Abstract
Background
Metabolic disorders and malnutrition are a double burden worldwide. The aim was to determine whether low calf circumference (CC) could predict nutritional risk and the cut-off values of CC for predicting nutritional risk in metabolic syndrome (MetS) patients aged over 80 years. We aimed to evaluate the risk factors for predicting mortality in MetS.
Methods
A total of 514 patients aged over 80 years with MetS were enrolled and followed for 2.5 years. On admission, demographic data, CC, and laboratory parameters were obtained. Patients with a Nutritional Risk Screening 2002 (NRS 2002) total score ≥ 3 were considered to have nutritional risk.
Results
The CC level was significantly lower in the nutritional risk group than in the non-nutritional risk with MetS group (27.1 ± 4.0 cm vs. 30.8 ± 3.9 cm). Logistic regression analysis of nutritional risk revealed that increasing CC (adjusted OR, 0.81; 95% CI, 0.74–0.88) was an independent protective factor against nutrition risk. The best CC cut-off value for predicting nutritional risk according to the NRS 2002 was 28.8 cm. Cox regression multivariate models showed nutritional risk (HR, 2.48; 95% CI, 1.22–5.04) and decreased CC (HR, 2.78; 95% CI, 1.27–5.98) remained independent risk factors for mortality.
Conclusion
Decreased CC could predict not only nutritional risk but also mortality in MetS patients aged over 80 years. The elderly who had MetS with nutritional risk should be discovered early, early intervention and early treatment. CC may be a valuable index to screen out this population.
Similar content being viewed by others
Background
With the rapid development of science and technology, the problem of ageing is becoming increasingly serious. The proportion of adults over 65 to adults of working age in most parts of the world is expected to almost double in the next 40 years [1]. Moreover, the very old people group (adults aged more than 80) has rapidly risen in the last century [2]. As people enjoy longevity, the prevalence of metabolic disorders and malnutrition is significantly increasing and has become a double burden worldwide [3].
Metabolic syndrome (MetS) is a cluster of multiple metabolic abnormalities, including abdominal obesity, dyslipidaemia, elevated blood pressure, insulin resistance, and hyperglycaemia. MetS is associated with a 2-fold increase in cardiovascular disease risk, cardiovascular mortality, myocardial infarction, and stroke, and a 1.5-fold increase in all-cause mortality [4, 5]. According to the International Diabetes Federation (IDF) report, people aged over 65 years are particularly liable to have MetS, and the prevalence of MetS ranges from 37 to 41.9% [6]. Even recently, the Singapore Population Health Study reported that the prevalence of MetS is 50.0% in older adults aged over 85 years [7].
On the other hand, increasing disease-associated malnutrition or nutritional risk, is also an important issue that can cause a significant economic burden [8]. Some research has shown that malnutrition or nutritional risk is associated with a high incidence rate of long hospital stays and high mortality [8, 9]. Some studies have identified that diabetes [10], obesity [11], and hypertension [12] are associated with malnutrition or nutritional risk increases in both young and old people. As a cluster of multiple metabolic abnormalities, the nutritional risk of MetS has not received much attention. Kim HJ identified that an increased nutritional risk was related to elderly MetS patients [13]. Furthermore, MetS with malnutrition causes high mortality in chronic kidney patients [14]. Since MetS with high nutritional risk patients may have a worse prognosis, it is necessary to confirm high-risk individuals and provide appropriate interventions in this population.
Calf circumference (CC) is a stable, highly accessible, and easily measurable index that is better than)body mass index (BMI) or waist circumference (WC) in reflecting muscle loss of the lower extremities with ageing or decreasing physical activity. In some studies, CC has been shown to be a screening method to diagnose sarcopenia, nutritional status, and mortality in hospitalized patients [15,16,17,18]. A study identified that CC could be simply substituted for WC and showed higher all-cause and cancer mortality risks than the traditional definition of MetS [19]. Since the measurement of nutritional status in elderly people may serve as a marker for MetS, CC may have the potential to identify MetS with nutritional risk. Our previous study identified that CC could predict nutritional risk in elderly people [15]. However, there is a lack of evidence to identify the association between CC and nutritional risk in the MetS group. In addition, whether CC or other factors could predict mortality is unknown in MetS.
