Z = the standard normal deviation, set at 1.96 (for 95% confidence interval), P = prevalence of poor self-care behaviors toward diabetes = 49%, d = the margin of error (precision) = 5%. The final sample size was determined as follows by using the following correction / reduction formula for the estimated Sample size < 10,000 as a following: nf = ni/(1 + ni/N), Where: nf = The final sample size, ni = Initial sample size 384, N = Estimated total sample size of T2DM patient = 106, nf = 384/ (1 + 384/106) = 83.08, Considering a 10% non-response rate, the total sample size was:
10/100*83 = 8.3 + 83 = 91.3. So, by adding non-response rate to the final simple size it gives 91.3. Hence, 93 Type II diabetes patients were included in this study.
Eligibility criteria
Patients who were 18 years of age or older and diagnosed with type II diabetes, residents of the catchment area, neither mentally nor physically handicapped, and not having acute illness as opposed to chronic disease like DM.
Ethical consideration
Ethical clearance was obtained from Institutional Review Board (IRB) of Rift Valley University for research to be performed in accordance with the Declaration of Helsinki. Interview was carried out only with full informed consent of the patient being interviewed. Each patient was assured that the information provided by him/ her was confidential and used only for the purpose of research. Patients were allowed to refuse or discontinue participation at any time they want.
Results
Socio demographic characteristics
A total of 93 male and female adult type II diabetes patients were interviewed using prospective cross-sectional standardized structure questionnaire and included in the analysis. Of all patients 52 (55.9%) and 41 (41.1%) were female and male respectively. The majority of the study participants were in the age group of 38 to 67 years. The mean age in which diabetes disease started was 52.8 ± 14.7 years with minimum age of 24 and maximum age of 81. The mean duration of diabetes was 11.11 ± 8.019 years with minimum of 1 year and maximum of 34 years. The BMI of the respondents was 23.2 + 3.2 with minimum BMI of 16 and maximum BMI of 34.7 and FBS of the patients was by mean of 177.88 + 49.24 with minimum of 71 and maximum of 358. Sixty-one (65.6%) were married, 30 (32.3%) completed primary level of education and 34 (36.6%) were housewives (Table 1).
Knowledge and attitude towards diabetes
The majority of the patients, 63 (67.7%), had negative attitude towards the disease, thus illustrating that most of the patients were pessimistic towards diabetes. Fifty-four (58.1%), subjects had good knowledge about diabetes and its care principles. Overall, patients had good knowledge on diabetes and its self-care practices when asked about causes, types and management principles of diabetes, accordingly (Table 2).
Co-morbidity conditions and treatment intensity
Twenty-two (23.7%) have Hypertension and 2 (2.2%) Ischaemic heart disease. The other medical conditions reported are Asthma and Chronic Kidney Disease (CKD), and chronic complications are Peripheral Neuropathy, and Retinopathy. From the total of study participants about 48 (51.6%) followed by 41(44.1%) and 4 (4.3%) had utilized insulin therapy, oral hypoglycemic agents (OHA), and both (OHA & Insulin) respectively (Table 3).
Self-care practice domains and adherence conditions
From the different self-practice domains patients showed greater adherence towards medication adherence (97.8%), health care (86%), dietary plan (66.7%), DSMQ (63.5%) and poor adherence SMBG (38.7%), and physical activity (32.3%). Majority of participants (65.5%) were not adhered to SMBG which means, monitored less than 7 times per week and almost all patients alleged that they did SMBG practices when they had symptoms of hyperglycemia or hypoglycemia. Presence of glucometer at home, education and monthly income was found to have statistically significant association with adherence to SMBG practice (Table 4).
Among factors listed, presence of co-morbidities (p = 001) and educational status (p = 0.037) have significant association with self-glucose management practices. The other factors like consumption of social drugs, glucometer presence at home, diet management and presence of complications don’t have significant association (Table 5).
A Fischer Exact test of independence was performed to the relationship between different factors and medication adherence. Among the factors physical exercise and marital status has significant association (p = 0.007) and (p = 001) respectively. The other factors like family history of diabetes, patients attitude, presence of glucometer at home etc. didn’t have a significant association (Table 6).