Here, in the above statement, the aim of this study was to determine whether CC could predict nutritional risk in MetS patients aged over 80 years. If CC was an important factor in predicting nutritional status in our study, we identified the cut-off value of CC. More importantly, we further aimed to evaluate the risk factors for predicting mortality in MetS.
Methods
Study population
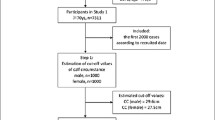
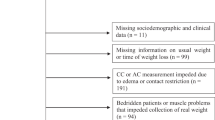
A total of 1234 hospitalized patients admitted to the Department of Geriatrics at Shanghai Jiaotong University Affiliated Sixth People’s Hospital between July 2017 and April 2018 were recruited for this study. We included people who were diagnosed with MetS according to the American National Cholesterol Education Programme (Adult Treatment Panel III) guidelines [20] for more than 80 years and who had complete medical and nutritional information available from the medical records of the institution. We excluded people who were non-MetS, were less than 80 years, had presence of carcinomatous cachexia (referent to the clinical history), had critical illness, were unable to communicate, had bedridden status, or had oedema. Finally, 514 hospitalized participants were included in the analysis and followed up by October 30, 2019. Due to the participants accepting healthcare at Shanghai Jiaotong University Affiliated Sixth People’s Hospital, there were no missing follow-ups. The study was approved by the Ethics Committee of the Shanghai Jiaotong University Affiliated Sixth People’s Hospital [approval number, 2016–141-(1)]. Written informed consent was obtained from all participants and in accordance with the principle of the Helsinki Declaration. Written informed consent was obtained from each participant.
Data collection
Detailed information about medical history and lifestyle, including smoking and drinking status, was obtained using questionnaires and confirmed through examination of medical records by trained physicians. Current smoking status was defined as yes if the subject smoked at least one cigarette per day or seven cigarettes per week in the past 6 months. Current drinking status was defined as yes if the subject consumed alcohol at least once a week in the past 6 months. Blood pressure (BP) was measured at the nondominant arm in a seated position after a 5-min rest using an automated electronic device (OMRON Model HEM-752 FUZZY’ Omron Co., Dalian, China). Three measurements were taken one minute apart, and the average of the three measurements was used in the analysis. The diagnostic criteria of MetS and its components - abdominal obesity, diabetes, hypertension, high triglycerides, decreased HDL-c were defined according to the Adult Treatment Panel III guidelines [20]. Coronary heart disease was identified if patients had a myocardial ischaemic history or electrocardiographic typical ischaemia pattern. Cerebral infarction was confirmed as a history of ischaemia attack confirmed by cerebral CT or MRI scan.
Anthropometric measurement
Body height, weight, and WC were measured by experienced physicians. Height and weight were recorded to the nearest 0.1 cm and 0.1 kg, respectively, while participants were wearing light indoor clothing without shoes. BMI (kg/m2) was calculated as weight in kilograms divided by height in square metres. WC was measured to the nearest 0.1 cm with participants in the standing position. The greatest circumference of the lower right leg was measured in the standing position as CC [21].
Nutritional risk assessment
NRS 2002 was used to determine nutritional risk. The total NRS 2002 score indicates whether the patient is nutritional risk (score ≥ 3) or non-nutritional risk (score < 3) [22]. A multidisciplinary nutrition support team evaluated the nutritional status of each patient. All patients underwent nutritional status assessment in the first 24 h of hospital stay.
Laboratory measurements
All patients fasted overnight before blood samples were collected. Haemoglobin levels were measured using a standard cyanmethemoglobin method. The measurements of fasting plasma glucose (FPG), triglycerides (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-c), and high-density lipoprotein cholesterol (HDL-c) were serum albumin were assessed using turbidimetric immunoassay (Hitachi, Tokyo, Japan). Haemoglobin levels were measured using a standard cyanmethemoglobin method. Haemoglobin A1c (HbA1c) was measured by high-performance liquid chromatography using Bio-Rad D-10 (Bio-Rad, Inc. USA).
Statistical analysis
SAS version 9.1 (SAS Institute, Cary, NC) was used for database management and statistical analysis. Data are presented as the means ± standard deviation (SD) for continuous variables or numbers (percentages) for categorical variables. Comparisons of means and proportions were performed with variance analysis and x2 tests, respectively. The association between CC and other variables was evaluated with Pearson or Spearman correlation analysis. In addition, we used logistic regression analysis to evaluate the association of CC with nutritional risk. A receiver operating characteristic (ROC) curve was used to identify the optimal CC cut-off point to predict malnutrition. Multivariable Cox regression models with hazard ratios (HRs) and 95% CIs were conducted to examine the association of independent factors with mortality. In the present study, subjects with CC values below 28.8 cm (the optimal CC cut-off point to predict nutritional risk according to the ROC curve) were defined as those with decreased CC. Adjusted odds)ratios (ORs), HRs and corresponding 95% confidence intervals (CIs) were calculated, and P < 0.05 was considered statistically significant.
Results
General characteristics of the participants
A total of 514 hospitalized patients participated in this study (mean age, 86.5 ± 6.0 years; male/female, 368/146); 43.58% in our patients of advanced age had malnutrition risk. Table 1 shows the nutritional risk and non-nutritional risk subjects’ clinical characteristics. The FPG, albumin, haemoglobin, BMI, WC and prevalence of abdominal obesity were significantly different between the two groups (P = 0.02, < 0.01, < 0.01, < 0.01, < 0.01 and < 0.01, respectively). A total of 514 MetS patients were followed for 2.5 years at the longest, 2.0 years on the average, and 105 patients died. The mortality of MetS was higher in the nutritional risk group than in the non-nutritional risk group (35.3% vs. 8.4%, P < 0.01). However, age, sex, smoking status, drinking status, systolic BP (SBP), diastolic BP (DBP), HbA1c, TC, TG, LDL-c, and HDL-c were not significantly different between the nutritional risk and non-nutritional risk participants (all P > 0.05). The prevalence of cerebral infarction, coronary heart disease, diabetes, hypertension, high triglycerides, and decreased HDL-c were not different between the two groups (P = 0.10, P = 0.24, P = 0.67, P = 0.81, P = 0.08 and P = 0.12, respectively).
The difference in CC between nutritional risk and non-nutritional risk participants
A total of 224 cases were divided as nutritional risk according to NRS 2002. The CC level was lower in the nutritional risk group than in the non-nutritional risk group (27.1 ± 4.0 cm vs. 30.8 ± 3.9 cm, P < 0.01) (Fig. 1).
Factors associated with CC
CC was significantly negatively correlated with age (r = − 0.26, P < 0.01) and nutritional risk (r = − 0.43, P < 0.01). CC values were lower in males than in females (r = − 0.21, P < 0.01). However, CC was significantly positively related to SBP, albumin, haemoglobin, BMI and WC (all P < 0.01) (Table 2).
Factors associated with nutritional risk
The adjusted OR (95% CI) of CC associated with nutritional risk was calculated in the logistic regression model (Fig.2). Increasing CC (adjusted OR, 0.81; 95% CI, 0.74–0.88; P < 0.01) and albumin (adjusted OR, 0.91; 95% CI, 0.84–0.98; P = 0.02) were independent protective factors against nutrition risk. It was also revealed that increasing FPG (adjusted OR, 1.18; 95% CI, 1.02–1.36; P = 0.03) was an independent risk factor for malnutrition risk.