Presence of comorbidities (p = 0.024), diabetic complications (p = 0.08) and physical exercise (p = 0.012) significantly affected self-care dietary management practices as compared other factors listed in the table below (Table 7).
As can be seen in Table 8, with an exception of diabetes follow up (p = 0.012) the other factors don’t have significant association with physical exercise practice.
Among all factor’s, marital status (p = 0.024) and diabetes follow up (p = 0.002) have greatly affected the self-care physician contact practices of the patients (Table 9).
It is observed that the overall self-care practices of the patients were significantly affected by the sex of the patients (p = 0.03), marital status (p = 0.035), and presence of comorbidities (p = 0.021) (Table 10).
Discussion
Inadequate diabetes self-management remains a significant problem facing health care providers and populations in all settings. Patients, who have adequate self-management have better outcomes, live longer, enjoy a higher quality of life, and suffer fewer symptoms and minimal complications. Diabetes self-management strategies increase lifestyle adjustments to maintain best possible diabetes management to achieve optimal glycemic control in patients with type II diabetes [4, 5]. In this study the current situation of adherence to self-care practices of patients with type II diabetes in AHMC and factors that contribute to efficient adherence to self-care practices of diabetes was investigated. Accordingly, about 48(51.6%) practiced the recommended self-care practices activities which is similar with the study done Jimma University specialized Hospital (50.1%) [17].
High level of diabetic knowledge was the reference group practice which is better than study conducted in Nekemte Referral Hospital (45%). This variation could be due to difference in glycemic target range used, instruments used to self-care practices adherence. From the total of study participants, the treatment intensity of the patients was insulin therapy 48(51.6%), oral hypoglycemic agents 41(44.09%) and both treatment 4(4.3%) respectively when compared to the treatment intensity of the patients done in Black Lion Specialized Hospital, Ethiopia [6, 7, 19].
This study also showed that only 34.4% were adhered to SMBG (self-monitoring of blood glucose) practices. This result is slightly lower than study done in Ethiopia (36.1%) elsewhere. Although SMBG is recognized to be useful and effective in achieving diabetes control, this study has found that only a minority of patients with diabetes were performed SMBG practices. This is probably related to lack of awareness on its importance in the management of diabetes and there are relevant financial barriers to purchase the device and its strips [18].
There was no significant association between education, Glucometer at home, diet control knowledge and presence of complications, presence of co morbidities and self-care glucose management practices. When compared with the study done in TASH Majority of participants (63.9%) were not adhered to self-monitoring of blood glucose which means, even almost all patients were said that they did SMBG practices when they had symptoms of hyperglycemia or hypoglycemia or at the time of health care visit and so that only (36.1%) were adhered which means monitored at least highly estimated monthly income were adhered two times more than counterpart which is similar with our study [20].
According to this study those patients with comorbid conditions, with family history of diabetes, who did not follow a physical exercise were more likely to exercise poor self-care medication adherence than patients with the listed conditions. Patients who were married, single, widow/er, who were not having glucometer at home, who didn’t follow diet control, who didn’t experience hypoglycemic episode, were more likely to exercise good self-care medication adherence practice. Patients who were hospitalized due to diabetes were more likely to exercise optimal self-care medication adherence practice when compared to patients who were not hospitalized due to diabetes and this study is in line with the study done in Cambodia [21].
There was no significant association between genders and diabetes follow up and self-care medication adherence practices. When compared with the study done in TASH total of (63%) study participants were adhered with prescribed anti-diabetes drugs but out of the total study subjects (37%) were not adhered. Of the whole adhered patients (60.3%) and (66%) were female and male respectively. In other hand the treatment intensity of the patients were oral hypoglycemic agents (28.4%), insulin therapy (59.6%) and both treatment (12%). Individuals who took insulin injection as treatment intensity were three times adhered than those who took oral hypoglycemic agents. However, no association to other health status data and socio demographic characteristics which is similar with our study by adherence and type of treatment highly taken [7, 20].