The difference in the prevalence of nutritional risk according to the CC tertile
The prevalence of nutrition risk was compared according to the CC tertile. Compared with patients in tertile 3 (≥ 31.0 cm), the prevalence of nutritional risk was significantly lower among participants in tertile 2 (27.0–31.0 cm) and tertile 1 (27.0 cm) (P for trend < 0.01) (Fig. 3).
The cut-off value of CC for nutritional risk
ROC curve analysis was used to find CC’s best cut-off value for identifying nutritional risk in older MetS patients. The best CC cut-off value was 28.8 cm, and the AUC was 0.75 (95% CI, 0.70–0.79), with 72.0% sensitivity and 67.0% specificity according to the Youden index (P < 0.01) (Fig. 4).
Cox proportional Hazard analysis for mortality
Univariate Cox regression analysis indicated that age, SBP, DBP, FPG, albumin, haemoglobin, BMI, cerebral infarction, coronary heart disease, nutritional status and decreased CC were significantly correlated with mortality (Table 3). There were so few people who drank alcohol that we excluded drinking factors in the Cox regression analysis. All significant factors in the univariate Cox analysis were entered into the multivariate regression analysis. Finally, FPG, nutritional status, haemoglobin and decreased CC were independent factors influencing the mortality of MetS patients aged over 80 years. The risk of mortality increased 18.6% when FPG increased by 1 mmol/L. Nutritional risk (HR, 2.48; 95% CI, 1.22–5.04; P = 0.01) and decreased CC (HR, 2.78; 95% CI, 1.27–5.98; P = 0.01) remained independent risk factors for mortality. However, the risk of mortality decreased 4.4% as haemoglobin increased by 1 g/dL (Table 3).
Discussion
The present study provided important evidence that low CC could predict nutritional risk and mortality in MetS patients aged over 80 years. The CC value was significantly lower in MetS patients with nutritional risk than in the non-nutritional risk group. The optimal CC cut-off point for predicting nutritional risk in MetS adults aged over 80 years was 28.8 cm. Subjects with CC values below 28.8 cm were defined as those with decreased CC. Moreover, decreased CC, nutritional risk and increasing FPG were independent risk factors influencing mortality in Cox regression multivariate models.
CC is a novel, useful anthropometric parameter used to measure muscle mass and is being investigated in many fields. Some studies reported that subjects with lower CC had an increased frequency of carotid plaques and was positively associated with insulin resistance and cardiovascular disease in diabetic patients [19]. In our study, we suggested that decreasing CC and increasing FPG were all independent risk factors for nutritional risk. Our previous study identified that CC is strongly related to frailty in diabetic adults aged over 80 years [23]. As geriatrics are shifting towards identifying early stages of disability, understanding frailty and sarcopenia is essential and is still developing in the quest to prevent physical dependence. Frailty and sarcopenia overlap with each other, which could bring serious health consequences, such as mobility limitations and fracture [15]. Malnutrition plays a key role in the pathogenesis of frailty and sarcopenia [24]. Malnutrition is accompanied by loss of muscle mass and muscle function and exaggerates the observed loss of fat-free mass in elderly persons, reducing metabolic reserve and insulin sensitivity [8]. Muscle plays a variety of important roles in the human body. Therefore, the loss of muscle mass and strength will lead to a variety of functional disabilities and metabolic disorders in elderly persons [25,26,27,28]. A review indicated that protein-deficient diets markedly affect skeletal muscle function, and malnourished rats present low muscle weight and impaired morphological, metabolic, and functional development. This review also showed that impaired insulin release in malnourished rats is related to lower mitochondrial oxidative and anaplerotic capacity [29].