Patients with comorbid conditions were more likely to exercise poor self-care dietary management practice than were patients who did not had co-morbid conditions. Patients who did not follow a physical exercise plan were more likely to exercise poor self-care dietary management practice when compared to patients who followed a physical exercise plan. Patients who didn’t preferred special diet were more likely to exercise poor self-care dietary management practice when compared to patients who preferred special diet. Female patients were more likely to exercise poor self-care dietary management practice when compared to male patients. Patients who abused social drugs were more likely to exercise poor self-care dietary management practice when compared to male patients, there was no significant association between presence of complications, knowledge of complications, diabetes follow up, experienced hypoglycemia, marital status and self-care dietary management practice.
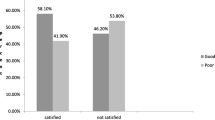
Majority (58.6%) of the study participants were not adhered to recommended diet management practices and only (41.4%) of patients were adhered which means follow recommended diet management practices as compared to the study conducted in TASH. This study showed contrast result in TASH where participants with high level of education were about three times more likely to be adhered to diet management practices when compared with their counterparts and patients with high monthly income were showed six times more engaged in diet management practices when compared with very low monthly [20].
Patients who preferred diet control were more likely to exercise good self-care physical management practice when compared to patients who did not prefer diet control. Patients who did not follow a physical exercise plan were more likely to exercise poor self-care physical management practice when compared to patients who followed a physical exercise plan. One possible reason for the diverge results of the present study may be due to the behavior of patients regarding medication adherence. Some diabetes drugs cause a hypoglycemic complication, so patient who adhere the medication can face hypoglycemic episode.
Patients with family history of diabetes were more likely to exercise optimal self-care physical management practice than were patients with no family history of diabetes. On the other hand, findings of a study conducted in Nepal indicated that only 84 (21.4%) of the patients with family history of diabetes adhere to physical activity and 79.1% were not adhered which is lower than our study [21].
There was no significant association between education, follow-up, gender and self-care physical management practice. When compared with the study done in TASH of the total study participants one hundred fifty-nine (49.1%) were reported adhered to physical activities that exactly meet the recommended guidelines and about one hundred sixty-fives were not adhered. Single marital status participants and who attended higher level of education showed a significant association to their adherence condition which is about five times and two times with regard to physical activity relatively when compared with their counterparts and in the same way also patients who had greater average monthly income were adhered to the physical activity practices about three times which is similar result with our study by adherence which is slightly poor [20]. When compared with the study done in Arba Minch of the total study participants 169 (87.1%) of patients had good relationship with professionals caring for their diabetes and only 13(6.7%) respondents had poor relationship with health professionals caring for their diabetes [22].
Patients who were single were more likely to exercise good self-care overall management practice when compared to patients who were married, divorced and widow/er. Male patients were more likely to exercise self-care overall management practice than female patients. Those patients who had hypoglycemic episode, who didn’t prefer special diet were less likely to exercise optimal self-care overall management as compared to patients who didn’t experienced hypoglycemic and who preferred special diet. There was no significant association between presence of co morbidities, social drugs abuse and overall self-care management practice. When compared with the study done in TASH Self-care practice were reported adhered in (51.5%) patients and not adhered in (48.5%) participants. There was statistically significant association between females with higher level of education and adherence level to overall diabetes self-care practice and about two and three times more likely to be engaged in self-care practices when compared with male and illiterate participants. Similarly, those participants who have high income were adhered two times more which is similar result with our study [20].
Conclusion
The important role of self-care practices in management of diabetes were recognized to be useful and effective in achieving diabetes control and preventing its serious complications. However, this study revealed that; adherence to self-care practices particularly physical activity, self-monitoring of blood glucose and glycemic control of adult type II diabetes was low. In this study patients had high level of knowledge and attitude on diabetes. The patients gender, marital status and hypoglycemic episode experience are independent associated factors for adherence to overall self-care practices towards type II DM.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due fear of data using by another person but are available from the corresponding author on reasonable request.
Abbreviations
- ADA:
-
American diabetes association
- AHMC:
-
Adama Hospital Medical College
- BMI:
-
Body mass index
- DKT:
-
Diabetic Knowledge Test
- DM:
-
Diabetes mellitus
- DSMQ:
-
Diabetes self-management questionnaires
- EC:
-
Ethiopian calendar
- EDA:
-
Ethiopian diabetes association
- FBG:
-
Fasting blood glucose
- FBS:
-
Fasting blood sugar
- IDF:
-
International diabetes federation
- IRB:
-
Institutional review board
- MMAS:
-
Morisky medication adherence scale
- OHA:
-
Oral hypoglycemic agent
- RVU:
-
Rift Valley University
- SDSCA:
-
Summary of diabetes self-care Activities
- SMBG:
-
Self–monitoring blood glucose
- SPSS:
-
Statistical packaging for social sciences
- TASH:
-
Tikur Anbessa Specialized Hospital
- T2DM:
-
Type II diabetes mellitus
- WHO:
-
World Health Organization
References
Zekewos A, Loha E, Egeno T, Wubshet K, Merga Z. Prevalence of Diabetes Mellitus and Associated Factors in Southern Ethiopia: A Community Based Study. Ethiop J Health Sci. 2018;28(4):451–60. https://doi.org/10.4314/ejhs.v28i4.11.
Ismail M, Omar M, Piterman L, Lieng T, Wijesinha S. Self-monitoring of blood glucose among diabetes patients attending government health clinics. Med J Malaysia. 2007;62(2):147–51.
Majra JP, Acharya D. Awareness regarding self-cares among diabetes in rural area. Middle east journal of medicine, 2009.
Tan M. Self-care practices of Malaysian adults with diabetes and sub-optimal glycemic control patient. Patient Educ Couns. 2008;72(2):252–67.
a Jankowska-Polanska B, Swiaotoniowska-Lonc N, Karniej P, Polanski J, Tanski W, Grochans E. Influential factors in adherence to the therapeutic regime in patients with type 2 diabetes and hypertension. Diab Res Clin Prac. 2021;173:108693. https://doi.org/10.1016/j.diabres.2021.108693.
Dagnew B, Demissie GD, Angaw DA. Systematic Review and Meta-Analysis of Good Self-Care Practice among People Living with Type 2 Diabetes Mellitus in Ethiopia: A National Call to Bolster Lifestyle Changes. Evidence-Based Complementary and Alternative Medicine. 2021;2021:420–43. https://doi.org/10.1155/2021/8896896.
Al kabi J, Al-maskari F, Saadi H, Afandi B, Parkar H, Nagelkerke N. Assessment of Dietary practice among diabetes patients in United Arab Emirates. J soc biomed diab res. 2008;5(2):110–5.
Al-Kaabi J, Al-Maskari F, Afandi B, Parkar H, Nagelkerke N. Physical activity and reported barrier to activity among type 2 diabetes patterns in United Arab Emirates. Journal of the society for biomedical diabetic research. 2009;6(4):271–8.
Świątoniowska Lonc N, Polański J, Tański W, Jankowska-Polańska B. Impact of Cognitive Impairment on Adherence to Treatment and Self-Care in Patients with Type 2 Diabetes. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2021;14:193–203. https://doi.org/10.2147/DMSO.S284468.
Bonger Z, Shiferaw S, Tariku EZ. Adherence to diabetic self-care practices and its associated factors among patients with type 2 diabetes in Addis Ababa. Ethiopia Patient Prefer Adherence. 2018;12:963–70. https://doi.org/10.2147/PPA.S156043.
Yusuff KB, Obe O, Joseph PY. Adherence to antidiabetic drug therapy and self-management practices among type 2 diabetics. Pharm World Sci. 2008;30(6):876–83. https://doi.org/10.1007/s11096-008-9243-2.
Toljamo M, Hentinen M. Adherence to self-care and glycemic control among people with insulin dependent diabetes mellitus journal of advanced nursing. J Adv Nurs. 2001;34(6):780–6. https://doi.org/10.1046/j.1365-2648.2001.01808.x.
Aschalew AY, Yitayal M, Minyihun A, Bisetegn TA. Self-care practice and associated factors among patients with diabetes mellitus on follow up at University of Gondar Referral Hospital, Gondar. Northwest Ethiopia BMC Res Notes. 2019;12:591. https://doi.org/10.1186/s13104-019-4630-4.
Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E. Self-Care Behavior among Patients with Diabetes in Harari, Eastern Ethiopia: The Health Belief Model Perspective. PLoS ONE. 2012;7(4): e35515. https://doi.org/10.1371/journal.pone.0035515.2012;(7).
Ketema DB, Leshargie CT, Kibret GD, Assemie MG, Alamneh AD, Kassa GM, Alebel A. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20:309. https://doi.org/10.1186/s12889-020-8425-2.
Toobert DJ, Hampson SE, Glasgow RE. The summary of Diabetes self-care activities measure: Results from seven studies and a revised scale. Diabetes Care. 2000;23(7):943–50. https://doi.org/10.2337/diacare.23.7.943.
Mekonnen Y, Hussien N. Self-care Related Knowledge, Attitude, and Practice and Associated Factors Among Patients with Type 2 Diabetes in JUSH. Ethiopia Diabetes Metab Syndr Obes. 2021;5(14):535–46. https://doi.org/10.2147/DMSO.S296112.
Sorato MM, Tesfahun C, Lamessa D. Levels and Predictors of Adherence to Self-care Behaviour among Adult Type 2 Diabetics at Arba Minch General Hospital. Southern Ethiopia Diabetes Metab. 2016;7:6. https://doi.org/10.4172/2155-6156.1000684.
Amente T, Belachew T, Hailu E, Berhanu N. Self-care practice and its predictors among adults with diabetes mellitus on follow up at Nekemte Hospital Diabetic Clinic, West Ethiopia. World Journal of Medicine and Medical Science. 2014;2(3):1–16.
Bayray A. Self-Care Practices and Associated Factors Among Type Diabetic Patients in Tikur Anbessa Specialized Hospital, Addis Ababa. Ethiopia Research Gate. 2012;13:4219–29.
Parajuli J, Saleh F, Thapa N, Ali L. Factors associated with non-adherence to diet and physical activity among Nepalese type 2 diabetes patients; a cross sectional study. BMC Res Notes. 2014;7:758. https://doi.org/10.1186/1756-0500-7-758.2014:7:758.
Nonogaki A, Heang H, Yi S, van Pelt M, Yamashina H, Taniguchi C, et al. Factors associated with medication adherence among people with diabetes mellitus in poor urban areas of Cambodia: A cross-sectional study. PLoS ONE. 2019;14(11):e0225000. https://doi.org/10.4172/2155-6156.1000684.
Acknowledgements
We would like to express our deepest appreciation to Mr. Mehari Gebremeskel by his initiative, owner of Henon Pharmacy, Addis Ababa, Ethiopia for giving us this golden research opportunity and also for covering the fund. We would also like to thank Adama Hospital Medical College staffs especially pharmacy department for their assistance in data collection. Without their involvement, this study would have not been imaginable.
Funding
The research expense is covered by Mr. Mehari Gebremeskel, owner of Henon pharmacy (Private Pharmacy).
Author information
Authors and Affiliations
Contributions
Conceptualization: Sileshi Tadesse, Zinash Beyene. Data entry: Sileshi Tadesse, Zinash Beyene. Formal analysis: Sileshi Tadesse. Investigation: Zinash Beyene. Methodology: Sileshi Tadesse, Zinash Beyene. Supervision: Sileshi Tadesse, Zinash Beyene. Manuscript preparation, Original draft: Sileshi Tadesse. Writing, review & editing: Sileshi Tadesse. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from Institutional review board (IRB) of Rift valley University. Interview was carried out only with full consent of the patient being interviewed. Each respondent was assured that the information provided by him/ her was confidential and used only for the purpose of research. Patients were allowed to refuse or discontinue participation at any time they want. The research is performed in accordance with relevant guidelines and regulations.
Competing interests
The authors have not stated any conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gemeda, S.T., Woldemariam, Z.B. Assessment of self-care practice amongst patients with type II diabetes attending Adama Hospital Medical College, Ethiopia. BMC Endocr Disord 22, 132 (2022). https://doi.org/10.1186/s12902-022-01049-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01049-9