CC was also significantly positively related to albumin, haemoglobin, BMI and WC in our study. Albumin and haemoglobin were once the standard blood biomarkers in judging nutritional status in clinical activities. It is a complex process to assess nutritional risk, including the status of recent diet and weight loss. Due to the decline of physiological function, slow movement and cognitive function, the replacement of caregivers for elderly persons, it is more challenging to assess nutritional status in elderly persons. As a simple and noninvasive index, CC can predict the risk of nutritional risk and mortality in elderly patients with MetS, which is a very significant discovery. In 2019, the Asian Sarcopenia working group recommended the use of CC for screening sarcopenia, with a critical value of < 34 cm for men and < 33 cm for women [30]. In our previous study, we concluded that the best CC cut-off value for predicting nutritional risk according to the NRS 2002 was 29.75 cm in men and 28.25 cm in women in hospitalized patients aged more than 80 years [15]. In this research, we identified the optimal CC cut-off point (28.8 cm) for predicting nutritional status in MetS adults aged over 80 years.
MetS is often accompanied by cerebral infarction and coronary heart disease, which increase mortality in elderly persons. Lim HJ showed that well-nourished status is inversely associated with cerebral infarction [31]. However, we did not find a difference in cerebral infarction or coronary heart disease between the nutritional risk and non-nutritional risk groups. Dolores Sanchez-Rodríguez also found no difference in coronary heart disease regarding nutritional status in elderly persons [32]. BMI and WC are crucial makers in defining obesity and overweight. Although low BMI is a phenotypic criterion that may lead to malnutrition diagnosis, Rocco Barazzoni showed that obesity might present with true malnutrition because of inability to maintain body composition and performance with loss of skeletal muscle loss and function that exert major negative influences on morbidity and survival [11]. However, in our study, the prevalence of abdominal obesity was lower in the nutritional risk group than in the non-nutritional risk group (46.88% vs. 65.86%), which was possibly caused by using NRS 2002 to judge nutritional status. BMI is one of the criteria in NRS 2002. Even so, the increased prevalence of nutritional risk and the decreased CC in elderly individuals with MetS were not affected. During the process of ageing, fat is redistributed from subcutaneous to abdominal depots and to liver, muscle, and other ectopic sites [33]. Our study was conducted on elderly people who were more susceptible to abdominal obesity and did not have an elevated BMI. Hence, we speculate that there may be some patients with “sarcopenic MetS” in our study population, which is a new concept. As we had expected, we found 77.2% of our population suffered from both sarcopenia and metabolic syndrome (sarcopenic MetS), which is extremely high. There may be some differences between patients with “sarcopenic MetS” and non-“sarcopenic MetS”. Further prospective studies are needed to confirm this hypothesis.
Nutritional risk was associated with a 4.4-fold increased risk of mortality after 12 years of follow-up in healthy community-dwelling French women aged 75 or older [32]. Low CC was associated with a 1.44-fold increase in mortality in patients with cancer [18]. The findings suggest the use of CC as a simple, easy, and cost-effective anthropometric measurement to quickly screen patients at risk of death. We indicated that nutritional status and decreased CC were independent risk factors in predicting the mortality of MetS. Our conclusion proved that CC might be a very useful, simple, and noninvasive index to predict nutritional status and was a perfect factor in predicting mortality in elderly individuals with MetS.
This study had some strengths. First, this study included a large sample of more than 500 subjects, which could better reflect the nutritional status of elderly patients than previous studies. Second, the longest follow-up period was 2.5 years, so we analysed the effect of nutritional status on mortality in our MetS group. Finally, we focused on subjects aged over 80 years, who are usually excluded from many studies.
This study also had some limitations. First, elderly individuals with nutritional risk defined as an NRS 2002 score ≥ 3 were supplemented, which might change the risk of mortality. Second, due to the low proportion of female subjects in this study, we were unable to estimate the potential gender impact. Finally, this is a single-centre study of inpatients in geriatric wards. All the participants in the study were Chinese, so the results may not be applicable to other ethnic groups.
Conclusion
Decreased CC could predict not only nutritional risk but also mortality in MetS patients aged over 80 years. The optimal CC cut-off for predicting nutritional risk in our population was 28.8 cm. Our findings showed that people of very advanced age who had MetS with nutritional risk should be discovered early, and have early intervention and early treatment. CC may be a valuable index to screen out this population in MetS.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CC:
-
Calf circumference
- CIs:
-
Confidence intervals
- DBP:
-
Diastolic blood pressure
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Haemoglobin A1c
- HDL-c:
-
High-density lipoprotein cholesterol
- HRs:
-
Hazard ratios
- IDF:
-
International Diabetes Federation
- LDL-c:
-
Low-density lipoprotein cholesterol
- MetS:
-
Metabolic syndrome
- NRS 2002:
-
Nutritional Risk Screening 2002
- ROC:
-
Receiver operating characteristic
- ORs:
-
Odds ratios
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- WC:
-
Waist circumference
References
Akpek EK, Smith RA. Overview of age-related ocular conditions. Am J Manag Care. 2013;19(5 Suppl):S67–75.
Granic A, Mendonça N, Hill TR, Jagger C, Stevenson EJ, Mathers JC, et al. Nutrition in the very old. Nutrients. 2018;10(3):269.
Besora-Moreno M, Llauradó E, Tarro L, Solà R. Social and economic factors and malnutrition or the risk of malnutrition in the elderly: a systematic review and Meta-analysis of observational studies. Nutrients. 2020;12(3):737.
Bombelli M, Quarti-Trevano F, Tadic M, Facchetti R, Cuspidi C, Mancia G, et al. Uric acid and risk of new-onset metabolic syndrome, impaired fasting glucose and diabetes mellitus in a general Italian population: data from the Pressioni Arteriose Monitorate E Loro Associazioni study. J Hypertens. 2018;36(7):1492–8.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32.
Li X, Sun L, Zhang W, Li H, Wang S, Mu H, et al. Association of serum glycine levels with metabolic syndrome in an elderly Chinese population. Nutr Metab (Lond). 2018;15:89.
Merchant RA, Chan YH, Lim JY, Morley JE. Prevalence of metabolic syndrome and association with grip strength in older adults: findings from the HOPE study. Diabetes Metab Syndr Obes. 2020;13:2677–86.
Corkins MR. Why is diagnosing pediatric malnutrition important? Nutr Clin Pract. 2017;32(1):15–8.
Gingrich A, Volkert D, Kiesswetter E, Thomanek M, Bach S, Sieber CC, et al. Prevalence and overlap of sarcopenia, frailty, cachexia and malnutrition in older medical inpatients. BMC Geriatr. 2019;19(1):120.
Rajamanickam A, Munisankar S, Dolla CK, Thiruvengadam K, Babu S. Impact of malnutrition on systemic immune and metabolic profiles in type 2 diabetes. BMC Endocr Disord. 2020;20(1):168.
Barazzoni R, Gortan CG. Double burden of malnutrition in persons with obesity. Rev Endocr Metab Disord. 2020;21(3):307–13.
Azupogo F, Abizari AR, Aurino E, Gelli A, Osendarp SJM, Bras H, et al. Malnutrition, hypertension risk, and correlates: an analysis of the 2014 Ghana demographic and health survey data for 15-19 years adolescent boys and girls. Nutrients. 2020;12(9):2737.
Cruz-Jentoft AJ, Kiesswetter E, Drey M, Sieber CC. Nutrition, frailty, and sarcopenia. Aging Clin Exp Res. 2017;29(1):43–8.
Shoji T, Nishizawa Y. Chronic kidney disease as a metabolic syndrome with malnutrition--need for strict control of risk factors. Intern Med. 2005;44(3):179–87.
Zhang XY, Zhang XL, Zhu YX, Tao J, Zhang Z, Zhang Y, et al. Low calf circumference predicts nutritional risks in hospitalized patients aged more than 80 years. Biomed Environ Sci. 2019;32(8):571–7.
Maeda K, Koga T, Nasu T, Takaki M, Akagi J. Predictive accuracy of calf circumference measurements to detect decreased skeletal muscle mass and European Society for Clinical Nutrition and Metabolism-Defined Malnutrition in hospitalized older patients. Ann Nutr Metab. 2017;71(1–2):10–5.
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. 2015;15(8):969–76.
Sousa IM, Bielemann RM, Gonzalez MC, da Rocha IMG, Barbalho ER, de Carvalho ALM, et al. Low calf circumference is an independent predictor of mortality in cancer patients: a prospective cohort study. Nutrition. 2020;79-80:110816.
Wu CJ, Kao TW, Chang YW, Peng TC, Wu LW, Yang HF, et al. Does the additional component of calf circumference refine metabolic syndrome in correlating with cardiovascular risk? J Clin Endocrinol Metab. 2018;103(3):1151–60.
Gu D, Reynolds K, Wu X, Chen J, Duan X, Reynolds RF, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. 2005;365(9468):1398–405.
Zhang X, Zhang X, Zhu Y, Tao J, Zhang Z, Zhang Y, et al. Predictive value of nutritional risk screening 2002 and Mini nutritional assessment short form in mortality in Chinese hospitalized geriatric patients. Clin Interv Aging. 2020;15:441–9.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - an ESPEN consensus statement. Clin Nutr. 2015;34(3):335–40.
Zhu YX, Zhang Y, Wang YY, Ren CX, Xu J, Zhang XY. Low calf circumference is associated with frailty in diabetic adults aged over 80 years. BMC Geriatr. 2020;20(1):414.
Zhang Z, Pereira SL, Luo M, Matheson EM. Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and Meta-analysis. Nutrients. 2017;9(8):829.
Li F, Li Y, Duan Y, Hu CA, Tang Y, Yin Y. Myokines and adipokines: involvement in the crosstalk between skeletal muscle and adipose tissue. Cytokine Growth Factor Rev. 2017;33:73–82.
Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8(8):457–65.
Zoppi CC, Silveira LR, Oliveira CA, Boschero AC, Curi R, Carneiro EM. Insulin release, peripheral insulin resistance and muscle function in protein malnutrition: a role of tricarboxylic acid cycle anaplerosis. Br J Nutr. 2010;103(9):1237–50.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Lee JH, Jun HS. Role of Myokines in regulating skeletal muscle mass and function. Front Physiol. 2019;10:42.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–307.e2.
Lim HJ, Choue R. Association between poor nutritional status and severe depression in Korean cerebral infarction patients. Nutr Neurosci. 2012;15(1):25–30.
Sánchez-Rodríguez D, Marco E, Schott AM, Rolland Y, Blain H, Vázquez-Ibar O, et al. Malnutrition according to ESPEN definition predicts long-term mortality in general older population: findings from the EPIDOS study-Toulouse cohort. Clin Nutr. 2019;38(6):2652–8.
Kuk JL, Saunders TJ, Davidson LE, Ross R. Age-related changes in total and regional fat distribution. Ageing Res Rev. 2009;8(4):339–48.
Acknowledgements
We thank all the teams involved in the development and implementation of the study: Fengfeng Pan, Ding Li, Zhe Zhao, Youyi Tu, Yingying Feng.
Funding
This project was not funded by any organization.
Author information
Authors and Affiliations
Contributions
CXR and XYZ equally contributed to the conception and design of the research; YX contributed to the design of the research; CXR, YXZ and JX contributed to the acquisition and analysis of the data; CXR and XYZ contributed to the interpretation of the data; CXR and XYZ drafted the manuscript. All authors critically revised the manuscript, agree to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Shanghai Jiaotong University Affiliated Sixth People’s Hospital [approval number, 2016–141-(1)]. Written informed consent was obtained from all participants and in accordance with the principle of the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors of this study declare having no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ren, C., Zhang, X., Zhu, Y. et al. Low calf circumference can predict nutritional risk and mortality in adults with metabolic syndrome aged over 80 years. BMC Endocr Disord 22, 47 (2022). https://doi.org/10.1186/s12902-022-00964-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-00964-1